Abstract
Background
Most of prior studies to demonstrate the association between mean platelet volume (MPV) and type 2 diabetes mellitus (T2DM) risk were cross-sectional design with inconsistent results. In the present prospective cohort study, we aimed to explore the relationship between MPV and incident T2DM risk among a middle-aged and older Chinese population.
Methods
This prospective study included 14,009 individuals derived from the Dongfeng–Tongji cohort which was launched in 2008. A total of 997 incident T2DM patients were diagnosed during the mean 4.51 years of follow-up period. MPV levels were divided into quartiles. The adjusted hazard ratios (HRs) and 95% confidence intervals (95% CIs) of incident T2DM was estimated by Cox proportional hazard models.
Results
Compared with study participants with MPV < 7.49 fL, the HRs of T2DM incidence were 1.39 (95% CI 1.11–1.75), 1.14 (0.90–1.44), and 1.39 (95% CI 1.07–1.81) in study participants with 7.49 ≤ MPV < 8.43 fL, 8.43 fL ≤ MPV < 9.69 fL and MPV ≥ 9.69 fL, respectively. This positive association was more pronounced after exclusion of the newly diagnosed incident cases during the first 2 years follow-up. Further adjustment for baseline fasting blood glucose level (FBG) did not materially alter the positive association. The positive association was particularly evident among females, non-current smokers and study participants with FBG level less than 5.6 mmol/L at baseline.
Conclusion
Higher levels of MPV were independently associated with increased incident risk of T2DM in a middle-aged and older Chinese population.
Similar content being viewed by others
Background
Diabetes mellitus (DM) is a major problem worldwide and the prevalence increased rapidly especially in developing countries [1]. In China it is estimated that DM prevalence increased to 11.6% (113.9 million adults) [2]. Studies indicated that inflammation played an important role in the development of DM [3]. Systemic sub-clinical inflammation has been implicated in the development of type 2 diabetes (T2DM) [4]. Inflammatory biomarkers, such as white cell counts (WBC), C-reactive protein (CRP), tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6), were showed to be correlated with prevalent and incident diabetes [5, 6].
Platelets, the second most abundant cell type in the circulation, play a classical role in thrombosis and homeostasis [7]. In recent decades, an increasing number of evidence showed that platelets were also related to inflammation [8]. Mean platelet volume (MPV), an important morphological parameters of platelets and an easily accessible indice in routine blood test, could reflect the size and activity of platelet [9]. Higher MPV level indicates larger platelets, which are metabolically and enzymatically more active [10]. In recent decade, MPV was defined as an inflammatory marker in different diseases such as fever and inflammatory bowel disease [11, 12].
Studies showed that DM cases have increased platelet activity [13]. A latest meta-analysis [14] which included 30 case–control and cross-sectional studies found that MPV was significantly higher in T2DM cases than study participants without DM. Nevertheless, other cross-sectional studies [15, 16] and a cohort study [17] exploring the relationship between MPV and diabetes obtained inconsistent findings. In the National Health and Nutrition Examination Survey the researchers reported that MPV was strongly and independently associated with the presence and severity of diabetes in study participants with diabetes [15]. However, the large prospective study to evaluate the impact of diabetes on MPV found no associations between DM and MPV [17].
Most published studies aimed to investigate the relationship between MPV and the prevalence and severity of diabetes [15] and its complications [18, 19]. However, few study examined causal effect of MPV and incident risk of T2DM. In addition, most of the previous studies were conducted in Europeans and the sample size was relatively small. Therefore, it still remains to elucidate whether MPV level is associated with incident diabetes risk, especially in other populations including the Chinese population.
In the current study, we aimed to investigate whether MPV is independently associated with the risk of incident T2DM in a large cohort of middle-aged and older Chinese adults. We further investigated whether the association could be modified by different characteristics or health status.
