Abstract
Background
A recent systematic review identified four candidate serum-soluble bone-turnover biomarkers (dickkopf-1, Dkk-1; macrophage-colony stimulating factor, M-CSF; matrix metalloproteinase-3, MMP-3; osteoprotegerin, OPG) showing possible association with psoriatic arthritis (PsA). We aimed to: (i) confirm and determine if these four biomarkers are associated with PsA; (ii) differentiate psoriasis cases with and without arthritis; and (iii) differentiate PsA cases with and without axial arthritis.
Methods
A prospective cross-sectional comparative two-centre study recruited 200 patients with psoriasis without arthritis (PsC), 127 with PsA without axial arthritis (pPsA), 117 with PsA with axial arthritis (psoriatic spondyloarthritis, PsSpA), 157 with ankylosing spondylitis (AS) without psoriasis, and 50 matched healthy controls (HC). Serum biomarker concentrations were measured using ELISA. Multivariable regression and receiver operating characteristic analyses were performed.
Results
MMP-3 concentrations were significantly higher and M-CSF significantly lower in each arthritis disease group compared with HC (p ≤ 0.02). MMP-3 concentrations were significantly higher (adjusted odds ratio, ORadj 1.02 per ng/ml increase in concentration; p = 0.0004) and M-CSF significantly lower (ORadj 0.44 per ng/ml increase; p = 0.01) in PsA (pPsA and PsSpA combined) compared with PsC. Dkk-1 concentrations were significantly higher (ORadj 1.22 per ng/mL increase; p = 0.01), and OPG concentrations significantly lower (ORadj 0.20 per ng/mL increase; p = 0.02) in patients with axial arthritis (PsSpA and AS combined) than in those without (pPsA). Furthermore, Dkk-1 concentrations were significantly higher along a spectrum of increasing axial arthritis; Dkk-1 concentrations were higher in AS compared with PsSpA (ORadj 1.18 per ng/mL increase; p = 0.02). Receiver operating characteristic analysis showed MMP-3 to be the best single biomarker for differentiating PsA from PsC (AUC 0.70 for a cut-off of 14.51 ng/mL; sensitivity 0.76, specificity 0.60).
Conclusions
MMP-3 and M-CSF are biomarkers for the presence of arthritis in psoriatic disease, and could therefore be used to screen for PsA in psoriasis cohorts. Dkk-1 and OPG are biomarkers of axial arthritis; they could therefore be used to screen for the presence of axial disease in PsA cases, and help differentiate PsSpA from AS. High concentrations of Dkk-1 in AS and PsSpA compared with HC, support previous reports that Dkk-1 is dysfunctional in the spondyloarthritides.
Similar content being viewed by others
Background
Psoriatic arthritis (PsA) and ankylosing spondylitis (AS) are chronic inflammatory conditions of the musculoskeletal system belonging to the family of spondyloarthritis (SpA). They are characterised by bone resorption in the form of erosion and osteolysis, and new bone formation (osteoproliferation) in the form of syndesmophytes, periostitis and sacroiliac joint (SIJ) ankylosis. The bone forming and resorbing phenotypes of PsA and AS make them good candidates to investigate the role of serum-soluble bone-turnover biomarkers.
A systematic literature review of serum-soluble bone and cartilage-turnover markers in PsA and psoriatic spondyloarthritis (PsSpA) [1], identified four candidate bone-turnover markers in PsA: dickkopf 1 (Dkk-1), which inhibits Wnt-mediated bone formation; osteoprotegerin (OPG), which inhibits RANK-mediated bone resorption; macrophage colony stimulating factor (M-CSF),which promotes bone resorption; and matrix metalloproteinase 3 (MMP-3), which degrades the extra-cellular matrix of bone and cartilage, leading to bone erosion and joint space narrowing.
We have previously reported that the presence of psoriasis and HLA-B27 are important factors that define the pattern of axial disease in SpA [2]. We now hypothesise that serum-soluble bone-turnover biomarkers are associated with disease phenotype and disease severity in patients with SpA. Using the same cohort and comparator samples from patients with psoriasis only (cases) and matched healthy controls, the aims of this study were to confirm and determine if these four biomarkers (Dkk-1, M-CSF, MMP-3, and OPG): (i) are associated with PsA; (ii) differentiate patients with psoriasis with and without arthritis; and (iii) differentiate patients with PsA with and without axial arthritis.
Methods
Study participants
A prospective cross-sectional comparative two-centre study (Axial Disease in Psoriatic Arthritis study; ADIPSA) was performed, recruiting unselected consecutive patients with PsA and AS from a secondary-care teaching hospital attended by approximately 600 patients with PsA and 700 with AS between August 2012 and October 2013. The study inclusion criteria were: patients aged ≥ 18 years with either PsA fulfilling the Classification of Psoriatic Arthritis (CASPAR) criteria [3, 4] or AS fulfilling the 1987 modified New York diagnostic criteria (mNYc) for AS [5]. The enrolled patients with PsA and AS were reclassified as: peripheral-only PsA (pPsA) without radiographic axial disease (RAD), PsA with RAD (psoriatic spondyloarthritis; PsSpA), and AS without psoriasis (AS). In keeping with previous publications [6, 7], inflammatory RAD was defined in patients with PsSpA as the presence of: New York criteria sacroiliitis (unilateral grade ≥ 3, or bilateral grade ≥ 2 sacroiliitis), and/or ≥ 1 marginal/paramarginal syndesmophyte(s) of the cervical or lumbar spine. The most recent (≤10 years) axial radiographs of all participants with SpA were scored using two validated indices: the Psoriatic Arthritis Spondylitis Radiology Index (PASRI) [8] and the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) [9].
