Abstract
Introduction
Rheumatic diseases (RDs) are associated with different cancers; however, it is unclear whether particular cancers are more prevalent in certain RDs. In the present study, we examined the relative incidence of several cancers in a single homogeneous cohort of patients with different RDs.
Methods
Patients (N = 3,586) diagnosed with rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SSc), dermatomyositis (DM) or polymyositis were included. Cancer diagnosis was based on histopathology. The 2008 Korean National Cancer Registry served as the reference for calculating standardized incidence ratios (SIRs).
Results
During the follow-up period of 31,064 person-years, 187 patients developed cancer. RA and SLE patients showed an increased risk of non-Hodgkin’s lymphoma (SIR for RA patients = 3.387, 95% confidence interval (CI) = 1.462 to 6.673; SIR for SLE patients = 7.408, 95% CI = 2.405 to 17.287). SLE patients also had a higher risk of cervical cancer (SIR = 4.282, 95% CI = 1.722 to 8.824). SSc patients showed a higher risk of lung cancer (SIR = 4.917, 95% CI = 1.977 to 10.131). Endometrial cancer was increased only in patients with DM (SIR = 30.529, 95% CI = 3.697 to 110.283). RA patients had a lower risk for gastric cancer (SIR = 0.663, 95% CI = 0.327 to 0.998). The mean time between the RD and cancer diagnoses ranged from 0.1 to 16.6 years, with the shortest time observed in patients with DM (2.0 ± 2.1 years).
Conclusions
Different RDs are associated with particular cancers. Thus, cancer surveillance tailored to specific RDs might be beneficial.
Similar content being viewed by others
Introduction
Rheumatic diseases (RDs) result from immune dysfunction, which leads to chronic systemic inflammation and damage to multiple organs. Precancerous cells can escape cancer surveillance associated with impaired immune response [1]. Chronic inflammation, along with the associated production of cytokines and growth factors, may promote the progression of precancerous cells to a clinically relevant cancer [2]. Indeed, there is a robust link between cancer and RDs. Patients with rheumatoid arthritis (RA), systemic lupus erythematosus (SLE) and Sjögren’s syndrome (SS) have a higher risk of developing lymphoma [3]-[5], and those with systemic sclerosis (SSc) tend to have a higher risk of developing lung cancer [6],[7]. These studies suggest that the type of RD a patient has is associated with an increased risk of developing certain cancers. This may be due to the nature of the underlying immune dysfunction and the extent of involved organ damage.
However, previous studies have shown marked variations in the estimated incidence of cancer in patients with the same type of RD. This is likely due to differences in genetic background, environmental factors and available treatment options. For example, patients with dermatomyositis (DM) in Scandinavia show an increased risk of lung or endometrial cancer [8], whereas those in Taiwan show an increased risk of head and neck cancer [9]. The cancer risk even differs between different Asian populations with the same RD. Taiwanese RA patients have an increased risk of kidney and vaginal cancer, but no such associations are observed in Japanese RA patients [10],[11]. In addition to the heterogeneity of the study populations, the methodological differences in case ascertainment likely contribute to the varying SIR estimates across studies. Population-based studies using National Health Insurance claims or hospital discharge registry data might reveal rare cancers at the expense of diagnostic accuracy of RDs and cancer, especially when longitudinal follow-up data are not available. Thus, comparison of cancer incidences from multiple studies would not conclusively address the question whether a particular RD is associated with a higher risk of developing a certain cancer. Our aim in the present study was to compare the relative incidence of several common cancers in different RDs in a single homogeneous cohort.
Methods
Patients
As patients with a rare or critical illness, including RDs and cancer, are entitled to reimbursement of a majority of their medical copayments, diagnosis of RDs and cancer is subjected to comprehensive clinical and laboratory assessments in Korea. Thus, when the same International Classification of Diseases (ICD) codes are entered repeatedly over a certain period of time for billing and reimbursement purposes, diagnosis of RD is accurate with a high probability.
