Abstract
Background
Capacity to work is impacted by psoriatic arthritis (PsA). Our objective was to describe the course of work productivity and leisure activity in patients with PsA treated with biologic (b) and targeted synthetic (ts) disease-modifying antirheumatic drugs (DMARDs).
Methods
A systematic literature review identified all trials and observational studies published January 1, 2010–October 22, 2021, reporting work productivity using the Work Productivity and Activity Impairment Questionnaire (WPAI) in patients with PsA treated with b/tsDMARDs. Outcomes for WPAI domains (absenteeism, presenteeism, total work productivity, and activity impairment) were collected at baseline and time point closest to 24 weeks of treatment. A random effects meta-analysis of single means was conducted to calculate an overall absolute mean change from baseline for each WPAI domain.
Results
Twelve studies (ten randomized controlled and two observational) assessing patients treated with adalimumab, bimekizumab, guselkumab, ixekizumab, risankizumab, secukinumab, or upadacitinib were analysed. Among 3741 employed patients, overall mean baseline scores were 11.4%, 38.7%, 42.7%, and 48.9% for absenteeism, presenteeism, total work productivity impairment, and activity impairment, respectively. Estimated absolute mean improvements (95% confidence interval) to week 24 were 2.4 percentage points (%p) (0.6, 4.1), 17.8%p (16.2,19.3), 17.6%p (15.9,19.4), and 19.3%p (17.6, 21.0) respectively, leading to a mean relative improvement of 41% for total work productivity. The change in work outcomes in the b/tsDMARDs appeared similar.
Conclusions
This systematic literature review and meta-analysis confirmed that patients with active PsA have a substantially reduced capacity to work and participate in leisure activities. Substantial improvements across various WPAI domains were noted after 24 weeks of b/tsDMARD treatment, especially in presenteeism, total work productivity, and activity impairment. These findings may be useful for reimbursement purposes and in the context of shared decision-making.
Key summary points
This systematic literature review (SLR) of randomized clinical trials and observational studies of biologic (b) and targeted synthetic (ts) disease-modifying antirheumatic drugs b/tsDMARDs in patients with PsA found that at treatment introduction, patients presented with a 42.7% mean productivity loss per week as assessed by the Work Productivity and Activity Impairment (WPAI) Questionnaire.
Through a meta-analysis comparing before/after values without adjustment for placebo response, we found that after 24 weeks of treatment with b/tsDMARDs, there was a mean absolute improvement of 17.6 percentage points and a mean relative improvement of 41% in total work productivity, with similar magnitudes of improvement in time spent at work and regular activities outside of work.
These results provide clinical-, regulatory- and reimbursement decision-makers with data on the potential societal and socio-economic benefits of b/tsDMARDs in PsA.
Plain language summary
Psoriatic arthritis (PsA) has a major impact on patients’ lives, including their ability to work by causing absence and reducing productivity. By pooling together published studies (12 studies, corresponding to 3741 patients) and comparing what patients reported before starting treatment to during treatment, we found that over the course of treatment with biologic (b) and targeted synthetic (ts) disease-modifying antirheumatic drugs (DMARDs), patients with PsA had an average of 18% higher total work productivity, translating to a 41% reduced impact of PsA at the group level (without looking at comparisons to a placebo response). It is important for health professionals and patients to know that work outcomes affected by PsA are improved when patients take b/tsDMARDS.
Similar content being viewed by others
Introduction
Psoriatic arthritis (PsA) has a substantial impact on health-related quality of life (HRQoL) [1]. As the clinical presentation of PsA varies, its impact often extends beyond joint damage to include comorbidities such as obesity, depression, anxiety, and cardiovascular disease [2, 3]. In particular, patients with PsA have reported its effect on individual activities and social participation, as well as physiological functioning as linked to the World Health Organization (WHO) International Classification of Functioning, Disability, and Health (ICF) [4, 5]. The consequences of PsA on work are important and include deleterious effects such as hours of missed work (absenteeism), diminished productivity while at work (presenteeism), and increased economic burden due to indirect costs [4, 6,7,8,9,10].
The availability of biologic (b) and targeted synthetic (ts) disease-modifying antirheumatic drugs (DMARDs) over the last 20 years has improved clinical outcomes in PsA [11]. However, work and work productivity following b/tsDMARD treatment initiation in PsA based on evidence from both randomized controlled trials and observational studies has not been comprehensively assessed.
The objective of this systematic literature review (SLR) and meta-analysis was to describe work and work productivity in patients with PsA prior to and following b/tsDMARD treatment, and to explore the potential economic impact of changes in productivity.
Methods
This SLR was conducted according to the methodological guidance of the Centre for Reviews and Dissemination and reporting requirements of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [12, 13].
Search strategy and selection criteria
The search aimed to capture all trials of b/tsDMARDs in PsA reporting patient-reported outcomes. The eligibility criteria were defined according to Population, Intervention, Comparator, Outcome, and Study Design (PICOS) criteria as reported in Table S1. While the SLR was designed to assess HRQoL in addition to the work impact of PsA, for this analysis we only included studies reporting work impact, captured using the Work Productivity and Activity Impairment (WPAI) questionnaire [14]. Only studies reporting outcomes related to a specific intervention as listed in the eligibility criteria were included.
