Abstract
Background
The high prevalence of metabolic syndrome in low- and middle-income countries is linked to an increase in Western diet consumption, characterized by a high intake of processed foods, which impacts the levels of blood sugar and lipids, hormones, and cytokines. Hematophagous insect vectors, such as the yellow fever mosquito Aedes aegypti, rely on blood meals for reproduction and development and are therefore exposed to the components of blood plasma. However, the impact of the alteration of blood composition due to malnutrition and metabolic conditions on mosquito biology remains understudied.
Methods
In this study, we investigated the impact of whole-blood alterations resulting from a Western-type diet on the biology of Ae. aegypti. We kept C57Bl6/J mice on a high-fat, high-sucrose (HFHS) diet for 20 weeks and followed biological parameters, including plasma insulin and lipid levels, insulin tolerance, and weight gain, to validate the development of metabolic syndrome. We further allowed Ae. aegypti mosquitoes to feed on mice and tracked how altered host blood composition modulated parameters of vector capacity.
Results
Our findings identified that HFHS-fed mice resulted in reduced mosquito longevity and increased fecundity upon mosquito feeding, which correlated with alteration in the gene expression profile of nutrient sensing and physiological and metabolic markers as studied up to several days after blood ingestion.
Conclusions
Our study provides new insights into the overall effect of alterations of blood components on mosquito biology and its implications for the transmission of infectious diseases in conditions where the frequency of Western diet-induced metabolic syndromes is becoming more frequent. These findings highlight the importance of addressing metabolic health to further understand the spread of mosquito-borne illnesses in endemic areas.
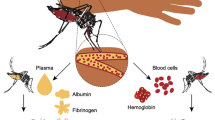
Graphical Abstract

Similar content being viewed by others
Background
The World Health Organization has identified obesity as one of the most serious public health challenges of the twenty-first century, with > 650 million adults worldwide being classified as obese [1]. This epidemic is largely driven by the global increased consumption of Western diets [2], characterized by a high intake of processed foods, added sugars, unhealthy fats, and a low intake of fruits, vegetables, and whole grains [3]. In low- and middle-income countries (LMIC), Western dietary patterns often correlate with economic transition in high socioeconomic families [4] and the increased affordability of cheap, calorie-dense processed foods compared to fresh, whole foods in the lower socioeconomic strata [5, 6]. These dietary habits result in alterations of blood composition, including levels of inflammatory cytokines, lipids, glucose, and other blood components. As such, Western diets are predisposing factors for developing obesity, type 2 diabetes, and other non-communicable diseases, such as cardiovascular diseases—the leading cause of death globally [7]. The simultaneous occurrence of these conditions is defined as metabolic syndrome [8].
Mosquito-borne illnesses like malaria, transmitted by Anopheles sp., or dengue, and Zika, primarily transmitted by Aedes aegypti, are major threats in tropical LMIC areas of the world [9]. The transmission of these diseases is strictly linked to the ingestion of blood by mosquitoes. This is a necessary step for pathogen development in the mosquito host and transmission following the pathogen cycle in the mosquito. Blood ingestion and digestion trigger nutrient sensing pathway-dependent physiological response [10,11,12] that must be tightly coordinated through several organs to coordinate energetic balance and immune status [13]. Mosquito vitellogenesis is also coordinated during this process. Here, a blood meal triggers a 20-hydroxyecdysone (20E) hormonal cascade [14], which drives the expression of the yolk protein precursor gene vitellogenin under the control of target of rapamycin (TOR) [15] and insulin signaling pathways [16]. Concurrently, the lipid transport protein lipophorin [17] mobilizes triglycerides [18] from the fat body toward the ovaries.
Previous studies have highlighted that individual components of the blood plasma can regulate this balance and influence vector biology and immunity. For example, it has been shown that human insulin and IGF1 supplementation during artificial meals can activate AKT and ERK-dependent pathways and reduce mosquito longevity [19] and immunity [20, 21]. A negative impact on Plasmodium infection levels has also been observed in Anopheles fed with a TGFß-1 supplemented blood meal [22]. In Aedes, other blood components, such as glucose, have also been shown to modulate mosquito vector capacity through AKT/TOR [23]. However, artificial single-point alterations of blood composition rarely reflect the blood's physiological modulations where several components are found altered because of metabolic syndromes and altered physiological states [24, 25]. In that sense, the impact of metabolic syndromes and nutritional imbalance, such as those derived from Western-type diets on mosquito biology, remains mostly unknown.
In this study, we investigated how blood alterations derived from a Western diet affect Aedes aegypti biology and several components of vector capacity. To do this, we fed mice a high-fat high-sucrose (HFHS) diet for 20 weeks, inducing weight gain, insulin resistance, and other metabolic syndrome-related conditions, and allowed mosquitoes to feed on these animals. Our findings identified an impact on mosquito longevity and fitness because of the ingestion of blood from mice with metabolic syndrome. Albeit a discrete impact on the overall transcriptional profile, we identified markers that were modulated because of the vertebrate host metabolic status. Our study provides new insights into the overall effect of alterations of blood components on mosquito biology and may have implications for the transmission of infectious diseases in conditions where the frequency of Western diet-induced metabolic syndromes is becoming more frequent. These findings highlight the importance of addressing metabolic health to further understand the spread of mosquito-borne illnesses.
Methods
Aedes aegypti rearing
The Ae. aegypti Red Eye strain used in this study has been kept at Universidade Federal do Rio de Janeiro since 2000. For this study, 100–150 larvae were reared in 1L of filtered water at 27 ± 1 °C with a 12 h:12 h light:dark cycle. Larvae were fed 1.5 g of Pedigree dog chow. Pupae were collected and placed in a 3-L plastic cage for adult emergence, maintained at 27 ± 1 °C and 70% relative humidity with a 12 h:12 h light:dark cycle. Adults were fed a 10% sucrose solution and allowed to mate in the cage before being used for experiments.