We first selected patients with the same ICD-10 code for a specific RD (that is, RA (M 05.X, M 06.X), SLE (M 32.X), SSc (M 34.X), DM (M 33.0, 33.1, 33.9), PM (M 33.2)] for more than 6 months during their longitudinal medical care at Seoul National University Hospital (SNUH) between January 2000 and April 2012. Next, the medical records of all selected patients with a diagnosis of probable RD were reviewed. Only the patients with a definitive RD diagnosis who fulfilled the criteria for RA, SLE, SSc, DM or PM were enrolled in this study (Additional file 1: Figure S1) [12]-[15]. Patients who developed cancer before or within 1 month of RD diagnosis were excluded.
The 2008 Korean National Cancer Registry, provided by the Ministry of Health and Welfare of Korea [16], was used as the reference for calculating the standardized incidence ratios (SIRs). The study was approved by the Institutional Review Board (IRB) of SNUH. Obtaining a patient consent was waived by the IRB, as this study involved no more than minimal risk as a retrospective study and no identifiable information was used.
Cancer diagnosis
Histopathology reports were available in all cancer cases. A complete data set regarding cancer histopathology was obtained from the medical records.
Statistical analysis
The expected number of cancers was calculated by multiplying the number of patients in the study cohort by the age- and sex-matched cancer incidence rate for Koreans obtained from the 2008 Korean National Cancer Registry. When a patient was diagnosed with two or more cancers during follow-up, each was considered as an individual event. The SIR was calculated as the ratio of the observed to the expected number of cancers, and the 95% confidence interval (95% CI) was calculated based on the assumption that the observed findings followed a Poisson distribution [17]. Analysis of variance or Student’s t-tests were used for group comparisons as appropriate. The results were expressed as the mean ± standard deviation. A P-value ≤0.05 was considered statistically significant. All analyses were performed using SPSS version 16.0 statistical software (IBM SPSS, Chicago, IL, USA).
Results
Study population
A total of 3,586 patients (84.0% female) with a definitive RD diagnosis were identified and enrolled in the study. The mean duration of follow-up was 7.8 ± 4.5 years, with a total follow-up of 31,064 person-years (PYs). All patients were ethnic Koreans. The mean age at the time of RD diagnosis was 45.9 ± 15.2 years. RA was the most common diagnosis (2,104 patients; 58.7%), followed by SLE (1,052; 29.3%), SSc (274; 7.6%), DM (107; 3.0%) and PM (49; 1.4%). Of these, 185 patients were diagnosed with a malignancy, and 2 patients had 2 cancers, with an overall cancer incidence of 0.60/100 PYs. The mean time between the RD diagnosis and that of cancer ranged from 0.1 to 16.6 years, with the shortest time observed in patients with DM (2.0 ± 2.1 years). Notably, 5 (50.5%) of the 10 malignancies were diagnosed within 1 year of the DM diagnosis (Table 1).
Cancer incidence
The incidence of cancer varied between patients with different types of RD. Compared with the incidence in the general population, the cancer incidence was higher in patients with SLE (SIR = 1.555; 95% CI, 1.137 to 1.974) and DM (SIR = 2.602; 95% CI, 1.248 to 4.785), but lower in patients with RA (SIR = 0.803; 95% CI, 0.65 to 0.955) (Figure 1).
Cancer incidence in patients with rheumatic disease. The incidence of cancer was higher in patients with systemic lupus erythematosus and dermatomyositis, but lower in those with rheumatoid arthritis, compared with that in the general population. SIR, Standardized incidence ratio; CI, Confidence interval.
Association between individual rheumatic diseases and particular cancers
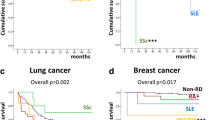
The SIR for NHL was increased in patients with RA (SIR = 3.387; 95% CI, 1.462 to 6.673) and in patients with SLE (SIR = 7.408; 95% CI, 2.405 to 17.287). The incidence of cervical cancer was increased only in patients with SLE (SIR = 4.282; 95% CI, 1.722 to 8.824), whereas that of lung cancer was increased only in patients with SSc (SIR = 4.282; 95% CI, 1.722 to 8.824). A higher incidence of endometrial cancer was estimated only in patients with DM (SIR = 30.529; 95% CI, 3.697 to 110.283). The incidence of gastric cancer was estimated to be lower in patients with RA (SIR = 0.663; 95% CI, 0.327 to 0.997) (Table 2).
