Abstract
Background
The association between systemic sclerosis and the development of bronchiectasis is unclear. This study aimed to compare the risk of bronchiectasis between individuals with systemic sclerosis and those without using a nationwide longitudinal dataset.
Methods
Using the Korean National Health Insurance Service dataset between 2010 and 2017, we identified 4845 individuals aged ≥ 20 years with systemic sclerosis and 24,225 without systemic sclerosis who were matched 1:5 by age and sex. They were followed up until the date of a bronchiectasis diagnosis, death, or December 31, 2019, whichever came first.
Results
During a median follow-up period of 6.0 (interquartile range, 3.2–8.7) years, 5.3% of the systemic sclerosis cohort and 1.9% of the matched cohort developed bronchiectasis, with incidence rates of 9.99 and 3.23 per 1000 person-years, respectively. Even after adjusting for potential confounders, the risk of incident bronchiectasis was significantly higher in the systemic sclerosis cohort than in the matched cohort (adjusted hazard ratio 2.63, 95% confidence interval 2.22–3.12). A subgroup analysis of individuals with systemic sclerosis revealed that the risk of incident bronchiectasis was notably higher in younger individuals aged 20–39 years (P for interaction = 0.048) and in those without other coexisting connective tissue diseases (P for interaction = 0.006) than in their counterparts.
Conclusions
The risk of incident bronchiectasis is higher in individuals with systemic sclerosis than those without. Bronchiectasis should be considered one of the pulmonary manifestations related to systemic sclerosis.
Similar content being viewed by others
Background
Systemic sclerosis is an autoimmune condition characterized by cutaneous fibrosis and multi-organ involvement, resulting in significant morbidity and mortality [1]. Before the availability of angiotensin-converting enzyme inhibitor therapeutics, renal disease was the most common cause of death [2]. However, pulmonary complications such as pulmonary arterial hypertension and interstitial lung disease (ILD) [3, 4], are the leading causes of death in patients with systemic sclerosis in recent years, suggesting the importance of managing comorbid pulmonary conditions [5,6,7].
Non-cystic fibrosis bronchiectasis (hereafter referred to as bronchiectasis) is a chronic lung disease characterized radiologically by permanent bronchial dilatation and clinically by the presence of cough, sputum, and recurrent chest infections [8]. A few systemic sclerosis cohort studies have reported that bronchiectasis is a common pulmonary comorbidity in patients with systemic sclerosis, ranging from 3.3 to 59.1% [9,10,11]. However, it is not well known whether the risk of incident bronchiectasis is higher in patients with systemic sclerosis due to small study populations and the absence of comparable controls [9,10,11]. Furthermore, bronchiectasis itself is known to be associated with increased mortality [12], and an inflammatory process in the lungs could provoke autoimmune responses in rheumatoid arthritis potentially creating a worse prognosis [13, 14]. This suggests that bronchiectasis may affect the prognosis of systemic sclerosis. In this regard, we need to consider comorbid bronchiectasis in patients with systemic sclerosis and an appropriate starting point would be to determine whether individuals with systemic sclerosis are at a higher risk of bronchiectasis than those without systemic sclerosis.
Therefore, this study aimed to compare the risk of incident bronchiectasis between a systemic sclerosis cohort and an age and sex-matched non-systemic sclerosis cohort drawn from a large nationally representative longitudinal database in Korea.
Materials and methods
Data source
This study used a dataset provided by the Korean National Health Insurance Service (NHIS), a universal insurance provider managed by the government that covers 97% of the Korean population, approximately 50 million people. The NHIS dataset includes information on socioeconomics, demographic variables, healthcare utilization, health examination findings, disease diagnosis based on the 10th revision of the International Classification of Disease (ICD-10) codes, and medical treatment and procedures [15]. The NHIS database includes a variety of medical and health information and has been widely used in various epidemiologic studies to identify risk factors for diseases [16, 17].