Mice diet
Six-week-old C57Bl6/J mice were used and were kept under controlled conditions (24 ± 1 °C; 55 ± 15% humidity; and 12 h/12 h light/dark cycle) during the 20-week protocol. After the acclimation period, animals were randomly divided into two groups of 40 animals each; one group was given a chow AIN93M diet (control group) and the other to a HFHS diet (HFHS group). The composition of CHOW and HFHS diets [26] is presented in Additional file 1: Table S1. Mice were allowed to feed and drink water ad libitum during the entire protocol.
Weight monitoring, insulin, and glucose tolerance tests
Throughout the 20-week dietary intervention, animals' body weights were measured weekly using a digital balance. In the 12th and 20th week of the protocol, animals underwent an oral glucose tolerance test (oGTT) to assess their responsiveness to the diet. In the 19th week, an insulin tolerance test (ITT) was performed to evaluate insulin resistance. At the end of the 20 weeks of intervention, the animals were killed, and their serum was collected and stored. The oGTT and ITT were performed as previously described [27]. Briefly, animals were fastened for 5 h before performing the tests. For oGTT, a dextrose solution was administered at a dose of 2 g per kilogram of body weight for each mouse. For ITT, 0.5 U of insulin (Humalin R, Eli Lilly, Indianapolis, IN, USA) per kilogram of body weight for each mouse was intraperitoneally injected. Blood samples were collected from the caudal vein immediately just before the start of the procedure and 15, 30, 60, and 120 min after administration of a single dose of dextrose or insulin. Glycemia was evaluated using a FreeStyle Precision Neo glucometer (Abbott Laboratories, Chicago, IL, USA). To measure liver cholesterol and triglycerides, Folch's method was used as described previously [28], and plasma insulin levels were assessed by ELISA using the Insulin Mouse ELISA Kit (ThermoFisher), following manufacturer instructions. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were evaluated as a marker of liver damage, as previously described [29].
Mosquito feeding on mice
To assess the effect of the altered blood composition in mice with metabolic syndromes on mosquito biology, we allowed mosquitoes to feed directly on 6.66 mg/kg xylazine and 66.6 mg/kg ketamine anesthetized mice [30, 31]. Sugar sources were removed from the mosquito environment the night before offering the mice to ensure a higher propensity for blood feeding. Biological replicates were prepared using independent hatches of mosquitoes and mice from independent dietary protocols.
Groups of mosquitoes, aged between 5 and 6 days, and numbering between 50 and 80 individuals, were allowed to feed for 30 min. After this period, unfed or not fully engorged mosquitoes were identified by visual inspection and were removed from the mosquito cages. Mosquitoes fed on CHOW mice were used as control groups. Mosquito survival was monitored daily for 30 days post blood meal (pbm), and the survival curve was analyzed. Sugar-fed (SF) mosquitoes from the same hatch and age were not allowed to feed on blood and were used as a baseline group. To allow mosquitoes to lay eggs, we placed a moistened paper filter inside the mosquito cages at day 5 pbm. To maintain consistent moisture, the filter paper was positioned on small plastic contained above a column of water to prevent filter drying during the period. The mosquitoes were allowed to lay eggs for 48 h before the filter was removed and dried, and the total mass was weighted [32] and normalized by the total number of mosquitoes present inside the cage at the moment the filter paper was placed.
Lipid quantification
Following blood feeding on mice, mosquitoes were collected between 1 and 4 days pbm and anesthetized by exposure to cold for 60 s. Mosquitoes were dissected to obtain separated ovaries and abdominal body wall samples, which were further homogenized in PBS using pools of 15 mosquitoes. For the analysis of the triacylglycerol content, the enzyme system Triglycerides 120 (Doles Reagentes®, Goiânia, Brazil) was used, according to the manufacturer's protocol; 1 μl homogenized tissues (ovaries and abdominal body wall) were mixed with 200 μl enzyme reagent and incubated at 37 °C for 30 min. Absorbance was measured at 510 nm (Emax®Plus-Microplate Reader. Molecular Devices, CA-USA).
Gene expression
To analyze gene expression, mosquitoes were collected from experimental and control mice at days 1 and 4 pbm, comprising the peak of the blood digestion process and its terminus, respectively [33, 34]. SF mosquitoes from the same hatch were not allowed to feed on blood and were used as a baseline group. SF mosquitoes were dissected and processed on the same day that day 1 pbm mosquitoes were. Briefly, RNA was extracted from the pools of 15–20 whole mosquitoes using the Trizol reagent (Invitrogen) following the manufacturer's protocol. cDNA synthesis was performed using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems). Quantitative real-time PCR (qRT-PCR) was performed using SyGreen (Applied Biosystems) and the StepOnePlus Real-Time PCR System (Applied Biosystems). The qRT-PCR cycling conditions were as follows: 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s, 60 °C for 30 s, and 72 °C for 30 s. Gene expression levels were analyzed using the ∆Ct method, and the data were normalized to the expression level of the housekeeping gene rp49. We measured expression of genes of (1) lipid metabolism: fatty acid synthase I (FASI) (AAEL001194), lipid storage droplet surface-binding protein 1 (LSD1) (AAEL005951), lipid storage droplet surface-binding protein 2 (LSD2) (AAEL006820); (2) glucose or energetic metabolism: pyruvate kinase (AAEL014913), glycogen synthase (AAEL004221), PINK1 (AAEL011594); (3) vitellogenesis: apolipophorin (AAEL009955), vitellogenin A1 (AAEL010434); (4) TOR pathway: target of rapamycin (TOR) (AAEL020638); (5) insulin pathway: insulin receptor (AAEL002317), forkhead box O (FoxO) (AAEL019672); (6) epidermal growth factor receptor (EGFR) pathway: Keren (AAEL010067), Vein (AAEL012977); (7) Janus kinase/signal transducers and activators of transcription (JAK/STAT) pathway: signal transducer and activator of transcription (STAT) (AAEL009692), Domeless (AAEL012471), protein inhibitor of activated STAT (PIAS) (AAEL015099); (8) c-Jun N-terminal kinase (JNK) pathway: c-Jun N-terminal kinase (JNK) (AAEL008622 and AAEL008634), Kayak (AAEL008953); (9) cell death/autophagy: autophagy-related protein 8 (ATG8) (AAEL007162); (10) ROS detoxification: catalase (AAEL013407-RB); glutathione peroxidase (AAEL012069); oxidation resistance 1 (AAEL021746); microbiota: Universal 16S. Primer sequences are described in Additional file 1: Table S2.
