Abstract
Background
Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians due to its portability, excellent safety profile, and diagnostic utility. Despite its growing use, the potential risks of POCUS use should be considered by providers. We analyzed the Canadian Medical Protective Association (CMPA) repository to identify medico-legal cases arising from the use of POCUS.
Methods
We retrospectively searched the CMPA closed-case repository for cases involving diagnostic POCUS between January 1st, 2012 and December 31st, 2021. Cases included civil-legal actions, medical regulatory authority (College) cases, and hospital complaints. Patient and physician demographics, outcomes, reason for complaint, and expert-identified contributing factors were analyzed.
Results
From 2012 to 2021, there were 58,626 closed medico-legal cases in the CMPA repository with POCUS determined to be a contributing factor for medico-legal action in 15 cases; in all cases the medico-legal outcome was decided against the physicians. The most common reasons for patient complaints were diagnostic error, deficient assessment, and failure to perform a test or intervention. Expert analysis of these cases determined the most common contributing factors for medico-legal action was failure to perform POCUS when indicated (7 cases, 47%); however, medico-legal action also resulted from diagnostic error, incorrect sonographic approach, deficient assessment, inadequate skill, inadequate documentation, or inadequate reporting.
Conclusions
Although the most common reason associated with the medico-legal action in these cases is failure to perform POCUS when indicated, inappropriate use of POCUS may lead to medico-legal action. Due to limitations in granularity of data, the exact number of civil-legal, College cases, and hospital complaints for each contributing factor is unavailable. To enhance patient care and mitigate risk for providers, POCUS should be carefully integrated with other clinical information, performed by providers with adequate skill, and carefully documented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians [1]. Its portability, excellent safety profile, and ability to make important diagnoses in real-time helps expedite care. The importance of POCUS has been recognized by many undergraduate and post-graduate medical institutions, and it has seen planned or actual integration into core medical curricula [2,3,4,5]. Additionally, its safety and ability to enhance patient care has led to its endorsement by multiple major clinical societies [6,7,8,9,10]. Despite being an invaluable tool, there is a risk that the rapid uptake of POCUS may outpace development of best practices to safeguard both patients and providers.
Medico-legal analyses can help promote patient safety and improve the quality of healthcare delivery. By analyzing medico-legal cases, we can identify patterns of error, understand the root causes of adverse events, and develop strategies to prevent future occurrences [11].
The current POCUS medico-legal literature has not identified any cases where performing diagnostic POCUS has resulted in civil-legal action [12,13,14,15,16,17]. Instead, all cases have arisen from failure to perform POCUS when clinically indicated [12,13,14,15,16,17]. These small studies are limited by sample size, non-comprehensive legal databases, and differences in legal systems between countries, leaving important questions about the medico-legal risk for physicians performing POCUS for Canadian physicians.
The objective of our study was to analyze the Canadian Medical Protective Association (CMPA) closed-case repository to identify medico-legal cases (civil-legal, college complaints, or hospital complaints) related to the use of POCUS. We describe the nature and frequency of medico-legal claims, identify common errors and contributing factors, and discuss strategies for mitigating medico-legal risks when performing POCUS.
Methods
In January 2023, the Canadian Medical Protective Association (CMPA), a not-for-profit mutual defense organization, represented over 107,000 physician members. The CMPA offers medico-legal support, advice, and education to physicians, and engages in safe medical care research using medico-legal data from its repository. The repository relies on physician members to voluntarily contact the CMPA and submit materials when seeking advice or support for medico-legal matters. We conducted a 10-year retrospective descriptive analysis of medico-legal cases related to diagnostic POCUS performed in a hospital setting. In this study, cases included civil-legal actions (class action legal cases were excluded), medical regulatory authority cases (College) and hospital complaints. A statistical data analyst searched all cases closed between January 1st, 2012 and December 31st, 2021. Prior to analysis, all cases were de-identified and reported at the aggregate level to ensure confidentiality for both patients and healthcare providers. This means that detailed descriptions of individual cases are not possible and may leave an unavoidable lack of granularity. The Advarra Institutional Review Board provided ethical approval for this study.