Our study protocol was approved by the Institutional Review Board of Chungbuk National University Hospital (No. 2023-01-014). The requirement for informed consent was waived because the NHIS database uses an anonymous patient identification system.
Study population and characteristics
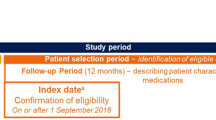
We initially included 5986 individuals who were diagnosed with systemic sclerosis between 2010 and 2017. After excluding those with missing data or who were younger than 20 years (n = 277), those who had previously been diagnosed with cystic fibrosis (n = 8), those who had previously been diagnosed with bronchiectasis (n = 617), and those who were diagnosed with bronchiectasis within 1 year after systemic sclerosis diagnosis (n = 235), we enrolled 4849 for the systemic sclerosis cohort. Of these 4849 individuals, 4845 were eligible for 1:5 age and sex matching. Thus, the study enrolled 4845 individuals for the systemic sclerosis cohort and matched these by age and sex to 24,225 control subjects who had not been diagnosed with systemic sclerosis or bronchiectasis (Fig. 1). The control group had health insurance claims for diseases other than systemic sclerosis in the same year that the matched participants with systemic sclerosis were diagnosed with the disease. Thus, the date of healthcare utilization in the matched year was regarded as the index date for the control group. Additionally, participants who had been diagnosed with cystic fibrosis and those who developed bronchiectasis within one year of enrollment were excluded from the control group.
Study exposure
The exposure of this study was systemic sclerosis, of which the definition required (1) at least one hospital visit with the ICD-10 diagnostic code M34.0, and 2) registration with the Rare and Intractable Disease program (code V138) [17]. Since January 2006, patients with rare and intractable diseases (e.g., malignancy, tuberculosis, and connective tissue disease [CTD]) have been registered in the Individual Copayment Beneficiaries Program in the Republic of Korea to reduce the burden of medical expenses [16, 18]. Thus, the validity of the systemic sclerosis diagnosis was strictly reviewed by the Health Insurance Review and Assessment Service. The date of registration in the Rare and Intractable Disease program for systemic sclerosis was defined as the index date.
Study outcome
The outcome of this study was the incidence of bronchiectasis. Bronchiectasis was defined as claims under the ICD-10 diagnosis code J47 without a concomitant diagnosis of cystic fibrosis (ICD-10 code E84) in any form of healthcare utilizations (i.e., outpatient department visits, emergency room visits, and hospitalization) [16, 19,20,21]. The study participants were followed up from the index date to the date of bronchiectasis incidence, censored date, or December 31, 2019 (end date of the study).
Covariates
The definitions of comorbidities (diabetes mellitus, hypertension, dyslipidemia, end-stage renal disease, ischemic heart disease, congestive heart failure, asthma, and chronic obstructive pulmonary disease [COPD]) were based on ICD-10 codes as previously described [19, 20, 22,23,24]. Additionally, tuberculosis and other CTDs (rheumatoid arthritis, systemic lupus erythematosus, dermatomyositis, mixed CTD, and polymyalgia rheumatica) were defined using ICD-10 codes as well as registration with the national rare intractable disease supporting program [17, 23, 24]. Household income was categorized into quartiles based on insurance premium levels (in Korea, insurance premiums are determined by income level), with those covered by Medical Aid (poorest 3%) being merged into the lowest income quartile [23,24,25].
Statistical analysis
Descriptive statistics are presented as numbers (percentages) for categorical variables and mean ± standard deviations (SDs) for continuous variables. We compared the two groups using the χ2 test for categorical variables, and t-test for continuous variables. The incidence rates of bronchiectasis were calculated by dividing the number of incident events by the total follow-up period (1000 person-years). A cumulative incidence plot was used to compare the incidence of bronchiectasis between the systemic sclerosis and matched cohorts, and a log-rank test was used to evaluate significant differences between the groups.