Results
A long-term dietary intervention mimicking Western diets induced insulin resistance and weight gain in mice
To investigate the effect of the Western Diet on Aedes mosquito biology, we kept C57Bl6/J mice under an HFHS diet for 20 weeks. We monitored the progression of weight gain and performed glucose tolerance (oGTT) and insulin tolerance (ITT) tests over the course of the dietary intervention. The consumption of the HFHS diet resulted in a significant increase in body weight (11.96 g vs. 20.85 g, P < 0.0005) (Fig. 1a). Accordingly, the HFHS diet induced glucose (6542 AU vs. 11,795 AU, P < 0.05) (Fig. 1b) and insulin intolerance (14,634 AU vs. 22,901 AU, P < 0.01) (Fig. 1c), as detected by glucose clearance following glucose and insulin administration by gavage. To further analyze metabolic alterations produced in mice following an HFHS diet, we quantified metabolites in the blood plasma after the 20-week intervention. Our results show that HFHS mice had increased insulin (13.32 μUI/ml vs. 26.65 μUI/ml, P < 0.0001), glucose (1.90 µg/µl vs. 2.58 µg/µl, P < 0.05), TAG (1.40 µg/µl vs. 2.72 µg/µl, P < 0.05), and cholesterol (2.54 µg/µl vs. 4.12 µg/µl, P < 0.05) levels in the blood compared to the CHOW control mice (Fig. 1d–g). Additionally, we found that the aspartate aminotransferase (AST) and alanine aminotransferase (ALT) ratio—a marker for liver damage—was significantly increased in the HFHS group (0.79 UI/l vs. 1.88 UI/l, P < 0.01) (Fig. 1h). These findings indicate that an HFHS 20-week dietary intervention successfully induced metabolic changes compatible with those found in metabolic syndrome.
A 20-week HSHF dietary intervention induced metabolic syndrome symptoms in C57 mice. Mice were fed with either a CHOW or an HSHF diet for 20 weeks. Over the course of the experiment, A weight gain was monitored weekly, while B insulin and C glucose tolerance were evaluated in the 19th and 20th weeks, respectively. By the end of the dietary intervention, blood was collected, and D insulin, E glucose, F triglycerides, G total cholesterol, and H AST/ALT levels were measured. At least six mice were used in each experiment (A–H). Unpaired t-test was performed. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Blood alterations induced by the HFHS diet result in reduced lifespan and increased egg production and triacylglycerol allocation after mosquito ingestion
We investigated the impact of blood alterations resulting from a Western-type diet on the biology of the yellow fever mosquito Ae. aegypti by allowing mosquitoes to feed directly on anesthetized mice. Mosquito survival was daily monitored for 30 days, and the survival curve was analyzed. Blood feeding negatively impacted the 30-day survival rates of mosquitoes compared to sugar feeding (P < 0.05). This effect was enhanced when mosquitoes were fed on HFHS-fed mice resulting in an increase in the total number of dead mosquitoes by the end of the period (P < 0.001) (Fig. 2a). We looked for differences in the expression of markers of the TOR and insulin pathway, two nutrient-sensing pathways that have a role in the regulation of the aging process [35, 36]. While we could not identify statistical differences in the expression of TOR (Fig. 2b) and insulin receptor (Fig. 2c), we found that forkhead box O (FoxO) (Fig. 2d), a negative regulator of the insulin pathway [37, 38], was downregulated in mosquitoes fed on HFHS blood compared to CHOW-fed mosquitoes 4 days pbm (0.432 vs. 0.240 relative to RP49, P < 0.05).
Mosquitoes fed on an HFHS mouse had a reduced survival rate. Mice were fed with either a CHOW or an HSHF diet for 20 weeks. Over the course of the experiment, metabolic syndrome was followed by tracking weight gain, glucose, and insulin sensitivity. Then, Aedes mosquitoes were allowed to feed on anesthetized mice, and A daily survival was measured over the course of 30 days. Alternatively, whole-body relative expression levels of B TOR, C insulin receptor, and D FoxO was measured by qRT-PCR 1 and 4 days pbm. Four biological replicates were prepared using independent mosquito hatches and dietary protocols. Sugar-fed (SF) mosquitoes were used as a baseline for survival and gene expression. A Mantel-Cox test and B–D one-way ANOVA followed by Tukey’s multiple comparison tests were performed. ns: non-significant, *P < 0.05, ***P < 0.001
We also investigated the impact of mice diet on egg production by Ae. aegypti females. For that, we allowed mosquitoes to lay eggs on a filter paper at 5 days pbm. Mosquitoes fed on HFHS mice had an increased reproductive output compared to CHOW-fed mosquitoes (0.00034 g/mosquito vs. 0.00059 g/mosquito, P < 0.01) (Fig. 3a). We further dissected mosquitoes fed on either CHOW or HFHS mice to quantify fat body lipid reserves' buildup and mobilization into the ovaries following a blood meal. We found that triacylglycerol (TAG) content in the fat body was increased in mosquitoes fed on HFHS-fed mice compared to CHOW-fed mice 2 days pbm (4.23 µg/µl vs. 13.30 µg/µl, P < 0.05) (Fig. 3b). This was followed by an increase in TAG content in the ovaries 3 days pbm (36.50 µg/µl vs. 61.67 µg/µl, P < 0.001) (Fig. 3c). Increased egg mass and TAG deposition did not correlate with alterations in the expression of lipophorin (Fig. 3d) and vitellogenin (Fig. 3e)—the major lipid transporters in the hemolymph [17] and the major egg yolk protein [39], respectively. However, feeding on HFHS mice resulted in an apparent early activation of in fatty acid synthase I whole-body expression levels at day 1 pbm, followed by a modest increase in lipid storage protein 2 levels at day 4 pbm (Additional file 1: Fig. S1A–C). We did not detect any major regulation of genes involved in glucose oxidation or metabolism, including pyruvate kinase, glycogen synthase, or PINK1—a marker of mitochondrial turnover (Additional file 1: Fig. S1D–F).
