Abstract
Background
The Gran Chaco ecoregion is a well-known hotspot of several neglected tropical diseases (NTDs) including Chagas disease, soil-transmitted helminthiasis and multiparasitic infections. Interspecific interactions between parasite species can modify host susceptibility, pathogenesis and transmissibility through immunomodulation. Our objective was to test the association between human co-infection with intestinal parasites and host parasitaemia, infectiousness to the vector and immunological profiles in Trypanosoma cruzi-seropositive individuals residing in an endemic region of the Argentine Chaco.
Methods
We conducted a cross-sectional serological survey for T. cruzi infection along with an intestinal parasite survey in two adjacent rural villages. Each participant was tested for T. cruzi and Strongyloides stercoralis infection by serodiagnosis, and by coprological tests for intestinal parasite detection. Trypanosoma cruzi bloodstream parasite load was determined by quantitative PCR (qPCR), host infectiousness by artificial xenodiagnosis and serum human cytokine levels by flow cytometry.
Results
The seroprevalence for T. cruzi was 16.1% and for S. stercoralis 11.5% (n = 87). We found 25.3% of patients with Enterobius vermicularis. The most frequent protozoan parasites were Blastocystis spp. (39.1%), Giardia lamblia (6.9%) and Cryptosporidium spp. (3.4%). Multiparasitism occurred in 36.8% of the examined patients. Co-infection ranged from 6.9% to 8.1% for T. cruzi-seropositive humans simultaneously infected with at least one protozoan or helminth species, respectively. The relative odds of being positive by qPCR or xenodiagnosis (i.e. infectious) of 28 T. cruzi-seropositive patients was eight times higher in people co-infected with at least one helminth species than in patients with no such co-infection. Trypanosoma cruzi parasite load and host infectiousness were positively associated with helminth co-infection in a multiple regression analysis. Interferon-gamma (IFN-γ) response, measured in relation to interleukin (IL)-4 among humans infected with T. cruzi only, was 1.5-fold higher than for T. cruzi-seropositive patients co-infected with helminths. The median concentration of IL-4 was significantly higher in T. cruzi-seropositive patients with a positive qPCR test than in qPCR-negative patients.
Conclusions
Our results show a high level of multiparasitism and suggest that co-infection with intestinal helminths increased T. cruzi parasitaemia and upregulated the Th2-type response in the study patients.
Graphical Abstract

Similar content being viewed by others
Background
Chagas disease, with the protozoan Trypanosoma cruzi as aetiological agent, is a neglected tropical disease (NTD) and remains a major public health problem in the American continent. It is estimated that 5–7 million people are infected and approximately 30% of them will be potentially affected by the disease [1]. Diagnosis of chronic human infection with T. cruzi for clinical purposes is based on the composite outcome of two serological tests with antigens that detect different antibodies against T. cruzi [enzyme-linked immunosorbent assays, (ELISA), indirect hemagglutination assay (IHA) or indirect immunofluorescence (IIF)] plus a third test if discordant results are obtained. However, the use of an ELISA or an immunochromatographic test is recommended for seroepidemiological surveys [2, 3]. Several regional intergovernmental initiatives coordinated intensified efforts to control the main triatomine species of public health relevance through the domestic application of pyrethroid insecticides [4]. However, the emergence of pyrethroid resistance in T. infestans and other vector species and associated control failures have jeopardized these achievements [5,6,7].
The Gran Chaco ecoregion is a hotspot of chronic poverty, Chagas disease and intestinal helminth infections, including soil-transmitted helminthiasis (STH) [8]. Soil-transmitted parasitic nematodes of humans include Ascaris lumbricoides (roundworms), Trichuris trichiura (whipworms), Necator americanus and Ancylostoma duodenale (hookworms) and Strongyloides stercoralis. Disease pathology caused by STH infections, mainly associated with heavier worm burdens, shares several features: diarrhoea and abdominal pain, anaemia and impaired growth and physical development [9, 10]. STHs, not considered major causes of global mortality [11], are the main cause of disability, with almost 2 million annual disability-adjusted life years (DALYs) worldwide [12]. Examination of stool samples by several methods has been recommended for diagnosis of STH infections [13]. However, because of the intermittent larval excretion during S. stercoralis chronic infection, serodiagnosis is more sensitive than faecal-based methods. Sensitivity of serological tests for S. stercoralis diagnosis ranged between 75% and 94%, whereas specificity ranged between 92% and 100%, depending on the study population, serologic methods (IIF or ELISA), antigen and reference method employed [14].
Other intestinal parasites co-circulate in the Gran Chaco ecoregion [15,16,17,18,19,20,21]. Enterobius vermicularis mainly affects children asymptomatically or with perianal pruritus as the main symptom. A strong positive correlation was found between E. vermicularis infection and appendicitis [22]. Giardia sp. and Cryptosporidium spp. cause moderate-to-severe diarrhoea and can also be accompanied by colic and nausea [23]. Blastocystis spp., one of the most frequent protozoa infecting humans, was associated with abdominal discomfort, anorexia, diarrhoea and flatulence [23, 24]. Other studies have suggested that Blastocystis is a non-pathogenic protozoan, as it is frequently seen in healthy individuals (e.g. [23]).
Multiparasitism (i.e. co-infection by more than one parasite species in the same host) is the rule in co-endemic areas for several parasitic diseases. Interspecific interactions between concomitant parasite species can modify host susceptibility to other parasites, their pathology and transmission risk [25, 26]. These features have favoured a major shift towards a multi-host and multi-parasite paradigm in research and control of infectious diseases [27, 28]. The main suggested mechanism of interaction between parasite species is the modulation of the immune response [29, 30]. In general, helminth infections mainly activate Th2 and Th9 immune response plus regulatory cytokines [31], polarizing the host immune response and reducing the ability to carry out an effective Th1-type response against intracellular parasites such as T. cruzi, Toxoplasma gondii and Plasmodium sp. [32]. Th17 has an important role in the control of T. cruzi infection [33, 34].
Several studies have provided evidence of immunomodulation by intestinal helminths and filarial worms in humans, especially in co-infections with Plasmodium sp. [35,36,37]. Immunomodulation was suggested as the underlying mechanism in T. cruzi-seropositive dogs co-infected with Dirofilaria immitis, which showed less intense heart inflammatory response than helminth-free dogs [38]. Trypanosoma cruzi-seropositive children with concomitant intestinal infections had high parasite loads, and malnutrition/growth retardation was up to four times higher than the national average in El Salvador [39]. The seroprevalence of T. cruzi and the detectability of bloodstream parasite DNA were significantly higher in Latin American immigrants co-infected with S. stercoralis than in those without the helminth [40, 41].
In vector-borne diseases, host infectiousness is the ability of an infected host to infect the vector; this can be measured directly by xenodiagnosis or indirectly by host parasitaemia. For T. cruzi, host infectiousness measured by xenodiagnosis is strongly overdispersed in humans and domestic or wild mammals [42,43,44,45,46]. These patterns involve ‘superspreaders’, defined as a small fraction of the host population infecting disproportionately more susceptible contacts than most infected hosts [47]. The bloodstream parasite load measured by quantitative PCR (qPCR) in humans and domestic or wild mammals naturally infected with T. cruzi was positively associated with host infectiousness and supported the 80–20 rule [48, 49]. Concomitant parasitic infections may in part account for the observed heterogeneous distribution of parasitaemia and infectiousness in mammalian populations infected with T. cruzi.
Here, we tested whether human co-infections with T. cruzi and intestinal parasites modified host parasitaemia, infectiousness to the vector and immunological profiles in an endemic rural area of the Argentine Chaco. Immunological profiles were measured through serum levels of Th1 (interferon-gamma, IFN-γ), Th2 (interleukin 4, IL-4), Th17 (IL-17A) and IL-10 cytokines. Our hypothesis is that intestinal helminth co-infection modulates the immune response towards a Th2-type response and thus increases host parasitaemia and infectiousness to the vector. No study apparently has addressed this research question in patients residing in an endemic region.