The risk of incident bronchiectasis in the systemic sclerosis cohort compared to the matched cohort was estimated using univariable and multivariable Cox proportional hazards regression analyses. Model 1 was an unadjusted model. Model 2 was adjusted for sex, age, income, diabetes mellitus, hypertension, and dyslipidemia. Model 3 was additionally adjusted for end-stage renal disease, ischemic heart disease, congestive heart failure, COPD, asthma, tuberculosis, and other CTDs. Stratified analyses were performed by sex, age, income, and comorbidities (COPD, asthma, tuberculosis, and other CTDs). Additionally, to exclude traction bronchiectasis associated with ILD, we performed a sensitivity analysis to assess the risk of bronchiectasis without a diagnostic code for ILD (J84). A two-sided P value < 0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
The mean age of the study population was 53.5 years (SD, 12.6 years) and 15.2% were male. The proportions of pulmonary and extra-pulmonary comorbidities were higher in the systemic sclerosis cohort than the matched cohort (p < 0.001 for all), except for diabetes mellitus (p = 0.840). Moreover, the proportions of other CTDs (rheumatoid arthritis, systemic lupus erythematosus, dermatomyositis, and mixed CTD) were also higher in the systemic sclerosis cohort than the matched cohort (p < 0.001 for all), except for polymyalgia rheumatica (p = 0.206) (Table 1).
Incidence and risk of bronchiectasis
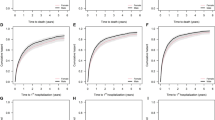
During the median follow-up period of 6.0 (interquartile range, 3.2–8.7) years, 5.3% (n = 259/4845) of the systemic sclerosis cohort and 1.9% (n = 455/24,225) of the matched cohort developed bronchiectasis, with incidence rates of 9.99 and 3.23 per 1000 person-years, respectively (Table 2). A cumulative incidence plot depicts a significantly higher incidence of bronchiectasis in the systemic sclerosis cohort than in the matched cohort (a log-rank p < 0.001; Fig. 2). Even after adjusting for potential confounders, the risk of incident bronchiectasis was also significantly higher in the systemic sclerosis cohort than in the matched cohort: unadjusted hazard ratio (HR) in Model 1 3.10, 95% confidence interval [CI], 2.66–3.61; adjusted HR in Model 2 3.08, 95% CI 2.63–3.61; adjusted HR in Model 3 2.63, 95% CI 2.22–3.12) (Table 2).
Subgroup analysis
As shown in Table 3, sex, income, and pulmonary comorbidities (COPD, asthma, or tuberculosis) did not have a significant impact on the association between systemic sclerosis and bronchiectasis development. In contrast, age and the presence of other CTDs had a significant interaction on the association of systemic sclerosis with bronchiectasis development. The risk of incident bronchiectasis was higher in younger individuals aged 20–39 years (P for interaction = 0.048) and in those without other coexisting CTDs (P for interaction = 0.006) than in their counterparts. Subgroup analysis according to other comorbidities is shown in Supplementary Table 3.
Discussion
To the best of our knowledge, this is the largest comprehensive study to evaluate the risk of bronchiectasis in systemic sclerosis by using a nationwide dataset. In this study, individuals with systemic sclerosis had a 9.99 per 1000 person-years of bronchiectasis incidence rate, which is 3-fold higher compared to that in those without systemic sclerosis (3.23 per 1000 person-years). Additionally, the risk of bronchiectasis development in systemic sclerosis was especially higher in younger individuals and in those without concomitant CTDs than in their counterparts.
Previous studies reporting the prevalence of bronchiectasis in patients with systemic sclerosis were based on small cohorts of systemic sclerosis (the largest study population was 256). In this regard, the prevalence of bronchiectasis in systemic sclerosis was reported to range widely from 3.3 to 59.1% [9,10,11]. To overcome the limitations of small study populations in previous studies, our study included a large number of individuals with systemic sclerosis (n = 4485) and revealed that about 5.5% of individuals with systemic sclerosis developed new bronchiectasis during a median 6-year follow-up period. Furthermore, by comparing the incidence of bronchiectasis between systemic sclerosis and control groups, we could reveal that systemic sclerosis could be an important etiology of bronchiectasis.