Discussion
Impaired immune surveillance in patients with autoimmune disease might allow precancerous cells to grow, thereby increasing the overall risk of developing a clinically relevant cancer [1]. Indeed, an association between particular cancers and specific RDs has been reported, and the risk of developing a specific cancer appears to vary markedly depending on the RD [18],[19]. However, as previous studies have shown marked variations in the estimated incidence of the same cancer in patients with the same RD, comparison of estimated SIRs from different studies has limitations. To the best of our knowledge, the present study is the first in which the incidence of common cancers in a single homogeneous cohort of patients with different RDs has been estimated and compared.
In line with previous reports, our data show that patients with RA and SLE, but not those with SSc, DM or PM, had an increased risk of developing lymphoma, suggesting that the strong activation of lymphoid tissue is a driving force (similar to the finding that chronic viral or bacterial infections increase the risk of developing lymphoma) [20]. Indeed, overexpression of B lymphocyte simulator (BLyS) is associated with lymphoproliferative disorders in patients with SS [21]. Patients with RA and SLE exhibit high levels of BLyS [22],[23].
Consistent with prior studies, lung cancer risk was higher in patients with SSc [24],[25]. Reduced forced vital capacity and pulmonary fibrosis are associated with an increased risk of developing lung cancer, suggesting that the extent of lung damage may predict subsequent cancer development [7]. In the present study, the incidence of lung cancer in patients with DM, which often involves severe interstitial lung disease, appeared to be increased, although the increase did not reach statistical significance.
The overall risk of developing cancer was lower for RA patients, in part due to the lower incidence of stomach cancer (Table 2). This is striking because stomach cancer is common in Korea, with an incidence of 43.8 per 100,000, which is due, at least in part, to the high prevalence of Helicobacter pylori infection [26]. The lower overall incidence of gastric cancer in RA patients could be explained by the increased use of nonsteroidal anti-inflammatory drugs (NSAIDs), which reduce proliferative stimuli and may slow down the progression of a precancerous lesion [27]. Wu et al. reported that regular NSAID use for 6 months or longer was associated with a lower risk of developing a gastric cancer [28]. In a pilot study, we compared NSAID use between RA patients with gastric cancer and those without cancer. Thirteen of fifteen RA patients with gastric cancer and forty of forty-five age- and sex-matched RA patients without gastric cancer took NSAIDs on regular basis for 6 months or longer (86.7% vs. 88.9%, P = 1.0 by Fisher’s exact test). Although we could not confirm the protective effect of NSAIDs on gastric cancer in our cohort, it is still possible that gastrointestinal complaints associated with frequent use of NSAIDs might lead to early diagnosis and eradication of subclinical H. pylori infections in RA patients, thereby reducing the overall incidence of gastric cancer.
A population-based study using data from Sweden, Denmark and Finland showed that ovarian and cervical cancers were particularly increased in DM and PM [8]. In our present study, such associations were not found. Instead, a higher SIR for endometrial cancer was observed in DM patients.
Strikingly, five of the ten DM patients developed cancer within 1 year of their DM diagnosis (Additional file 1: Table S1), with a mean time between RD and cancer diagnosis of 2.0 ± 2.1 years as compared to 7.4 ± 4.2 years, 8.9 ± 4.8 years and 6.6 ± 4.5 years for RA, SLE and SSc patients, respectively. The tight temporal relationship between DM and cancer suggests that a DM subset might be triggered as an immunologic response to cancer, similar to what is seen in SSc patients with autoantibodies against RNA polymerase III. In those SSc patients, cancer was detected before or simultaneously with their SSc diagnosis, and their peripheral T cells reacted to the peptides derived from mutated RNA polymerase III [29]. It is tempting to speculate that preclinical malignancies may initiate and drive the development of DM through molecular mimicry between mutated cancer protein and self-antigen, because treatment of the underlying cancer has been reported to improve DM [30].