CMPA medical analysts, who are experienced registered nurses with training in medico-legal research, used standardized methods to code information retrieved from medico-legal cases, including the case information, patient characteristics, health conditions, complications, peer expert criticisms classified using the CMPA’s contributing factors framework [11], patient harm classified using an in-house classification of harms, and the court ruling or final regulatory authority or hospital decisions. Peer experts are physicians retained by the parties in a legal action to interpret and provide their opinion on clinical, scientific, or technical issues surrounding the care provided. Clinical coding was applied using the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada (ICD-10-CA), the Canadian Classification of Health Interventions, and in-house CMPA coding. To reduce misclassification, nurse-analysts conducted regular quality assurance reviews of coding electronically and as a group.
Closed cases with sufficient information involved various physician specialties caring for patients undergoing diagnostic POCUS. Some cases involved more than one physician and more than one physician specialty per case.
Cases were extracted using word search for point of care ultrasound (see Appendix A for list of terms). We excluded cases involving radiologists, obstetricians performing obstetric ultrasounds, and cardiologists performing echocardiography from the extraction and a manual review excluded cases when POCUS was not the medico-legal issue in the case. A descriptive analysis of the selected cases included an analysis of the contributing factors identified by peer experts as well as analysis of the indications for POCUS, patient harm, care settings, geographical location of care, patient demographics, physician specialty and years in practice.
We report all variables with frequencies and proportions using SAS software, version 9.4 for all statistical analyses (SAS® Enterprise Guide® software, Version 9.4. Cary, North Carolina: SAS Institute Inc.; 2013).
Results
Search
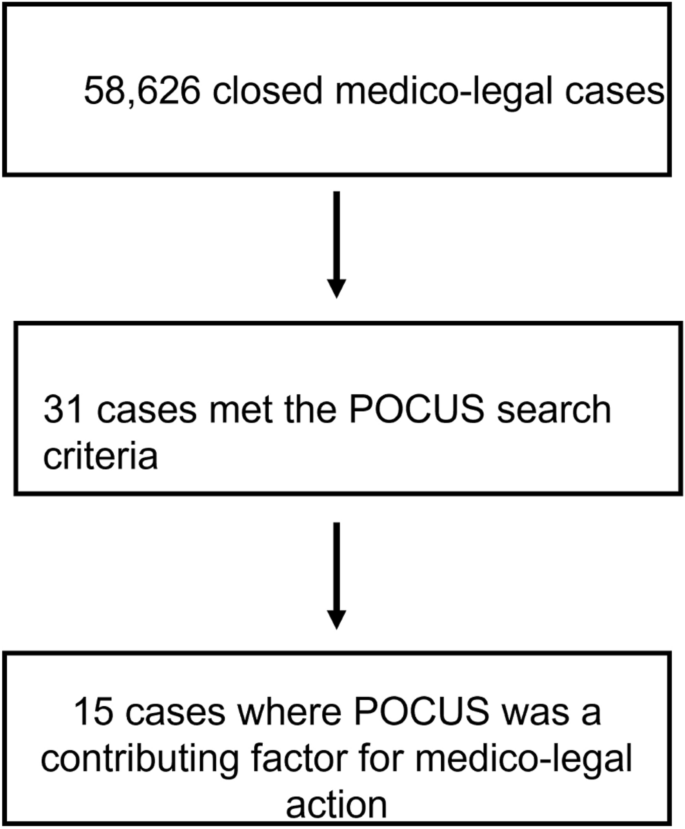
From 2012 to 2021, a total of 58,626 medico-legal cases were captured in the CMPA database. Of these, 31 cases met the database search strategy. POCUS was a contributing factor towards medico-legal action in 15/31 (48%) cases. Nine cases were college complaints, the rest were civil-legal actions (five) or hospital complaints. The medico-legal outcomes for physicians were decided against the physician in all 15 cases.
Patient demographics and outcomes
Ten of the 15 patients were female (67%). The age ranges for patients were: 0–18 years old (2, 13%), 19–29 (3, 20%), 30–49 (7, 47%), 50–64 (2, 13%), and 65–79 (1, 7%). Most cases occurred in the emergency department (13, 87%). Thirteen of the 15 cases (87%) resulted from healthcare related harm to the patient, with 2 cases (13.3%) resulting from non-clinical issues (e.g. documentation). Of the 13 patients with healthcare related harm, 5 patients died (33%). For the remaining patients, the harm classification was mild for 4 patients (26.7%), moderate for 2 patients (13%) severe for 1 patient (7%), and 1 patient experienced no harm (7%). See Appendix 2 for the definitions of patient harm.
