Abstract
Background
We examined the association between levothyroxine use and longitudinal MRI biomarkers for thigh muscle mass and composition in at-risk participants for knee osteoarthritis (KOA) and their mediatory role in subsequent KOA incidence.
Methods
Using the Osteoarthritis Initiative (OAI) data, we included the thighs and corresponding knees of participants at risk but without established radiographic KOA (baseline Kellgren-Lawrence grade (KL) < 2). Levothyroxine users were defined as self-reported use at all annual follow-up visits until the 4th year and were matched with levothyroxine non-users for potential confounders (KOA risk factors, comorbidities, and relevant medications covariates) using 1:2/3 propensity score (PS) matching. Using a previously developed and validated deep learning method for thigh segmentation, we assessed the association between levothyroxine use and 4-year longitudinal changes in muscle mass, including cross-sectional area (CSA) and muscle composition biomarkers including intra-MAT (within-muscle fat), contractile percentage (non-fat muscle CSA/total muscle CSA), and specific force (force per CSA). We further assessed whether levothyroxine use is associated with an 8-year risk of standard KOA radiographic (KL ≥ 2) and symptomatic incidence (incidence of radiographic KOA and pain on most of the days in the past 12 months). Finally, using a mediation analysis, we assessed whether the association between levothyroxine use and KOA incidence is mediated via muscle changes.
Results
We included 1043 matched thighs/knees (266:777 levothyroxine users:non-users; average ± SD age: 61 ± 9 years, female/male: 4). Levothyroxine use was associated with decreased quadriceps CSAs (mean difference, 95%CI: − 16.06 mm2/year, − 26.70 to − 5.41) but not thigh muscles’ composition (e.g., intra-MAT). Levothyroxine use was also associated with an increased 8-year risk of radiographic (hazard ratio (HR), 95%CI: 1.78, 1.15–2.75) and symptomatic KOA incidence (HR, 95%CI: 1.93, 1.19–3.13). Mediation analysis showed that a decrease in quadriceps mass (i.e., CSA) partially mediated the increased risk of KOA incidence associated with levothyroxine use.
Conclusions
Our exploratory analyses suggest that levothyroxine use may be associated with loss of quadriceps muscle mass, which may also partially mediate the increased risk of subsequent KOA incidence. Study interpretation should consider underlying thyroid function as a potential confounder or effect modifier. Therefore, future studies are warranted to investigate the underlying thyroid function biomarkers for longitudinal changes in the thigh muscles.
Similar content being viewed by others
Background
Levothyroxine, the primary treatment for hypothyroidism, prescribed for more than 7% of Americans, is one of the most commonly used medications in the USA [1]. In a recent report using administrative claims data, among levothyroxine users with available thyroid function test results, 30% initiated the therapy for normal thyroid function and 60% for subclinical hypothyroidism [2]. Using a dual-energy X-ray analysis scan, previous work has shown an association between levothyroxine therapy and changes in body composition primarily via a decrease in muscle and lean body mass but not fat or bone mass [3]. In addition to levothyroxine use, the underlying thyroid dysfunction, as a potential confounder or effect modifier, can be associated with a wide range of muscle impairments such as myalgia, fatigability, proximal myopathy, myxoedema, or even rhabdomyolysis [4]. Changes in thigh muscle composition in the setting of levothyroxine therapy can be significant in elderly adults, who are also at risk of KOA, in which thigh muscle dysfunction is reported as an independent risk factor for KOA incidence [5]. This is important in clinical practice since thigh muscle degeneration is known as a modifiable risk factor for KOA incidence [5, 6] that can be mitigated by using specific training interventions and neuromuscular exercises [7, 8].
No prior work has investigated the association between levothyroxine use and thigh muscles’ volume and function. MRI is recognized as a valuable tool for the precise assessment of thigh muscle changes in various metabolic and non-metabolic settings [9,10,11,12,13]. However, studies on thyroid dysfunction-associated changes in the thigh muscles using MRI have been limited to only case reports [14, 15]. Moreover, no prior study has assessed whether thyroid dysfunction or levothyroxine use-associated changes in the thigh muscles are associated with an increased risk of KOA incidence in an at-risk population such as the Osteoarthritis Initiative (OAI) cohort.