The search strategy was based on key terms and synonyms related to the WPAI, work (e.g. work, employment), and productivity (e.g. presenteeism, absenteeism, impact, loss, capacity). We searched MEDLINE, Embase, EconLit, and Cochrane from January 1, 2010, through the search date of October 22, 2021. A hand search was conducted in August 2022 to update the evidence base. Data sources and the full search strategy are provided in Table S2 and Table S3, respectively.
All records were screened independently by two reviewers. Disagreements on a publication’s eligibility were resolved by discussion and/or arbitration provided by a third reviewer. Data extraction of study characteristics and outcomes of included studies was performed by a single reviewer (MR) and validated by a senior member of the research team (BH).
Outcomes
The primary outcome of interest for this analysis was health-related work impairment as measured using the WPAI, a patient-reported outcome [14].
The WPAI has four domains to assess absenteeism (the percentage of work time missed), presenteeism (the percentage of impairment experienced while at work), overall or total work productivity impairment (work impairment due to absenteeism and presenteeism), and leisure activity impairment (impairment of activities of daily living). The four domain scores are expressed as percentages, with high percentage scores indicating a high degree of impairment and less productivity over the past 7 days [14]. Only patients employed at baseline are included in the evaluation of WPAI, with the exception of the activity impairment domain which may also include non-employed patients.
We estimated changes in WPAI by comparing WPAI domains, when starting a b/tsDMARD and after around 6 months of treatment. Of note, this corresponds to a pre-post analysis but was not adjusted for placebo response (i.e. there was no comparison to improvements in the placebo group). Indeed, not all the studies had a placebo group, and to compare to placebo, a network meta-analysis would have been needed.
To explore the indirect costs attributable to PsA and the changes following treatment (again, this corresponds to ‘raw’ changes not adjusted to placebo response), we estimated a monetary value for the total productivity loss using the human capital approach, as explained below [15, 16].
Evidence synthesis
A random effects meta-analysis of single means was performed using RStudio Version 2022.07.1 (meta package v4.17–0) [17]. The outcome of interest was the mean change in WPAI scores from baseline to the timepoint closest to 24 weeks (i.e. 24 weeks ± 4 weeks). Meta-analysis results were reported as absolute mean change from baseline in WPAI score (weighted by study sample size) and 95% confidence interval (CI), which equates to a pooled or summary estimate of the WPAI score across the included studies around 24 weeks. For illustrative purposes, relative change was also assessed. Results for absolute change are presented as percentage point (%p), whereas relative change is percent. The reference case analysis included any studies reporting WPAI outcomes as a mean change or least-squares mean (LSM) change from baseline. A scenario analysis was performed in which the adjusted means (i.e. LSM change) were excluded from the meta-analysis and only the raw values (i.e. mean change) were considered to examine internal validity.
The results from the meta-analyses were also used to estimate the indirect costs attributable to PsA [15]. For this analysis, we assigned a monetary value to lost productivity using the human capital approach, which takes the patient’s perspective by counting any hour not worked as an hour of lost productivity [16]. Domain scores were multiplied by 40 h (assuming a standard work week) to estimate the total lost productivity (total work impairment due to absenteeism and presenteeism). We then multiplied the lost hours of productivity by €29.10 [18, 19], the reported 2021 average hourly labour costs in the European Union (27 countries, from 2020) and $40.35 [20], the 2021 employer cost for employee compensation for the United States (US), to broadly capture the international nature of the studies used in this analysis.
Results
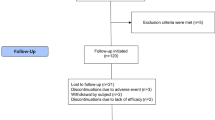
Of 6689 records, 751 publications were selected for full-text review, and 27 publications (from 14 unique studies) reported WPAI data. Two additional studies were identified from the hand search and one data on file from the sponsor (UCB) was also included, resulting in a total of 30 reports from 17 unique studies. Among these, 12 studies reported outcomes at a timepoint close to 24 weeks and were evaluated in the meta-analysis (Fig. 1).
Of the 12 studies, 10 drew evidence from randomized controlled trials (RCTs) with a placebo comparator and two from prospective observational studies (Table 1). Study sample sizes ranged from 100 [21] to 1281 [22] patients (mean, 532 patients). The interventions assessed included adalimumab (n = 4 studies), secukinumab (n = 3), ixekizumab (n = 2), risankizumab (n = 2), upadacitinib (n = 2), bimekizumab (n = 1), and guselkumab (n = 1). Most RCTs allowed patients in the intervention and placebo arms to take concomitant conventional synthetic (cs)DMARDs such as methotrexate, corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), or other analgesics. A risk of bias assessment was performed and presented in Table S4.