There was no association between thyroid cancer and RD or between breast cancer and RD, and their SIRs were similar across RD as well (Table 2). It appears that having RD does not increase the risk of developing cancers that are common in the general population, particularly if the cancer site is not an organ affected by the systemic inflammation associated with RD.
A strength of the present study as a single center study is the homogeneity of study population and the high quality of the clinical data obtained in conjunction with a relatively long follow-up of 31,064 PYs. This study design allowed us to better estimate the “pure” effect of individual RDs on cancer development. However, our study has several limitations. Compared to a population-based study, the cohort size was relatively small, with a wide CI for SIR estimates and a low sensitivity for detecting rare cancers. Because our hospital is a major tertiary referral center, the patients in our cohort may have had more severe disease and multiple comorbidities; therefore, they may have been monitored more closely and treated more quickly or differently, thereby leading to possible treatment bias. As this was a retrospective study, another limitation is that information on the cancer in some patients with RD could not be captured completely, especially when patients received their cancer treatment outside our center, possibly contributing to the lower SIR of cancers in patients with RD. Last but not least, we did not examine the treatment effects on cancer development. For example, pulmonary fibrosis may be a side effect of methotrexate and can predispose a patient to developing lung cancer. Cyclophosphamide can induce the development of secondary cancers [31]. In addition, the prolonged use of corticosteroids and immunosuppressants can increase infection rates, which may then increase cancer risk [32].
Conclusions
Different RDs appear to be associated with particular cancers. Therefore, RD patients might benefit from cancer surveillance that is tailored to their RD.
Authors’ contributions
SHC and JKP participated in the study design, collection and analysis of the data, and preparation of the manuscript. YJL, JAY, EYL and YWS participated in data analysis and preparation of the manuscript. JAY participated in data collection and helped revision of the manuscript. EBL conceived of the study and participated in the study design, interpretation of the data and preparation of the manuscript. All authors read and approved the final manuscript.
Additional file
Abbreviations
- ACR:
-
American College of Rheumatology
- BLyS:
-
B lymphocyte simulator
- CI:
-
Confidence interval
- DM:
-
Dermatomyositis
- IRB:
-
Institutional Review Board
- NHL:
-
Non-Hodgkin’s lymphoma
- PM:
-
Polymyositis
- PY:
-
Person-year
- RA:
-
Rheumatoid arthritis
- RD:
-
Rheumatic disease
- SD:
-
Standard deviation
- SIR:
-
Standardized incidence ratio
- SLE:
-
Systemic lupus erythematosus
- SSc:
-
Systemic sclerosis
References
Swann JB, Smyth MJ: Immune surveillance of tumors. J Clin Invest. 2007, 117: 1137-1146. 10.1172/JCI31405.
Balkwill F, Mantovani A: Inflammation and cancer: back to Virchow?. Lancet. 2001, 357: 539-545. 10.1016/S0140-6736(00)04046-0.
Weng MY, Huang YT, Liu MF, Lu TH: Incidence of cancer in a nationwide population cohort of 7852 patients with primary Sjogren’s syndrome in Taiwan. Ann Rheum Dis. 2012, 71: 524-527. 10.1136/annrheumdis-2011-200402.
Bernatsky S, Ramsey-Goldman R, Labrecque J, Joseph L, Boivin JF, Petri M, Zoma A, Manzi S, Urowitz MB, Gladman D, Fortin PR, Ginzler E, Yelin E, Bae SC, Wallace DJ, Edworthy S, Jacobsen S, Gordon C, Dooley MA, Peschken CA, Hanly JG, Alarcón GS, Nived O, Ruiz-Irastorza G, Isenberg D, Rahman A, Witte T, Aranow C, Kamen DL, Steinsson K: Cancer risk in systemic lupus: an updated international multi-centre cohort study. J Autoimmun. 2013, 42: 130-135. 10.1016/j.jaut.2012.12.009.