Several potential hypotheses that can explain the development of bronchiectasis in patients with systemic sclerosis exist. First, approximately 90% of patients with systemic sclerosis have gastrointestinal tract involvement [26], and the most common site is the esophagus (80%) [27]. Esophageal dysmotility could be associated with the aspiration of upper gastrointestinal contents into the airways [28]. Thus, aspiration of gastrointestinal contents might result in local bronchial inflammation, immune cell recruitment, and free radical release, which may be followed by bronchial wall damage and a consequent irreversible abnormal bronchial wall dilatation, a characteristic of bronchiectasis [29]. Second, in other CTDs, such as rheumatoid arthritis, previous studies have suggested that precedent systemic inflammation leads to the development of bronchiectasis. This notion is supported by the association between antibodies against citrullinated protein antigens and a higher risk of bronchiectasis [30] or between longer rheumatoid arthritis duration and bronchiectasis [31, 32]. This phenomenon may also explain the association between systemic sclerosis and the development of bronchiectasis. Third, the use of immunosuppressants in systemic sclerosis might be related to recurrent respiratory infection, which is an important cause of bronchiectasis [33]. Fourth, a mechanism by which sclerosis occurs within the bronchial wall, impairing ciliary contractility, and pathogen clearance, is also proposed as a hypothesis [34].
Interestingly, our subgroup analysis showed that the association between systemic sclerosis and bronchiectasis was more prominent in younger participants than in older participants. This phenomenon could be explained by the fact that older participants have many factors that influence the development of bronchiectasis (i.e., antedated respiratory infections, tuberculosis history, and comorbid airway diseases), whereas bronchiectasis development in younger participants may be relatively more influenced by systemic sclerosis. Furthermore, if bronchiectasis occurs in younger individuals with systemic sclerosis, they would experience the development of respiratory symptoms and deterioration of the quality of life during treatment for systemic sclerosis. Because immunosuppressants are used for treating systemic sclerosis, patients with comorbid bronchiectasis may be prone to recurrent respiratory infections [35]. Thus, bronchiectasis might affect the prognosis in patients with systemic sclerosis so actively diagnosing and managing bronchiectasis would be of paramount importance [36].
Our study provides two relevant considerations for clinicians and researchers. First, an increased risk of bronchiectasis in individuals with systemic sclerosis suggests that bronchiectasis should be regarded as an important pulmonary comorbidity along with ILD and pulmonary hypertension. Early screening strategies to detect bronchiectasis might be helpful, especially in those at an early age, who are at a higher risk of developing bronchiectasis compared to controls. Second, the increased risk of bronchiectasis in systemic sclerosis warrants future studies on the relationship between the two diseases: studies focusing on whether bronchiectasis affects the natural course of systemic sclerosis. If so, management of bronchiectasis to modulate the treatment outcomes of systemic sclerosis is needed.
This study has some limitations. First, since this study was conducted in a Korean population, it may be difficult to generalize the study results to other countries and ethnic groups. Second, as the NHIS database does not contain specific data on smoking history, body mass index, lung function test, type of systemic sclerosis (limited vs. diffuse), related symptoms, and use of immunosuppressants, we could not include these factors in our analysis. Third, bronchiectasis was determined using ICD-10 codes. Thus, this study captured only bronchiectasis cases that were of sufficient clinical significance to lead clinicians to claim diagnostic codes for bronchiectasis, which implies an underestimation of the incidence estimates. Fourth, traction bronchiectasis associated with ILD might have been included as bronchiectasis in this study. However, sensitivity analysis evaluating the risk of bronchiectasis without a diagnosis code for ILD (ICD-10 code for bronchiectasis, but without ICD-10 code for ILD) showed similar results (Supplementary Tables 1–2 and Supplementary Fig. 1). Finally, our study had a relatively short follow-up period, which may have led to underestimation of the true incidence of bronchiectasis in patients with systemic sclerosis.