Overall, across all WPAI domains between 3683 and 5774 patients at baseline and 2425 and 3774 patients at week 24 were analysed. Among all studies, 48.8% of patients were male, the weighted mean age of patients was 50.1 years, and the weighted mean disease duration was 7.0 years (Table 1). Where reported, an average of 58.7% of patients were employed at baseline.
Absenteeism
Among the 3741 patients with baseline WPAI data included in the meta-analysis, the pooled estimated mean absenteeism score (percent of time missed from work over a 7-day period due to PsA) was 11.4%, range 5.8–16.3% (95% CI 10.2, 12.6) (Table 2). This can be illustrated as 4.6 h absent from work per week, based on a 40-h work week. At week 24, the pooled absolute mean change from baseline among patients treated with a b/tsDMARD was − 2.4%p, range − 12.5 to 6.1%p (95% CI − 4.1, − 0.6) (Fig. 2), i.e. a relative improvement of 21.0%. In general, there was a greater estimated improvement in absenteeism scores among patients receiving a b/tsDMARD compared to patients taking placebo (Figure S1).
Meta-analysis of percent mean CFB in absenteeism scores per intervention at 24 weeks. Note: Point estimates represent the mean CFB scores reported for each intervention. No direct comparison is intended nor was made across interventions. *Denotes observational study. CFB, change from baseline; CI, confidence interval; Q2W, every 2 weeks; Q4W, every 4 weeks; Q8W, every 8 weeks
Presenteeism
The meta-analysis estimated mean presenteeism score (percent of impairment while working due to PsA) at baseline was 38.7% (n = 3620), range 30.5–47.3% (95% CI 35.7, 43.2) (Table 2). This equates to 15.5 h of impaired or reduced work performance per week.
In the 12 studies (2425 patients), the pooled absolute mean change from baseline in presenteeism scores was − 17.8%p, range − 24.3 to − 8.7%p (95% CI − 19.3, − 16.2) among patients treated with a b/tsDMARD (Fig. 3) with a relative improvement of 46.0%. Improvements in presenteeism scores among patients taking placebo were smaller, with an estimated pooled mean change of − 5.5% from baseline (Figure S2).
Meta-analysis of percent mean CFB in presenteeism scores per intervention at 24 weeks. Note: Point estimates represent the mean CFB scores reported for each intervention. No direct comparison is intended nor was made across interventions. *Denotes observational study. CFB, change from baseline; CI, confidence interval; Q2W, every 2 weeks; Q4W, every 4 weeks; Q8W, every 8 weeks
Work productivity impairment
Baseline work productivity impairment scores were available for 3683 patients. The meta-analysis estimated mean loss of work productivity at baseline was 42.7%, range 34.2–50.8% (95% CI 40.6, 44.9) (Table 2), which can be estimated as 17.1 h of total work productivity lost per week. At 24 weeks, for patients treated with a b/tsDMARD, the pooled absolute mean change in total work productivity was − 17.6%p, range − 25.2 to − 12.2%p (95% CI − 19.4, − 15.9) (Fig. 4) with a mean relative improvement of 41.2%. Similar to other WPAI domains, improvements in total work productivity scores among patients taking placebo for up to 24 weeks were small (Figure S3).
Meta-analysis of percent mean CFB total work productivity impairment scores per intervention at 24 weeks. Note: Point estimates represent the mean CFB scores reported for each intervention. No direct comparison is intended nor was made across interventions. *Denotes observational study. CFB, change from baseline; CI, confidence interval; Q2W, every 2 weeks; Q4W, every 4 weeks; Q8W, every 8 weeks
Activity impairment
Baseline activity impairment was reported for 5774 patients, since unlike the other WPAI domains, this domain includes patients who were not employed. The estimated mean baseline impairment was 48.9%, range 41.7–55.1% (95% CI 47.5, 50.4), indicating the percent of impaired or reduced ability to participate in leisure activities over a 7-day period (Table 2). Overall, all patients treated with b/tsDMARDs reported a reduction in activity impairment from baseline with a pooled absolute mean change of − 19.3%p (95% CI − 21.4, − 17.6) (Fig. 5) and a mean relative improvement of 39.5%.
Meta-analysis of percent mean CFB in activity impairment scores per intervention at 24 weeks. Note: Point estimates represent the mean CFB scores reported for each intervention. No direct comparison is intended nor was made across interventions. *Denotes observational study. CFB, change from baseline; CI, confidence interval; Q2W, every 2 weeks; Q4W, every 4 weeks; Q8W, every 8 weeks
Indirect costs
At baseline, the overall productivity loss among patients with PsA reported in this review ranged from 13.7 to 20.3 h per week. This equates to an estimated range of indirect costs for the European Union of €20,757 to €30,833 per patient per year (US$28,782 to US$42,753). After treatment with a b/tsDMARD, there was a pooled mean improvement in total work productivity of 7.0 h per week (mean change from baseline, − 17.6%). Based on the analysis of change from baseline among patients treated with b/tsDMARDs, and without adjusting on placebo response, the estimated absolute mean decrease in PsA-related indirect costs linked to productivity was €10,688 (US$14,820) per patient, per year.