Mercer LK, Davies R, Galloway JB, Low A, Lunt M, Dixon WG, Watson KD, Symmons DP, Hyrich KL: Risk of cancer in patients receiving non-biologic disease-modifying therapy for rheumatoid arthritis compared with the UK general population. Rheumatology (Oxford). 2013, 52: 91-98. 10.1093/rheumatology/kes350.
Chatterjee S, Dombi GW, Severson RK, Mayes MD: Risk of malignancy in scleroderma: a population-based cohort study. Arthritis Rheum. 2005, 52: 2415-2424. 10.1002/art.21225.
Kang KY, Yim HW, Kim IJ, Yoon JU, Ju JH, Kim HY, Park SH: Incidence of cancer among patients with systemic sclerosis in Korea: results from a single centre. Scand J Rheumatol. 2009, 38: 299-303. 10.1080/03009740802642062.
Hill CL, Zhang Y, Sigurgeirsson B, Pukkala E, Mellemkjaer L, Airio A, Evans SR, Felson DT: Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001, 357: 96-100. 10.1016/S0140-6736(00)03540-6.
Kuo CF, See LC, Yu KH, Chou IJ, Chang HC, Chiou MJ, Luo SF: Incidence, cancer risk and mortality of dermatomyositis and polymyositis in Taiwan: a nationwide population study. Br J Dermatol. 2011, 165: 1273-1279. 10.1111/j.1365-2133.2011.10595.x.
Chen YJ, Chang YT, Wang CB, Wu CY: The risk of cancer in patients with rheumatoid arthritis: a nationwide cohort study in Taiwan. Arthritis Rheum. 2011, 63: 352-358. 10.1002/art.30134.
Yamada T, Nakajima A, Inoue E, Tanaka E, Taniguchi A, Momohara S, Yamanaka H: Incidence of malignancy in Japanese patients with rheumatoid arthritis. Rheumatol Int. 2011, 31: 1487-1492. 10.1007/s00296-010-1524-0.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medsger TA, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Sharp JT, Wilder RL, Hunder GG: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324. 10.1002/art.1780310302.
Hochberg MC: Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus.Arthritis Rheum 1997, 40:1725.,
Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum. 1980, 23: 581-590. 10.1002/art.1780230510.
Bohan A, Peter JB: Polymyositis and dermatomyositis. N Engl J Med. 1975, 292: 344-347. 10.1056/NEJM197502132920706.
Korea Central Cancer Registry, Ministry of Health and Welfare (South Korea): Annual Report of Cancer Statistics in Korea in 2008. Goyang-si, South Korea: National Cancer Center (South Korea); 2010. Available from ., [http://www.cancer.go.kr]
Ulm K: A simple method to calculate the confidence interval of a standardized mortality ratio (SMR). Am J Epidemiol. 1990, 131: 373-375.
Carsons S: The association of malignancy with rheumatic and connective tissue diseases. Semin Oncol. 1997, 24: 360-372.
Naschitz JE, Rosner I: Musculoskeletal syndromes associated with malignancy (excluding hypertrophic osteoarthropathy). Curr Opin Rheumatol. 2008, 20: 100-105. 10.1097/BOR.0b013e3282f1ecd4.
Zufferey P, Meyer OC, Grossin M, Kahn MF: Primary Sjögren’s syndrome (SS) and malignant lymphoma: a retrospective cohort study of 55 patients with SS. Scand J Rheumatol. 1995, 24: 342-345. 10.3109/03009749509095178.
Quartuccio L, Salvin S, Fabris M, Maset M, Pontarini E, Isola M, De Vita S: BLyS upregulation in Sjogren’s syndrome associated with lymphoproliferative disorders, higher ESSDAI score and B-cell clonal expansion in the salivary glands. Rheumatology (Oxford). 2013, 52: 276-281. 10.1093/rheumatology/kes180.
Bosello S, Youinou P, Daridon C, Tolusso B, Bendaoud B, Pietrapertosa D, Morelli A, Ferraccioli G: Concentrations of BAFF correlate with autoantibody levels, clinical disease activity, and response to treatment in early rheumatoid arthritis. J Rheumatol. 2008, 35: 1256-1264.