Methods
Study area
This study is part of a broader research project on the transmission and control of Chagas disease in the Argentine Chaco. This project, launched in 2015, encompassed a rural-to-urban gradient in Avia Terai municipality (26° 42′ S 60° 44′ W), Chaco province, north-eastern Argentina. The main features of the study area were described elsewhere [50]. The urban setting had 1409 inhabited dwellings arranged in a 10 × 10 block matrix as of 2016. Peri-urban settings included 575 inhabited dwellings. The rural setting comprised 308 inhabited houses as of 2015. The intervention program against Triatoma infestans included a municipality-wide baseline assessment of house infestation with triatomines, house spraying with pyrethroid insecticides and periodic searches to assess house re-infestation between November 2016 and November 2019 [7]. After the triatomine control program was initiated, a cross-sectional serosurvey of human infection with T. cruzi and treatment campaign was carried out between June 2016 and August 2017 in cooperation with personnel from the only local hospital (Dr. Ezequiel P. Morante).
Study population
We conducted a cross-sectional serological survey for T. cruzi infection in which residents of two adjacent rural villages (Lote 9 and Lote 10) were invited to the nearest healthcare post or school for blood sample extraction. In parallel, intestinal parasite surveys were coupled with the T. cruzi serosurvey. A total of 87 individuals out of 415 residents voluntarily agreed to participate in both surveys. The exclusion criteria were: (i) being younger than 9 months of age, since maternal antibodies to T. cruzi may still be detectable; (ii) children younger than 18 years of age with no parent or guardian that provided written consent; and (iii) adults unable to give consent. In total, 28 T. cruzi-seropositive humans were included to evaluate host infectiousness, bloodstream parasite load and cytokines concentration profiles and its association with intestinal parasite co-infection. These included 9 out of 14 T. cruzi-seropositive humans from the serosurvey in Lote 9 and Lote 10 villages, and 19 T. cruzi-seropositive humans from other rural and urban areas in Avia Terai. The mean age of the 28 T. cruzi-seropositive humans was 27.9 years old (standard deviation, SD, 12.5) (Table 1), and approximately half of the patients were women. All humans seropositive for T. cruzi were in the chronic phase of the infection.
Following national guidelines, all T. cruzi-seropositive people aged ≤ 18 years were referred to the local hospital for aetiological treatment against T. cruzi. Local physicians also considered eligible for aetiological treatment seropositive people between 18 and 65 years of age who specifically requested to be treated.
Serosurvey
Up to 5 ml of blood were extracted by venipuncture from all participants aged more than 2 years. A retractile lancet was used for younger children and the maximum blood obtained was 0.5 ml. Blood samples were allowed to clot at room temperature for up to 3 h. Each serum was separated by centrifugation at 3000 rpm for 15 min and allocated in triplicate vials. Two aliquots were stored at −20 °C for serodiagnosis and one at −80 °C for cytokine quantification.
Serodiagnosis of Trypanosoma cruzi
Each participant was tested by a recombinant antigen enzyme-linked immunosorbent assay (ELISA Rec V3.0, Wiener) and by an indirect hemagglutination assay (IHA) (Polychaco, Buenos Aires, Argentina) or by an in-house IHA tested at the national reference centre for T. cruzi diagnosis; Instituto Nacional de Parasitología Dr. Mario Fatala Chabén (ANLIS-Malbrán, Buenos Aires, Argentina). Each sample was tested in duplicate in the ELISA test as reported [51]. Discordant samples were tested by an indirect immunofluorescence (IIF) at the national reference centre for final outcome. An individual was considered seropositive when reactive to at least two assays. At the time of performing routine tests prior to Chagas aetiological treatment, a 2 ml aliquot of blood was mixed with an equal volume of Guanidine-EDTA Buffer (GEB) for molecular diagnosis and quantification of the bloodstream load of T. cruzi, and 3 ml of blood was mixed with heparin for artificial xenodiagnosis.
Serodiagnosis of Strongyloides stercoralis
An in-house enzyme-linked immunosorbent assay was performed with the NIE antigen (NIE-ELISA) as described elsewhere [52]. Each sample was tested in duplicate. The cut-off was estimated by a standard curve using a positive serum control from S. stercoralis-infected humans. A serum sample from a non-infected human was used as a negative control. The cut-off was set at 120 units/mL, corresponding to a sensitivity and specificity of 75% and 95%, respectively [52]. Positive and negative control sera were run in each ELISA plate.
Artificial xenodiagnosis and host infectiousness
Artificial xenodiagnostic tests were performed with heparinized blood from T. cruzi-seropositive humans. For each test, 20 fourth-instar nymphs of laboratory-reared T. infestans (kept unfed for at least 3 weeks) were offered 3 ml of heparinized blood from each patient using a blood-feeding device [53]. The elapsed time between blood extraction and the onset of feeding was < 5 min. Each triatomine was individually examined for T. cruzi infection by optical microscopy at 400 × magnification at 30 days and 60 days after exposure. Host infectiousness was calculated as the total number of triatomines infected with T. cruzi divided by the total number of triatomines exposed to the infected host and examined for infection at least once.
Quantitative DNA amplification
All GEB samples were heated in boiling water for 10–15 min. Prior to DNA extraction, a bacterial commercial plasmid, pQE (Qiagen, Valencia, CA, USA), was added to a 400 μl GEB aliquot as an internal standard of DNA extraction, and DNA was extracted as reported [46]. Purified DNA was eluted in 200 μl of distilled water and used as template for qPCR amplification. An ABI 7500 thermocycler (Applied Biosystems, Carlsbad, CA, USA) was used to amplify a T. cruzi satellite DNA of 140 bp flanked by the Sat Fw and Sat Rv oligonucleotides, highly conserved in the parasite genome. Samples were run in duplicate. A standard curve reflecting a dynamic range of T. cruzi between 0.1 and 106 parasites/ml was used for DNA quantification as described elsewhere [54]. DNA quantification was normalized according to the Discrete Typing Units of T. cruzi [55]. We expressed parasite DNA concentration as equivalent amounts of parasite DNA per ml (Pe/ml). The cut-off value of this method was 0.14 Pe/ml [54]. Samples in which parasite DNA was not detected by qPCR were considered to have a zero parasite load per ml.
Stool sampling
The procedure for stool sample collection (at least three independent samples over seven consecutive days) was explained verbally to all patients, who were provided with labelled containers with 3 ml sodium acetate–acetic acid–formalin (SAF). Three glass slides with a cellophane adhesive tape for Graham’s test were given to patients for detection of E. vermicularis. Two sets of printed instructions were used to describe the stool and adhesive tape test collection [56].
Coprological examination and identification of intestinal parasites
Coprological examination was carried out by two concentration methods: a flotation test using a saturated sodium chloride solution (specific gravity 1.20 g/ml) and a modified sedimentation test employing washings with saline solution while avoiding the usual lipid extraction step [57]. We performed four independent observations for the sedimentation test (one of them iodine-stained), and one observation for the flotation technique with the addition of a drop of iodine. In both cases, all helminth eggs detected in each preparation were identified to genus by comparison with atlas photomicrographs [58]. For the detection of intestinal protozoa, a preparation was made for each faecal sample processed by the sedimentation protocol and adding a drop of iodine. The preparation was entirely examined by optical microscopy at 400 × to detect the presence of protozoa by comparison with atlas photomicrographs [58]. Cryptosporidium spp. oocysts were detected in stool smears by staining with a modified Ziehl–Neelsen stain [59]. Smears were examined by optical microscopy at 1000 × and oocysts recognized by the morphometric characteristics of fuchsia-stained spherical or ovoid elements (length, 4–6 μm). A patient was considered infected with a helminth species when an egg or larvae was detected by at least one method of enrichment (i.e. flotation or sedimentation), and/or infected with a protozoan when cysts or coccidian oocysts were observed. Infected patients were referred for aetiological treatment.
Multiplex assay for cytokine quantification
Human cytokine levels were measured in frozen serum samples using a bead-based multiplex assay, LEGENDplex™ Human Th Cytokine Panel (BioLegend, Inc., USA). We measured the levels of four cytokines: IFN-γ, IL-4, IL-10 and IL-17A. All samples were assayed according to the manufacturer’s instructions on a FACSAria II flow cytometer (BD Immunocytometry Systems). The concentration of each cytokine was determined using a standard curve, provided with the LEGENDplex™ kit, generated in the same assay. Serum samples were tested in duplicate in 96-well plates. The FCS files generated on the flow cytometer were analysed using BioLegend’s LEGENDplex™ Data Analysis Software.