Using a longitudinal propensity score (PS)-matched sample of participants at risk of KOA, in this exploratory study, we determined the longitudinal changes in thigh muscle size and composition and their potential association with levothyroxine use. Furthermore, we investigated whether levothyroxine use is associated with subsequent radiographic and symptomatic KOA incidence. Finally, we explored the mediatory role of these muscle biomarkers in the potential association between levothyroxine use and KOA incidence. If successfully concluded, interventions like levothyroxine dose adjustments or specific exercises aiming at the thigh muscles might be found clinically useful in modifying thigh muscle quality and subsequently in reducing the rate of KOA incidence.
Methods
Study participants
The data of this longitudinal observational study was obtained from the OAI cohort, which studied 4796 women and men 45–79 years of age from all ethnic groups in four clinical centers and a data coordinating center (2004–2015 clinicaltrials.gov registration code: NCT00080171). Provided with a complete explanation of the procedures and purposes of the study, all enrolled participants gave written informed consent. The protocol of the OAI cohort has been approved by the ethics review boards of all OAI collaborating centers (approval code: 10-00532) [16]. OAI study excludes participants with either inflammatory arthropathies, bilateral end-stage KOA, ambulatory aids other than a single straight cane, positive pregnancy tests, and contraindications to MRI (https://nda.nih.gov/oai/study-details). OAI participants were recruited in three cohorts of progression (cohort with KOA at baseline), incidence (cohort without KOA at baseline but exposed to risk factors), and non-exposed (cohort without KOA and its risk factors at baseline).
In this study, we further excluded participants from OAI non-exposed cohort due to the minimal risk of KOA incidence. We included the knees from the incident cohort and only the knees without radiographic KOA (semi-quantitative Kellgren-Lawrence grade (KL) < 2; the radiographs were from the knees at a fixed-flexion position) [17] in participants with unilateral OA from the progression cohort. The knees with established radiographic KOA at baseline (KL ≥ 2), unavailable KL grading, or KOA outcomes were excluded. In addition, the thighs (and corresponding knees) of participants without available baseline or 2nd- or 4th-year follow-up MRIs or with unacceptable image quality (visually assessed by two trained readers) were excluded (Fig. 1). The naming and version of the OAI dataset files used in the current study can be found in Additional file 1: Table S1.
Exposure definition and propensity score matching
According to OAI protocol, participants brought their medications with them at baseline and annual visits. The use of levothyroxine was assessed at baseline and annual follow-up visits until year 4 of the OAI cohort, and levothyroxine use was defined as use at baseline and all annual visits while non-use was defined as no history of use during the 4-year follow-up. Non-adherent levothyroxine users in either baseline to 4th-year visits were excluded. The knees (and corresponding thighs) of levothyroxine users and non-users were matched for an exhaustive list of potential confounders, including demographic characteristics, comorbidities, risk factors, and medications (listed in Table 1 and Additional file 1: Appendix 1). After evaluating the missing data pattern in confounding variables using Little’s test [18], we implemented the multiple imputation method to estimate missing values (< 2.8% of data in each variable, Additional file 1: Table S2) since this method is associated with less biased estimates in comparison with excluding the missing data [19]. Next, the knees/thighs of participants were assigned to two matched groups of levothyroxine users and non-users, using the 1:2/3 PS-matching method on the imputed dataset (logistic regression and the nearest-neighbor matching methods). The groups were considered matched for a confounding variable as far as the standardized mean difference (SMD) between the groups for that variable was < 0.1 (Table 1).
Quantitative thigh muscle MRI biomarkers of size and composition
3T MRI systems (Trio, Siemens Healthcare) were used to acquire 15 continuous axial T1-weighted images from a specific region of thighs, initiating 10 cm proximal to the distal femoral epiphysis [16]. Due to the possible variation in the site of axial images between participants with different thigh lengths, an image was selected from the region of interest (ROI), which is the 33% distal length of the femur bone, based on previous studies on the OAI dataset [20, 21]. Normalization and field inhomogeneity correction was performed for the selected images using the N4ITK method [22], and a fully automated supervised deep learning algorithm was trained and validated on the images to segment all available axial thigh images in the OAI dataset [23].