At the time of blood sample collection all study participants were assessed by a rheumatologist (DRJ) who collected data on patient-reported outcome measures (PROMs), clinical examination indices, and axial radiographic indices. Further details on the ADIPSA cohort have been published previously [2].
Serum from 200 patients with purely cutaneous psoriasis (PsC) without clinical evidence of joint problems for ≥ 10 years since the diagnosis of psoriasis, assessed by a dermatologist, were provided from the Department of Dermatology (University of Michigan), for whom associated clinical details including sex, age, disease duration, biologic and synthetic disease-modifying anti-rheumatic drug (DMARD) use, and Psoriasis Area Severity Index (PASI) were available. Serum from 50 healthy controls (HC) was obtained from the UK Health and Social Care Information Centre (HSIC), the controls having been deemed healthy using a screening questionnaire. HCs were age, sex and ethnicity matched to the enrolled patients with PsA.
Serum biomarker testing
Patients provided non-fasted blood samples on the morning of clinical assessment and serum was stored at − 80 °C, with minimal freeze-thaw cycles [10]. Commercially available enzyme-linked immunosorbent assay (ELISA) kits were used to measure biomarker concentrations in each subject group in duplicate. Quantikine ELISA kits (R&D systems, UK) were used to measure total Dkk-1 (functionally active and inactive Dkk-1), total MMP-3 (pro-MMP-3 and active-MMP-3), and total M-CSF. Another ELISA kit (Biorbyte, UK) was used to measure total OPG. A percentage coefficient of variation (CV%) ≤ 15% between duplicate samples was considered acceptable, and samples were re-tested until CV% ≤ 15% was attained.
Statistical analysis
A statistical analysis plan was decided a priori, guided by the systematic review of biomarkers [1] and mechanistic hypotheses. Adjustment for multiple testing was therefore not required. Data were analysed using STATA12.1 (2011 TX, USA). Since serum biomarker concentrations were not normally distributed (skewed to the right, at group and cohort level), a logarithmic transformation was applied prior to all analyses. Reverse, stepwise, logistic regression, adjusted for covariables at blood sampling (sex, age, disease duration from diagnosis, anti-TNF use, body mass index (BMI), AS Disease Activity Score (ASDAS), and PASI) was used to compare biomarker concentrations between subject groups. The alpha level for statistical significance was 0.05.
Results
The study enrolled 651 subjects: 200 with PsA, 201 with AS, 200 with PsC and 50 HC. The PsA and AS cases were reclassified as: 127 pPsA, 117 PsSpA, and 157 AS (43 cases of psoriasis, but meeting both modified New York criteria for AS and CASPAR criteria for PsA, were reclassified as PsSpA for this research study). The clinical characteristics of the groups are detailed in Table 1. Axial radiographs were mostly recent (median interval between radiographs being performed and study enrolment 2.4 years, IQR 1.4, 4.1). Excellent inter-rater (intraclass correlation coefficient (ICC) ≥ 0.85) and intra-rater (ICC ≥ 0.88) reliability was achieved by raters for the PASRI, mSASSS and regional subdomains. For brevity, further clinical, radiographic and treatment characteristics of this cohort are described in the clinical-radiographic paper on the ADIPSA cohort [2].
Assay reliability
Each of the four biomarkers achieved an acceptable inter-assay CV% (≤15%). However, despite several runs, 48 of 651 duplicate OPG samples did not attain an acceptable intra-assay CV% ≤ 10, and were excluded from subsequent analyses (14/157 AS, 1/118 PsSpA, 19/127 pPsA, 6/200 PsC, 9/50 HC).
Biomarker concentrations in the cohort and analysis of covariables
Serum biomarker concentrations are detailed in Table 2. Linear and logistic regression were used to determine if biomarker concentrations were affected by the following covariables at blood sampling: sex, age, disease duration, anti-TNF use, BMI, HLA-B27 positivity, high-sensitivity C-reactive protein (hsCRP), and ASDAS. The covariables included in the final regression models are given in Table 2 . MMP-3 (regression coefficient, ß 0.01; p = 0.04) and OPG (ß 0.01; p < 0.0001) concentrations significantly increased with age.