Data analysis
Agresti–Coull binomial 95% confidence intervals (CI) were used for proportions [60]. The proportion of qPCR- and xenodiagnosis-positive humans co-infected or not with helminths (i.e. E. vermicularis and/or S. stercoralis) was analysed using Fisher’s exact test. A nominal significance level of 5% was considered. We used Kruskal–Wallis or Mann–Whitney tests to compare the median parasite load of T. cruzi and cytokine concentrations among groups.
We included the following parasite species to assess the relationship between parasite co-infections and host infectiousness and parasite load of T. cruzi-seropositive humans: E. vermicularis (number of humans infected, n = 8), S. stercoralis (n = 5), G. lamblia (n = 3), Cryptosporidium spp. (n = 1) and Blastocystis spp. (n = 8). These parasites exert detrimental health effects and modify the immune response of infected humans. We did not include other less frequent or non-pathogenic parasite species (e.g. Hymenolepis nana, Entamoeba histolystica/dispar, Dientamoeba fragilis). To reduce the number of independent variables, intestinal parasites were pooled in two groups on the basis of their phylogenetic relationship. One group included E. vermicularis and S. stercoralis (i.e. helminths; n = 10); the other group included the protozoa G. lamblia, Cryptosporidium spp. and Blastocystis spp. (n = 10), five of which co-occurred with at least a helminth species. Trypanosoma cruzi-seropositive humans not infected with any intestinal parasite (n = 13) functioned as a negative control group.
Multiple logistic regression analysis with robust standard errors, implemented in Stata (Stata 15, Stata Corp, College Station, Texas), was used to evaluate the association between T. cruzi infection-status and intestinal parasites infection categorized in two groups of parasites, that is, helminths and protozoa. The sample included the 87 humans tested in the serosurvey. The relationship between host infectiousness to the vector or parasite load (response variables) of T. cruzi-seropositive humans and selected predictors was tested through random-effects multiple logistic regression and linear regression with robust standard errors, respectively. The sample included 28 T. cruzi-seropositive humans. Because the triatomines used in xenodiagnosis were clustered on individual humans, observations are not independent. Two logistic regression models were tested for infectiousness in which the dependent variable was the infection status of each triatomine used in xenodiagnosis. The first model assessed whether host infectiousness was associated with bloodstream parasite load (a continuous variable) and included age of the host. The second model evaluated the relationship between host infectiousness and co-infection with at least one parasite from each group, taken as dichotomous variables: helminths (E. vermicularis and/or S. stercoralis), and protozoa (Blastocystis spp. and/or Cryptosporidium spp. and/or G. lamblia). The parasite load was log-transformed and a multiple linear regression with robust standard errors was performed with selected predictors. The age of the host (measured in months) was included in all regression analyses as a potential confounder. The interaction term between parasite groups was dropped from the final model for host infectiousness due to converging problems. The Wald test examined the hypothesis that all regression coefficients were 0. Multicollinearity was evaluated by the variance inflation factor (VIF); the mean VIF values (< 2) indicated the absence of significant collinearity.
The comparison of serum cytokine levels was carried out considering the following human infection-status groups: (i) humans not infected with any of the studied parasites (i.e. control group; n = 4); (ii) humans infected with T. cruzi only (n = 6); (iii) humans infected with helminths only (i.e. infected with E. vermicularis and/or S. stercoralis; n = 6); (iv) humans infected with protozoa only (i.e. Blastocystis spp. and/or Cryptosporidium spp. and/or Giardia sp., n = 8); (v) T. cruzi-seropositive humans co-infected with helminths (n = 4); (vi) T. cruzi-seropositive humans co-infected with protozoa (n = 5); and (vii) T. cruzi-seropositive humans co-infected with both helminths and protozoa (n = 5). The immune response was summarized into one variable “t” (Eq. 1) [61] to allow for quantitative comparisons between the different infection-status groups; “t” is defined as the relative concentration of IFN-γ, as a driver of Th1-type response, in relation to the concentration of IL-4, as a driver of Th2-type response, plus IFN-γ, that is, in the total cytokine pool [61]. Therefore, it measures whether the immune response is skewed towards a Th1 or Th2 profile, and takes values between 0 and 1. Similarly, the immune response can be estimated in relation to IL-10.
Results
Trypanosoma cruzi and intestinal parasite infection
The seroprevalence of T. cruzi was 16.1% among the 87 survey participants. Overall, 69.0% (60 of 87) of the individuals were infected with at least one intestinal parasite: 54.0% of them with intestinal protozoa, and 34.5% with helminths. The only three intestinal helminth species found by coprological or serological tests were E. vermicularis (25.3%), S. stercoralis (11.5%) and H. nana (1.0%). The enteropathogenic protozoa found were Blastocystis spp. (39.1%), G. lamblia (6.9%) and Cryptosporidium spp. (3.4%). We also detected Entamoeba hystolytica/dispar (8.0%), but the species identification remained inconclusive. We found other non-pathogenic protozoa such as Entamoeba coli (11.5%), Endolimax nana (16.1%), Iodamoeba bütschlii (5.7%) and Dientamoeba fragilis (11.5%) (Table S1).
Of the 87 study individuals, 74.7% were infected with at least one intestinal parasite species and/or T. cruzi. The prevalence of multiparasitism was 36.8%. The prevalence of co-infection with T. cruzi and a helminth was 8.1%. The prevalence of T. cruzi and S. stercoralis co-infection was 2.3%, and 5.8% for co-infection with T. cruzi and E. vermicularis. The prevalence of co-infection with T. cruzi and protozoa was 6.9%; 4.6% with Blastocystis spp., and 1.2% with G. lamblia. We found no T. cruzi-infected patient co-infected with Cryptosporidium spp. and H. nana. Multiple logistic regression showed that the relative odds of being seropositive for T. cruzi was significantly associated with age of host (OR 1.04; 95% CI 1.01–1.07, P < 0.01) and was not significantly associated with infection with a protozoa (OR 0.57; 95% CI 0.22–1.51, P = 0.26), helminth (OR 2.8; 95% CI 0.80–9.76, P = 0.95) or with a helminth and protozoa co-infection (OR 5.45; 95% CI 0.43–69.07, P = 0.19) (Wald χ2 = 10.71; P = 0.01).
Association between host infectiousness and parasitaemia in co-infections with intestinal helminths and protozoa
Of 28 T. cruzi-seropositive humans, 7 (25%, 95% CI 13–43) were positive by qPCR and xenodiagnosis with 100% concordance (Table 1). Among the 13 individuals seropositive for T. cruzi only, only 2 were qPCR-positive and xenodiagnosis-positive; 5 patients positive by qPCR and xenodiagnosis were co-infected with helminths, and 2 of these were also co-infected with protozoa. Therefore, having a detectable parasitaemia by qPCR or xenodiagnosis was significantly associated with a T. cruzi-helminth co-infection (Fisher’s exact test, df = 1, P = 0.03) (Table 1). The relative odds of having a positive test result by qPCR and xenodiagnosis was eight times higher in individuals co-infected with helminths than in those with no such co-infection (95% CI 1.35–47.41). Detectability of T. cruzi DNA by qPCR was also marginally significantly higher in patients co-infected with each one of the helminth species than in those with no co-infection. Three of five S. stercoralis co-infected patients (Fisher’s exact test, df = 1, P = 0.08; OR 7.13, 95% CI 1.04–48.58) and four of eight E. vermicularis co-infected ones were qPCR-positive (Fisher’s exact test, df = 1, P = 0.08; OR 5.67, 95% CI 1.00–32.26).