The most common patient safety indicators were diagnostic error (12/15, 80%), contraindicated procedure or pharmacotherapy (2/15, 13%), and injury associated with healthcare (1/15, 7%). The most common reasons for patient complaints included diagnostic error (14, 93%), deficient assessment (12, 80%), and failure to perform a test or intervention (8, 53%) (Table 1).
Physician demographics
The distribution of specialties for physicians involved in the cases (n = 19) were: emergency medicine (9, 47%), resident physician (3,16%), family medicine (3, 16%), obstetrics and gynecology (1, 5%), internal medicine (1, 5%), general surgery (1, 5%), and diagnostic radiology (1, 5%). Note, cases where the POCUS provider was an obstetrician or radiologist were excluded from our search, however, these specialists may have been included in cases if they were listed as co-complainants. Eleven of 19 physicians (58%) were in practice 5 years of less; five of 19 physicians (26%) were in practice 11–20 years; three of 19 physicians (16%) were in practice 21–30 years. Nine cases (60%) occurred in large urban population centers (> 100,000 people), with 3 cases (20%) occurring in medium population centers (30,000 to 100,000 people), and 3 (20%) cases occurring in small population centers (less than 30,000 people).
Expert contributing factor analysis
Expert analysis identified the root cause of medico-legal action for each case. They found that in 7 cases POCUS was not performed when clinically indicated. In 8 cases, POCUS was performed but there was an issue with its application: in 2 cases, inadequate skill; in 1 case, an incorrect approach used (e.g. a surface POCUS instead of an invasive modality); in 1 case, deficient reporting; in 1 case, deficient documentation;, in 1 case, inappropriate use; in 1 case, misdiagnosis; in 1 case, the expert analysis was not recorded. The lack of granularity of the data limits the ability to report how many of the above cases were civil-legal cases, college complaints, or hospital complaints.
For cases involving a diagnostic error (12 cases), 6 (50%) were related to performing POCUS, and 6 (50%) were related to not performing POCUS. For cases of deficient assessment, in one case, the physician relied on serial POCUS exams, disregarding an important physical exam finding that should have prompted additional imaging. In 4 cases (36%) a misinterpretation of the POCUS led to the failure to perform an indicated test or intervention. Notably, whereas only 1 case had inadequate documentation listed as the cause of complaint from the patient or family members, peer expert criticism identified 11 cases where inadequate documentation contributed to the medico-legal outcome. One important note is that not all documentation issues were specific to POCUS; however, failure to document POCUS findings, and failure to use standardized wording for POCUS reports were identified as contributing factors by peer review.
The contributing factor analysis of 14 cases with criticisms related to patient care (not the 1 case related to documentation), identified provider factors in 13/14 case (93%), team factors in 13/14 cases (93%), and system factors in 3/14 cases (21%). The complete list of provider, team, and system factors identified are included in Table 2; however, the most common contributing factors included failure to perform a test or intervention, deficient assessment, and misinterpretation of a test. At the team level, these were documentation issues and communication breakdown with a patient. At a system level these were related to resource issues, and protocol, policy, or procedural issues. Of note, the system level issues that arose from lack of resources were not related to lack of POCUS machine access or lack of access to POCUS infrastructure (e.g. image archiving), but rather inadequate staffing of departments in a way that contributed to patient harm.
Interpretation
In this analysis of closed medico-legal cases in the CMPA repository we identified 15 cases where POCUS was a contributing factor towards medico-legal action. Almost half of the cases were due to physicians failing to perform POCUS when indicated. In contrast to previous literature that had not identified POCUS cases that resulted in a medico-legal action [12,13,14,15,16,17], we found a number of cases where POCUS use resulted in a medico-legal action due to issues with provider skill, sonographic approach, reporting, documentation, misdiagnosis, and inappropriate use. All cases resulted in findings against the physician involved. Five cases involved patient death.
Contrasting our study to existing literature [12,13,14,15,16,17] (which report civil-legal cases only), the increased number of medico-legal cases identified may be accountable by several factors. First, the CMPA repository is a comprehensive database capturing essentially all medico-legal cases against Canadian physicians, with data coded prospectively in a highly searchable way. Additionally, most of the cases were hospital or college complaints, which have a lower barrier to filing compared with civil litigation. This is important as this is the first study to examine hospital and college complaints, in addition to civil litigation. Thus, whereas patients and families may have felt POCUS was applied inappropriately and submitted a hospital or college complaint, it may not have met a threshold to proceed with civil litigation (Fig. 1).