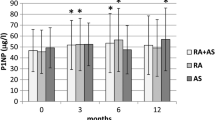
Men had significantly lower MMP-3 concentrations than women (adjusted odds ratio, ORadj 0.91; 95% CI 0.83, 0.99; p < 0.0001). MMP-3 was associated with hsCRP in patients with PsSpA, pPsA and AS. In patients with AS, the ASDAS was positively associated with Dkk-1 (ß 0.07; p = 0.003), M-CSF (ß 0.87; p = 0.001), and MMP-3 (ß 0.001; p = 0.05), and negatively associated with OPG (ß − 1.66; p = 0.03). In patients with PsSpA, the ASDAS was positively associated with M-CSF (ß 0.61; p = 0.05) only. ASDAS was included in regression models comparing concentrations in the arthritis groups, to adjust for axial disease activity as a potential confounder, acknowledging that peripheral arthritis is also somewhat captured by the ASDAS. Anti-TNF use did not appear to influence the concentrations of these four biomarkers in this cross-sectional analysis.
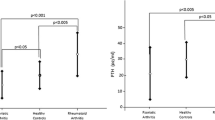
Biomarker concentrations in HC compared with each disease group
On multinomial logistic regression, Dkk-1 concentrations were significantly lower in patients with PsC compared with HC (ORadj 0.72 per ng/mL increase in concentration; 95% CI 0.61, 0.86; p = 2 × 10−4) (Table 2). M-CSF concentrations were significantly lower in patients with pPsA (ORadj 0.14 per ng/mL increase; 95% CI 0.06, 0.32; p < 1 × 10−5), PsSpA (ORadj 0.07 per ng/ml increase; 95% CI 0.03, 0.17; p < 1 × 10−8), and AS (ORadj 0.37 per ng/mL increase; 95% CI 0.16, 0.85; p < 1 × 10−7) compared with HC. MMP-3 concentrations were significantly higher patients with in pPsA (ORadj 1.06 per ng/mL increase; 95% CI 1.01, 1.10; p = 0.02), PsSpA (ORadj 1.06 per ng/mL increase; 95% CI 1.01, 1.11; p = 0.02), and AS (ORadj 1.06 per ng/mL increase; 95% CI 1.01, 1.11; p = 0.01) compared with HC. OPG concentrations were statistically no different in HC compared with any disease group. The test for homogeneity was used to determine whether biomarkers had significantly different effects when disease groups were modelled separately, whilst controlling for sex, age, and other biomarkers. MMP-3 (homogeneity p = 4 × 10−4) and OPG (homogeneity p = 5 × 10−8) concentrations were significantly different across the five groups (Table 2). Taken together, these analyses indicate that Dkk-1, M-CSF, and MMP-3 have different concentrations in healthy controls compared with disease groups, and therefore may be biomarkers of pathology.
Biomarkers of disease phenotypes
Biomarkers of arthritis in patients with psoriasis
Biomarker concentrations were compared in patients with psoriasis with (PsA; n = 244) and without (PsC; n = 200) inflammatory arthritis. MMP-3 concentrations were significantly higher in patients with PsA (median 17.44 ng/mL; IQR 11.79, 26.88) compared with PsC (median 13.13 ng/mL; IQR 9.52, 18.37) (ORadj 1.02 per ng/mL increase; 95% CI 1.01, 1.03; p = 0.0004) (Table 3). Patients with PsA (median 0.28 ng/mL; IQR 0.16, 0.67) had significantly lower M-CSF concentrations than PsC (median 0.62 ng/mL; IQR 0.25, 0.88) (ORadj 0.44 per ng/mL increase in PsA vs. PsC; 95% CI 0.24, 0.82; p = 0.01).
Biomarkers of radiographic axial disease
Biomarker concentrations were compared in patients with arthritis with radiographic axial disease (RAD; n = 274; 117 PsSpA and 157 AS) and without RAD (non-RAD; n = 127 pPsA). Dkk-1 concentrations were significantly higher in RAD (median 3.42 ng/mL; IQR 2.75, 4.49) compared with non-RAD (median 3.03 ng/mL; IQR 1.93, 3.69) cases (ORadj 1.22 per ng/mL increase; 95% CI 1.05, 1.42; p = 0.01) (Table 3). OPG concentrations were significantly lower in patients with RAD (median 0.16 ng/mL; IQR 0.11, 0.22) compared with non-RAD (median 0.19 ng/mL; IQR 0.12, 0.28) (ORadj 0.20 per ng/mL increase; 95% CI 0.05, 0.80; p = 0.02). Skin psoriasis was not a significant covariable.
Biomarkers were tested along a spectrum of increasing RAD. Patients with AS had significantly higher Dkk-1 concentrations than those with PsSpA (ORadj 1.18 per ng/mL increase; 95% CI 1.02, 1.35; p = 0.02) (Table 3). Biomarker concentrations were statistically no different in patients with PsSpA and patients with pPsA.