Methods
Study population
The study design, methods and other detailed information of the Dongfeng–Tongji (DFTJ) cohort have been described elsewhere [20]. Briefly, a total of 27,009 retired employees of the Dongfeng Motor Corporation (DMC) were recruited in the cohort and completed baseline questionnaires, medical examinations, and provided baseline blood samples between September 2008 and June 2010, and were followed until October 2013. At the first follow-up survey in 2013, participants repeated the questionnaire interview, physical examinations, and blood collection. In total, 25,978 individuals (96.2% of those at baseline) completed the first follow-up until October 2013.
Of these 27,009 individuals, we excluded participants with myocardial infarction (MI), coronary heart diseases (CHD), stroke, tumor (n = 5258), DM (n = 3080), and who was using anti-coagulation drugs, aspirin and thrombolytic drugs (n = 2182), with abnormal platelet count (PLT) data (n = 13) as well as those with missing data on baseline MPV (n = 2467) resulting in a final study sample of 14,009 participants (5980 males and 8029 females with a mean age of 62.23 years). This study was approved by the Ethics and Human Subject committee of Tongji Medical College, Dongfeng General Hospital, and DMC. All study participants provided informed consents.
Assessment of covariates
Trained interviewers administrated interview questionnaire face to face to collect baseline information including socio-demographic characteristics (age, sex, and education), lifestyle habits such as smoking status (current, former, never), alcohol drinking status (current, former, never), physical activity, occupational history, environmental exposures, and family and medical histories. Participants who smoke at least one cigarette per day for more than half a year were defined as current smokers. Those who drink alcohol at least one time per week for more than half a year were defined as current alcohol drinkers. Physical activity was considered as those who regularly exercised at least 20 min per time for more than 6 months. Physical examination was performed at DMC-owned hospitals by trained physicians, nurses and technicians. Standing height, body weight and waist circumference were measured in individuals with light indoor clothing and without shoes. B-scan ultrasonography of the liver, gall bladder, spleen, kidney, prostate (for males) and uterus, ovaries and fallopian tubes (for females) were conducted. Body mass index (BMI) was calculated as weight (kilogram) divided by height (meter) squared. Hypertension was defined as individuals with self-reported physician diagnosed hypertension, or blood pressure ≥ 140/90 mmHg, or current use of antihypertensive medication. Hyperlipidemia was defined as total cholesterol > 5.72 mmol/L or triglycerides > 1.70 mmol/L at medical examination, or a previous physician diagnosis of hyperlipidemia, or taking lipid lowering medication.
Blood samples were collected after an overnight fast. Platelet counts (PLT), MPV, white blood counts (WBC), total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), fasting blood glucose (FBG), and hemoglobin A1c (HbA1c) were determined at the DMC-owned hospital’s laboratory. MPV, PLT and WBC were measured using a fully automated analyzer CELL-DYN 3700 (Abbott Laboratories. Abbott Park, Illinois, USA). The level of FBG was determined by aeroset automatic analyzer (Abbott Laboratories. Abbott Park, Illinois, USA) and the HbA1c level was measured with high-performance liquid chromatography D-10 system (Bio-Rad Laboratories. Hercules, CA, USA). The serum lipids were measured with the architect ci8200 automatic analyzer (Abbott Laboratories. Abbott Park, Illinois, USA).
Ascertainment of baseline and incident diabetes
The diagnosis of DM was based on the American Diabetes Association (ADA) criteria [21] when meeting any of the following criteria: (1) self-reported of physician’s diagnosis of diabetes, (2) FBG level ≥ 7.0 mmol/L, (3) HbA1c level ≥ 6.5%, (4) usage of diabetes medication (insulin or oral hypoglycemic agent). The patients were those occurred after baseline survey but before the end of October 2013. A total of 997 incident patients were diagnosed during the follow-up period.
Statistical analysis
The baseline continuous variables are expressed in means (SD) and compared by Student’s t test or analysis of variation (ANOVA) unless otherwise specified. The Categorical variables are presented as numbers and percentages and compared by Chi square analysis or Fisher’s exact test. A two-sided P value of less than 0.05 was considered to indicate statistical significance.