Quantitative biomarkers were used to evaluate the longitudinal changes in the thigh muscles’ size and composition. MRI markers of thigh muscles’ size included the cross-sectional area (CSA) for the total and each thigh muscle group (quadriceps, flexors, adductors, and sartorius). The composition was assessed using intra-muscular adipose tissue (intra-MAT, adipose tissue inside the thigh muscles) and contractile percentage (measured by dividing the CSA of the fat-free area of the muscle by the total muscle’s CSA). Using the ImageJ software, a validated Otsu intensity thresholding method was performed on the T1-weighted images [24, 25], and the intra-MAT was calculated (in pixels) using the sum of fat-containing (white) pixels inside the muscle segments and multiplied by pixel area (mm2) (Additional file 1: Fig. S1). We further calculated the specific contractile force as the force generated by muscle per area unit. Participants completed isometric knee extension and flexion maximum voluntary contractions using the “Good Strength Chair” apparatus (Metitur, Jyväskylä, Finland) three times [26, 27]. The highest force of the three measurements represented the contractile force for each thigh (measured in newtons or N). The specific contractile force was calculated by dividing the maximal isometric extensor and flexor strength of the thighs by thigh muscle CSA [28]. The outcome variables are listed in Table 1.
KOA incidence outcomes
KOA outcomes were radiographic and symptomatic KOA incidence in follow-up in participants with baseline KL grade < 2. First, we defined KOA incidence as a knee with KL grade 0 or 1 (no KOA) at baseline that developed radiographic KL grade ≥ 2 during the 8 years of the follow-up period [29]. Similar to previous studies on the OAI dataset [30, 31], symptomatic KOA incidence was defined as the incidence of both of the following (1) radiographic incidence of KOA and (2) frequent knee symptoms in the past 12 months, defined as “pain, aching, or stiffness in or around the knee on most days” for at least 1 month during the past 12 months.
Statistical analysis
Statistical data analysis was performed using the R software version 4.0.3 (packages: haven, MatchIt, mice, survival, lme4, lmerTest, mediation, and tableone). Multilevel linear mixed-effect regression models were used to compare 4-year changes in the thigh muscle markers between levothyroxine users and non-users while considering random intercept and slope for each matched cluster of thighs of levothyroxine users: non-users and a random intercept for within-subject similarities (due to the inclusion of knees/thighs of both sides). Interaction of the time and levothyroxine use was defined as the independent predictor, while MRI biomarkers of thigh muscle size and composition were the dependent outcomes. Assumptions of regression models, including homoscedasticity, exogeneity, linearity, and normal distribution of data and residuals, were assessed and confirmed.
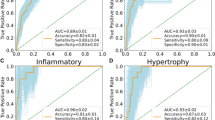
KOA outcomes were assessed using survival analysis, with levothyroxine use as the independent variable and KOA radiographic and symptomatic incidence as dependent outcomes; the Cox proportional hazard model (meeting the linearity and influential observations assumptions) over 8 years was used, and the results were reported as hazard ratio (HR) and 95% confidence intervals (CI). Finally, we used mediation analysis with 1000 Monte Carlo draws for non-parametric bootstrap approximation to evaluate whether the changes in the thigh muscles have a mediatory role in the association between levothyroxine use and KOA incidence (Fig. 2).
Causal mediation analysis. We evaluated the mediatory role (i.e., intermediary variable) of changes in the quantitative muscle markers of the thigh (baseline to 4th year) for the association between levothyroxine use (i.e., exposure variable) and incidence of KOA (baseline to 8th year) (i.e., outcome variable). KOA, knee osteoarthritis
The false discovery rate (FDR) method was used to correct p-values for errors related to multiple comparisons. Differences with a two-tailed FDR-corrected p-value below 0.05 were considered statistically significant.
To test the robustness of the results, as the sensitivity analysis, we also performed similar PS-matched analyses on all levothyroxine users, including non-adherent users from baseline to 4th-year visit (sensitivity analysis in Fig. 1).
Results
Baseline characteristics of participants
As depicted in Fig. 1, the knees of thighs without quality baseline or follow-up (2nd- or 4th-year) thigh MRI (n: 3748), with baseline KOA (KL ≥ 2, n: 2524), missing baseline KL grade or KOA outcomes (n:335), from non-exposed OAI cohort (n: 20), and/or of participants non-adherent to levothyroxine use during baseline to 4th-year visit (n: 113) were excluded. After 1:2/3 PS-matching, from a total of 2852 knees/thighs, 1043 were included (266:777 levothyroxine users:non-users) (Fig. 1). No statistical imbalance was found in covariates (SMDs < 0.1) following the PS matching (Table 1). More importantly, there was no significant difference in baseline biomarkers of thigh muscle MRI between the PS-matched study groups.