Association of phenotype with a biomarker panel
Multivariable logistic regression was performed to determine whether a combination (panel) of bone biomarkers and hsCRP, excluding clinical covariables, might have a stronger association with disease phenotype. A number of different panels were tested. The panel comprising Dkk-1 (ORadj 0.09 per ng/mL increase; 95% CI 0.03, 0.23; p = 4 × 10−7), MMP-3 (ORadj 1.07 per ng/mL increase; 95% CI 1.02, 1.12; p = 0.002) and OPG (ORadj 31.00 per ng/mL increase; 95% CI 0.66, 1451.86; p = 0.08) was best able to differentiate patients with PsA from HC, with an area under the receiver operating characteristic (ROC) curve (AUC) of 0.84. The AUC was < 0.73 for other all other biomarker panels as determinants of phenotype (PsA vs. PsC, PsC vs. HC, RAD vs. non-RAD, PsSpA vs. pPsA, and PsSpA vs. AS).
Biomarkers of radiographic axial disease severity and morphology
Using multivariable generalised additive models, no biomarker was associated with RAD severity (as measured by the mSASSS and PASRI) or morphology (as measured by the osteoproliferation subdomain of the PASRI, which scores for vertebral corner sclerosis, vertebral syndesmophyte formation, and cervical facet joint fusion) in either PsSpA or AS. In patients with PsSpA only, Dkk-1 concentrations were significantly lower in patients with a PASRI erosion score ≥ 1 (ORadj 0.28 per ng/mL increase; 95% CI 0.10, 0.80; p = 0.02) than in those without erosions.
Biomarker concentration thresholds differentiating disease groups
ROC analyses were performed to determine whether MMP-3 and M-CSF concentration thresholds could usefully differentiate patients with PsA from HC. In a model of maximum accuracy (proportion of cases correctly classified), an MMP-3 threshold of 7.21 ng/mL had sensitivity of 0.99 and specificity of 0.12 (AUC 0.66; 95% CI 0.59, 0.74), and an M-CSF threshold of 0.02 ng/mL had sensitivity of 1.00 and specificity of 0.00 (AUC 0.24; 95% CI 0.17, 0.31) (Table 4).
Similarly, ROC analyses were used to determine whether MMP-3 and M-CSF concentration thresholds could usefully differentiate PsA from PsC. In a model of maximum accuracy an MMP-3 threshold of 14.51 ng/mL had sensitivity of 0.76 and specificity of 0.60 (AUC 0.70; 95% CI 0.65, 0.75); and an M-CSF threshold of 0.05 ng/ml had sensitivity of 0.99 and specificity of 0.01 (AUC 0.34; 95% CI 0.29, 0.40). The effect of mandating sensitivity of > 0.95, possibly at the expense of specificity, is shown in Table 4.
Since in patients with PsA (n = 200), Dkk-1 concentrations were higher and OPG concentrations were lower in patients with with RAD compared to those without RAD, biomarker concentration thresholds could potentially be used to identify patients with PsA for spinal imaging. In a model of maximum accuracy, a Dkk-1 threshold of 4.96 ng/mL had sensitivity of 0.15 and specificity of 0.94 (AUC 0.56; 95% CI 0.44, 0.67); and an OPG threshold of 3.88 ng/ml had sensitivity of 0.00 and specificity of 0.99 (AUC 0.47; 95% CI 0.39, 0.56) (Table 4). The effect of mandating sensitivity of > 0.95, possibly at the expense of specificity, is shown in Table 4.
Discussion
We have previously reported a study of the same cohort, showing clinical, imaging, and genetic signatures unique to pPsA, PsSpA, and AS [2]. Using the same large cohort of well-characterised cases and matched healthy controls, we sought to determine whether there are unique serum-soluble bone-turnover biomarker signatures. Previously reported studies that have investigated PsA in terms of serum bone biomarkers have been limited by small sample size, variable endpoints, and heterogenous laboratory methods [1].
MMP-3 and M-CSF appear to be biomarkers of arthritis, differentiating patients with PsA from those with PsC, and patients with SpA from HC. Hence, MMP-3 and M-CSF concentration thresholds may be useful to screen for PsA in patients with PsC. We have presented two such models, allowing the clinician to choose whether very high sensitivity at the expense of specificity is most important in their setting (model with ≥ 0.95 sensitivity), or a more equitable balance between sensitivity and specificity is required (model of maximum accuracy). Neither MMP-3 nor M-CSF differentiated various forms of SpA, i.e. pPsA, PsSpA and AS, implying they may share a common pathological pathway, e.g. entheseal disease or bone resorption. Other studies have shown MMP-3 levels to be four times higher in synovial fluid compared with serum in patients with AS with peripheral involvement [11], and a thousand times higher in synovial tissue compared with serum in patients with SpA with peripheral involvement [12]. MMP-3 levels are higher in patients with axial SpA with peripheral arthritis rather than without [12,13,14]. MMP-3 may therefore be a biomarker more specific to peripheral synovial-based arthritis, than to axial non-synovial entheseal-based arthritis. MMP-3 and M-CSF need further testing to determine their performance in differentiating PsA from rheumatoid arthritis (RA) and inflammatory osteoarthritis of the interphalangeal joints.