Discussion
This review reports important information on the burden of PsA on work prior to and following b/tsDMARD treatment. In studies of b/tsDMARDs among patients with PsA, at treatment introduction, patients presented with a high burden of their disease on work, with an estimated mean work productivity loss of 17.1 h per week, or a mean reduction of 42.7% in total work productivity. In all studies, presenteeism was a greater contributor to overall work productivity loss than absenteeism. Exploratory extrapolations of indirect costs associated with work productivity impairment yielded estimates between €20,000 to €30,000 (US$28,000 to US$42,000) per person annually. Beyond work outcomes, the additional burden was noted in the form of leisure activity impairment (mean, 48.9%). Through a meta-analysis corresponding to changes with treatment (without adjustments for placebo response), we found that after 24 weeks of treatment with b/tsDMARDs, there was a mean absolute improvement of 17.6%p in total work productivity, corresponding to a mean relative improvement of 41%. After treatment with a b/tsDMARD, the pooled mean improvement in total work productivity of 7.0 h per week led to an estimated absolute mean decrease in PsA-related indirect costs of €10,688 (US$14,820) per patient, per year. These results provide clinical-, regulatory- and reimbursement decision-makers with valuable data on the societal and socio-economic benefits of b/tsDMARDs in PsA.
The findings of our review are consistent with previous studies, confirming the significant impact of PsA on work outcomes [7] and how presenteeism is a higher contributor to overall lost work productivity than absenteeism among patients with PsA [15]. This highlights that when patients with PsA attend work, their productivity is considerably impacted by PsA [34]. The reported effects of diminished productivity include reduced personal and professional development. Furthermore, as work plays an important role in one’s social life and integration into society, reduced ability to participate in work may increase isolation and have deleterious effects on the wellbeing of patients; decreased work productivity has been linked to decrements in QoL and mental health [35,36,37].
PsA has a high cost for society. Published estimations of the annual direct PsA-related health care costs have been reported to be as high as US$1.9 billion [8]. Indirect costs are estimated to be even greater, accounting for 52 to 72% of total disease-related costs [8]. In a systematic review and meta-analysis [38], Kawalec and colleagues estimated that the average annual indirect costs of PsA range from US$1694 to $12,318 (using the friction cost approach) or from US$1751 to $50,271 (using the human capital approach). When using the human capital approach, this range of estimates is higher than our review and can be attributed to differences in the included studies and the scope of indirect costs calculated.
Overall, improvements in productivity were significant and clinically relevant after 24 weeks of b/tsDMARDs, though variation in different domains was observed. It is important to note that the results presented here for improvements after treatment were not adjusted for changes in a comparator or placebo arm; therefore, these improvements correspond to a ‘simple’ before-after analysis and cannot in any way be considered as due to treatment (no causality is claimed). Findings for the absenteeism domain presented mixed results, with several studies not reporting an improvement in scores at 24 weeks. In contrast, all studies reported an improvement in presenteeism at 24 weeks, with a pooled estimated mean change from baseline of − 17.8% p (95% CI − 19.3, − 16.2). This is close to the minimal clinically important difference (MCID) of 20%, which was estimated by Tillett and colleagues [39]. This reported MCID applies to patient-level data; however, it provides a useful benchmark for our review.
Previous studies have demonstrated associations between productivity and response (minimal disease activity [MDA] or low disease activity according to PsA Disease Activity Score [PASDAS]) [10, 40] and found greater improvements in productivity with bDMARDs than with csDMARDs [41]. Generally, the estimated effects of the b/tsDMARDs in the current analysis were similar with respect to improving a patient’s capacity to work and participate in leisure activities. However, it is important to note that we did not directly compare the drugs as this would necessitate specific statistics such as network meta-analyses, which can provide rankings of relative effects of different treatments, but may also be influenced by heterogeneity between studies, leading to limitations in interpretability in some cases. Studies aimed to measure both the effectiveness and the impact of specific interventions on productivity and HRQoL in patients with PsA may be valuable in supporting optimized treatment selection from a holistic perspective.
This review has several strengths. The evidence was retrieved through a systematic search of the literature according to methodological guidance and reporting and included a recent update to account for the evolving treatment landscape in PsA. Analyses were based on both RCTs and observational studies, allowing for a wider scope than a previous review on this topic, which was limited to RCTs and included only five studies [42].
Despite these strengths, this review has some limitations. The analysis focused solely on the WPAI, a widely used measure of productivity that has been validated for use among patients with PsA [14, 43]. While there is no gold standard measure for assessing productivity in PsA, the WPAI was one of six instruments identified by the OMERACT Worker Productivity Group as a candidate for assessing work productivity based on available evidence regarding psychometric properties (e.g. test–retest reliability, construct validity) [44]. However, other questionnaires, such as the Work Productivity Scale (WPS) [45] or the Work Limitations Questionnaire (WLQ) [43, 46], may also be used to evaluate work impact. While this review excludes studies using these alternative assessment tools, the selection of a single measure facilitated the comparability of findings and allowed us to conduct a quantitative synthesis of findings. A network meta-analysis was not performed in which comparative treatment effects were estimated. Our approach to the analysis was taken to allow for the inclusion of observational studies that did not have a placebo arm; thus, a limitation is that no causal conclusions on the effect of b/tsDMARDs on work productivity can be derived. Future research using an NMA approach and limiting study inclusion to RCTs may provide more robust estimates.