The association between levothyroxine use and 4-year change in thigh muscles
Linear mixed-effect regression models showed that levothyroxine use is associated with a significant decrease in quadriceps CSA (mean difference/year, 95%CI: − 16.06 mm2/year, − 26.70 to − 5.41) and total thigh muscles CSA (− 22.23 mm2/year, − 40.25 to − 4.21, Table 2). Only the results of quadriceps CSA remained significant after FDR correction. As also shown in the table, the rest of the thigh muscle markers were not associated with levothyroxine use (FDR corrected p values > 0.05).
The association between levothyroxine use and 8-year risk of KOA incidence
Levothyroxine use was associated with an increased risk of radiographic KOA incidence (HR, 95%CI: 1.78, 1.15–2.75). Levothyroxine use was also associated with an increased risk of symptomatic KOA incidence (1.93, 1.19–3.13) (Table 3).
Mediatory role of thigh muscle changes in the association between levothyroxine use and KOA incidence
Using mediation analysis on thigh muscle markers that had shown an association with levothyroxine use (i.e., quadriceps CSA and total thigh muscles CSA), we observed that 4-year changes of quadriceps CSA partially mediated the association between levothyroxine use and increased radiographic (β estimate, 95%CI: 0.58, 0.21–1.05) and symptomatic (0.35, 0.14–0.60) KOA incidence risk (Table 4).
Sensitivity analysis
Sensitivity analysis indicated that the results were not sensitive to including non-adherent levothyroxine users with levothyroxine use in either baseline to 4th-year annual visits. However, the effect sizes in all analyses were comparatively smaller (Additional file 1: Table S3).
Discussion
In this exploratory study, using a propensity score-matched design on a large sample of participants at risk of KOA, we found that levothyroxine use may be associated with a longitudinal decrease in quadriceps muscle size but not changes in their composition. In addition, participants with levothyroxine use also exhibited an increased risk of KOA incidence, partially mediated by the loss of quadriceps muscle mass, observed as a reduction in its CSA. The fact that there was no significant imbalance between MRI muscle biomarkers of levothyroxine users and non-users at baseline reduces the risk of selection bias and reinforces that the observed longitudinal changes were associated with levothyroxine use and not heterogeneity between study cohorts’ characteristics at baseline. Besides, even though the effects of potential covariates on the study results were minimized using the PS-matching method, there was a considerable heterogeneity in some of these variables such as gender and race, which necessitates further research works stratifying the participants based on these variables and studying the levothyroxine use-associated changes in each subgroup. Due to the exploratory nature of this study, the reported results cannot be interpreted as causal inferences and should be interpreted with caution as the underlying thyroid function status can play a potential role as a confounder or effect modifier for the association in this observational study.
OAI cohort provides a unique and robust database with a large sample size, long-term follow-up, a detailed list of confounders, and various demographic, clinical, and ancillary data. Given the availability of the prospectively designed optimized MRI protocol for skeletal muscle and adipose tissue segmentation [16], we developed a fully automated deep learning model of thigh segmentation to include all eligible participants in the analyses, used the PS-matching method to minimize potential confounding bias, and performed sensitivity to assess the robustness of our results.
The pathogenesis of muscle changes in patients with levothyroxine use has been only sparsely investigated [3]. Thyroid hormones are a major regulator of glucose metabolism and oxidative phosphorylation [32, 33], muscle units’ function and plasticity, and connective tissue metabolism [34], and clinical overt thyroid dysfunction has a known association with generalized myopathy. More importantly, in accordance with our findings, while loss of quadriceps muscle mass was observed, there was minimal fat infiltration and adipose changes in the muscle [35].
In addition to muscle changes, only a few case series and cross-sectional studies have investigated the association between thyroid dysfunction and KOA [36,37,38], and no prior study has focused on levothyroxine use and KOA outcomes. The overall results have also been inconclusive, probably due to incomplete adjustment of potential confounders, small sample size, and heterogeneity of the target population considering OA risk factors [36, 39, 40]. This longitudinal exploratory study aimed to test the hypothesis for the potential “levothyroxine use-loss of quadriceps muscle mass-KOA incidence” pathophysiological pathway. However, any causal interpretation is limited by the study design and the lack of available data on thyroid function as the potential confounder or effect modifier in the OAI database. The quadriceps muscles stabilize the knee joint during weight-bearing; therefore, its changes can be considered an independent risk factor for knee joint OA incidence [41,42,43]. Besides, as the mediatory role of loss of quadriceps muscle mass on KOA incidence was partial, there are other mechanisms mediating levothyroxine use and the KOA association. Previous experimental studies of KOA have shown the essential role of thyroid hormone signaling in the modulation of subchondral bone [44, 45], articular cartilage [46], and synovial fibroblasts [47]. Therefore, further exploration of several alternative mechanisms can help better delineate this suggested association pathophysiological pathway.