Dkk-1 appears to be a biomarker of axial disease in SpA, with a pattern for increasing concentration along a spectrum of increasing axial arthritis. Dkk-1 could be used to differentiate patients with PsA with and without axial arthritis, and patients with PsSpA from those with AS. Our previous research has shown that 25% of patients with PsA with radiographic axial disease do not recall ever having inflammatory axial symptoms [2]. Dkk-1 and OPG testing may therefore offer an opportunity to identify “symptomatically-silent” axial disease in PsA. We have therefore proposed Dkk-1 concentration thresholds that might be used to screen for axial disease in patients with PsA. Similarly, OPG appears to be a biomarker of axial disease in patients with SpA, and could be used to differentiate patients with axial SpA from peripheral-only SpA, independently of psoriasis status.
Since Dkk-1 is an inhibitor of the Wnt pathway, which normally induces osteoblastogenesis and new bone formation, one might expect Dkk-1 concentrations to be progressively lower along a spectrum of diseases with increasing new bone formation. However, consistent with most other studies, Dkk-1 concentrations were higher in patients with AS compared with HC [15,16,17]; no different in patients with pPsA compared with HC [15]; and higher in patients with AS compared with PsA [15]. Dkk-1 levels may be higher in SpA, particularly AS, because Dkk-1 is pathologically dysfunctional. Daoussis et al. found that whilst serum total Dkk-1 levels are higher in patients with AS compared with HC or patients with PsA, Dkk-1 is dysfunctional in AS; Dkk-1 binds less avidly to its receptor LRP6, has an abnormal stimulatory effect on the Wnt pathway, and responds abnormally to anti-Dkk-1 monoclonal antibodies [15]. Yucong et al. also reported less avid binding of Dkk-1 to its receptor in patients with AS compared with HC [18]. These studies explain the progressively higher Dkk-1 concentrations along our spectrum of patients with increasing RAD, as an attempt to compensate for dysfunctional Dkk-1. Dysfunctional Dkk-1 is inadequately inhibiting Wnt-pathways, allowing unimpeded bone formation, possibly translating to the osteoproliferative phenotype of SpA.
We found lower Dkk-1 concentrations in patients with PsSpA with vertebral erosions. In human embryonic stems cells, Dkk-1 plays an important role promoting synovial angiogenesis, that might encourage inflammatory pannus formation, and subsequent erosion [19]. There is emerging evidence that Wnt-pathways are involved in non-bone pathways associated with psoriasis, characterised by keratinocyte hyperproliferation and altered innate immunity [20,21,22,23,24,25].
In SpA there is a paradox of osteoproliferation and bone resorption. Patients with AS [26,27,28] or PsA [29] are prone to osteoporosis. As OPG inhibits bone resorption, low OPG levels may translate to low bone mineral density. However, as we did not measure bone mineral density, we cannot determine if these serum biomarkers are reflecting SpA-related pathology in trabecular bone, or vertebral corners and sacroiliac joints. The measurement of these bone markers in tissues sampled from the vertebral corners and sacroiliac joints would be mechanistically more informative. However, obtaining such samples in live participants would be procedurally challenging, painful for participants, and likely hamper study enrolment. Our study would have been further strengthened had we measured serum RANKL levels, as there is some evidence that the ratio of RANKL:OPG is more indicative of axis dysregulation than either biomarker alone [30,31,32,33].
Further research is needed to determine whether synthetic and biological DMARDs directly alter bone biomarkers, independently of their influence on disease activity. Within the constraints of our cross-sectional study design, we demonstrated no relationship between anti-TNF use and levels of biomarkers. However, other studies have shown that biomarker concentrations are influenced by anti-TNF use, longitudinally in PsA [34, 35], cross-sectionally [32, 36] and longitudinally [11, 17, 37,38,39,40] in AS, in AS clinical responders and non-responders [38], only in AS patients with peripheral arthritis [41], and with differential direction of change (Dkk-1) in AS compared with RA [15].
The reliability of our results is strengthened by the large sample size, robust case classification, no missing data for three biomarkers, matching of HCs with PsA cases, and multivariable regression modelling allowing adjustment for confounders, particularly disease duration and activity. Our results are generalisable to real-world clinical practice, because consecutive unselected clinic attendees were invited to participate, reducing selection bias, and enrolling patients of differing ages, stages of disease, and disease activity.
Our results would have been strengthened had reliable commercially available kits been available to measure active-MMP-3 rather than total MMP-3 [42,43,44,45], functional Dkk-1 or Dkk-1 biological activity rather than total Dkk-1 [15, 18, 46], RANK ligand [30,31,32,33], sclerostin, and neoepitopes of type 2 collagen metabolism (CPII and C2C). The cross-sectional design of our study reduced the ability to entirely adjust for time-varying variables such as disease activity, medication use and BMI, and unmeasured confounders known to alter OPG and MMP-3 concentrations [10, 47, 48]. However, the direction and magnitude of their confounding is unlikely to be significantly different across the four disease groups. We acknowledge that some patients with pPsA will have non-radiographic PsSpA, perhaps better detected on magnetic resonance imaging (MRI) or computed tomography (CT).
Conclusions
This study gives further insight into the pathophysiology of psoriasis, PsA, and AS. These bone biomarkers offer potential to screen for PsA in psoriasis cohorts, screen for axial arthritis in PsA, and help differentiate PsSpA from AS. A larger study is underway by our group to replicate these findings in an independent well-characterised inception cohort. These four markers will also be investigated longitudinally as biomarkers of disease activity, treatment response, and prognosis.