The variation in reporting of WPAI outcomes required certain assumptions for the meta-analysis. For example, data reported as means and LSM were pooled following a scenario analysis to explore the internal validity of using raw and adjusted means. No major differences were observed between these analyses. As WPAI is often considered a secondary outcome measure, there was a lack of reporting of subgroup analyses related to patient characteristics (e.g. tumour necrosis factor inhibitors experience) and other factors that may contribute to work and/or activity impairment (e.g. pain, fatigue, participation in manual work). This limited our ability to conduct sensitivity analysis or additional analyses on subgroups of interest. This limitation reflects a shortcoming in the body of published evidence and not the methodology of the review itself.
A final limitation is the variation in the methods of estimating the costs attributable to lost productivity due to PsA. While the WPAI focuses on absenteeism and presenteeism, other components of productivity may be considered, such as early retirement due to disease or patients returning to work after successful treatment [38]. Lost productivity can also be valued using different approaches, with indirect costs typically calculated using the friction cost method or the human capital approach [16]. We estimated indirect costs using the human capital approach, which may overestimate the indirect costs incurred by employers given the limited amount of published data available. Cost conclusions are further limited by the level of heterogeneity across studies. However, these estimates are a reflection of the larger, societal burden of PsA.
Our review focused on patients with PsA treated with a b/tsDMARD. These patients could be considered as having a more severe form of disease due to failure of first-line treatment with NSAIDs and csDMARDs. Future research could consider productivity among a broader PsA population [47, 48].
The review was also structured to consider both RCT and observational evidence. Only two observational studies provided WPAI scores at 24 weeks. These studies reported some of the largest [33] and lowest [21] improvements in mean change from baseline WPAI domain scores. This suggests potential variation in productivity outcomes in real-life settings. It is important to note that one study was from the US and the other from Japan, which may have inherent differences in working and productivity. However, it is not feasible to explore this potential “country-effect” due to limited evidence and the fact that both studies had limited sample sizes; therefore, the results should be interpreted with caution.
Conclusion
Measuring work impact should be considered an essential part of the overall assessment of the economic burden and the value assessment of therapies in PsA. This review systematically and comprehensively quantified the impact of PsA on work productivity and impairment using the WPAI among patients treated with a b/tsDMARD. The results demonstrate that patients with PsA suffered from substantial total work productivity impairment but report meaningful improvement after 24 weeks of treatment with a b/tsDMARD. This provides payers and other decision-makers with valuable data to inform decisions about the cost-effectiveness of b/tsDMARDs in PsA.
Availability of data and materials
The data that support the findings of this study are primarily from published literature. Data from BE OPTIMAL (NCT03895203) [25] may be requested by qualified researchers 6 months after product approval in the US and/or Europe, or global development is discontinued, and 18 months after trial completion. Investigators may request access to anonymized individual patient-level data and redacted trial documents which may include analysis-ready datasets, study protocol, annotated case report form, statistical analysis plan, dataset specifications, and clinical study report. Prior to the use of the data, proposals need to be approved by an independent review panel at www.Vivli.org and a signed data-sharing agreement will need to be executed. All documents are available in English only, for a pre-specified time, typically 12 months, on a password-protected portal. This plan may change if the risk of re-identifying trial participants is determined to be too high after the trial is completed; in this case and to protect participants, individual patient-level data would not be made available.
Abbreviations
- %p:
-
Percentage point
- b:
-
Biologic
- CI:
-
Confidence interval
- cs:
-
Conventional synthetic
- DMARDs:
-
Disease-modifying antirheumatic drugs
- HRQoL:
-
Health-related quality of life
- ICF:
-
International Classification of Functioning, Disability and Health
- LSM:
-
Least-squares mean
- MCID:
-
Minimal clinically important difference
- MDA:
-
Minimal disease activity
- NSAID:
-
Non-steroidal anti-inflammatory drugs
- PASDAS:
-
Psoriatic Arthritis Disease Activity Score
- PICOS:
-
Population, Intervention, Comparator, Outcome and Study Design
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PsA:
-
Psoriatic arthritis
- RCT:
-
Randomized controlled trials
- SLR:
-
Systematic literature review
- ts:
-
Targeted synthetic
- WHO:
-
World Health Organization
- WLQ:
-
Work Limitations Questionnaire
- WPAI:
-
Work Productivity and Activity Impairment Questionnaire
- WPS:
-
Work Productivity Scale
References
Husni ME, Merola JF, Davin S. The psychosocial burden of psoriatic arthritis. Semin Arthritis Rheum. 2017;47(3):351–60. https://doi.org/10.1016/j.semarthrit.2017.05.010.