Using thigh MRI biomarkers of size and composition, for the first time, we showed levothyroxine use is associated with loss of quadriceps muscle mass. This finding bolds thigh MRI as a precise measurement tool for detecting early and subtle muscle changes. Even though the loss of quadriceps muscle mass was not accompanied by the changes in muscle composition, its association had a mediatory role in the increased KOA incidence risk associated with levothyroxine use. If adequately detected, the levothyroxine use-associated changes in quadriceps muscle mass may be potentially modifiable through levothyroxine dose adjustments or specific exercises and interventions aiming at the thigh muscles. Future trials are needed to assess the causal role of thigh muscle changes in this mediation.
This exploratory observational study has several limitations. First and perhaps most importantly, thyroid function assessments (e.g., serum TSH and thyroid hormone levels, thyroid iodine uptake) are not available in the OAI cohort. Therefore, we can not delineate the detailed association between underlying thyroid dysfunction and muscle degeneration in levothyroxine users. Thus, the study interpretation should consider underlying thyroid function as a potential confounder or effect modifier. This limitation needs to be addressed in future studies. Second, the OAI dataset is designed and longitudinally collected to assess the association between clinical, imaging, or laboratory-based measurements and KOA development and progression. Therefore, the OAI selection criteria are not specifically designed for subjects with thyroid dysfunction, and post hoc analyses on this dataset may be inherently susceptible to selection bias. We tried to address this possible non-random subject selection using comprehensive PS matching for potential confounders. Third, even though the physical activity scale for the elderly (PASE) is primarily designed for older adults, we also used it for participants of younger ages. This is due to the fact that numerous prior studies have confirmed the utility of the PASE in younger adults [48,49,50,51], and the OAI cohort provides the PASE scale score for all participants regardless of age. Finally, considering the absence of 3D volumetric assessments in the OAI data, we conducted a thigh MRI on a specific anatomical location at 33% distal length of the femur bone. While the exact MRI interpretation of the thigh was not feasible at other levels, previous studies have shown that muscle CSAs calculated at this level are strongly correlated with 3D muscle volume and can appropriately detect anatomical variations, cross-sectional differences, and longitudinal changes [21, 52, 53].
Conclusions
This study showed that levothyroxine use may be associated with loss of quadriceps muscle mass which may also partially mediate the increased risk of KOA radiographic and symptomatic incidence in these participants. Further trials and prospectively designed observational studies are certainly warranted to assess the role of underlying thyroid function as a potential confounder or effect modifier on muscle changes and KOA risk. Such studies are important since levothyroxine users may benefit from clinical examinations, prescription modification, and simple preventative measures aiming at mitigating loss of muscle mass and KOA.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CSA:
-
Cross-sectional area
- HR:
-
Hazard ratio
- inter-MAT:
-
Inter-muscular adipose tissue
- intra-MAT:
-
Intra-muscular adipose tissue
- JSN:
-
Joint space narrowing
- KL:
-
Kellgren-Lawrence
- KOA:
-
Knee osteoarthritis
- NASS:
-
Non-acceptable symptomatic state
- OAI:
-
Osteoarthritis Initiative
- PASE:
-
Physical activity scale for the elderly
- PS:
-
Propensity score
- SMD:
-
Standardized mean difference
References
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818–30.
Brito JP, Ross JS, El Kawkgi OM, Maraka S, Deng Y, Shah ND, et al. Levothyroxine use in the United States, 2008-2018. JAMA Intern Med. 2021;181(10):1402–5.
Karmisholt J, Andersen S, Laurberg P. Weight loss after therapy of hypothyroidism is mainly caused by excretion of excess body water associated with myxoedema. J Clin Endocrinol Metab. 2011;96(1):E99–103.
Sindoni A, Rodolico C, Pappalardo MA, Portaro S, Benvenga S. Hypothyroid myopathy: a peculiar clinical presentation of thyroid failure. Review of the literature. Rev Endocr Metab Disord. 2016;17(4):499–519.