Abbreviations
- ADIPSA:
-
Axial Disease in Psoriatic Arthritis study
- AS:
-
Ankylosing spondylitis
- ASDAS:
-
Ankylosing Spondylitis Disease Activity Score
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CASPAR:
-
Classification of Psoriatic Arthritis
- Dkk-1:
-
Dickkopf-1
- ELISA:
-
enzyme-linked immunosorbent assay
- HC:
-
Healthy controls
- hsCRP:
-
High-sensitivity C-reactive protein
- M-CSF:
-
Macrophage-colony stimulating factor
- MMP-3:
-
Matrix metalloproteinase-3
- mSASSS:
-
Modified Stoke Ankylosing Spondylitis Spinal Score
- OPG:
-
Osteoprotegerin
- PASRI:
-
Psoriatic Arthritis Spondylitis Radiology Index
- pPsA:
-
Psoriatic arthritis without axial arthritis
- PsA:
-
Psoriatic arthritis
- PsC:
-
Psoriasis without arthritis
- PsSpA:
-
Psoriatic spondyloarthritis
- RA:
-
Rheumatoid arthritis
- RAD:
-
Radiographic axial disease
- ROC:
-
Receiver operating characteristic
- SIJ:
-
sacroiliac joint
- TNF:
-
Tumour necrosis factor
References
Jadon DR, Nightingale AL, McHugh NJ, Lindsay MA, Korendowych E, Sengupta R. Serum soluble bone turnover biomarkers in psoriatic arthritis and psoriatic spondyloarthropathy. J Rheumatol. 2014;42(1):21–30.
Jadon DR, Sengupta R, Nightingale A, Lindsay M, Korendowych E, Robinson G, et al. Axial Disease in Psoriatic Arthritis study: defining the clinical and radiographic phenotype of psoriatic spondyloarthritis. Ann Rheum Dis. 2016;76(4):701–7.
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006;54(8):2665–73.
Tillett W, Jadon D, Costa L, Wallis D, Cavill C, McHugh J, et al. The Classification for Psoriatic Arthritis (CASPAR) criteria - a retrospective feasibility, sensitivity, and specificity study. J Rheumatol. 2012;39(1):154–6.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–8.
Jadon D, Tillett W, Wallis D, Cavill C, Bowes J, Waldron N, et al. Exploring ankylosing spondylitis-associated ERAP1, IL23R and IL12B gene polymorphisms in subphenotypes of psoriatic arthritis. Rheumatology (Oxford). 2013;52(2):261–6.
Chandran V, Barrett J, Schentag CT, Farewell VT, Gladman DD. Axial psoriatic arthritis: update on a longterm prospective study. J Rheumatol. 2009;36(12):2744–50.
Lubrano E, Marchesoni A, Olivieri I, D’Angelo S, Spadaro A, Parsons WJ, et al. Psoriatic arthritis spondylitis radiology index: a modified index for radiologic assessment of axial involvement in psoriatic arthritis. J Rheumatol. 2009;36(5):1006–11.
Creemers MCW. Assessment of outcome in ankylosing spondylitis: an extended radiographic scoring system. Ann Rheum Dis. 2005;64(1):127–9.
Clowes JA. Effect of feeding on bone turnover markers and its impact on biological variability of measurements. Bone. 2002;30(6):886–90.
Yang C, Gu J, Rihl M, Baeten D, Huang F, Zhao M, et al. Serum levels of matrix metalloproteinase 3 and macrophage colony-stimulating factor 1 correlate with disease activity in ankylosing spondylitis. Arthritis Rheum. 2004;51(5):691–9.
Vandooren B, Kruithof E, Yu DTY, Rihl M, Gu J, De Rycke L, et al. Involvement of matrix metalloproteinases and their inhibitors in peripheral synovitis and down-regulation by tumor necrosis factor-alpha blockade in spondylarthropathy. Arthritis Rheum. 2004;50(9):2942–53.
Pedersen SJ, Sorensen IJ, Garnero P, Johansen JS, Madsen OR, Tvede N, et al. ASDAS, BASDAI and different treatment responses and their relation to biomarkers of inflammation, cartilage and bone turnover in patients with axial spondyloarthritis treated with TNFalpha inhibitors. Ann Rheum Dis. 2011;70(8):1375–81.
Maksymowych WP, Rahman P, Shojania K, Olszynski WP, Thomson GT, Ballal S, et al. Beneficial effects of adalimumab on biomarkers reflecting structural damage in patients with ankylosing spondylitis. J Rheumatol. 2008;35(10):2030–7.
Daoussis D, Liossis S-NC, Solomou EE, Tsanaktsi A, Bounia K, Karampetsou M, et al. Evidence that Dkk-1 is dysfunctional in ankylosing spondylitis. Arthritis Rheum. 2010;62(1):150–8.