Trypanosoma cruzi parasite load and infectiousness to Triatoma infestans
The median parasite load of T. cruzi was 0.00 Pe/ml in all infection-status groups except for the group co-infected with at least one helminth (n = 5, median parasite load = 0.33 Pe/ml, Q1–Q3 = 0.00–0.74), which was marginally significantly higher than patients infected with T. cruzi only (Kruskal–Wallis test, df = 1, H = 2.04, P = 0.06) (Table 1). Log-parasite load was positively associated with a helminth co-infection (Coef. = 0.98, 95% CI −0.005 to 1.971, P = 0.05), but not with host age or co-infection with a protozoan (Table 2; P ˃ F = 0.04) in a multiple linear regression.
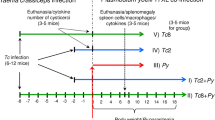
In the xenodiagnostic tests, bug mortality and moulting rates at 30 days of post-exposure to heparinized blood from seropositive humans were 8% and 10%, respectively, indicating they were of acceptable quality though less than before [45]. The mean infectiousness to the vector was 3.8% (n = 477 triatomines, 95% CI 2.4–5.9). Infectiousness significantly increased with T. cruzi parasite load (OR 6.54, 95% CI 1.47–29.14, P = 0.01) in an age-adjusted logistic regression (Wald χ2 = 6.23, P = 0.04). The mean infectiousness of the five patients co-infected with at least one helminth only was 12.4% (95% CI 6.9–21.3), which was 5.6-fold higher than in individuals in the negative control group, that is, T. cruzi-seropositive patients not co-infected with any intestinal parasite (2.2%, 95% CI 0.9–5.0) (Fig. 1). When all patients co-infected with helminths were included, the between-group difference was reduced to 3.6-fold (8.0%; 95% CI 4.6–13.3). People co-infected with protozoa were the least infectious (0.0%, 95% CI 0.0–4.3) and those co-infected with helminths and protozoa had a mean infectiousness of 3.7% (95% CI 1.3–10.2). Infectiousness was positively associated with being co-infected with at least one helminth (OR 20.83, 95% CI 1.37–316.78, P = 0.03), but not with a protozoan in a multiple logistic regression adjusted for age (Table 2; (Wald χ2 = 5.21, P = 0.16).
Mean infectiousness to T. infestans of T. cruzi-seropositive humans co-infected with intestinal parasite species. Avia Terai, Chaco, 2016–2017. The bars show mean host infectiousness of each group of individuals seropositive for T. cruzi and their co-infection status. The whiskers above each bar represent the 95% confidence interval, and the number of humans in each case is also indicated
Cytokine profiles
The median cytokine concentration among the 38 tested patients was 1.14 picograms/milliliters (pg/ml) (Q1–Q3 = 0.77–2.31) for IL-10, 11.04 pg/ml (Q1–Q3 = 3.67–30.58) for IL-4, 0.31 pg/ml (Q1–Q3 = 0.00–0.63) for IL-17A and 8.34 pg/ml (Q1–Q3 = 0.00–18.93) for IFN-γ. There was a strong positive correlation among the four cytokine concentrations (range of Pearson’s correlation coefficients, r: 0.81–0.95, Fig. 2), with the weakest between IL-17A and IFN-γ. Median cytokine concentrations were not significantly different among infection-status groups (Kruskal–Wallis, range of H = 1.62–3.68, df = 6, P = 0.67–0.95) (Table S2). However, the median concentrations of IL-10 and IL-4 were the highest among T. cruzi-seropositive patients co-infected with at least one helminth, followed by those co-infected with protozoa (Fig. 3; Table S2). The opposite pattern was observed for IFN-γ and IL-17A: the median concentration was higher among T. cruzi-seropositive humans co-infected with protozoa followed by those co-infected with helminths. The median Th1-type response, measured by the relative concentrations of IFN-γ among humans infected with T. cruzi only, was the lowest among human infection-status groups when it was relativized by IL-10 (range of t = 0.41–0.92), and 1.5-fold higher than for T. cruzi-seropositive patients co-infected with helminths when it was relativized by IL-4 (Table S2).
Higher median cytokine concentration values were observed in T. cruzi- positive patients by qPCR (n = 5) compared with those found in T. cruzi-negative patients by qPCR (n = 15), regardless of co-infection status with intestinal parasites. Significantly higher IL-4 concentrations occurred in qPCR-positive patients compared with qPCR-negative patients (30.58 pg/ml versus 6.52 pg/ml, Mann–Whitney U-test, Z = −2.06, P = 0.04), while there were marginally significant differences for IFN-γ (18.93 pg/ml versus 5.20 pg/ml, Mann–Whitney U-test, Z = −1.83, P = 0.07) and IL-17A levels (0.46 pg/ml versus 0.29 pg/ml, Mann–Whitney U-test, Z = −1.74, P = 0.08). Furthermore there was no significant differences for IL-10 concentrations (Mann–Whitney U-test, Z = −1.67, P = 0.10) (Table 3).
Discussion
Identifying factors and mechanisms that lead to overdispersed bloodstream parasite load in T. cruzi-infected host may provide a better understanding of vector-borne transmission dynamics and novel targeted control strategies. In this field study in the Argentine Chaco, we recorded nearly 75% of the study population infected with at least one intestinal parasite species and/or T. cruzi. As hypothesized, we found a positive association between the bloodstream parasite load of T. cruzi and co-infection with S. stercoralis and/or E. vermicularis. Infectiousness was higher in patients co-infected with T. cruzi and helminths, particularly when the co-infection excluded intestinal protozoa. Furthermore, T. cruzi-infected humans co-infected with helminths showed the highest Th2 immune response, suggesting it may exert a potential modulatory effect on T. cruzi parasitaemia.
Our study population resided in rural settings of northern Argentina, where the transmission of infectious diseases is strongly influenced by socio-economic and environmental factors characteristic of this ecoregion. In rural areas across Avia Terai municipality, other studies reported a high prevalence of house infestation with T. infestans (46%) and of houses harbouring T. cruzi-infected vectors (14%) [50, 62]. Rural households had characteristics suitable for transmission of intestinal parasites, such as lack of sanitary structures and access to safe drinking water, overcrowding and several unrestrained domestic animals that enhance the transmission of zoonotic intestinal parasites [63]. As NTDs and other infectious diseases share similar risk factors and there are potential interspecific interactions among parasite species, a multi-disease integrated approach may be necessary and cost-effective in regions with high co-endemicity [64, 65], as in the Gran Chaco.
Although we performed standard diagnostic methods that allow for the identification of several parasitic infections, the serological assay employed for S. stercoralis diagnosis (NIE-ELISA) has some limitations. In the first place, it is less reliable for acute infections or immunocompromised patients; cross-reactivity with other nematode infections may occur, and it cannot distinguish current from past infections. However, there are some points that suggest that seropositive patients were having a chronic S. stercoralis infection: (i) NIE-ELISA was among the first methods that revealed a seroreversion among five serological tests when infected patients underwent antihelminthic treatment [66]; (ii) infection with S. stercoralis could persist for years in the host because of autoinfection [67, 68]; and (iii) the study area is endemic for S. stercoralis and there has been no geohelminth management program to date.
In Avia Terai, the frequency of co-infections including T. cruzi and S. stercoralis (2%) was lower than elsewhere in northern Argentina (5%) [69]. We did not find a statistically significant association between these infections, nor did Fleitas et al. [69]. However, among Latin American expatriates, T. cruzi infection was more frequent in humans seropositive to S. stercoralis [41], and such co-infection was positively associated with eosinophilia [70]. The apparent lack of an association between human infection with T. cruzi and S. stercoralis or other intestinal parasites in co-endemic regions may perhaps be related to the inherent limitations of cross-sectional surveys for evaluating interspecific interactions between parasites [71, 72].
Half of the patients with T. cruzi infection were concomitantly infected with a pathogenic intestinal parasite. Patients co-infected with T. cruzi and S. stercoralis, or with T. cruzi and E. vermicularis, were more likely to harbour a detectable bloodstream parasite load by qPCR. This pattern agrees with previous results found in humans co-infected T. cruzi and S. strongyloides [40, 73], and here we expand it for humans co-infected with T. cruzi and E. vermicularis. Experimental animal models revealed an association between co-infection with intestinal helminths and Leishmania pathology or parasitaemia [74, 75]. Parasitaemia, qualitatively determined by blood culture, was higher in Golden lion tamarins naturally infected with T. cruzi and Trichostrongyloidae [76]. Similarly, a T. cruzi-helminth co-infection in dogs was associated with increased host parasitaemia and infectiousness [77].