Teichtahl AJ, Wluka AE, Wang Y, Wijethilake PN, Strauss BJ, Proietto J, et al. Vastus medialis fat infiltration - a modifiable determinant of knee cartilage loss. Osteoarthr Cartil. 2015;23(12):2150–7.
Raynauld J-P, Pelletier J-P, Roubille C, Dorais M, Abram F, Li W, et al. Magnetic resonance imaging–assessed vastus medialis muscle fat content and risk for knee osteoarthritis progression: relevance from a clinical trial. Arthritis Care Res. 2015;67(10):1406–15.
de Almeida AC, Aily JB, Pedroso MG, Gonçalves GH, de Carvalho FJ, Ferrari RJ, et al. A periodized training attenuates thigh intermuscular fat and improves muscle quality in patients with knee osteoarthritis: results from a randomized controlled trial. Clin Rheumatol. 2020;39(4):1265–75.
Ageberg E, Roos EM. Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015;43(1):14–22.
Zheng Y, Liu L, Wang L, Xiao J, Wang Z, Lv H, et al. Magnetic resonance imaging changes of thigh muscles in myopathy with antibodies to signal recognition particle. Rheumatology. 2014;54(6):1017–24.
Thierfelder KM, Gerhardt JS, Gemescu IN, Notohamiprodjo S, Rehnitz C, Weber M-A. Imaging of hip and thigh muscle injury: a pictorial review. Insights Imaging. 2019;10(1):20.
Smitaman E, Flores DV, Gómez CM, Pathria MN. MR imaging of atraumatic muscle disorders. Radiographics. 2018;38(2):500–22.
Hilton TN, Tuttle LJ, Bohnert KL, Mueller MJ, Sinacore DR. Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Phys Ther. 2008;88(11):1336–44.
Modesto AE, Ko J, Stuart CE, Bharmal SH, Cho J, Petrov MS. Reduced skeletal muscle volume and increased skeletal muscle fat deposition characterize diabetes in individuals after pancreatitis: a magnetic resonance imaging study. Diseases (Basel, Switzerland). 2020;8(3):25.
Chung J, Ahn KS, Kang CH, Hong SJ, Kim BH. Hoffmann’s disease: MR imaging of hypothyroid myopathy. Skelet Radiol. 2015;44(11):1701–4.
Nalini A, Govindaraju C, Kalra P, Kadukar P. Hoffmann’s syndrome with unusually long duration: report on clinical, laboratory and muscle imaging findings in two cases. Ann Indian Acad Neurol. 2014;17(2):217–21.
Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage. 2008;16(12):1433–41.
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M, et al. Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behaviour disorder: an observational cohort study. Lancet Neurol. 2013;12(5):443–53.
Li C. Little’s test of missing completely at random. Stata J. 2013;13(4):795–809.
Donders AR, van der Heijden GJ, Stijnen T, Moons KG. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59(10):1087–91.
Kemnitz J, Wirth W, Eckstein F, Culvenor AG. The role of thigh muscle and adipose tissue in knee osteoarthritis progression in women: data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2018;26(9):1190–5.
Cotofana S, Hudelmaier M, Wirth W, Himmer M, Ring-Dimitriou S, Sänger AM, et al. Correlation between single-slice muscle anatomical cross-sectional area and muscle volume in thigh extensors, flexors and adductors of perimenopausal women. Eur J Appl Physiol. 2010;110(1):91–7.
Tustison NJ, Avants BB, Cook PA, Zheng Y, Egan A, Yushkevich PA, et al. N4ITK: improved N3 bias correction. IEEE Trans Med Imaging. 2010;29(6):1310–20.
Mohajer B, Dolatshahi M, Moradi K, Najafzadeh N, Eng J, Zikria B, et al. Role of thigh muscle changes in knee osteoarthritis outcomes: osteoarthritis initiative data. Radiology. 2022;305(1):169–78.
Ogier AC, Hostin MA, Bellemare ME, Bendahan D. Overview of MR image segmentation strategies in neuromuscular disorders. Front Neurol. 2021;12:625308.
Ahmad E, McPhee J, Degens H, Yap MH. Automatic segmentation of MRI human thigh muscles: combination of reliable and fast framework methods for quadriceps, femur and marrow segmentation. In: ICBET ‘18; 2018.
Rantanen T, Era P, Heikkinen E. Maximal isometric strength and mobility among 75-year-old men and women. Age Ageing. 1994;23(2):132–7.