Ogdie A, Weiss PF. The epidemiology of psoriatic arthritis. Rheum Dis Clin North Am. 2015;41(4):545–68.
Karmacharya P, Ogdie A, Eder L. Psoriatic arthritis and the association with cardiometabolic disease: a narrative review. Ther Adv Musculoskelet Dis. 2021;13:1759720X21998279. https://doi.org/10.1177/1759720X21998279.
Gudu T, Gossec L. Quality of life in psoriatic arthritis. Expert Rev Clin Immunol. 2018;14(5):405–17. https://doi.org/10.1080/1744666X.2018.1468252.
Gudu T, Kiltz U, de Wit M, Kvien TK, Gossec L. Mapping the effect of psoriatic arthritis using the International Classification of Functioning, Disability and Health. J Rheumatol. 2017;44(2):193–200. https://doi.org/10.3899/jrheum.160180.
Tillett W, Shaddick G, Askari A, et al. Factors influencing work disability in psoriatic arthritis: first results from a large UK multicentre study. Rheumatology. 2014;54(1):157–62. https://doi.org/10.1093/rheumatology/keu264.
Tillett W, de Vries C, McHugh NJ. Work disability in psoriatic arthritis: a systematic review. Rheumatology (Oxford). 2012;51(2):275–83. https://doi.org/10.1093/rheumatology/ker216.
Lee S, Mendelsohn A, Sarnes E. The burden of psoriatic arthritis: a literature review from a global health systems perspective. P t. 2010;35(12):680–9.
Gossec L, Walsh JA, Michaud K, et al. Effect of fatigue on health-related quality of life and work productivity in psoriatic arthritis: Findings From a Real-World Survey. J Rheumatol. 2022;49(11):1221–8. https://doi.org/10.3899/jrheum.211288.
van Hal TW, Mulder MLM, Wenink MH, Vriezekolk JE. Determinants of work and social participation in patients with psoriatic arthritis in the Netherlands: an observational study. BMC Rheumatol. 2022;6(1):49. https://doi.org/10.1186/s41927-022-00279-7.
Coates L, Gossec L. The updated GRAPPA and EULAR recommendations for the management of psoriatic arthritis: similarities and differences. Joint Bone Spine. 2023;90(1):105469. https://doi.org/10.1016/j.jbspin.2022.105469.
Systematic Reviews: CRD's guidance for undertaking reviews in health care. University of York. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf. Accessed 19 May 2022
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65. https://doi.org/10.2165/00019053-199304050-00006.
Kruntorádová K, Klimeš J, Šedová L, Štolfa J, Doležal T, Petříková A. Work productivity and costs related to patients with ankylosing spondylitis, rheumatoid arthritis, and psoriasis. Value in Health Reg Issues. 2014;4:100–6. https://doi.org/10.1016/j.vhri.2014.07.008.
van den Hout WB. The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis. 2010;69(Suppl 1):i89-91. https://doi.org/10.1136/ard.2009.117150.
Balduzzi S, Rucker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60. https://doi.org/10.1136/ebmental-2019-300117.
Labour costs levels by NACE Rev. 2 activity. European Commission. Updated 17 May 2022. https://ec.europa.eu/eurostat/databrowser/view/LC_LCI_LEV__custom_709491/bookmark/table?lang=en&bookmarkId=eb78a6c4-aa9b-4210-ad86-6f9d003e1952. Accessed Aug 18 2022
Low and high pay in the UK: 2021 - The distribution of hourly earnings of high-paid and low-paid jobs and jobs paid below the National Minimum Wage. Office for National Statistics. Updated 26 October 2021. https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/lowandhighpayuk/2021. Accessed 08 Aug 2022
Total compensation cost per hour worked for civilian workers (Q4, 2021). U.S. Bureau of Labor Statistics. https://www.bls.gov/ncs/ect/. Accessed 11 Jan 2023
Mease PJ, Blachley T, Glynn M, et al. Secukinumab improves clinical and patient-reported outcomes at 6 months among patients with psoriatic arthritis in the US-based corrona psoriatic arthritis/spondyloarthritis (PSA/SPA) registry. Conference Abstract. Ann Rheum Dis. 2020;79(SUPPL 1):1169. https://doi.org/10.1136/annrheumdis-2020-eular.1014.
Strand V, Mease PJ, Soriano ER, et al. Improvement in patient-reported outcomes in patients with psoriatic arthritis treated with upadacitinib versus placebo or adalimumab: results from SELECT-PsA 1. Rheumatol Ther. 2021 https://doi.org/10.1007/s40744-021-00379-9
Kristensen LE, Soliman AM, Papp K, et al. Risankizumab improved health-related quality of life, fatigue, pain and work productivity in psoriatic arthritis: results of KEEPsAKE 1. Rheumatology. 2022:keac342. https://doi.org/10.1093/rheumatology/keac342
Ostor AJK, Soliman AM, Papp KA, et al. Improved patient-reported outcomes in patients with psoriatic arthritis treated with risankizumab: analysis of the Phase 3 trial KEEPsAKE 2. RMD Open. 2022;8(2):e002286.