Conclusions
A nationwide longitudinal database demonstrated that the risk of incident bronchiectasis is higher in individuals with systemic sclerosis than in those without. Because pulmonary complications play a major role in deciding mortality in patients with systemic sclerosis, clinicians need to identify and appropriately manage bronchiectasis in this population, particularly in younger people. Follow-up studies are needed to investigate how bronchiectasis in patients with systemic sclerosis affects the risk of infection, lung function, and quality of life.
Availability of data and materials
All data extracted in this study are included in the current article.
Abbreviations
- ILD:
-
Interstitial lung disease
- NHIS:
-
National Health Insurance Service
- ICD:
-
International Classification of Disease
- CTD:
-
Connective tissue disease
- COPD:
-
Chronic obstructive pulmonary disease
- SD:
-
Standard deviation
- CI:
-
Confidence interval
References
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA Jr, Rowell N, Wollheim F. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol. 1988;15(2):202–5.
Abu-Shakra M, Lee P. Mortality in systemic sclerosis: a comparison with the general population. J Rheumatol. 1995;22(11):2100–2.
Wigley FM, Lima JA, Mayes M, McLain D, Chapin JL, Ward-Able C. The prevalence of undiagnosed pulmonary arterial hypertension in subjects with connective tissue disease at the secondary health care level of community-based rheumatologists (the UNCOVER study). Arthritis Rheum. 2005;52(7):2125–32.
Steen VD, Conte C, Owens GR, Medsger TA Jr. Severe restrictive lung disease in systemic sclerosis. Arthritis Rheum. 1994;37(9):1283–9.
Mathai SC, Hummers LK, Champion HC, Wigley FM, Zaiman A, Hassoun PM, Girgis RE. Survival in pulmonary hypertension associated with the scleroderma spectrum of diseases: impact of interstitial lung disease. Arthritis Rheum. 2009;60(2):569–77.
Ioannidis JP, Vlachoyiannopoulos PG, Haidich AB, Medsger TA Jr, Lucas M, Michet CJ, Kuwana M, Yasuoka H, van den Hoogen F, Te Boome L, et al. Mortality in systemic sclerosis: an international meta-analysis of individual patient data. Am J Med. 2005;118(1):2–10.
Steen V. Predictors of end stage lung disease in systemic sclerosis. Ann Rheum Dis. 2003;62(2):97–9.
Chalmers JD, Chang AB, Chotirmall SH, Dhar R, McShane PJ. Bronchiectasis. Nat Rev Dis Primers. 2018;4(1):45.
Smith R, Harrison M, Lam KV, Adler B, Bulsara M, Sahhar J, Stevens W, Proudman S, Nikpour M, Gabbay E. The emerging association between bronchiectasis and systemic sclerosis: assessing prevalence and potential causality. Intern Med J. 2023;53(7):1204–11.
Andonopoulos AP, Yarmenitis S, Georgiou P, Bounas A, Vlahanastasi C. Bronchiectasis in systemic sclerosis. A study using high resolution computed tomography. Clin Exp Rheumatol. 2001;19(2):187–90.
Phung S, Strange G, Chung LP, Leong J, Dalton B, Roddy J, Deague J, Playford D, Musk M, Gabbay E. Prevalence of pulmonary arterial hypertension in an Australian scleroderma population: screening allows for earlier diagnosis. Intern Med J. 2009;39(10):682–91.
Choi H, Yang B, Kim YJ, Sin S, Jo YS, Kim Y, Park HY, Ra SW, Oh YM, Chung SJ, et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci Rep. 2021;11(1):7126.
Duarte AC, Porter J, Leandro MJ. Bronchiectasis in rheumatoid arthritis. A clinical appraisial. Joint Bone Spine. 2020;87(5):419–24.