Sattler M, Dannhauer T, Hudelmaier M, Wirth W, Sänger AM, Kwoh CK, et al. Side differences of thigh muscle cross-sectional areas and maximal isometric muscle force in bilateral knees with the same radiographic disease stage, but unilateral frequent pain - data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2012;20(6):532–40.
Culvenor AG, Felson DT, Niu J, Wirth W, Sattler M, Dannhauer T, et al. Thigh muscle specific-strength and the risk of incident knee osteoarthritis: the influence of sex and greater body mass index. Arthritis Care Res. 2017;69(8):1266–70.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502.
Riddle DL, Kong X, Jiranek WA. Two-year incidence and predictors of future knee arthroplasty in persons with symptomatic knee osteoarthritis: preliminary analysis of longitudinal data from the Osteoarthritis Initiative. Knee. 2009;16(6):494–500.
Laslett LL, Kingsbury SR, Hensor EMA, Bowes MA, Conaghan PG. Effect of bisphosphonate use in patients with symptomatic and radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. Ann Rheum Dis. 2014;73(5):824.
Clément K, Viguerie N, Diehn M, Alizadeh A, Barbe P, Thalamas C, et al. In vivo regulation of human skeletal muscle gene expression by thyroid hormone. Genome Res. 2002;12(2):281–91.
McDaniel HG, Pittman CS, Oh SJ, DiMauro S. Carbohydrate metabolism in hypothyroid myopathy. Metabolism. 1977;26(8):867–73.
Wład H, Fenrych W, Lacka K, Sikorska-Horst W. Urinary glycosaminoglycans in patients with hypothyroidism and in healthy subjects. J Clin Chem Clin Biochem. 1988;26(5):259–64.
Villar J, Finol HJ, Torres SH, Roschman-González A. Myopathy in patients with Hashimoto’s disease. Investig Clin. 2015;56(1):33–46.
McLean RM, Podell DN. Bone and joint manifestations of hypothyroidism. Semin Arthritis Rheum. 1995;24(4):282–90.
Becker KL, Ferguson RH, Mc CW. The connective-tissue diseases and symptoms associated with Hashimoto’s thyroiditis. N Engl J Med. 1963;268:277–80.
Tagoe CE, Zezon A, Khattri S. Rheumatic manifestations of autoimmune thyroid disease: the other autoimmune disease. J Rheumatol. 2012;39(6):1125–9.
Garg M, Aggarwal D. Bone and joint manifestations in 25 hypothyroidism patients: a case series. J Adv Med Dental Sci Res. 2021;9(3):127–9.
Tagoe CE, Wang W, Wang S, Barbour KE. Association of anti-thyroid antibodies with radiographic knee osteoarthritis and chondrocalcinosis: a NHANES III study. Ther Adv Musculoskelet Dis. 2021;13:1759720X211035199.
Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127(2):97–104.
Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthr Cartil. 2010;18(6):769–75.
Jefferson RJ, Collins JJ, Whittle MW, Radin EL, O’Connor JJ. The role of the quadriceps in controlling impulsive forces around heel strike. Proc Inst Mech Eng H. 1990;204(1):21–8.
Li L, Li M, Pang Y, Wang J, Wan Y, Zhu C, et al. Abnormal thyroid hormone receptor signaling in osteoarthritic osteoblasts regulates microangiogenesis in subchondral bone. Life Sci. 2019;239:116975.
Waung JA, Bassett JD, Williams GR. Adult mice lacking the type 2 iodothyronine deiodinase have increased subchondral bone but normal articular cartilage. Thyroid. 2015;25(3):269–77.
Williams GR. Thyroid hormone actions in cartilage and bone. Eur Thyroid J. 2013;2(1):3–13.
Pörings A-S, Lowin T, Dufner B, Grifka J, Straub RH. A thyroid hormone network exists in synovial fibroblasts of rheumatoid arthritis and osteoarthritis patients. Sci Rep. 2019;9(1):13235.
Felson DT, Niu J, Yang T, Torner J, Lewis CE, Aliabadi P, et al. Physical activity, alignment and knee osteoarthritis: data from MOST and the OAI. Osteoarthr Cartil. 2013;21(6):789–95.
Pignato M, Arbeeva L, Schwartz TA, Callahan LF, Cooke J, Golightly YM, et al. Level of participation in physical therapy or an internet-based exercise training program: associations with outcomes for patients with knee osteoarthritis. BMC Musculoskelet Disord. 2018;19(1):238.