McInnes IB, Asahina A, Coates LC, et al. Bimekizumab in patients with psoriatic arthritis, naive to biologic treatment: a randomised, double-blind, placebo-controlled, phase 3 trial (BE OPTIMAL). Lancet. 2023;401(10370):25–37. https://doi.org/10.1016/S0140-6736(22)02302-9.
Curtis J, McInnes I, Rahman P, et al. Guselkumab provides sustained improvements in work productivity and non-work activity in psoriatic arthritis patients: Phase 3 results through year 1. Conference Abstract. Int J Rheum Dis. 2021;24(SUPPL 2):72–3. https://doi.org/10.1111/1756-185X.14199.
Strand V, Van den Bosch F, Ranza R, et al. Patient-reported outcomes in psoriatic arthritis patients with an inadequate response to biologic disease-modifying antirheumatic drugs: SELECT-PsA 2. Rheumatol Ther. 2021;https://doi.org/10.1007/s40744-021-00377-x
Strand V, Mease P, Gossec L, et al. Secukinumab improves patient-reported outcomes in subjects with active psoriatic arthritis: results from a randomised phase III trial (FUTURE 1). J Article Ann Rheum Dis. 2017;76(1):203–7.
Tillett W, Lin CY, TrevelinSprabery A, Birt JA, Kavanaugh A. Clinically meaningful improvement in work productivity loss in active psoriatic arthritis: post-hoc analysis of SPIRIT-P1 and SPIRIT-P2 trials. Clinical Trial, Phase III Randomized Controlled Trial. Clin Exp Rheum. 2020;38(6):1227–30.
Kavanaugh A, Marzo-Ortega H, Vender R, et al. Ixekizumab improves patient-reported outcomes in patients with active psoriatic arthritis and inadequate response to tumour necrosis factor inhibitors: SPIRIT-P2 results to 52 weeks. Randomized Controlled Trial. Clin Exp Rheum. 2019;37(4):566–74.
Gottlieb AB, Strand V, Kishimoto M, et al. Ixekizumab improves patient-reported outcomes up to 52 weeks in bDMARD-naive patients with active psoriatic arthritis (SPIRIT-P1). Randomized Controlled Trial; Research Support, Non-U.S. Gov’t. Rheumatol. 2018;57(10):1777–88. https://doi.org/10.1093/rheumatology/key161.
McInnes IB, Mease PJ, Ritchlin CT, et al. Secukinumab sustains improvement in signs and symptoms of psoriatic arthritis: 2 year results from the phase 3 FUTURE 2 study. Article. Rheumatology (oxford, england). 2017;56(11):1993–2003.
Nakagawa H, Tanaka Y, Sano S, et al. Real-world postmarketing study of the impact of adalimumab treatment on work productivity and activity impairment in patients with psoriatic arthritis. Adv Ther. 2019;36(3):691–707. https://doi.org/10.1007/s12325-018-0866-y.
Drouet JMS, Gossec L. Work-related issues and a high burden of disease are frequent in axial spondyloarthritis: what should we be doing better? J Rheumatol. 2023 https://doi.org/10.3899/jrheum.221252
Garrido-Cumbrera M, Hillmann O, Mahapatra R, et al. Improving the management of psoriatic arthritis and axial spondyloarthritis: roundtable discussions with healthcare professionals and patients. Rheumatol Ther. 2017;4(2):219–31. https://doi.org/10.1007/s40744-017-0066-2.
Haglund E, Bremander A, Bergman S, Jacobsson LT, Petersson IF. Work productivity in a population-based cohort of patients with spondyloarthritis. Rheumatology (Oxford). 2013;52(9):1708–14. https://doi.org/10.1093/rheumatology/ket217.
Ramonda R, Marchesoni A, Carletto A, et al. Patient-reported impact of spondyloarthritis on work disability and working life: the ATLANTIS survey. Arthritis Res Ther. 2016;18:78. https://doi.org/10.1186/s13075-016-0977-2.
Kawalec P, Malinowski KP. The indirect costs of psoriatic arthritis: systematic review and meta-analysis. Expert Rev Pharmacoecon Outcomes Res. 2015;15(1):125–32. https://doi.org/10.1586/14737167.2015.965154.
Tillett W, Lin C-Y, Zbrozek A, Sprabery AT, Birt J. A threshold of meaning for work disability improvement in psoriatic arthritis measured by the work productivity and activity impairment questionnaire. Rheumatol Ther. 2019;6(3):379–91. https://doi.org/10.1007/s40744-019-0155-5.
Wervers K, Luime JJ, Tchetverikov I, et al. Time to minimal disease activity in relation to quality of life, productivity, and radiographic damage 1 year after diagnosis in psoriatic arthritis. Arthritis Res Ther. 2019;21(1):25. https://doi.org/10.1186/s13075-019-1811-4.