De Soyza A, McDonnell MJ, Goeminne PC, Aliberti S, Lonni S, Davison J, Dupont LJ, Fardon TC, Rutherford RM, Hill AT, et al. Bronchiectasis rheumatoid overlap syndrome is an independent risk factor for mortality in patients with bronchiectasis: a multicenter cohort study. Chest. 2017;151(6):1247–54.
Shin DW, Cho J, Park JH, Cho B. National General Health Screening Program in Korea: history, current status, and future direction a scoping review. Precis Future Med. 2022;6(1):9–31.
Choi H, Park HY, Han K, Yoo J, Shin SH, Yang B, Kim Y, Park TS, Park DW, Moon JY, et al. Non-cystic fibrosis bronchiectasis increases the risk of lung cancer independent of smoking status. Ann Am Thorac Soc. 2022;19(9):1551–60.
Lee KA, Kim J, Choi W, Kim HS, Seo GH. Pregnancy-associated risk factors and incidence of systemic sclerosis in primiparous women: a nationwide population-based cohort study. Mod Rheumatol. 2022;32(1):149–54.
Choi H, Han K, Jung JH, Park SH, Kim SH, Kang HK, Sohn JW, Shin DW, Lee H. Long-term mortality of tuberculosis survivors in Korea: a population-based longitudinal study. Clin Infect Dis. 2023;76(3):e973–e981. https://doi.org/10.1093/cid/ciac411.
Choi H, Yang B, Nam H, Kyoung DS, Sim YS, Park HY, Lee JS, Lee SW, Oh YM, Ra SW, et al. Population-based prevalence of bronchiectasis and associated comorbidities in South Korea. Eur Respir J. 2019;54(2):1900194.
Yang B, Ryu J, Kim T, Jo YS, Kim Y, Park HY, Kang YA, Lee SJ, Lee OJ, Moon JY, et al. Impact of bronchiectasis on incident nontuberculous mycobacterial pulmonary disease: a 10-year national cohort study. Chest. 2021;159(5):1807–11.
Choi H, Kim SH, Han K, Park TS, Park DW, Moon JY, Kim SH, Kim TH, Sohn JW, Yoon HJ, et al. Association between exercise and risk of cardiovascular diseases in patients with non-cystic fibrosis bronchiectasis. Respir Res. 2022;23(1):288.
Lee H, Ryu J, Nam E, Chung SJ, Yeo Y, Park DW, Park TS, Moon JY, Kim TH, Sohn JW, et al. Increased mortality in patients with corticosteroid-dependent asthma: a nationwide population-based study. Eur Respir J. 2019;54(5):1900804.
Lee HR, Yoo JE, Choi H, Han K, Jung JH, Park J, Lee H, Shin DW. Tuberculosis and risk of ischemic stroke: a nationwide cohort study. Stroke. 2022;53(11):3401–9.
Lee HR, Yoo JE, Choi H, Han K, Lim YH, Lee H, Shin DW. Tuberculosis and the risk of ischemic heart disease: a nationwide cohort study. Clin Infect Dis. 2023;76(9):1576–84. https://doi.org/10.1093/cid/ciac946.
Choi H, Han K, Yang B, Shin DW, Sohn JW, Lee H. Female reproductive factors and incidence of nontuberculous mycobacterial pulmonary disease among postmenopausal women in Korea. Clin Infect Dis. 2022;75(8):1397–404.
Kirby DF, Chatterjee S. Evaluation and management of gastrointestinal manifestations in scleroderma. Curr Opin Rheumatol. 2014;26(6):621–9.
McFarlane IM, Bhamra MS, Kreps A, Iqbal S, Al-Ani F, Saladini-Aponte C, Grant C, Singh S, Awwal K, Koci K, et al. Gastrointestinal manifestations of systemic sclerosis. Rheumatology (Sunnyvale). 2018;8(1):235.
Farrokh D, Abbasi B, Fallah-Rastegar Y, Mirfeizi Z. The extrapulmonary manifestations of systemic sclerosis on chest high resolution computed tomography. Tanaffos. 2015;14(3):193–200.