Regardless, our study demonstrates an important reality for the twenty-first century acute care physician: failure to perform POCUS when indicated may result in medico-legal action. For some specialties and indications, POCUS may no longer be an adjunct to augment traditional bedside assessment but rather a core part of the diagnostic process itself. While POCUS infrastructure and expertise varies between different settings, as the evidence and use of POCUS grows, so too can the expectation that it is appropriately used when clinically indicated. This may be particularly relevant for specific use cases of POCUS with well-established diagnostic pathways including the Focused Assessment with Sonography in Trauma (FAST) exam during trauma resuscitation, or its use to diagnosis undifferentiated shock [18,19,20]. The excellent safety and diagnostic prowess of acute care POCUS has led to its endorsement by various societal guidelines [6,7,8,9,10].
Despite increasing adoption of POCUS in acute care medicine, adequate training and skill is necessary for its safe implementation, and in this analysis was flagged as a contributing factor for medico-legal action in several cases. One systems level approach to POCUS education being implemented at multiple institutions is to teach ultrasound physics, knobology, and anatomy in parallel with traditional medical school curriculum to provide learners with a base skillset that can be built on during further training [3,4,5]. Then, specialty specific POCUS training with a focus on interpretation and synthesis can be taught during residency. Although this approach will help ensure future generations of physicians have base competency in POCUS, for clinicians in practice, alternative educational approaches should be considered. These include informal or formal instruction from colleagues with POCUS expertise to help develop core skills. Alternatively, continuing medical education opportunities like POCUS courses, conferences, rotations, or fellowships are an excellent resource, however, may not be feasible for many physicians in practice. Some societies have suggested processes for credentialing and privileging practicing physicians, which may be helpful roadmaps for interested clinicians [6].
In addition to helping clinicians obtain and interpret POCUS images, formalized training helps clinicians appropriately integrate POCUS findings with other clinical information. In fact, diagnostic errors, deficient assessments, and failure to perform other indicated tests or interventions were the most common reasons for patient complaints in our study, indicating a failure to properly integrate POCUS into the diagnostic workup of patients. Ideally, POCUS findings should be integrated into patient care with a ‘Bayesian mindset’, meaning that the positive or negative finding on POCUS helps change the post-test probability of a pathology being present. This contrasts with an oversimplified view of POCUS where the presence or absence of findings on POCUS dictates whether a disease is present. This dichotomized view of POCUS is potentially dangerous, and in our experience seen more with novice POCUS practitioners. The visual nature of the medium may lend itself to a ‘seeing is believing’ phenomenon, which can lead some clinicians to place inappropriate weight on the POCUS findings, disregarding other competing clinical information.
Inappropriate integration of POCUS into practice may also result from a failure to understand the test characteristics for POCUS in that population. For instance, FAST scan has high specificity (> 98%) to detect intraperitoneal free fluid, however only moderate sensitivity (70–90%) with test characteristics varying between operators [18, 21, 22]. For a trauma patient with a very high pre-test probability for intrabdominal hemorrhage (e.g. 80%), even with a negative FAST scan (assume sensitivity of 70%), the post-test chance of intrabdominal hemorrhage is 55%. Overreliance on POCUS and failure to integrate other clinical information is a crucial pitfall to avoid.
Inadequate documentation led to medico-legal action and was a major theme in the contributing factor analysis. If a POCUS is performed, the indication, views acquired, findings, and interpretation should be recorded in the patient's chart. At a minimum, this should be written as a progress note or included as part of a consultation. A better practice, although not available at many centers, is to save images in an accessible archiving system, and then generate a written report to allow for accountability and communication between providers [23, 24]. Ideal practice would have all archived scans undergo quality assurance by a POCUS expert, with the amended reports subsequently uploaded into a patient’s electronic medical record. The practice of "shadow" scans where results are communicated by verbal handover between providers is not acceptable and may expose physicians to medico-legal risk.
Future directions
Although this represents a preliminary analysis of Canadian medico-legal cases involving POCUS, we expect the number of medico-legal cases to grow in parallel with increased POCUS use across. A repeat analysis of this work in 5 or 10 years will be helpful to assess for evolving patterns in POCUS medico-legal risk. Furthermore, this study excluded procedural use of POCUS (e.g. central line insertion) which would be an important area for future research. Additionally, knowledge translation surrounding best practices in POCUS training, clinical integration, and documentation is needed to promote optimal POCUS use among physicians.