Petri M, Stohl W, Chatham W, McCune WJ, Chevrier M, Ryel J, Recta V, Zhong J, Freimuth W: Association of plasma B lymphocyte stimulator levels and disease activity in systemic lupus erythematosus. Arthritis Rheum. 2008, 58: 2453-2459. 10.1002/art.23678.
Bonifazi M, Tramacere I, Pomponio G, Gabrielli B, Avvedimento EV, La Vecchia C, Negri E, Gabrielli A: Systemic sclerosis (scleroderma) and cancer risk: systematic review and meta-analysis of observational studies. Rheumatology (Oxford). 2013, 52: 143-154. 10.1093/rheumatology/kes303.
Onishi A, Sugiyama D, Kumagai S, Morinobu A: Cancer incidence in systemic sclerosis: meta-analysis of population-based cohort studies. Arthritis Rheum. 2013, 65: 1913-1921. 10.1002/art.37969.
Shin A, Kim J, Park S: Gastric cancer epidemiology in Korea. J Gastric Cancer. 2011, 11: 135-140. 10.5230/jgc.2011.11.3.135.
Wong BC, Zhang L, Ma JL, Pan KF, Li JY, Shen L, Liu WD, Feng GS, Zhang XD, Li J, Lu AP, Xia HH, Lam S, You WC: Effects of selective COX-2 inhibitor and Helicobacter pylori eradication on precancerous gastric lesions. Gut. 2012, 61: 812-818. 10.1136/gutjnl-2011-300154.
Wu CY, Wu MS, Kuo KN, Wang CB, Chen YJ, Lin JT: Effective reduction of gastric cancer risk with regular use of nonsteroidal anti-inflammatory drugs in Helicobacter pylori-infected patients. J Clin Oncol. 2010, 28: 2952-2957. 10.1200/JCO.2009.26.0695.
Joseph CG, Darrah E, Shah AA, Skora AD, Casciola-Rosen LA, Wigley FM, Boin F, Fava A, Thoburn C, Kinde I, Jiao Y, Papadopoulos N, Kinzler KW, Vogelstein B, Rosen A: Association of the autoimmune disease scleroderma with an immunologic response to cancer. Science. 2014, 343: 152-157. 10.1126/science.1246886.
Park JK, Subhawong AP, Ziminski CM, Grader-Beck T: Dermatomyositis as the initial presentation of a large anaplastic T-cell lymphoma. J Clin Oncol. 2011, 29: e378-e380. 10.1200/JCO.2010.33.2528.
Radis CD, Kahl LE, Baker GL, Wasko MC, Cash JM, Gallatin A, Stolzer BL, Agarwal AK, Medsger TA, Kwoh CK: Effects of cyclophosphamide on the development of malignancy and on long-term survival of patients with rheumatoid arthritis: a 20-year followup study. Arthritis Rheum. 1995, 38: 1120-1127. 10.1002/art.1780380815.
Yang EV, Webster Marketon JI, Chen M, Lo KW, Kim SJ, Glaser R: Glucocorticoids activate Epstein Barr virus lytic replication through the upregulation of immediate early BZLF1 gene expression. Brain Behav Immun. 2010, 24: 1089-1096. 10.1016/j.bbi.2010.04.013.
Acknowledgements
This work was supported by 800-20120026 from the Seoul National University College of Medicine. We thank the Medical Research Collaborating Center (MRCC) for its assistance with statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Electronic supplementary material
13075_2014_428_MOESM1_ESM.doc
Additional file 1: Figure S1.: Study population. Table S1. Characteristics of dermatomyositis patients with cancer. (DOC 670 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chang, S.H., Park, J.K., Lee, Y.J. et al. Comparison of cancer incidence among patients with rheumatic disease: a retrospective cohort study. Arthritis Res Ther 16, 428 (2014). https://doi.org/10.1186/s13075-014-0428-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-014-0428-x