Klingberg E, Nurkkala M, Carlsten H, Forsblad-d’Elia H. Biomarkers of bone metabolism in ankylosing spondylitis in relation to osteoproliferation and osteoporosis. J Rheumatol. 2014;41(7):1349–56.
Wang SY, Liu YY, Ye H, Guo JP, Li R, Liu X, et al. Circulating Dickkopf-1 is correlated with bone erosion and inflammation in rheumatoid arthritis. J Rheumatol. 2011;38(5):821–7.
Yucong Z, Lu L, Shengfa L, Yongliang Y, Ruguo S, Yikai L. Serum functional dickkopf-1 levels are inversely correlated with radiographic severity of ankylosing spondylitis. Clin Lab. 2014;60(9):1527–31.
Yang L, Soonpaa MH, Adler ED, Roepke TK, Kattman SJ, Kennedy M, et al. Human cardiovascular progenitor cells develop from a KDR+ embryonic-stem-cell-derived population. Nature. 2008;453(7194):524–8.
Hampton PJ, Ross OK, Reynolds NJ. Increased nuclear beta-catenin in suprabasal involved psoriatic epidermis. Br J Dermatol. 2007;157(6):1168–77.
Teh MT, Blaydon D, Ghali LR, Briggs V, Edmunds S, Pantazi E, et al. Role for WNT16B in human epidermal keratinocyte proliferation and differentiation. J Cell Sci. 2007;120(Pt 2):330–9.
Yamaguchi Y, Passeron T, Watabe H, Yasumoto K, Rouzaud F, Hoashi T, et al. The effects of dickkopf 1 on gene expression and Wnt signaling by melanocytes: mechanisms underlying its suppression of melanocyte function and proliferation. J Invest Dermatol. 2007;127(5):1217–25.
Reischl J, Schwenke S, Beekman JM, Mrowietz U, Sturzebecher S, Heubach JF. Increased expression of Wnt5a in psoriatic plaques. J Invest Dermatol. 2007;127(1):163–9.
Gudjonsson JE, Johnston A, Stoll SW, Riblett MB, Xing X, Kochkodan JJ, et al. Evidence for altered Wnt signaling in psoriatic skin. J Invest Dermatol. 2010;130(7):1849–59.
Seifert O, Soderman J, Skarstedt M, Dienus O, Matussek A. Increased expression of the Wnt signalling inhibitor Dkk-1 in non-lesional skin and peripheral blood mononuclear cells of patients with plaque psoriasis. Acta Derm Venereol. 2015;95(4):407–10.
Franck H, Meurer T, Hofbauer LC. Evaluation of bone mineral density, hormones, biochemical markers of bone metabolism, and osteoprotegerin serum levels in patients with ankylosing spondylitis. J Rheumatol. 2004;31(11):2236–41.
Donnelly S, Doyle DV, Denton A, Rolfe I, McCloskey EV, Spector TD. Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis. 1994;53(2):117–21.
Klingberg E, Geijer M, Gothlin J, Mellstrom D, Lorentzon M, Hilme E, et al. Vertebral fractures in ankylosing spondylitis are associated with lower bone mineral density in both central and peripheral skeleton. J Rheumatol. 2012;39(10):1987–95.
Reddy SM, Anandarajah AP, Fisher MC, Mease PJ, Greenberg JD, Kremer JM, et al. Comparative analysis of disease activity measures, use of biologic agents, body mass index, radiographic features, and bone density in psoriatic arthritis and rheumatoid arthritis patients followed in a large U.S. disease registry. J Rheumatol. 2010;37(12):2566–72.
Kim HR, Lee SH, Kim HY. Elevated serum levels of soluble receptor activator of nuclear factors-kappaB ligand (sRANKL) and reduced bone mineral density in patients with ankylosing spondylitis (AS). Rheumatology (Oxford). 2006;45(10):1197–200.
Chen CH, Chen HA, Liao HT, Liu CH, Tsai CY, Chou CT. Soluble receptor activator of nuclear factor-kappaB ligand (RANKL) and osteoprotegerin in ankylosing spondylitis: OPG is associated with poor physical mobility and reflects systemic inflammation. Clin Rheumatol. 2010;29(10):1155–61.
Taylan A, Sari I, Akinci B, Bilge S, Kozaci D, Akar S, et al. Biomarkers and cytokines of bone turnover: extensive evaluation in a cohort of patients with ankylosing spondylitis. BMC Musculoskelet Disord. 2012;13:191.
Geusens PP, Landewe RB, Garnero P, Chen D, Dunstan CR, Lems WF, et al. The ratio of circulating osteoprotegerin to RANKL in early rheumatoid arthritis predicts later joint destruction. Arthritis Rheum. 2006;54(6):1772–7.
Chandran V, Shen H, Pollock RA, Pellett FJ, Carty A, Cook RJ, et al. Soluble biomarkers associated with response to treatment with tumor necrosis factor inhibitors in psoriatic arthritis. J Rheumatol. 2013;40(6):866–71.