Several studies have provided strong evidence that S. stercoralis may modulate disease severity in tuberculosis and was positively associated with higher bacterial burden [78,79,80,81]. Further, the low pathogenicity of E. vermicularis suggests it may have a low capacity to modulate the immune response of the infected host, and consequently, it would not affect the establishment or intensity of infection with other parasites. However, patients co-infected with Plasmodium malaria and E. vermicularis had higher parasitaemia and an increased risk of anaemia [82], supporting the hypothesis that helminth infections usually favour high microparasite loads. Accordingly, our results on T. cruzi-seropositive humans co-infected with two intestinal helminths suggest they may exert positive effects on host parasitaemia and infectiousness. If parasitaemia could be better controlled after deworming, this strategy may bring health benefits at the individual host and population levels by reducing the number and intensity of infectious hosts.
Co-infection with protozoa may also modulate the observed immune response. For example, Giardia spp. and Cryptosporidium spp. may affect the efficacy of vaccines against viral pathogens [83]. However, our results show that T. cruzi bloodstream parasite load and host infectiousness was not associated with Giardia spp. and/or Cryptosporidium spp. infection. This pattern was also reported for dogs co-infected with T. cruzi and Cryptosporidium spp. and/or Giardia spp. in the Argentine Chaco [77].
Patients co-infected with S. stercoralis and Mycobacterium tuberculosis had higher levels of Th2-type anti-inflammatory and regulatory cytokines (IL-4, IL-9, IL-10, TGF) and lower pro-inflammatory cytokine levels (IFN-γ, TNF- α, IL-2, IL-17) than patients infected with the mycobacteria only [78, 80]. Elevated plasma levels of IL-1β in association with anaemia, pyrexia and exacerbated parasitaemia occurred in patients co-infected with Plasmodium falciparum and E. vermicularis or multiple helminth species [82]. We found moderately higher concentrations of regulatory (IL-4 and IL-10) and pro-inflammatory (IFN-γ and IL-17A) cytokines in T. cruzi-seropositive humans co-infected with helminths or protozoa, respectively, compared with humans seropositive for T. cruzi only. Furthermore, IFN-γ response (measured in relation to IL-4) was lower for T. cruzi-seropositive humans co-infected with helminths than in patients infected with T. cruzi only. Altogether, we speculate that S. stercoralis and E. vermicularis infections exert an immunomodulatory phenomenon towards a Th2-type response in T. cruzi-infected patients inducing detrimental effects on the host’s ability to control parasitaemia with T. cruzi. A limitation of our study is the low number of serum samples evaluated for each infection/co-infection group; larger sample sizes are required to confirm the tendency found in serum cytokine levels.
Next, we analysed cytokine levels on the basis of the results of PCR and found that T. cruzi-infected patients with a positive qPCR had nearly five-fold higher levels of IL-4, a cytokine associated with Th2-type immune response respect to qPCR-negative patients. Th2-type IL-4 and IL-10 cytokines were crucial for downregulation of the pro-inflammatory response in T. cruzi infection [84, 85]. In experimental mouse models, increases of IL-4 were associated with increases of T. cruzi parasitaemia [86]; IL-4 depleted mice presented lower parasitaemia, associated with an increase of IFN-γ [87]. However, more research is required to determine whether the increase in IL-4 has a positive effect on the detection of patent parasitaemia in humans infected with T. cruzi, as well as to determine whether the concentration of IL-4 is due exclusively to the balance between the anti- and pro-inflammatory immune responses against T. cruzi infection or whether it is further exacerbated by co-infections with other parasite species. Our results support this last hypothesis, since the lowest levels of IFN-γ were found in relation to IL-4 in T. cruzi-seropositive patients co-infected with helminths. Interestingly, our study also recorded relatively elevated levels of IFN-γ and IL-17A in patients with patent parasitaemia by qPCR.
Amongst the strengths of our study are the collection of serial stool samples and the use of two concentration methods for parasitological diagnosis, use of differential staining to confirm the presence of Cryptosporidium spp. and use of ELISA for S. stercoralis diagnosis. However, we did not evaluate infection by virus or parasitic species with other locations in the human body, which may also influence host immune response affecting T. cruzi infection. One of the main limitations of this study is the low number of co-infected patients included. Despite the limited sample size, the difference in infectiousness and parasite load between infection-status groups was large enough to detect significant differences. By contrast, sample sizes were not sufficient to detect significant differences in serum cytokine levels. The stability of frozen cytokines, which is affected after 4 years of storage even at −80 °C [88], and differences in the balance of Th1/Th2/Th17/Treg adaptive immune responses between phase of the T. cruzi infection, that is, acute or chronic phase, asymptomatic patients and patients with the cardiac form of chronic Chagas disease [33, 34, 89], could also have added to the low discriminating power of the comparative analyses performed. The concentrations of the cytokines found in this study were close to or slightly below those found in other studies with parasitic infection, including patients with T. cruzi infection [90,91,92,93]. Imperfect detection in the qualitative and quantitative diagnostic methods can influence the results of analyses [94], especially in low concentrations, as it is the case of T. cruzi parasitaemia. However, the 100% of concordance between qPCR and xenodiagnosis test results suggest that the proportion of patients infected with T. cruzi who had detectable parasitaemia by these methods may be the true proportion of individuals with parasitaemia in the sample.
Conclusions
Our study revealed high levels of multiparasitism in the Argentine Chaco. The prevalence of intestinal helminths was high to moderate, mostly represented by E. vermicularis and S. stercoralis. Trypanosoma cruzi-seropositive patients co-infected with helminths displayed substantially higher parasitaemia levels and host infectiousness; this may have important implications for the epidemiology and control of vector-borne transmission of T. cruzi. Heterogeneities in infectiousness, vector-host contact rates and host susceptibility to infection increase the basic reproduction number of pathogens [49]. Identifying the small fraction of superspreaders would allow for the design of intervention strategies targeting the population subgroups with a higher risk of infection or with a greater potential contribution to transmission. Experimental removal of helminth infections in T. cruzi-seropositive patients may confirm the effect of co-infections on T. cruzi parasitaemia and infectiousness to the vector and provide more evidence on the role of immunomodulation as an underlying mechanism.
Availability of data and materials
The datasets supporting the conclusions of this article are included in the article (and its additional files).
Abbreviations
- ELISA:
-
Enzyme-linked immunosorbent assays
- GEB:
-
Guanidine–EDTA blood samples
- IAC:
-
Internal amplification control DNA
- IHA:
-
Indirect hemagglutination assay
- IIF:
-
Indirect immunofluorescence
- kDNA-PCR, SAT DNA-PCR:
-
PCR amplification of the minicircle of kinetoplast DNA and satellite DNA, respectively
- NTD:
-
Neglected tropical disease
- Pe:
-
Parasite equivalents
- qPCR:
-
Quantitative PCR
- SAF:
-
acetate–acetic acid–formalin
- STH:
-
Soil-transmitted helminthiasis
- Th:
-
T helper type immune response
References
Global Health Metrics. Chagas disease—Level 3 cause. https://www.thelancet.com/pb-assets/Lancet/gbd/summaries/diseases/chagas-disease.pdf. Accessed 16 Dec 2023.
Organization PAH. Guidelines for the diagnosis and treatment of Chagas diseases. Washington, D.C.: PAHO; 2019.
Kelly EA, Bulman CA, Gunderson EL, Irish AM, Townsend RL, Sakanari JA, et al. Comparative performance of latest-generation and FDA-cleared serology tests for the diagnosis of Chagas disease. Pritt BS, editor. J Clin Microbiol. 2021;59:e00158-e221.
Gürtler RE, Cecere MC. Chagas disease vector control. In: Guarneri A, Lorenzo M, editors. Triatominae: the biology of Chagas disease vectors. New York: Springer; 2021.
Lardeux F, Depickere S, Duchon S, Chavez T. Insecticide resistance of Triatoma infestans (Hemiptera, Reduviidae) vector of Chagas disease in Bolivia. Trop Med Int Health. 2010;15:1037–48.