Eligible participants were grouped according to quartiles of MPV, and the first quartile (Q1) was regarded as the reference group. Cox proportional hazards regression model was used to evaluate the relationship between MPV and incident DM risk adjusting for covariates including age, sex, smoking status, alcohol drinking status, education, physical activity (hours per week), BMI, examination center, hypertension, hyperlipidemia, family history of DM, WBC, and PLT.
Among women, number of children, menopausal status, hormone replacement therapy, and contraception status were additionally adjusted in the Cox regression models.
Stratified analyses were further performed by baseline characteristics (including age [< 60, ≥ 60 years], sex, BMI [< 25, ≥ 25 kg/m2], current smoking [yes, no], current drinking [yes, no], hypertension [yes, no], hyperlipidemia [yes, no], WBC [< 5.7E9/L, ≥ 5.7E9/L], and baseline FBG [< 5.6, ≥ 5.6 mmol/L]). Moreover, to analyze potential interactions between MPV and main characteristics, an interaction product term was included in the model.
Finally, in order to eliminate the reverse causality between MPV and DM, we conducted sensitivity analysis by exclusion of the incident diabetes patients diagnosed during the first 2 years of follow-up. To examine whether the potential association between MPV and DM risk was due to the FBG levels at baseline, we further adjusted for baseline FBG concentrations in the full adjustment model.
Results
Baseline characteristics
Baseline characteristics of the participants according to the quartile of MPV are summarized in Table 1.
During 60,761.74 person-years of follow up, we identified a total of 997 incident diabetes cases. Among the 14,009 study participants, 42.7% were men and mean age was 62.23 years old. Overall, there were 25.07, 24.93, 24.99 and 24.99% of participant with MPV level < 7.49 fL, 7.49 ≤ MPV < 8.43 fL and 8.43 fL ≤ MPV < 9.69 fL and MPV ≥ 9.69 fL, respectively. Compared with Q1, individuals with higher levels of MPV were more likely to be younger, females, with higher levels of triglycerides, HDL-cholesterol, and WBC, and with lower levels of total cholesterol, LDL-cholesterol, and PLT. Also, study participants with higher levels of MPV were less likely to be current smokers and current drinkers. The baseline characteristics according to the quartile of MPV in women and men respectively were presented in Additional file 1: Table S1.
Hazard ratios (HRs) of DM according to quartiles of MPV
As shown in Table 2, compared with study participants in Q1, the HRs and 95% CI of incident DM for individuals in Q2, Q3, and Q4 were 1.39 (1.11–1.75, P = 0.005), 1.14 (0.90–1.44, P = 0.277) and 1.39 (1.07–1.81, P = 0.014) respectively after adjustment for potential confounders. To reduce the possibility of reverse causality between MPV and DM events, sensitivity analyses were conducted by exclusion of the incident DM diagnosed during the first 2 years of follow-up (2009 and 2010, n = 249). After exclusion the positive association were even stronger (Q2 vs. Q1 HR: 1.44; 95% CI 1.13–1.84 and Q4 vs. Q1, HR: 1.51; 95% CI 1.14–1.99, P for trend = 0.028). In the full adjustment model we further adjusted the baseline FBG levels and the positive association did not alter materially (Q2 vs. Q1 HR: 1.39; 95% CI 1.10–1.74 and Q4 vs. Q1, HR: 1.33; 95% CI 1.02–1.73).
Stratification and interaction analysis
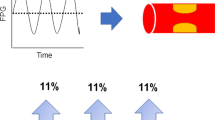
Stratified analyses were further performed by stratifying the baseline characteristics (including age [< 60, ≥ 60 years], sex, BMI [< 25, ≥ 25 kg/m2], current smoking [yes, no], current drinking [yes, no], hypertension [yes, no], hyperlipidemia [yes, no], WBC [< 5.7E9/L, ≥ 5.7E9/L], and baseline FBG [< 5.6, ≥ 5.6 mmol/L]). As Fig. 1 indicated, compared with the reference group, the HRs for study participants with MPV level ≥ 9.69 fL were more pronounced in females (HR: 1.56; 95% CI 1.07–2.53), non-current smokers (HR: 1.58; 95% CI 1.17–2.13) and individuals with baseline FPG level < 5.6 mmol/L (HR: 1.95; 95% CI 1.04–3.69) than their counterparts (P for interaction was 0.017, 0.013, and 0.021, respectively). In females, further adjustment for number of children, menopausal status, hormone replacement therapy, and contraception status obtained similar results. Females with MPV ≥ 9.80 fL had 92% increased incident risk of DM (95% CI 1.30–2.84) compared with those with MPV < 7.50 fL (P for trend = 0.002; see Additional file 2: Table S2). No interaction were found for MPV and age, BMI, current drinker, hypertension, hyperlipidemia, and WBC counts (all P for interaction > 0.05; see Additional file 3: Table S3).