Tillett W, Shaddick G, Jobling A, et al. Effect of anti-TNF and conventional synthetic disease-modifying anti-rheumatic drug treatment on work disability and clinical outcome in a multicentre observational cohort study of psoriatic arthritis. Rheumatology (Oxford). 2017;56(4):603–12. https://doi.org/10.1093/rheumatology/kew433.
Iragorri N, Hofmeister M, Spackman E, Hazlewood GS. The effect of biologic and targeted synthetic drugs on work- and productivity-related outcomes for patients with psoriatic arthritis: a systematic review. J Rheumatol. 2018;45(8):1124–30. https://doi.org/10.3899/jrheum.170874.
Prasad M, Wahlqvist P, Shikiar R, Tina Shih Y-C. A review of self-report instruments measuring health-related work productivity. PharmacoEconomics. 2004;22(4):225–44. https://doi.org/10.2165/00019053-200422040-00002.
Verstappen SMM, Lacaille D, Boonen A, et al. Considerations for evaluating and recommending worker productivity outcome measures: an update from the OMERACT Worker Productivity Group. J Rheumatol. 2019;46(10):1401–5. https://doi.org/10.3899/jrheum.181201.
Osterhaus JT, Purcaru O. Discriminant validity, responsiveness and reliability of the arthritis-specific Work Productivity Survey assessing workplace and household productivity in patients with psoriatic arthritis. Arthritis Res Ther. 2014;16(4):R140. https://doi.org/10.1186/ar4602.
Kennedy M, Papneja A, Thavaneswaran A, Chandran V, Gladman DD. Prevalence and predictors of reduced work productivity in patients with psoriatic arthritis. Clin Exp Rheumatol May-Jun. 2014;32(3):342–8.
Albrecht K, Regierer AC, Strangfeld A, Marschall U, Callhoff J. High burden of polypharmacy and comorbidity in persons with psoriatic arthritis: an analysis of claims data, stratified by age and sex. RMD Open. 2023;9(1) https://doi.org/10.1136/rmdopen-2022-002960
Puche-Larrubia MA, Ladehesa-Pineda L, Lopez-Montilla MD, et al. Differences between early vs. Late-onset of psoriatic arthritis: data from the respondia and regisponser registries. Joint Bone Spine. 2023:105563. https://doi.org/10.1016/j.jbspin.2023.105563
Acknowledgements
The authors acknowledge Heather Edens (UCB Pharma, Smyrna, GA, USA) for publication coordination and editorial assistance and Elizabeth Hubscher (Cytel, Inc., Waltham, MA) for medical writing and editorial assistance based on the authors’ input and direction. The authors also acknowledge Costello Medical for administrative and submission support.
Funding
This study was sponsored by UCB Pharma, including support for third-party writing assistance.
Author information
Authors and Affiliations
Contributions
DW, VT, BH, and MR conceptualized and designed the study. BH and MR were involved in the data collection and analysis. All authors were involved in the interpretation of the results. All authors were involved in preparation of the manuscript, critical review and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This SLR and meta-analysis was based on published literature and de-identified results of the BE OPTIMAL (NCT03895203) trial [25]; therefore, additional ethics approval was not required. This paper was developed in accordance with the Good Publication Practice (GPP3) guidelines (https://www.ismpp.org/gpp3).
Consent for publication
All authors agreed to the publication of this manuscript.
Competing interests
LG: Received grants or contracts from Pfizer, Sandoz and UCB, consulting fees from AbbVie, Bristol-Myers Squibb, Celltrion, Galapagos, Janssen, Novartis, Pfizer and UCB, honoraria for lectures from AbbVie, Amgen, Galapagos, Gilead, Janssen, Lilly, MSD, Novartis, Pfizer, Sandoz and UCB, support for attending meetings and/or travel from MSD, Novartis, and Viatris, and has received medical writing support from AbbVie, Janssen, Pfizer and UCB. All unrelated to the present study.
BH: Consultant to UCB Pharma.
MR: Consultant to UCB Pharma.
VT: Employee of UCB Pharma.
DW: Employee and shareholder of UCB.
WT: Research funding, consulting or speaker fees from AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Pfizer and UCB. Consulting and speaker fees from AbbVie, Amgen, Celgene, Eli Lilly, Janssen, MSD, Novartis, ONO Pharma, Pfizer and UCB.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
PICOS eligibility criteria. Figure S1. Meta-analysis of percent mean CFB in absenteeism scores for placebo at 24 weeks. Figure S2. Meta-analysis of percent mean CFB in presenteeism scores for placebo at 24 weeks. Figure S3. Meta-analysis of percent mean CFB in total work productivity scores for placebo at 24 weeks. Figure S4. Meta-analysis of percent mean CFB activity impairment scores for placebo at 24 weeks. Table S2. Data sources. Table S3. Search strategy with results. Table S4. Risk of bias assessment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gossec, L., Humphries, B., Rutherford, M. et al. Improvement in work productivity among psoriatic arthritis patients treated with biologic or targeted synthetic drugs: a systematic literature review and meta-analysis. Arthritis Res Ther 26, 50 (2024). https://doi.org/10.1186/s13075-024-03282-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-024-03282-0