Mougabure-Cueto G, Picollo MI. Insecticide resistance in vector Chagas disease: evolution, mechanisms and management. Acta Trop. 2015;149:70–85.
Gaspe MS, Cardinal MV, Fernández MP, Vassena CV, Santo-Orihuela PL, Enriquez GF, et al. Improved vector control of Triatoma infestans limited by emerging pyrethroid resistance across an urban-to-rural gradient in the Argentine Chaco. Parasit Vectors. 2021;14:437.
Hotez PJ. Ten global “hotspots” for the neglected tropical diseases. PLoS Negl Trop Dis. 2014;2014:2496.
Else KJ, Keiser J, Holland CV, Grencis RK, Sattelle DB, Fujiwara RT, et al. Whipworm and roundworm infections. Nat Rev Dis Primers. 2020;6:44.
W.H.O. Soil-transmitted helminth infections. 2023. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections. Accessed 19 Jun 2024.
Loukas A, Maizels RM, Hotez PJ. The yin and yang of human soil-transmitted helminth infections. Int J Parasitol. 2021;51:1243–53.
I.H.M.E.. Institute for health metrics and evaluation. Intestinal nematode infections—Level 3 cause. In: Globlal Health Metrics. 2024. https://www.healthdata.org/research-analysis/diseases-injuries-risks/factsheets/2021-intestinal-nematode-infections-level-3. Accessed 19 Jun 2024.
Khurana S, Singh S, Mewara A. Diagnostic techniques for soil-transmitted helminths–Recent advances. RRTM. 2021;12:181–96.
Bisoffi Z, Buonfrate D, Sequi M, Mejia R, Cimino RO, Krolewiecki AJ, et al. Diagnostic accuracy of five serologic tests for Strongyloides stercoralis infection. Siddiqui AA, editor. PLoS Negl Trop Dis. 2014;8:e2640.
Jara Castillo S, Riquelme Chavez F, Gonzalez Aponte N, Jara CE. Prevalencia de parasitosis intestinal, en niños de 6 a 12 años que acuden a las escuelas del proyecto barrios sostenibles de Calaverita y San José Olero de la ciudad de Concepción. RCUPAP. 2023;3:15–21.
Díaz V, Funes P, Echagüe G, Sosa L, Ruiz I, Zenteno J, et al. Estado nutricional-hematológico y parasitosis intestinal de niños escolares de 5 a 12 años de cuatro localidades rurales de Paraguay. Mem Inst Investig Cienc Salud. 2018;16:26–32.
Spinicci M, Macchioni F, Gabrielli S, Rojo D, Gamboa H, Villagrán AL, et al. Hymenolepis nana—An emerging intestinal parasite associated with anemia in school children from the Bolivian Chaco. Am J Trop Med Hyg. 2018;99:1598–601.
Aruni Chura J, Macchioni F, Furzi F, Balboa V, Mercado É, Gómez J, et al. Cross-sectional study on intestinal parasite infections in different ecological zones of the Department of La Paz. Bolivia One Health. 2021;13:100271.
Navone G, Zonta M, Cociancic P, Garraza M, Gamboa M, Giambelluca L, et al. Estudio transversal de las parasitosis intestinales en poblaciones infantiles de Argentina. Rev Panam Salud Publica. 2017;41:1–9.
Scavuzzo CM, Delgado C, Goy M, Crudo F, Porcasi X, Periago MV. Intestinal parasitic infections in a community from Pampa del Indio, Chaco (Argentina) and their association with socioeconomic and environmental factors. PLoS ONE. 2023;18:e0285371.
Gabrielli S, Macchioni F, Spinicci M, Strohmeyer M, Roselli M, Nicoletti A, et al. Long-standing international cooperation in parasitology research: a summary of 35 years of activities in the Bolivian Chaco. Tropical Med. 2022;7:275.
Taghipour A, Olfatifar M, Javanmard E, Norouzi M, Mirjalali H, Reza ZM. The neglected role of Enterobius vermicularis in appendicitis: a systematic review and meta-analysis. PLoS ONE. 2020;4:0232143.
Sardinha-Silva A, Alves-Ferreira EVC, Grigg ME. Intestinal immune responses to commensal and pathogenic protozoa. Front Immunol. 2022;13:963723.
Sheehan D, Raucher BG, Mkkitrick JC. Association of Blastocystis hominis with signs and symptoms of human disease. J Clin Microbiol. 1986;24:548–50.
Vaumourin E, Vourc’h G, Gasqui P, Vayssier-Taussat M. The importance of multiparasitism: examining the consequences of co-infections for human and animal health. Parasit Vectors. 2015;8:545.
Madinga J, Polman K, Kanobana K, Lieshout L, Brienen E, Praet N, et al. Epidemiology of polyparasitism with Taenia solium, schistosomes and soil-transmitted helminths in the co-endemic village of Malanga, Democratic Republic of Congo. Acta Trop. 2017;171:186–93.
Gibson AK, Raverty S, Lambourn DM, Huggins J, Magargal SL, Grigg ME. Polyparasitism is associated with increased disease severity in Toxoplasma gondii-infected marine sentinel species. PLoS Negl Trop Dis. 2011;5:e1142.
Bisanzio D, Mutuku F, Bustinduy AL, Mungai PL, Muchiri EM, King CH, et al. Cross-sectional study of the burden of vector-borne and soil-transmitted polyparasitism in rural communities of coast province. Kenya PLoS Negl Trop Dis. 2014;8:2992.
Telfer S, Birtles R, Bennett M, Lambin X, Paterson S, Begon M. Parasite interactions in natural populations: insights from longitudinal data. Parasitology. 2008;135:767–81.
Lafferty KD. Interacting parasites. Science. 2010;330:187–8.
Mosmann TR, Coffman RL. TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Rev Immunol. 1989;7:145–73.
Rodríguez M, Terrazas LI, Márquez R, Bojalil R. Susceptibility to Trypanosoma cruzi is modified by a previous non-related infection. Parasite Immunol. 1999;21:177–85.
Cristovão-Silva AC, Brelaz-de-Castro MCA, Hernandes MZ, Pereira VRA. Chagas disease: immunology of the disease at a glance. Cytokine Growth Factor Rev. 2021;62:15–22.
Koh CC, Neves EGA, De Souza-Silva TG, Carvalho AC, Pinto CHR, Galdino A, et al. Cytokine networks as targets for preventing and controlling Chagas heart disease. Pathogens. 2023;12:171.
Graham AL. Ecological rules governing helminth-microparasite coinfection. Proc Natl Acad Sci USA. 2008;105:566–70.
Wammes LJ, Hamid F, Wiria AE, May L, Kaisar MMM, Prasetyani-Gieseler MA, et al. Community deworming alleviates geohelminth-induced immune hyporesponsiveness. Proc Natl Acad Sci USA. 2016;113:12526–31.
Kathamuthu GR, Munisankar S, Banurekha VV, Nair D, Sridhar R, Babu S. Filarial coinfection is associated with higher bacterial burdens and altered plasma cytokine and chemokine responses in tuberculous lymphadenitis. Front Immunol. 2020;11:706.
Cruz-Chan JV, Quijano-Hernandez I, Ramirez-Sierra MJ, Dumonteil E. Dirofilaria immitis and Trypanosoma cruzi natural co-infection in dogs. Vet J. 2010;186:399–401.
Nolan MS, Murray KO, Mejia R, Hotez PJ, Villar Mondragon MJ, Rodriguez S, et al. Elevated pediatric Chagas disease burden complicated by concomitant intestinal parasites and malnutrition in El Salvador. Trop Med Infect Dis. 2021;6:72.
Salvador F, Sulleiro E, Piron M, Sánchez-Montalvá A, Sauleda S, Molina-Morant D, et al. Strongyloides stercoralis infection increases the likelihood to detect Trypanosoma cruzi DNA in peripheral blood in Chagas disease patients. Trop Med Int Health. 2017;22:1436–41.