Mosquitoes fed on an HFHS mouse had an increased oviposition and lipid uptake. Mice were fed with either a CHOW or an HSHF diet for 20 weeks. Over the course of the experiment, metabolic syndrome was followed by tracking weight gain, glucose, and insulin sensitivity. Aedes aegypti mosquitoes were allowed to feed on anesthetized mice, and A egg layering was measured at 5 days pbm. Following a blood meal, mosquitoes were dissected, and TAG content was measured in the B fat body and C ovaries at 2 and 3 days pbm, respectively. Whole-body relative expression levels of D lipophorin and E vitellogenin were measured by qRT-PCR 1 and 4 days pbm. Sugar-fed (SF) mosquitoes were used as a baseline for gene expression. Four biological replicates were prepared using independent mosquito hatches and dietary protocols. A–C Unpaired t-test was performed and D–E one-way ANOVA followed by Tukey’s multiple comparison tests were performed. ns: non-significant, *P < 0.05, **P < 0.01, ***P < 0.001
Blood alterations induced by HFHS-diet on Ae. aegypti homeostatic markers
We aimed to investigate how feeding on HFHS mice impacted mosquito physiology by analyzing different markers of homeostatic regulation at days 1 and 4 pbm—a period comprising the peak of blood digestion and its terminus [33, 34]. We quantified the expression levels of markers of the EGFR pathway—a regulator of cellular proliferation, differentiation, and survival, which has been shown to be activated by insulin following blood feeding in Aedes sp. [40] and to play a role in gut regeneration in Drosophila [41]. We observed an early expression of the Aedes homologs of the Drosophila EGFR ligand Keren [42] in HFHS mosquitoes at day 1 pbm (0.06 vs. 0.018 relative to RP49, P < 0.05) (Fig. 4a). A similar profile was observed with the Aedes homologs of the Drosophila EGFR ligand Vein [43] (0.002 vs. 0.007 relative to RP49, P < 0.01) (Fig. 4b). The EGFR and JAK/STAT pathways have been shown to co-coordinate embryonic development in Drosophila [44], and a co-regulation of the JAK/STAT and EGFR pathway has also been implicated in gut regeneration in Ae. albopictus [45]. Interestingly, we observed a decrease in STAT—a JAK/STAT pathway transcription factor [46]—in HFHS mosquito day 1 pbm (0.347 vs. 0.108 relative to RP49, P < 0.01) (Fig. 4c). However, no difference in expression levels was observed in Domeless and PIAS—the JAK/STAT pathway receptor and its inhibitor, respectively [47] (Fig. 4d, e).
Mosquitoes fed on an HFHS mouse display a discrete regulation of metabolic markers and nutrient-sensing regulators. Mice were fed with either a CHOW or an HFHS diet for 20 weeks. Over the course of the experiment, metabolic syndrome was followed by tracking weight gain, glucose, and insulin sensitivity. Then, mosquitoes were allowed to feed on anesthetized mice, and whole-body relative expression levels of A Keren, B Vein, C STAT, D Domeless, E PIAS, F JNK-AAEL008622, G JNK-AAEL008634, H Kayak, and I caspase 16 were measured by qRT-PCR 1 and 4 days pbm. Sugar-fed (SF) mosquitoes were used as a baseline for gene expression. Four biological replicates were prepared using independent mosquito hatches and dietary protocols. A–I One-way ANOVA followed by Tukey’s multiple comparison tests was performed. ns: non-significant, P < 0.05, **P < 0.01, ***P < 0.001
An interplay between EGFR and JNK during Drosophila development has recently been shown [48] in keeping with previous descriptions of its coordination in human and other vertebrate models [49, 50]. In Anopheles, the malaria vector mosquitoes, the JNK pathway has been shown to participate in the immune response during blood feeding [51] and to be negatively correlated with mosquito longevity [52]. Feeding on HFHS mice resulted in an early suppression of JNK—an activator of the JNK pathway—compared to CHOW-fed mosquitoes (0.003 vs. 0.001 relative to RP49, P < 0.05) (Fig. 4f). This early suppression was not observed in other markers of the JNK pathway (Fig. 4g–i), including caspase 16—a marker of cell death in Aedes [53] (Fig. 4i). Similarly, we did not detect changes in the total levels of microbiota or reactive oxygen species (ROS) detoxification genes (Additional file 1: Fig. S2), which have been shown to be regulated [54] or regulate the JNK pathway [55] in mosquitoes, respectively.
Discussion
The worldwide increasing prevalence of metabolic syndrome has been linked to the consumption of Western diets, which are high in saturated fats and simple sugars [2]. Continuous consumption of these diets increases inflammatory cytokines, free fatty acids, glucose, and lipids in blood plasma, which can have serious implications for health, potentially leading to an increased risk of cardiovascular disease and mortality. Mosquitoes, such as the yellow fever mosquito Ae. aegypti, rely on blood meals for reproduction and development and are therefore exposed to various components of blood plasma. Previous research has analyzed the effects of individual metabolites, such as insulin and glucose, on mosquito biology and immunity by blood meal supplementation with those components [19, 21, 23]. However, these single-point alterations rarely reflect physiological modulations of blood composition found during metabolic processes.