Wagner CL, Visvanathan S, Elashoff M, McInnes IB, Mease PJ, Krueger GG, et al. Markers of inflammation and bone remodelling associated with improvement in clinical response measures in psoriatic arthritis patients treated with golimumab. Ann Rheum Dis. 2013;72(1):83–8.
de Andrade KR, de Castro GR, Vicente G, da Rosa JS, Nader M, Pereira IA, et al. Evaluation of circulating levels of inflammatory and bone formation markers in axial spondyloarthritis. Int Immunopharmacol. 2014;21(2):481–6.
Woo JH, Lee HJ, Sung IH, Kim TH. Changes of clinical response and bone biochemical markers in patients with ankylosing spondylitis taking etanercept. J Rheumatol. 2007;34(8):1753–9.
Pedersen SJ, Hetland ML, Sorensen IJ, Ostergaard M, Nielsen HJ, Johansen JS. Circulating levels of interleukin-6, vascular endothelial growth factor, YKL-40, matrix metalloproteinase-3, and total aggrecan in spondyloarthritis patients during 3 years of treatment with TNF alpha inhibitors. Clin Rheumatol. 2010;29(11):1301–9.
Kwon SR, Lim MJ, Suh CH, Park SG, Hong YS, Yoon BY, et al. Dickkopf-1 level is lower in patients with ankylosing spondylitis than in healthy people and is not influenced by anti-tumor necrosis factor therapy. Rheumatol Int. 2012;32(8):2523–7.
Appel H, Janssen L, Listing J, Heydrich R, Rudwaleit M, Sieper J. Serum levels of biomarkers of bone and cartilage destruction and new bone formation in different cohorts of patients with axial spondyloarthritis with and without tumor necrosis factor-alpha blocker treatment. Arthritis Res Ther. 2008;10(5):R125.
Arends S, van der Veer E, Groen H, Houtman PM, Jansen TL, Leijsma MK, et al. Serum MMP-3 level as a biomarker for monitoring and predicting response to etanercept treatment in ankylosing spondylitis. J Rheumatol. 2011;38(8):1644–50.
Chen CH, Lin KC, Yu DT, Yang C, Huang F, Chen HA, et al. Serum matrix metalloproteinases and tissue inhibitors of metalloproteinases in ankylosing spondylitis: MMP-3 is a reproducibly sensitive and specific biomarker of disease activity. Rheumatology (Oxford). 2006;45(4):414–20.
Sun S, Bay-Jensen AC, Karsdal MA, Siebuhr AS, Zheng Q, Maksymowych WP, et al. The active form of MMP-3 is a marker of synovial inflammation and cartilage turnover in inflammatory joint diseases. BMC Musculoskelet Disord. 2014;15:93.
Baker AH, Edwards DR, Murphy G. Metalloproteinase inhibitors: biological actions and therapeutic opportunities. J Cell Sci. 2002;115(Pt 19):3719–27.
Sottrup-Jensen L. Alpha-macroglobulins: structure, shape, and mechanism of proteinase complex formation. J Biol Chem. 1989;264(20):11539–42.
Heiland GR, Appel H, Poddubnyy D, Zwerina J, Hueber A, Haibel H, et al. High level of functional dickkopf-1 predicts protection from syndesmophyte formation in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71(4):572–4.
Ribbens C, Martin y Porras M, Franchimont N, Kaiser MJ, Jaspar JM, Damas P, et al. Increased matrix metalloproteinase-3 serum levels in rheumatic diseases: relationship with synovitis and steroid treatment. Ann Rheum Dis. 2001;61(2):161–6.
Schlemmer A, Hassager C. Acute fasting diminishes the circadian rhythm of biochemical markers of bone resorption. European journal of endocrinology/European Federation of Endocrine Societies. 1999;140(4):332–7.
Acknowledgements
Not applicable.
Funding
This study was funded through an unrestricted Investigator-Initiated Research grant by Pfizer Limited awarded to DRJ and NJM. The collection of psoriasis cases was supported by the NIH grant R01-AR042743 and -AR050511 awarded to JTE. Pfizer and the NIH did not have a role in the design of the study, data collection, data analysis, interpretation of data or writing of the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
These authors made substantial contributions to conception and design: DJ, RS, AN, EK, ML, and NM; to acquisition of data: DJ, JD, HL, RN, JE, EK, NM, and RS; to analysis: DJ, RS, AN, JD, HL, AG, and NM); and to interpretation of data: DJ, RS, AN, RN, JE, and NM. These authors been involved in drafting the manuscript or revising it critically for important intellectual content: DJ, RS, AN, NM, AG, RN, and JT. All authors have given final approval of the version to be published. All authors have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed with ethical approval from the Frenchay Regional Ethics Committee (12/SW/0110) and Institutional Review Boards of the Royal National Hospital for Rheumatic Diseases (RBB376) and University of Michigan, with written consent from participants, and in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jadon, D.R., Sengupta, R., Nightingale, A. et al. Serum bone-turnover biomarkers are associated with the occurrence of peripheral and axial arthritis in psoriatic disease: a prospective cross-sectional comparative study. Arthritis Res Ther 19, 210 (2017). https://doi.org/10.1186/s13075-017-1417-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-017-1417-7