Puerta-Alcalde P, Gomez-Junyent J, Requena-Mendez A, Pinazo MJ, Álvarez-Martínez MJ, Rodríguez N, et al. High prevalence of S. stercoralis infection among patients with Chagas disease: a retrospective case-control study. PLoS Negl Trop Dis. 2018;12:e0006199.
Schenone H, Rojas AM, Castillo D. Estudio comparativo de la sensibilidad y mortalidad de las ninfas III y IV de Triatoma infestans usadas en el xenodiagnóstico de pacientes crónicos. Bol Chil Parasitol. 2000;55:14–7.
Gürtler RE, Cecere MC, Lauricella MA, Cardinal MV, Kitron U, Cohen JE. Domestic dogs and cats as sources of Trypanosoma cruzi infection in rural northwestern Argentina. Parasitology. 2007;134:69–82.
Cardinal MV, Lauricella MA, Ceballos AL, Lanati L, Marcet PL, Levin MJ, et al. Molecular epidemiology of domestic and sylvatic Trypanosoma cruzi infection in rural northwestern Argentina. Int J Parasitol. 2008;38:1533–43.
Macchiaverna NP, Enriquez GF, Bua J, Fernández MP, Sartor PA, Gürtler RE, et al. Human infectiousness and parasite load in chronic patients seropositive for Trypanosoma cruzi in a rural area of the Argentine Chaco. Infect Genet Evol. 2020;78:104062.
Enriquez GF, Bua J, Orozco MM, Wirth S, Schijman AG, Gürtler RE, et al. High levels of Trypanosoma cruzi DNA determined by qPCR and infectiousness to Triatoma infestans support dogs and cats are major sources of parasites for domestic transmission. Infect Genet Evol. 2014;25:36–43.
Stein RA. Super-spreaders in infectious diseases. Int J Infect Dis. 2011;15:510–3.
Enriquez GF, Bua J, Orozco MM, Macchiaverna NP, Alvarado Otegui JA, Argibay HD, et al. Over-dispersed Trypanosoma cruzi parasite load in sylvatic and domestic mammals and humans from northeastern Argentina. Parasit Vectors. 2022;15:37.
Woolhouse MEJ. Quantifying transmission. Microbiol Spectr. 2017;5:279.
Gaspe MS, Fernández MP, Cardinal MV, Enriquez GF, Rodríguez-Planes LI, Macchiaverna NP, et al. Urbanisation, risk stratification and house infestation with a major vector of Chagas disease in an endemic municipality of the Argentine Chaco. Parasit Vectors. 2020;13:1–4.
Sartor P, Colaianni I, Cardinal MV, Bua J, Freilij H, Gürtler RE. Improving access to Chagas disease diagnosis and etiologic treatment in remote rural communities of the Argentine Chaco through strengthened primary health care and broad social participation. PLoS Negl Trop Dis. 2017;11:1–18.
Cimino RO, Fleitas P, Fernández M, Echazú A, Juarez M, Floridia-Yapur N, et al. Seroprevalence of the Strongyloides stercoralis infection in humans from Yungas rainforest and Gran Chaco region from Argentina and Bolivia. Pathogens. 2020;9:394.
Macchiaverna NP, Enriquez GF, Buscaglia CA, Balouz V, Gürtler RE, Cardinal MV. New human isolates of Trypanosoma cruzi confirm the predominance of hybrid lineages in domestic transmission cycle of the Argentinean Chaco. Infect Genet Evol. 2018;66:229–35.
Bua J, Volta BJ, Velazquez EB, Ruiz AM, Rissio AM, Cardoni RL. Vertical transmission of Trypanosoma cruzi infection: quantification of parasite burden in mothers and their children by parasite DNA amplification. Trans R Soc Trop Med Hyg. 2012;106:623–8.
Duffy T, Bisio M, Altcheh J, Burgos JM, Diez M, Levin MJ, et al. Accurate real-time PCR strategy for monitoring bloodstream parasitic loads in Chagas disease patients. PLoS Negl Trop Dis. 2009;3:e419.
Buyayisqui MP, Bordoni N, Garbossa G. Overcoming language and cultural barriers: a graphical communication tool to perform a parasitological screening in two vulnerable populations from Argentina. J Health Commun. 2013;18:92–104.
Garbossa G, Buyayisqui MP, Geffner L, López Arias L, Fournière S, Haedo AS, et al. Social and environmental health determinants and their relationship with parasitic diseases in asymptomatic children from a shantytown in Buenos Aires. Argentina Pathog Glob Health. 2013;107:141–52.
Ash L, Orihel T. Atlas de Parasitología humana. 5a ed. Editorial Médica Panamericana, Madrid, España; 2010.
Duré F, Flaibani N, Romero MC, Garbossa G. The architectural design of urban space and its influence in the communities of parasites in two areas of Buenos Aires city with different circulation dynamic of companion animals. Rev Argent Parasitol. 2013;1:21–32.
Brown LD, Cai TT, Das GA. Interval estimation for a binomial proportion. Stat Sci. 2001;16:101–17.
Graham AL. Use of an optimality model to solve the immunological puzzle of concomitant infection. Parasitol. 2001;122:61–4.
Alvedro A, Gaspe MS, Milbourn H, Macchiaverna NP, Laiño MA, Enriquez GF, et al. Trypanosoma cruzi infection in Triatoma infestans and high levels of human–vector contact across a rural-to-urban gradient in the Argentine Chaco. Parasites Vectors. 2021;14:35.
Ojeda BL. Prevalencia y riqueza específica de parásitos intestinales en humanos en el municipio de Avia Terai, Chaco. [Buenos Aires, Argentina.]: Universidad de Buenos Aires; 2022.
Brooker S, Kabatereine NB, Gyapong JO, Stothard JR, Utzinger J. Rapid mapping of schistosomiasis and other neglected tropical diseases in the context of integrated control programmes in Africa. Parasitology. 2009;136:1707–18.
W.H.O. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases. 2020.
Buonfrate D, Sequi M, Mejia R, Cimino RO, Krolewiecki AJ, Albonico M, et al. Accuracy of five serologic tests for the follow up of Strongyloides stercoralis infection. PLoS Negl Trop Dis. 2015;9:e0003491.
Olsen A, Van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis–The most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg. 2009;103:967–72.
Repetto SA, Ruybal P, Batalla E, López C, Fridman V, Sierra M, et al. Strongyloidiasis outside endemic areas: long-term parasitological and clinical follow-up after ivermectin treatment. Clin Infect Dis. 2018;66:1558–65.
Fleitas PE, Floridia-Yapur N, Nieves EE, Echazu A, Vargas PA, Caro NR, et al. Strongyloides stercoralis and Trypanosoma cruzi coinfections in a highly endemic area in Argentina. PLoS Negl Trop Dis. 2022;16:0010179.
Dopico E, Rando-Matos Y, Solsona L, Almeda J, Santos FLN, Vinuesa T. Infection by Strongyloides stercoralis in immigrants with Chagas disease: evaluation of eosinophilia as screening method in primary care. Trop Med Int Health. 2020;25:467–74.
Fenton A, Knowles SC, Petchey OL, Pedersen AB. The reliability of observational approaches for detecting interspecific parasite interactions: comparison with experimental results. Int J Parasitol. 2014;44:437–45.
Vaumourin E, Vourc’h G, Telfer S, Lambin X, Salih D, Seitzer U, et al. To be or not to be associated: power study of four statistical modeling approaches to identify parasite associations in cross-sectional studies. Front Cell Infect Microbiol. 2014;4:62.
Salvador F, Sulleiro E, Sánchez-Montalvá A, Martínez-Gallo M, Carrillo E, Molina I. Impact of helminth infection on the clinical and microbiological presentation of Chagas diseases in chronically infected patients. PLoS Negl Trop Dis. 2016;10:e0004663.
Flamme AC, Scott P, Pearce EJ. Schistosomiasis delays lesion resolution during Leishmania major infection by impairing parasite killing by macrophages. Parasite Immunol. 2002;24:339–45.
Lamb TJ, Graham AL, Le Goff L, Allen JE. Co-infected C57BL/6 mice mount appropriately polarized and compartmentalized cytokine responses to Litomosoides sigmodontis and Leishmania major but disease progression is altered. Parasite Immunol. 2005;27:317–24.