Limitations
There are several important limitations: the search terms used may not have retrieved all medico-legal cases related to POCUS. To address this, the CMPA will now prospectively identify POCUS cases to facilitate future research. We omitted granular clinical details from the cases to protect patient and physician privacy, however this limits the analysis of factors leading to poor patient outcomes. This was unavoidable and was done in close collaboration with the CMPA to adhere to their rigorous privacy mandates. We recognize that this leaves unanswered questions, but feel this study still provides actionable take homes to improve patient safety. Finally, we have not included procedural POCUS, as we would lack granularity to distinguish between medico-legal action from the procedure itself, or the POCUS use.
Conclusions
Although failing to perform POCUS when clinically indicated remains an important contributing factor for medico-legal action, in contrast to the existing published literature, we identified cases where the application of POCUS resulted in adverse medico-legal outcomes. Due to limitations in granularity of data, the exact number of civil-legal, College cases, and hospital complaints for each contributing factor is unavailable. Overall, these cases resulted from inadequate skill, misdiagnosis, incorrect approach, deficient patient assessment, and incomplete documentation. The thoughtful and deliberate integration of POCUS into diagnostic pathways will help mitigate risk while allowing patients to experience benefits of this powerful tool.
Availability of data and materials
Data is available on reasonable request to the corresponding author.
Abbreviations
- CMPA:
-
Canadian Medical Protective Association
- FAST:
-
Focused assessment with sonography in trauma
- POCUS:
-
Point-of-care Ultrasound
References
Arntfield RT, Millington SJ (2012) Point of care cardiac ultrasound applications in the emergency department and intensive care unit–a review. Curr Cardiol Rev 8(2):98–108
Micks T, Braganza D, Peng S, McCarthy P, Sue K, Doran P et al (2018) Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician 64(10):e462–e467
Steinmetz P, Dobrescu O, Oleskevich S, Lewis J (2016) Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J 7(1):e78-86
Ma IWY, Steinmetz P, Weerdenburg K, Woo MY, Olszynski P, Heslop CL et al (2020) The Canadian medical student ultrasound curriculum: a statement from the Canadian ultrasound consensus for undergraduate medical education group. J Ultrasound Med 39(7):1279–1287
Weill S, Picard DA, Kim DJ, Woo MY (2023) Recommendations for POCUS curriculum in Canadian undergraduate medical education: consensus from the inaugural Seguin Canadian POCUS Education Conference. POCUS J 8(1):13–18
Lewis D, Rang L, Kim D, Robichaud L, Kwan C, Pham C et al (2019) Recommendations for the use of point-of-care ultrasound (POCUS) by emergency physicians in Canada. CJEM 21(6):721–726
Bronshteyn YS, Anderson TA, Badakhsh O, Boublik J, Brady MBW, Charnin JE et al (2022) Diagnostic point-of-care ultrasound: recommendations from an expert panel. J Cardiothorac Vasc Anesth 36(1):22–29
Ma IWY, Arishenkoff S, Wiseman J, Desy J, Ailon J, Martin L et al (2017) Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) group. J Gen Intern Med 32(9):1052–1057
Arntfield R, Millington S, Ainsworth C, Arora R, Boyd J, Finlayson G et al (2014) Canadian recommendations for critical care ultrasound training and competency. Can Respir J 21(6):341–345
Meineri M, Arellano R, Bryson G, Arzola C, Chen R, Collins P et al (2021) Canadian recommendations for training and performance in basic perioperative point-of-care ultrasound: recommendations from a consensus of Canadian anesthesiology academic centres. Can J Anaesth 68(3):376–386
McCleery A, Devenny K, Ogilby C, Dunn C, Steen A, Whyte E et al (2019) Using medicolegal data to support safe medical care: a contributing factor coding framework. J Healthc Risk Manag 38(4):11–18
Reaume M, Farishta M, Costello JA, Gibb T, Melgar TA (2021) Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. Postgrad Med J 97(1143):55–58
Solomon L, Emma M, Gibbons LM, Kusulas MP (2022) Current risk landscape of point-of-care ultrasound in pediatric emergency medicine in medical malpractice litigation. Am J Emerg Med 58:16–21