At present, only a few studies have evaluated the impact of whole-blood composition on mosquito biology. Recently, a correlation between blood from healthy humans and DENV levels in mosquitoes fed from blood from such donors identified free iron levels as a regulator of vector competence [56]. More recently, the impact of an in vivo model of type II diabetes using transgenic mice identified increased susceptibility to Zika virus [57]. These studies did not address the impact on mosquito biology of physiological alterations in total blood composition due to dietary manipulations. To address this gap in knowledge and investigate the impact of Western diets, C57Bl6/J mice were fed an HFHS diet for 20 weeks. By the end of the dietary protocol, mice showed increased weight gain and developed insulin and glucose intolerance, as well as increased levels of circulating insulin, TAGs, and glucose, corroborating that our dietary protocol successfully induced metabolic syndrome symptoms.
Blood digestion is a major challenge for hematophagous insects, which must mitigate free iron and heme toxicity [58,59,60], build nutritional storage, and coordinate oogenesis and reproduction through nutrient sensing pathways, such as insulin and TOR signaling [61,62,63]. Previous studies have shown that insulin signaling is a conserved determinant of an organism's life span [64, 65]. Mosquitoes express insulin receptors in the midgut, and artificial insulin supplementation during blood-feeding assays has been shown to negatively impact mosquito longevity [19]. Here, we observed that the HFHS diet resulted in increased plasma insulin levels in mice prior to mosquito feeding. Accordingly, ingestion of HFHS blood by mosquitoes resulted in a stronger reduction of mosquito longevity compared to the ingestion of CHOW blood, in keeping with the hypothesis that increased insulin signaling would reduce mosquito longevity [19]. The observed downregulation of FoxO, a negative regulator of the insulin pathway [38] repressed following insulin receptor/TOR activation [66], might partially explain these findings.
Nutrient sensing nodes play a crucial role in regulating metabolism by detecting changes in the availability of nutrients and signaling appropriate responses to maintain energy balance and mitochondrial function [67]. In that sense, the EGF pathway is an important regulator of PI3K/Akt/mTORC1 [68, 69] in vertebrate models where it plays a critical role in cell proliferation, motility, growth, and differentiation. Insulin and TOR signalings are also key regulators of nutritional allocation and have been shown to regulate egg production following blood feeding [10, 61]. Here, we observed an increase in total egg production following the HFHS diet, in accordance with the early upregulation levels of the EGFR ligands Keren and Vein found in HFHS-fed mosquitoes.
Interestingly, increased egg production did not correlate with a detectable increase in vitellogenin expression. On the other hand, lipid quantification detected that HFHS mice had increased serum TAG and cholesterol levels. Accordingly, mosquitoes fed on HFHS mice had elevated levels of TAG allocation of fat body and ovaries by the time of oogenesis. This pattern correlated with an early increase in the expression of fatty acid synthase and later expression of lipid storage protein 2. Overall, this suggests that the HFHS-induced alterations of blood plasma may impact lipid allocation and metabolism in mosquitoes and compensate for the reduced lifespan by increasing their reproductive output, as they lay significantly more eggs than those fed on control mice. In our experiments, we have used the same cohorts of blood-fed mosquitoes to measure survival and egg-laying, thus minimizing inter-group variability and directly linking survival and fecundity. However, we cannot exclude the possibility that some of the differences observed in total egg mass derive from the alteration of egg size [70] or individual egg mass. Future work should address the impact of different blood-feeding conditions on the correlation between egg number and egg size as well as its impact on egg hatching rates, larval development, and mosquito body size.
The results presented here provide new insights into the impact of blood components on mosquito biology on both biological output and gene expression profiles. Our findings suggest that the Western diet-induced alterations of plasma may have implications for the transmission of infectious diseases by mosquitoes. While we did not detect alteration in the gene expression of stress markers, such as cell death and ROS detoxication, we observed an altered expression of markers of the JNK and JAK/STAT pathways, which have been shown to be important determinators of mosquito immune efficiency and vector competence [40, 51, 71]. The expression of regulators of the EGF pathway, such as Keren and Vein, are likely upstream regulators of such alterations and might have an important role in the modulation of phenotypes observed here.
While further studies will need to address the impact of Western-type diets on Aedes immunity and on the extrinsic incubation period of arboviral infections and other pathogens, our present data suggest an impact on vector capacity through signaling pathways that result in altered longevity and fecundity. Reduced lifespan is likely to impact the ability of mosquitoes to transmit diseases during a subsequent blood meal by reducing daily survival rates of mosquitoes fed on such a diet. On the other hand, increased egg production and lipid allocation could result in an increase in mosquito density or larval population resistance. The interplay between metabolic disorders and mosquito-biting behavior also warrants further exploration, particularly as it relates to vector capacity. Mosquitoes are drawn to certain metabolites like CO2, lactic acid, and ammonia [72], which are known to be altered in obese or diabetic patients [73,74,75]. This alteration could feasibly affect the host-seeking behavior of mosquitoes, potentially increasing the propensity of disease vectors to bite affected individuals. The refinement of these variables could allow the refinement of models to correlate the ongoing increase in the prevalence of malnutrition-derived metabolic syndromes with altered vector capacity.
The present study emphasizes the importance of addressing metabolic health to combat the spread of mosquito-borne illnesses and provides a murine model for evaluating the effect of malnutrition on vector biology. Overall, apparent alterations of nutrient-sensing pathways are likely to influence mosquito immunometabolism, an emerging field of study that is only starting to be investigated in insect vectors [76, 77]. Future studies should aim to identify the specific components of blood that are responsible for these effects and to investigate the impact of these alterations on the transmission of mosquito-borne diseases. Overall, this study provides a foundation for further research into the complex interactions between blood components and mosquito biology, which may ultimately lead to the development of new strategies for controlling the spread of mosquito-borne illnesses.