Monteiro RV, Dietz JM, Raboy B, Beck B, Vleeschouwer K, Baker A, et al. Parasite community interactions: Trypanosoma cruzi and intestinal helminths infecting wild golden lion tamarins Leontopithecus rosalia and golden-headed lion tamarins L. chysomelas (Callitrichidae, L1766). Parasitol Res. 2007;101:1689–98.
Enriquez GF, Garbossa G, Macchiaverna NP, Argibay HD, Bua J, Gürtler RE, et al. Is the infectiousness of dogs naturally infected with Trypanosoma cruzi associated with poly-parasitism? Vet Parasitol. 2016;223:186–94.
Anuradha R, Munisankar S, Bhootra Y, Jagannathan J, Dolla C, Kumaran P, et al. Systemic cytokine profiles in Strongyloides stercoralis infection and alterations following treatment. Infect Immun. 2016;84:425–31.
Kumar NP, Kathamuthu GR, Moideen K, Banurekha VV, Nair D, Fay MP, et al. Strongyloides stercoralis coinfection is associated with greater disease severity, higher bacterial burden, and elevated plasma matrix metalloproteinases in pulmonary Tuberculosis. J Infect Dis. 2020;222:1021–6.
Donovan J, Tram TTB, Phu NH, Hiep NTT, Van VTT, Mui DTH, et al. Influence of Strongyloides stercoralis coinfection on the presentation, pathogenesis, and outcome of tuberculous meningitis. J Infect Dis. 2022;225:1653–62.
Zenebe Y, Habtamu M, Abebe M, Tulu B, Atnafu A, Mekonnen D, et al. Intestinal helminth co-infection and associated factors among pulmonary tuberculosis patients in Africa and Asia: a systematic review and meta-analysis. BMC Infect Dis. 2023;23:739.
Ntonifor HN, Chewa JS, Oumar M, Mbouobda HD. Intestinal helminths as predictors of some malaria clinical outcomes and IL-1β levels in outpatients attending two public hospitals in Bamenda, North West Cameroon. PLoS Negl Trop Dis. 2021;15:e0009174.
Akoolo L, Rocha SC, Parveen N. Protozoan co-infections and parasite influence on the efficacy of vaccines against bacterial and viral pathogens. Front Microbiol. 2022;13:1020029.
Brodskyn CI, Barral-Netto M. Resposta imune humana na doença de Chagas. In: Brener Z, Andrade ZA, Manoel B-N, editors. Trypanosoma cruzi e Doença de Chagas. Rio de Janeiro; 2000.
Neves EGA, Koh CC, Padilha Da Silva JL, Passos LSA, Villani FNA, Dos Santos JSC, et al. Systemic cytokines, chemokines and growth factors reveal specific and shared immunological characteristics in infectious cardiomyopathies. Cytokine. 2021;148:155711.
Hoft DF, Lynch RG, Kirchhoff LV. Kinetic analysis of antigen-specific immune responses in resistant and susceptible mice during infection with Trypanosoma cruzi. J Immunol. 1993;151:7038–47.
Hiyama K, Hamano S, Nakamura T, Nomoto K, Tada I. IL-4 reduces resistance of mice to Trypanosoma cruzi infection. Parasitol Res. 2001;87:269–74.
Jager W, Bourcier K, Rijkers GT, Prakken BJ, Seyfert-Margolis V. Prerequisites for cytokine measurements in clinical trials with multiplex immunoassays. Immunol. 2009;10:1.
Quebrada Palacio LP, Fernández ER, Hernández-Vásquez Y, Petray PB, Postan M. Circulating T follicular helper cell abnormalities associated to different clinical forms of chronic Chagas disease. Front Cell Infect Microbiol. 2020;10:126.
Weatherhead J, Cortés AA, Sandoval C, Vaca M, Chico M, Loor S, et al. Comparison of cytokine responses in Ecuadorian children infected with Giardia, Ascaris, or both parasites. Am J Trop Med Hyg. 2017;96:1394–9.
Volta BJ, Bustos PL, González C, Natale MA, Perrone AE, Milduberger N, et al. Circulating cytokine and chemokine profiles of Trypanosoma cruzi-infected women during pregnancy and its association with congenital transmission. J Infect Dis. 2021;224:1086–95.
Salvador F, Sánchez-Montalvá A, Martínez-Gallo M, Sulleiro E, Franco-Jarava C, Sao Avilés A, et al. Serum IL-10 levels and its relationship with parasitemia in chronic Chagas disease patients. Am J Trop Med Hyg. 2020;102:159–63.
Khalaf MM, Hussein MH, Hafedh AA. Evaluation of IL-2, IL-4 and IL-10 levels in patients with giardiosis. Ann Parasitol. 2021;67:697–702.
Abad-Franch F, Valença-Barbosa C, Sarquis O, Lima MM. All that glisters is not gold: sampling-process uncertainty in disease-vector surveys with false-negative and false-positive detections. PLoS Negl Trop Dis. 2014;8:e3187.
Acknowledgement
We thank the local communities for their warm welcome and commitment to the intervention program; municipal authorities (René Pallares, José Ponce, Oscar Cáceres), Carlos Navarrete and Patricia Rosana Martinez from Avia Terai Hospital for providing field technicians and laboratory facilities; Alejandra Alvedro and Mariano Laiño (Laboratorio de Eco-Epidemiología, FCEN-UBA); and Clarisa Rodriguez (Avia Terai Hospital) by fieldwork assistance. We also thank Tamara Garcia (Universidad Nacional de Salta, IIET) for her collaboration in the laboratory.
Funding
This work was supported by Fundación Bunge y Born (2015–2018), Agencia Nacional de Promoción Científica y Tecnológica MVC (PICT 2014–2661) to G.F.E. (PICT 2018–03706); and Universidad de Buenos Aires to R.E.G. (UBACYT 20020130100843BA).
Author information
Authors and Affiliations
Contributions
Conceptualization: G.F.E., M.V.C. and M.P. Data curation: G.F.E., B.L.O. and N.P.M. Formal analysis: G.F.E., M.V.C., N.P.M., M.P. and R.E.G. Funding acquisition: G.F.E., R.E.G., M.V.C. Investigation: G.F.E., N.P.M., G.G., Q.P.L.P., O.B.L., J.B., M.S.G., R.C., R.E.G., M.P. and M.V.C. Methodology: G.F.E., N.P.M., G.G., Q.P.L.P., O.B.L., J.B., M.S.G., R.C., M.P. and M.V.C. Project administration: G.F.E., M.V.C. and R.E.G. Resources: G.F.E., R.E.G. and M.V.C. Supervision: G.F.E., M.V.C. and R.E.G. Validation: G.F.E., N.P.M. and R.E.G. Visualization: G.F.E. Writing–original draft: G.F.E. Writing–review and editing: G.F.E., N.P.M., G.G., Q.P.L.P., O.B.L., J.B., M.S.G., R.C., R.E.G., M.P. and M.V.C.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol for human serological and coprodiagnosis and etiological treatment was approved by the Comité de Ética en Investigación Clínica (CEIC) (Ethical Committee for Clinical Research), Buenos Aires, Argentina (IRB no. 00001678; Protocol no. TW–01–004).
Consent for publication
All authors of this manuscript have read and agreed to the content within it. Furthermore, the contents of this article are original, and we agree with the BioMed Central Copyright and License Agreement.
Competing interests
Authors declare no conflicts of interest. The funding source has not been involved in study design, analysis and interpretation of data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Frequency and prevalence of intestinal parasites found in humans from Avia Terai, Chaco, 2016–2017.
Additional file 2: Table S2.
Cytokine concentration profiles of the study human population (n = 38) according to infection status groups. Avia Terai, Chaco, 2016–2017.
Additional file 3:
Dataset. Results per individual (Database).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Enriquez, G.F., Macchiaverna, N.P., Garbossa, G. et al. Humans seropositive for Trypanosoma cruzi co-infected with intestinal helminths have higher infectiousness, parasitaemia and Th2-type response in the Argentine Chaco. Parasites Vectors 17, 340 (2024). https://doi.org/10.1186/s13071-024-06401-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-024-06401-7