Adjusted HR (95% CI) for incident T2DM in individuals with higher MPV levels compared with the reference group (MPV < 7.49 fL). All covariates were age, sex, BMI, smoking status, drinking status, education, physical activity, hypertension, hyperlipidemia, family history of DM, examination center, WBC and PLT. Each group adjusted for the other covariates except itself
Discussion
In this large cohort study, we found that higher levels of MPV were associated with increased incident risk of diabetes independent of potential confounders. These positive associations were more evident in females, non-current smokers and those with baseline FBG levels less than 5.6 mmol/L.
To our best knowledge, this is the first cohort study to investigate the association between MPV and incident diabetes risk. Accumulating studies have demonstrated that MPV was associated with stroke [22], coronary artery disease [23] and myocardial infarction [24]. A study conducted to investigate the relationship between platelet activity and type 1 diabetes mellitus (T1DM) found that platelet activation did not precede the development of microvascular complications in T1DM [25]. Further investigation in T2DM cases [26] found that individuals with T2DM accompanied by macrovascular disease had higher levels of urine thromboxane metabolite.
Cross-sectional [10] and case–control studies with relative small sample size indicated that person with diabetes or study participants with impaired fasting glucose had higher levels of MPV compared to the healthy controls [15, 27, 28]. A latest meta-analysis enrolling 30 case–control and cross-sectional studies also indicated that MPV was significantly higher among study participants with established diabetes than the healthy controls [14]. However, till now no prospective cohort study was conducted to investigate the associations of MPV levels with incident DM risk. The findings from the present cohort study lend strong support to the positive association between MPV levels and incident DM risk.
Potential mechanisms that underlying this positive association remains unclear. However, several mechanisms might involve in these associations. Firstly, activated platelets could express soluble CD40 ligand (CD40L) [29] and CD40L and its receptor CD40 extensively involved in oxidative stress and inflammatory pathways [30], which may play a role in the development of diabetes [5]. Secondly, higher MPV might partly be due to the regulation of some cytokines, such as IL-6 [31],which could increase the incident diabetes risk by damaging the body’s glucose stability and β-cell function [32]. Notably, the aforementioned associations were more evident in females. Previous studies suggested that gender could influence platelet biology [33]. In the present study, we found a significantly higher level of MPV in females (8.79 fL) than males (8.63 fL), which was consistent with other observations [34]. Oral contraceptives intake and menstruation were strongly associated with higher MPV levels in females [35] which might contribute to sex differences in the MPV level. However, in the present analysis, further adjustment for the number of children, menopausal status, hormone replacement therapy and contraception status did not materially change the positive associations of MPV with incident DM risk in females.
In the present study we found that the positive association of higher MPV and DM incidence was more pronounced in non-current smokers. Smoking was positively associated with increased MPV levels [36], inflammation [37] and immune response [38]. High levels of inflammation in current smokers and relative higher ratio of females in the non-smokers compared to the current smokers (69.2% vs. 6.7%) might contribute to the smoking-MPV interaction on incident DM risk. Similar as smoking, more evident positive association of higher MPV levels and DM incidence was found in those with normal baseline FBG level. Previous studies reported that osmotic swelling due to increased blood glucose could increase MPV levels [27, 28]. Although the underlying pathophysiological mechanisms are unclear, hyperglycemia might cover up the effects of MPV on diabetes among high-risk individuals and leave the detrimental effects robust in relatively healthy population.