Stolz L, O’Brien KM, Miller ML, Winters-Brown ND, Blaivas M, Adhikari S (2015) A review of lawsuits related to point-of-care emergency ultrasound applications. West J Emerg Med 16(1):1–4
Russ B, Arthur J, Lewis Z, Snead G (2022) A review of lawsuits related to point-of-care emergency ultrasound applications. J Emerg Med 63(5):661–672
Blaivas M, Pawl R (2012) Analysis of lawsuits filed against emergency physicians for point-of-care emergency ultrasound examination performance and interpretation over a 20-year period. Am J Emerg Med 30(2):338–341
Nguyen J, Cascione M, Noori S (2016) Analysis of lawsuits related to point-of-care ultrasonography in neonatology and pediatric subspecialties. J Perinatol 36(9):784–786
Netherton S, Milenkovic V, Taylor M, Davis PJ (2019) Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis. CJEM 21(6):727–738
Vieillard-Baron A, Millington SJ, Sanfilippo F, Chew M, Diaz-Gomez J, McLean A et al (2019) A decade of progress in critical care echocardiography: a narrative review. Intensive Care Med 45(6):770–788
Stickles SP, Carpenter CR, Gekle R, Kraus CK, Scoville C, Theodoro D et al (2019) The diagnostic accuracy of a point-of-care ultrasound protocol for shock etiology: a systematic review and meta-analysis. CJEM 21(3):406–417
Lee C, Balk D, Schafer J, Welwarth J, Hardin J, Yarza S et al (2019) Accuracy of focused assessment with sonography for trauma (FAST) in disaster settings: a meta-analysis and systematic review. Disaster Med Public Health Prep 13(5–6):1059–1064
Stengel D, Leisterer J, Ferrada P, Ekkernkamp A, Mutze S, Hoenning A (2018) Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev 12(12):CD012669
Aspler A, Wu A, Chiu S, Mohindra R, Hannam P (2022) Towards quality assurance: implementation of a POCUS image archiving system in a high-volume community emergency department. CJEM 24(2):219–223
Lewis D, Alrashed R, Atkinson P (2022) Point-of-care ultrasound image archiving and quality improvement: not “If?” or “When?”…but “How?” and “What Next…?” CJEM 24(2):113–114
Acknowledgements
We would like to thank Anna MacIntyre for her contributions to the retrieval of cases from the CMPA database.
Funding
No funding was obtained for this research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design, analysis, interpretation, manuscript writing, and revisions of this study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Advarra Institutional Review Board provided ethical approval for this study.
Consent for publication
No patient information is provided in the manuscript.
Competing interests
None of the authors have relevant competing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
CMPA repository search strategy.
Word search terms:
-
FAST
-
Bedside
-
Bedside ultrasound
-
Bedside u/s
-
Point of care
-
Point of care ultrasound
-
Point of care u/s
-
POC U/S
-
POC ultrasound
Appendix 2
Patient harm classification definitions.
The harm classification distinguishes healthcare-associated harm from other medical-legal matters through a reliable method. The system categorizes harm arising from healthcare delivery either from an inherent risk of investigation or treatment, or from three types of patient safety incidents: harmful incident, no harm incident (i.e. incident occurred but did not lead to harm), or a near miss.
Harm classification | Definitions |
|---|---|
Healthcare-associated harm | Harm arising from, or associated with, plan or actions taken during the provision of healthcare, rather than an underlying disease or injury |
Inherent risk | Most investigations have inherent risks. Certain complications, adverse reactions, or side-effects may occur and may be independent of who is providing the care |
Harmful incident | A patient safety incident that resulted in harm to the patient |
No harm incident | A patient safety incident that reached a patient but no discernible harm resulted |
Near miss | A patient safety incident that did not reach the patient and therefore no harm resulted |
Patient safety incident | An event of circumstance which could have resulted, or did result in unnecessary harm to a patient |
Harm classification table.