Milliron B, Henry TS, Veeraraghavan S, Little BP. Bronchiectasis: mechanisms and imaging clues of associated common and uncommon diseases. Radiographics. 2015;35(4):1011–30.
Attar SM, Alamoudi OS, Aldabbag AA. Prevalence and risk factors of asymptomatic bronchiectasis in patients with rheumatoid arthritis at a tertiary care center in Saudi Arabia. Ann Thorac Med. 2015;10(3):176–80.
Duarte AC, Porter JC, Leandro MJ. The lung in a cohort of rheumatoid arthritis patients-an overview of different types of involvement and treatment. Rheumatology (Oxford). 2019;58(11):2031–8.
Zrour SH, Touzi M, Bejia I, Golli M, Rouatbi N, Sakly N, Younes M, Tabka Z, Bergaoui N. Correlations between high-resolution computed tomography of the chest and clinical function in patients with rheumatoid arthritis. Prospective study in 75 patients. Joint Bone Spine. 2005;72(1):41–7.
Lee H, Choi H, Chalmers JD, Dhar R, Nguyen TQ, Visser SK, Morgan LC, Oh YM. Characteristics of bronchiectasis in Korea: first data from the Korean Multicentre Bronchiectasis Audit and Research Collaboration registry and comparison with other international registries. Respirology (Carlton, VIC). 2021;26(6):619–21.
Lavie F, Rozenberg S, Coutaux A, Koeger AC, Bourgeois P, Fautrel B. Bronchiectasis in a patient with CREST syndrome. Joint Bone Spine. 2002;69(5):515–8.
Geri G, Dadoun S, Bui T, Del Castillo PN, Paternotte S, Dougados M, Gossec L. Risk of infections in bronchiectasis during disease-modifying treatment and biologics for rheumatic diseases. BMC Infect Dis. 2011;11:304.
Choi H, Chalmers JD. Bronchiectasis exacerbation: a narrative review of causes, risk factors, management and prevention. Ann Transl Med. 2022;11(1):25.
Acknowledgements
This study was performed using the National Health Insurance System database, and the results do not necessarily represent the opinions of the National Health Insurance Service.
Funding
This work was supported by grants from the National Research Foundation (NRF) of Korea (No. 2020R1A5A2017476). Also, this work was supported by the NRF grant funded by the Korean government (MSIT) (No. 2022R1F1A1074749 to B.Y.) and the Korean Ministry of Education (No. 2021R1I1A3052416 to H.C.). The funders had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.C. and H.L. are the guarantors of the manuscript and takes responsibility for the content of the manuscript, including the data and analysis. K.H., H.C., and H.L. contributed to the conception and design of the study. B.Y., B.-G.K., K.H., J.-H.J., J.H.K., D.W.P., S.-H.K., E.-G.K., J.W.S., H.J.Y., H.C, and H.L. were involved in the collection and interpretation of the data. K.H. and J.-H.J. were involved in the statistical analyses. B.Y. and B.-G.K. were a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of the Chungbuk National University Hospital (application no. 2023-01-014). The requirement for informed consent was waived because the NHIS database uses an anonymous patient identification system.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Figure S1.
Cumulative incidence probability of bronchiectasis (/100,000 person-years) in systemic sclerosis and matched cohorts excluding ILD diagnosis codes. Supplemental Table S1. Baseline characteristics in systemic sclerosis and matched cohorts excluding ILD diagnosis codes. Supplemental Table S2. Risk of bronchiectasis according to the presence or absence of systemic sclerosis excluding ILD diagnosis codes. Supplemental Table S3. Subgroup analysis of the risk of bronchiectasis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, B., Kim, BG., Han, K. et al. Systemic sclerosis and risk of bronchiectasis: a nationwide longitudinal cohort study. Arthritis Res Ther 25, 209 (2023). https://doi.org/10.1186/s13075-023-03189-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-023-03189-2