The current study has several strengths. Firstly, the prospective cohort study design and relatively large sample size enable us to obtain relatively strong evidence with moderate power. Secondly, the diagnosis of baseline and incident diabetes was based on rigorous criteria, which could reduce the false positive. Thirdly, to the best of our knowledge the present study is the first one to examine the effects of MPV on incident diabetes risk in a middle-aged and older Chinese population, which could provide new insight into diabetes prediction and prevention, especially in middle-aged and older population. Fourthly, in the Cox proportional hazards regression models we have adjusted for multiple confounders including baseline hypertension and hyperlipidemia; thus to some extent the bias of these potential confounders could be minimized. Finally, after exclusion of incident DM diagnosed during the first 2 years of follow-up the positive association was even stronger, indicating the robustness of the positive association.
Limitations
Some limitations also need to be noted in the present study. Firstly, in the present study MPV was measured only once and might not represent the real MPV levels over time. Secondly, Diaz et al. [39] reported that a progressive increase in MPV with storage in EDTA measured at different time intervals up to 24 h. In the present study blood samples were stored in EDTA anticoagulation tube. However, MPV levels were measured immediately once blood samples were collected. Therefore, the influence from EDTA might be reduced to a small extent. Thirdly, we did not collect information on atrial fibrillation, obstructive sleep apnea, and seasonal changes which is reported to be associated with the MPV levels [40,41,42]. Missing data on these factors could inevitably lead to potential bias in the evaluation of the HRs for DM. Fourthly, all the participants included in the present study were middle-aged and older Chinese, therefore the findings might not be generalized to younger population or other ethnicities.
Conclusions
In conclusion, the current findings indicate that MPV, a low-cost, widely available and noninvasive marker, might be a potential risk factor of diabetes in middle-aged and older population. These findings need to be verified in other population with long follow-up period.
Abbreviations
- DM:
-
diabetes mellitus
- MPV:
-
mean platelet volume
- T2DM:
-
type 2 diabetes mellitus
- T1DM:
-
type 1 diabetes mellitus
- WBC:
-
white blood counts
- PLT:
-
platelet counts
- FBG:
-
fasting blood glucose
- HDL-C:
-
high-density lipoprotein cholesterol
- LDL-C:
-
low-density lipoprotein cholesterol
- CRP:
-
C-reactive protein
- TNF-α:
-
tumor necrosis factor-α
- IL-6:
-
interleukin-6
- CD40L:
-
CD40 ligand
- MI:
-
myocardial infarction
- CHD:
-
coronary heart diseases
- BMI:
-
body mass index
- HR:
-
hazard ratio
- CI:
-
confidence interval
- DMC:
-
Dongfeng Motor Corporation
References
Ashcroft FM, Rorsman P. Diabetes mellitus and the beta cell: the last 10 years. Cell. 2012;148:1160–71.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–59.
Marques-Vidal P, Schmid R, Bochud M, Bastardot F, von Känel R, Paccaud F, et al. Adipocytokines, hepatic and inflammatory biomarkers and incidence of type 2 diabetes. The CoLaus study. PLoS ONE. 2012;7:e51768.
Kolb H, Mandrup-Poulsen T. An immune origin of type 2 diabetes? Diabetologia. 2005;48:1038–50.
Liu C, Feng X, Li Q, Wang Y, Li Q, Hua M. Adiponectin, TNF-alpha and inflammatory cytokines and risk of type 2 diabetes: a systematic review and meta-analysis. Cytokine. 2016;86:100–9.
Wang X, Bao W, Liu J, Ouyang YY, Wang D, Rong S, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013;36:166–75.
Vermylen J, Verstraete M, Fuster V. Role of platelet activation and fibrin formation in thrombogenesis. J Am Coll Cardiol. 1986;8:2b–9b.
McFadyen JD, Kaplan ZS. Platelets are not just for clots. Transfus Med Rev. 2015;29:110–9.
Bath PM, Butterworth RJ. Platelet size: measurement, physiology and vascular disease. Blood Coagul Fibrinolysis. 1996;7:157–61.