Safety event class | Level of harm | Harm category | Patient description |
|---|---|---|---|
HI—Harmful incident (reaches the patient) | |||
Harm results from the care or services provided to the patient due to failures in the processes of care or in the performance of procedures, including provider error Based on expert opinion | DE—Death | HI–DE | Unexpected death not related to the natural or expected course of the patient’s illness or underlying condition. On balance of probabilities, caused by or brought forward by the incident |
SE—Severe | HI–SE | Patient harm is symptomatic: • requiring life-saving intervention or major medical/surgical intervention, • shortening life expectancy, or • causing major temporary or permanent impact on physical, mental or social function • patient experienced enduring psychological difficulty that required specialist treatment (e.g. prolonged counselling and psychotropic medication management) Includes previous catastrophic disability | |
MO—Moderate | HI–MO | Patient harm is symptomatic: • requiring intervention (e.g. additional operative procedure, additional therapeutic treatment), and increased length of stay, or • causing temporary or permanent impact on physical, mental, or social function • patient experienced psychological difficulty requiring treatment (e.g. counselling with FP, therapist, or psychologist) | |
MI—Mild | HI–MI | Patient harm is symptomatic: • symptoms are mild • minimal or no intervention is required (e.g. extra observation, investigation, review, or minor treatment) • causing minimal (permanent or temporary) impact on physical, mental, or social function • patient experienced emotional distress that had an impact on lifestyle (e.g. mild sleep disturbances, occasional work absences) | |
NO—None† | HI–NO | Patient harm is asymptomatic. No symptoms detected and no treatment required | |
ID—Insufficient detail | HI–ID | • Insufficient information is available to evaluate the level of harm • There may be no description of any clinical outcome • There may be a patient safety incident but insufficient information to classify level of harm of the outcome | |
IR—Inherent risk (reaches the patient) | |||
A known risk associated with a particular investigation, medication, or treatment. It is the risk from undergoing a procedure in ideal conditions, performed by qualified staff using current standards, equipment and techniques* Includes non-preventable missed or delayed diagnosis Based on expert opinion | DE—Death | IR–DE | Unexpected death not related to the natural or expected course of the patient’s illness or underlying condition. Caused by or brought forward as a result of the inherent risk of the care |
SE—Severe | IR–SE | Patient harm is symptomatic: • requiring life-saving intervention or major medical/surgical intervention, • shortening life expectancy, or • causing major temporary or permanent impact on physical, mental or social function • patient experienced enduring psychological difficulty that required specialist treatment (e.g. prolonged counselling and psychotropic medication management) Includes previous catastrophic disability | |
MO—Moderate | IR–MO | Patient harm is symptomatic: • requiring intervention (e.g. additional operative procedure, additional therapeutic treatment), and increased length of stay, or • causing temporary or permanent impact on physical, mental, or social function • patient experienced psychological difficulty, requiring treatment (e.g. counselling with FP, therapist, or psychologist) | |
MI—Mild | IR–MI | Patient harm is symptomatic: • symptoms are mild • minimal or no intervention is required (e.g. extra observation, investigation, review, or minor treatment) • causing minimal (permanent or temporary) impact on physical, mental, or social function • patien t experienced emotional distress that had an impact on lifestyle (e.g. mild sleep disturbances, occasional work absences) | |
NO—None† | IR–NO | Patient harm is asymptomatic. No symptoms detected and no treatment required. Includes persistence of condition (e.g. myopia, carpal tunnel) | |
ID—Insufficient detail | IR–ID | • Insufficient information is available to evaluate the level of harm • There may be no description of any clinical outcome • There may be a patient safety incident but insufficient information to classify level of harm of the outcome | |
UN—Unknown (reaches the patient) | |||
Harm results from the care or services provided to the patient, but no expert opinion on file to categorize as harm arising from a harmful incident or inherent risk Usually involves cases with a contributing factor of UNKNOWN | Level of patient harm is not populated due to limited information on the file | ||
NM—Near miss | |||
A patient safety incident that did not reach the patient and therefore no harm results | No—None | NM–NO | Error or capacity to cause harm was caught by an error detection barrier, or by chance, before reaching the patient |
No healthcare-associated harm occurred | Level of harm | Harm category | Patient description |
NA-not applicable | NA | Involves all other medical-legal matters that are solely administrative (e.g. documentation) or related conduct (e.g. manner) | |
Based on ASHRM’s Healthcare Associated Preventable Harm Level Classification and Classification of patient safety incidents in primary care.
† Relates to a No harm incident: a patient safety incident that reached a patient but resulted in no discernable harm.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prager, R., Wu, D., Garber, G. et al. Medico-legal risks of point-of-care ultrasound: a closed-case analysis of Canadian Medical Protective Association medico-legal cases. Ultrasound J 16, 16 (2024). https://doi.org/10.1186/s13089-024-00364-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13089-024-00364-7