Svege I, Kolle E, Risberg MA. Reliability and validity of the Physical Activity Scale for the Elderly (PASE) in patients with hip osteoarthritis. BMC Musculoskelet Disord. 2012;13(1):26.
Dunlop DD, Semanik P, Song J, Sharma L, Nevitt M, Jackson R, et al. Moving to maintain function in knee osteoarthritis: evidence from the Osteoarthritis Initiative. Arch Phys Med Rehabil. 2010;91(5):714–21.
Ruhdorfer A, Wirth W, Dannhauer T, Eckstein F. Longitudinal (4 year) change of thigh muscle and adipose tissue distribution in chronically painful vs painless knees – data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2015;23(8):1348–56.
Culvenor AG, Hamler FC, Kemnitz J, Wirth W, Eckstein F. Brief report: loss of muscle strength prior to knee replacement: a question of anatomic cross-sectional area or specific strength? Arthritis Rheum. 2018;70(2):222–9.
Acknowledgements
The Osteoarthritis Initiative, a collaborative project between public and private sectors, includes five contracts N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262. This project is conducted by the Osteoarthritis Initiative project investigators and is financially supported by the National Institutes of Health (NIH). Private funding partners are Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc.
In preparing this manuscript, Osteoarthritis Initiative project publicly available datasets were used. The results of this work do not necessarily reflect the opinions of the Osteoarthritis Initiative project investigators, the NIH, or the private funding partners.
Funding
This research was supported by the NIH National Institute on Aging (NIA) under Award Number P01AG066603 and the NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) under Award Number R01AR079620-01.
Author information
Authors and Affiliations
Contributions
Literature research was performed by B.M., K.M., J.M., D.J.H, F.W.R., A.G., S.D. Statistical analysis was performed by B.M., K.M., S.D. All authors participated in the study design, interpretation of results, and drafting the manuscript or critically revising it for relevant intellectual content. All authors approved final version of submitted manuscript and agreed to ensure any questions related to the work are appropriately resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The medical ethics review boards of the University of California, San Francisco (Approval Number: 10-00532) and the four clinical centers of the Osteoarthritis Initiative project recognized the project as Health Insurance Portability and Accountability Act (HIPAA)-compliant. Subjects have given informed consent before participating in the Osteoarthritis Initiative (OAI) project.
Consent for publication
Not applicable.
Competing interests
DJH is the co-director of the Sydney Musculoskeletal Health Flagship. In addition, DJH is the editor of the osteoarthritis section for UpToDate and co-Editor in Chief of Osteoarthritis and Cartilage. DJH provides consulting advice on scientific advisory boards for Pfizer, Lilly, TLCBio, Novartis, Tissuegene, and Biobone. AG reported receiving funding from Pfizer, TissueGene, Novartis, Medipost, Coval, TrialSpark, and ICM (for consultation), and Boston Imaging Core Lab, LLC (as the president and stockholder). SD reported that he received funding from Toshiba Medical Systems (for consultation) and grants from GERRAF and Carestream Health (for a clinical trial study). None of the authors has any conflicting personal or financial relationships that could have influenced the results of this study. Other authors declare that they did not have any competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Variables included in the propensity-score matching. The pattern of missing data Little’s test. Table S1. Osteoarthritis Initiative (OAI) datasets used in the study. Table S2. Percentage of missing data of the covariate included in the multiple imputations and PS-matching methods. Table S3.1. Baseline characteristics of participants assessed in the sensitivity analysis to inclusion of all levothyroxine users (both adherent and non-adherent users) before and after propensity score matching according to levothyroxine use. Table S3.2. Sensitivity to inclusion of all levothyroxine users (both adherent and non-adherent users) for longitudinal changes in thigh muscle markers between levothyroxine users and nonuser participants. Table S3.3. Sensitivity inclusion of all levothyroxine users (both adherent and non-adherent users) for the assessment of the association between levothyroxine use and risk of KOA incidence. Table S3.4. Sensitivity analysis on the inclusion of all levothyroxine users (both adherent and non-adherent users) for mediatory role of thigh muscle markers in the association between levothyroxine use and KOA incidence. Figure S1. Study outcome variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohajer, B., Moradi, K., Guermazi, A. et al. Levothyroxine use and longitudinal changes in thigh muscles in at-risk participants for knee osteoarthritis: preliminary analysis from Osteoarthritis Initiative cohort. Arthritis Res Ther 25, 58 (2023). https://doi.org/10.1186/s13075-023-03012-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-023-03012-y