Conclusions
The rise of metabolic syndromes due to Western diets in various populations has significant ramifications beyond non-communicable diseases, extending to the realm of mosquito-borne disease transmission. Our research highlights that blood composition changes in HFHS diet-fed mice notably impact Ae. aegypti biology, with observed trends of decreased survival yet increased egg production. These biological shifts coincide with marked changes in gene expression pertinent to metabolism and nutrient processing. The implications of our study suggest that human dietary patterns in disease-endemic regions may influence vector physiology and disease spread by alterations of vector capacity. Continued research is critical to unravel these complex interactions and to inform disease control measures in the face of changing dietary landscapes.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AKT:
-
Protein kinase B
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- ATG8:
-
Autophagy-related protein 8
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- ERK:
-
Extracellular signal-regulated kinase
- FASI:
-
Fatty acid synthase I
- FoxO:
-
Forkhead Box O
- HFHS:
-
High-fat high-sugar
- IGF1:
-
Insulin-like growth factor 1
- ITT:
-
Insulin tolerance test
- JAK:
-
Janus kinase
- JNK:
-
C-Jun N-terminal kinase
- LMIC:
-
Low- and middle-income countries
- LSD1:
-
Lipid storage droplets surface-binding protein 1
- LSD2:
-
Lipid storage droplets surface-binding protein 2
- MAPK:
-
Mitogen-activated protein kinase
- oGTT:
-
Oral glucose tolerance test
- pbm:
-
Post blood meal
- PIAS:
-
Protein inhibitor of activated STAT
- ROS:
-
Reactive oxygen species
- STAT:
-
Signal transducer and activator of transcription
- SF:
-
Sugar-fed
- TAG:
-
Triacylglycerol
- TGFß:
-
Transforming growth factor beta
- TOR:
-
Target of rapamycin
References
James WPT. WHO recognition of the global obesity epidemic. Int J Obes. 2008;32:S120–6.
Rakhra V, Galappaththy SL, Bulchandani S, Cabandugama PK. Obesity and the western diet: how we got here. Mo Med. 2020;117:536–8.
Kopp W. How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab Syndr Obes. 2019;12:2221–36.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. Elsevier BV; 2011. p. 804–14.
Velásquez-Melendez G, Schlüssel MM, Brito AS, Silva AAM, Lopes-Filho JD, Kac G. Mild but not light or severe food insecurity is associated with obesity among Brazilian women. J Nutr. 2011;141:898–902.
Kac G, Velásquez-Melendez G, Schlüssel MM, Segall-Côrrea AM, Silva AA, Pérez-Escamilla R. Severe food insecurity is associated with obesity among Brazilian adolescent females. Public Health Nutr. 2012;15:1854–60.
Drake I, Sonestedt E, Ericson U, Wallström P, Orho-Melander M. A Western dietary pattern is prospectively associated with cardio-metabolic traits and incidence of the metabolic syndrome. Br J Nutr. 2018;119:1168–76.
Alberti KGMM, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366:1059–62.
Disease EM. Poverty and pathogens. Nature. 2016;531:S61–3.
Valzania L, Mattee MT, Strand MR, Brown MR. Blood feeding activates the vitellogenic stage of oogenesis in the mosquito Aedes aegypti through inhibition of glycogen synthase kinase 3 by the insulin and TOR pathways. Dev Biol. 2019;454:85–95.
Hansen IA, Attardo GM, Park J-H, Peng Q, Raikhel AS. Target of rapamycin-mediated amino acid signaling in mosquito anautogeny. Proc Natl Acad Sci USA. 2004;101:10626–31.
Surachetpong W, Singh N, Cheung KW, Luckhart S. MAPK ERK signaling regulates the TGF-beta1-dependent mosquito response to Plasmodium falciparum. PLoS Pathog. 2009;5:e1000366.
Pakpour N, Riehle MA, Luckhart S. Effects of ingested vertebrate-derived factors on insect immune responses. Curr Opin Insect Sci. 2014;3:1–5.
Zhu J, Miura K, Chen L, Raikhel AS. Cyclicity of mosquito vitellogenic ecdysteroid-mediated signaling is modulated by alternative dimerization of the RXR homologue Ultraspiracle. Proc Natl Acad Sci USA. 2003;100:544–9.
Roy SG, Raikhel AS. Nutritional and hormonal regulation of the TOR effector 4E-binding protein (4E-BP) in the mosquito Aedes aegypti. FASEB J. 2012;26:1334–42.
Roy SG, Hansen IA, Raikhel AS. Effect of insulin and 20-hydroxyecdysone in the fat body of the yellow fever mosquito, Aedes aegypti. Insect Biochem Mol Biol. 2007;37:1317–26.
Sun J, Hiraoka T, Dittmer NT, Cho KH, Raikhel AS. Lipophorin as a yolk protein precursor in the mosquito, Aedes aegypti. Insect Biochem Mol Biol. 2000;30:1161–71.
Ford PS, Van Heusden MC. Triglyceride-rich lipophorin in Aedes aegypti (Diptera: Culicidae). J Med Entomol. 1994;31:435–41.
Kang M-A, Mott TM, Tapley EC, Lewis EE, Luckhart S. Insulin regulates aging and oxidative stress in Anopheles stephensi. J Exp Biol. 2008;211:741–8.
Ahlers LRH, Trammell CE, Carrell GF, Mackinnon S, Torrevillas BK, Chow CY, et al. Insulin potentiates JAK/STAT signaling to broadly inhibit Flavivirus replication in insect vectors. Cell Rep. 2019;29:1946-1960.e5.
Drexler A, Nuss A, Hauck E, Glennon E, Cheung K, Brown M, et al. Human IGF1 extends lifespan and enhances resistance to Plasmodium falciparum infection in the malaria vector Anopheles stephensi. J Exp Biol. 2013;216:208–17.