Hekimsoy Z, Payzin B, Ornek T, Kandoğan G. Mean platelet volume in Type 2 diabetic patients. J Diabetes Complicat. 2004;18:173–6.
Sakalli H, Kal O. Mean platelet volume as a potential predictor of proteinuria and amyloidosis in familial mediterranean fever. Clin Rheumatol. 2013;32:1185–90.
Kapsoritakis AN, Koukourakis MI, Sfiridaki A, Potamianos SP, Kosmadaki MG, Koutroubakis IE, et al. Mean platelet volume: a useful marker of inflammatory bowel disease activity. Am J Gastroenterol. 2001;96:776–81.
Winocour PD. Platelet abnormalities in diabetes mellitus. Diabetes. 1992;41(Suppl 2):26–31.
Zaccardi F, Rocca B, Pitocco D, Tanese L, Rizzi A, Ghirlanda G. Platelet mean volume, distribution width, and count in type 2 diabetes, impaired fasting glucose, and metabolic syndrome: a meta-analysis. Diabetes Metab Res Rev. 2015;31:402–10.
Shah B, Sha D, Xie D, Mohler ER 3rd, Berger JS. The relationship between diabetes, metabolic syndrome, and platelet activity as measured by mean platelet volume: the National Health And Nutrition Examination Survey, 1999–2004. Diabetes Care. 2012;35:1074–8.
Morris AP, Voight BF, Teslovich TM, Ferreira T, Segrè AV, Steinthorsdottir V, et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44:981–90.
Verdoia M, Schaffer A, Barbieri L, Cassetti E, Nardin M, Bellomo G, et al. Diabetes, glucose control and mean platelet volume: a single-centre cohort study. Diabetes Res Clin Pract. 2014;104:288–94.
Kim ES, Mo EY, Moon SD, Han JH. Mean platelet volume is closely associated with serum glucose level but not with arterial stiffness and carotid atherosclerosis in patients with type 2 diabetes. J Clin Endocrinol Metab. 2015;100:3502–8.
Hudzik B, Szkodzinski J, Lekston A, Gierlotka M, Poloński L, Gąsior M. Mean platelet volume-to-lymphocyte ratio: a novel marker of poor short- and long-term prognosis in patients with diabetes mellitus and acute myocardial infarction. J Diabetes Complicat. 2016;30:1097–102.
Wang F, Zhu J, Yao P, Li X, He M, Liu Y, et al. Cohort profile: the Dongfeng–Tongji cohort study of retired workers. Int J Epidemiol. 2013;42:731–40.
AD Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–61.
Bath P, Algert C, Chapman N, Neal B, PROGRESS Collaborative Group. Association of mean platelet volume with risk of stroke among 3134 individuals with history of cerebrovascular disease. Stroke. 2004;35:622–6.
Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, Konkle B. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:148–56.
Klovaite J, Benn M, Yazdanyar S, Nordestgaard BG. High platelet volume and increased risk of myocardial infarction: 39,531 participants from the general population. J Thromb Haemost. 2011;9:49–56.
Alessandrini P, McRae J, Feman S, FitzGerald GA. Thromboxane biosynthesis and platelet function in type I diabetes mellitus. N Engl J Med. 1988;319:208–12.
Davi G, Catalano I, Averna M, Notarbartolo A, Strano A, Ciabattoni G, et al. Thromboxane biosynthesis and platelet function in type II diabetes mellitus. N Engl J Med. 1990;322:1769–74.
Demirtunc R, Duman D, Basar M, Bilgi M, Teomete M, Garip T. The relationship between glycemic control and platelet activity in type 2 diabetes mellitus. J Diabetes Complicat. 2009;23:89–94.
Kodiatte TA, Manikyam UK, Rao SB, Jagadish TM, Reddy M, Lingaiah HK, et al. Mean platelet volume in Type 2 diabetes mellitus. J Lab Phys. 2012;4:5–9.
Andre P, Nannizzi-Alaimo L, Prasad SK, Phillips DR. Platelet-derived CD40L: the switch-hitting player of cardiovascular disease. Circulation. 2002;106:896–9.
Rizvi M, Pathak D, Freedman JE, Chakrabarti S. CD40-CD40 ligand interactions in oxidative stress, inflammation and vascular disease. Trends Mol Med. 2008;14:530–8.
Brown AS, Hong Y, de Belder A, Beacon H, Beeso J, Sherwood R, et al. Megakaryocyte ploidy and platelet changes in human diabetes and atherosclerosis. Arterioscler Thromb Vasc Biol. 1997;17:802–7.
Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;15:2792–800.
Johnson M, Ramey E, Ramwell PW. Sex and age differences in human platelet aggregation. Nature. 1975;253:355–7.
Panova-Noeva M, Schulz A, Hermanns MI, Grossmann V, Pefani E, Spronk HM, et al. Sex-specific differences in genetic and non genetic determinants of mean platelet volume: results from the Gutenberg Health Study. Blood. 2016;127:251–9.
Ranganath LR, Christofides J, Semple MJ. Increased mean platelet volume after oestrogen replacement therapy. Ann Clin Biochem. 1996;33:555–60.
Yarlioglues M, Ardic I, Dogdu O, Akpek M, Zencir C, Kasapkara HA, et al. The acute effects of passive smoking on mean platelet volume in healthy volunteers. Angiology. 2012;63:353–7.
Alyan O, Kacmaz F, Ozdemir O, Karahan Z, Taşkesen T, Iyem H, et al. High levels of high-sensitivity C-reactive protein and impaired autonomic activity in smokers. Turk Kardiyol Dern Ars. 2008;36:368–75.
Andersson A, Malmhall C, Houltz B, Tengvall S, Sjöstrand M, Qvarfordt I, et al. Interleukin-16-producing NK cells and T-cells in the blood of tobacco smokers with and without COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:2245–58.
Diaz-Ricart M, Brunso L, Pino M, Navalon F, Jou JM, Heras M, et al. Preanalytical treatment of EDTA-anticoagulated blood to ensure stabilization of the mean platelet volume and component measured with the ADVIA counters. Thromb Res. 2010;126:e30–5.
Akyüz A, Akkoyun DÇ, Değirmenci H, Alp R. Atrial fibrillation is associated with increased mean platelet volume and apnea hypopnea index in patients with obstructive sleep apnea. Angiology. 2015;66(6):525–30.
Kanbay A, Tutar N, Kaya E, Buyukoglan H, Ozdogan N, Oymak FS, et al. Mean platelet volume in patients with obstructive sleep apnea syndrome and its relationship with cardiovascular diseases. Blood Coagul Fibrinolysis. 2013;24(5):532–6.
Crawford VL, McNerlan SE, Stout RW. Seasonal changes in platelets, fibrinogen and factor VII in elderly people. Age Ageing. 2003;32(6):661–5.
Authors’ contributions
MAH designed the research, interpreted data, and co-wrote the paper; ZYL analyzed data and co-wrote the paper; JW and XH performed data collection; JY, HG, XMZ, DZ, HDY, and YHT provided critical revisions to the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We gratefully thank all study participants for participating in the present DFTJ-cohort study as well as all volunteers for assisting in collecting the samples and data.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Ethics and Human Subject committee of Tongji Medical College, Dongfeng General Hospital, and DMC. All study participants provided informed consents.
Funding
This work was supported by the grants from the National Natural Science Foundation (Grants NSFC-81473051 and 81522040) and the Program for HUST Academic Frontier Youth Team.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Table S1.
Baseline characteristics of the study population in women and men.
Additional file 2: Table S2.
Multivariate adjusted hazard ratios with 95% CI for incident T2DM in women and men.
Additional file 3: Table S3.
Hazard ratios of T2DM incidence for MPV stratified by characteristics relevant to MPV.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, Z., Wang, J., Han, X. et al. Association of mean platelet volume with incident type 2 diabetes mellitus risk: the Dongfeng–Tongji cohort study. Diabetol Metab Syndr 10, 29 (2018). https://doi.org/10.1186/s13098-018-0333-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-018-0333-6