Luckhart S, Crampton AL, Zamora R, Lieber MJ, Dos Santos PC, Peterson TML, et al. Mammalian transforming growth factor β1 activated after ingestion by Anopheles stephensi modulates mosquito immunity. Infect Immun. 2003;71:3000–9.
Weng S-C, Tsao P-N, Shiao S-H. Blood glucose promotes dengue virus infection in the mosquito Aedes aegypti. Parasit Vectors. 2021;14:376.
Barouei J, Bendiks Z, Martinic A, Mishchuk D, Heeney D, Hsieh Y-H, et al. Microbiota, metabolome, and immune alterations in obese mice fed a high-fat diet containing type 2 resistant starch. Mol Nutr Food Res. 2017;61:1700184.
Fahrmann J, Grapov D, Yang J, Hammock B, Fiehn O, Bell GI, et al. Systemic alterations in the metabolome of diabetic NOD mice delineate increased oxidative stress accompanied by reduced inflammation and hypertriglyceremia. Am J Physiol Endocrinol Metab. 2015;308:E978–89.
Imbroisi Filho R, Ochioni AC, Esteves AM, Leandro JGB, Demaria TM, Sola-Penna M, et al. Western diet leads to aging-related tumorigenesis via activation of the inflammatory, UPR, and EMT pathways. Cell Death Dis. 2021;12:643.
Branco JR, Esteves AM, Imbroisi Filho R, Demaria TM, Lisboa PC, Lopes BP, et al. Citrate enrichment in a Western diet reduces weight gain via browning of adipose tissues without resolving diet-induced insulin resistance in mice. Food Funct. 2022;13:10947–55.
Demaria TM, Crepaldi LD, Costa-Bartuli E, Branco JR, Zancan P, Sola-Penna M. Once a week consumption of Western diet over twelve weeks promotes sustained insulin resistance and non-alcoholic fat liver disease in C57BL/6 J mice. Sci Rep. 2023;13:3058.
Branco JR, Esteves AM, Leandro JGB, Demaria TM, Godoi V, Marette A, et al. Dietary citrate acutely induces insulin resistance and markers of liver inflammation in mice. J Nutr Biochem. 2021;98:108834.
Uraki R, Hastings AK, Brackney DE, Armstrong PM, Fikrig E. AgBR1 antibodies delay lethal Aedes aegypti-borne West Nile virus infection in mice. NPJ Vaccines. 2019;4:23.
Accoti A, Damiani C, Nunzi E, Cappelli A, Iacomelli G, Monacchia G, et al. Anopheline mosquito saliva contains bacteria that are transferred to a mammalian host through blood feeding. Front Microbiol. 2023;14:1157613.
Zheng M-L, Zhang D-J, Damiens DD, Lees RS, Gilles JRL. Standard operating procedures for standardized mass rearing of the dengue and chikungunya vectors Aedes aegypti and Aedes albopictus (Diptera: Culicidae)—II—Egg storage and hatching. Parasit Vectors. 2015;8:348.
Hixson B, Bing X-L, Yang X, Bonfini A, Nagy P, Buchon N. A transcriptomic atlas of Aedes aegypti reveals detailed functional organization of major body parts and gut regional specializations in sugar-fed and blood-fed adult females. Elife [Internet]. 2022;11. Available from: https://doi.org/10.7554/eLife.76132.
Tsujimoto H, Adelman ZN. An 11-point time course midgut transcriptome across 72 h after blood feeding provides detailed temporal resolution of transcript expression in the arbovirus vector, Aedes aegypti. bioRxiv. 2023;2023–2023.
Kurauti MA, Soares GM, Marmentini C, Bronczek GA, Branco RCS, Boschero AC. Insulin and aging. Vitamins and Hormones. Elsevier; 2021. p. 185–219.
Antikainen H, Driscoll M, Haspel G, Dobrowolski R. TOR-mediated regulation of metabolism in aging. Aging Cell. 2017;16:1219–33.
Ni YG, Wang N, Cao DJ, Sachan N, Morris DJ, Gerard RD, et al. FoxO transcription factors activate Akt and attenuate insulin signaling in heart by inhibiting protein phosphatases. Proc Natl Acad Sci USA. 2007;104:20517–22.
Lee S, Dong HH. FoxO integration of insulin signaling with glucose and lipid metabolism. J Endocrinol. 2017;233:R67-79.
Koller CN, Raikhel AS. Initiation of vitellogenin uptake and protein synthesis in the mosquito (Aedes aegypti) ovary in response to a blood meal. J Insect Physiol. 1991;37:703–11.
Liu W-Q, Chen S-Q, Bai H-Q, Wei Q-M, Zhang S-N, Chen C, et al. The Ras/ERK signaling pathway couples antimicrobial peptides to mediate resistance to dengue virus in Aedes mosquitoes. PLoS Negl Trop Dis. 2020;14:e0008660.
Buchon N, Broderick NA, Kuraishi T, Lemaitre B. Drosophila EGFR pathway coordinates stem cell proliferation and gut remodeling following infection. BMC Biol. 2010;8:152.
Brown KE, Kerr M, Freeman M. The EGFR ligands Spitz and Keren act cooperatively in the Drosophila eye. Dev Biol. 2007;307:105–13.
Biteau B, Jasper H. EGF signaling regulates the proliferation of intestinal stem cells in Drosophila. Development. 2011;138:1045–55.
Wittes J, Schüpbach T. A gene expression screen in Drosophila melanogaster identifies novel JAK/STAT and EGFR targets during oogenesis. G3 (Bethesda). 2019;9:47–60.
Janeh M, Osman D, Kambris Z. Damage-induced cell regeneration in the midgut of Aedes albopictus mosquitoes. Sci Rep. 2017;7:44594.
Darnell JE Jr, Kerr LM, Stark GR. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science. 1994;264:1415–21.
Hombría JC-G, Brown S. The fertile field of Drosophila Jak/STAT signalling. Curr Biol. 2002;12:R569–75.
Kushnir T, Mezuman S, Bar-Cohen S, Lange R, Paroush Z, Helman A. Novel interplay between JNK and Egfr signaling in Drosophila dorsal closure. PLoS Genet. 2017;13:e1006860.
Morgan EL, Scarth JA, Patterson MR, Wasson CW, Hemingway GC, Barba-Moreno D, et al. E6-mediated activation of JNK drives EGFR signalling to promote proliferation and viral oncoprotein expression in cervical cancer. Cell Death Differ. 2021;28:1669–87.
Le A, Azouz A, Thomas S, Istaces N, Nguyen M, Goriely S. JNK1 signaling downstream of the EGFR pathway contributes to Aldara®-induced skin inflammation. Front Immunol. 2020;11:604785.
Garver LS, de Almeida OG, Barillas-Mury C. The JNK pathway is a key mediator of Anopheles gambiae antiplasmodial immunity. PLoS Pathog. 2013;9:e1003622.
Souvannaseng L, Hun LV, Baker H, Klyver JM, Wang B, Pakpour N, et al. Inhibition of JNK signaling in the Asian malaria vector Anopheles stephensi extends mosquito longevity and improves resistance to Plasmodium falciparum infection. PLoS Pathog [Internet]. 2018; Available from: https://doi.org/10.1371/journal.ppat.1007418
Ocampo CBCB, Caicedo PA, Jaramillo G, Ursic Bedoya R, Baron O, Serrato IM, et al. Differential expression of apoptosis related genes in selected strains of Aedes aegypti with different susceptibilities to dengue virus. PLoS ONE [Internet]. 2013;8. Available from: https://doi.org/10.1371/journal.pone.0061187.g004
Xiao X, Yang L, Pang X, Zhang R, Zhu Y, Wang P, et al. A Mesh–Duox pathway regulates homeostasis in the insect gut. Nat Microbiol. 2017;2:17020.
Jaramillo-Gutierrez G, Molina-Cruz A, Kumar S, Barillas-Mury C. The Anopheles gambiae oxidation resistance 1 (OXR1) gene regulates expression of enzymes that detoxify reactive oxygen species. PLoS ONE. 2010;5:e11168.
Zhu Y, Tong L, Nie K, Wiwatanaratanabutr I, Sun P, Li Q, et al. Host serum iron modulates dengue virus acquisition by mosquitoes. Nat Microbiol. 2019;1–11.
Azar SR, Campos RK, Yun R, Strange T, Rossi SL, Hanley KA, et al. Aedes aegypti Shows Increased Susceptibility to Zika Virus via Both In Vitro and In Vivo Models of Type II Diabetes. Viruses [Internet]. 2022;14. Available from: https://doi.org/10.3390/v14040665
Graça-Souza AV, Maya-Monteiro C, Paiva-Silva GO, Braz GRC, Paes MC, Sorgine MHF, et al. Adaptations against heme toxicity in blood-feeding arthropods. Insect Biochem Mol Biol. 2006;36:322–35.
Paiva-Silva GO, Cruz-Oliveira C, Nakayasu ES, Maya-Monteiro CM, Dunkov BC, Masuda H, et al. A heme-degradation pathway in a blood-sucking insect. Proc Natl Acad Sci. 2006;103:8030–5.
Oliveira MF, Timm BL, Machado EA, Miranda K, Attias M, Silva JR, et al. On the pro-oxidant effects of haemozoin. FEBS Lett. 2002;512:139–44.
Gulia-Nuss M, Robertson AE, Brown MR, Strand MR. Insulin-like peptides and the target of rapamycin pathway coordinately regulate blood digestion and egg maturation in the mosquito Aedes aegypti. PLoS ONE. 2011;6:e20401.
Park J-H, Attardo GM, Hansen IA, Raikhel AS. GATA factor translation is the final downstream step in the amino acid/target-of-rapamycin-mediated vitellogenin gene expression in the anautogenous mosquito Aedes aegypti. J Biol Chem. 2006;281:11167–76.
Hansen IA, Attardo GM, Rodriguez SD, Drake LL. Four-way regulation of mosquito yolk protein precursor genes by juvenile hormone-, ecdysone-, nutrient-, and insulin-like peptide signaling pathways. Front Physiol. 2014;5:103.
Taguchi A, White MF. Insulin-like signaling, nutrient homeostasis, and life span. Annu Rev Physiol. 2008;70:191–212.
Piper MDW, Selman C, McElwee JJ, Partridge L. Separating cause from effect: how does insulin/IGF signalling control lifespan in worms, flies and mice? J Intern Med. 2008;263:179–91.
Demontis F, Perrimon N. Integration of insulin receptor/foxo signaling and dMyc activity during muscle growth regulates body size in Drosophila. Development. 2009;136:983–93.
Luckhart S, Riehle MA. Conservation and convergence of immune signaling pathways with mitochondrial regulation in vector arthropod physiology. Elsevier Inc.; 2017. p. 15–33.
Zhang BK, Moran AM, Bailey CG, Rasko JEJ, Holst J, Wang Q. EGF-activated PI3K/Akt signalling coordinates leucine uptake by regulating LAT3 expression in prostate cancer. Cell Commun Signal [Internet]. 2019;17. Available from: https://doi.org/10.1186/s12964-019-0400-0
Nishimura Y, Takiguchi S, Ito S, Itoh K. EGF-stimulated AKT activation is mediated by EGFR recycling via an early endocytic pathway in a gefitinib-resistant human lung cancer cell line. Int J Oncol. 2015;46:1721–9.
Mundim-Pombo APM, Carvalho HJC de, Rodrigues Ribeiro R, León M, Maria DA, Miglino MA. Aedes aegypti: egg morphology and embryonic development. Parasit Vectors [Internet]. 2021;14. Available from: https://doi.org/10.1186/s13071-021-05024-6.
Souza-Neto JA, Sim S, Dimopoulos G. An evolutionary conserved function of the JAK-STAT pathway in anti-dengue defense. Proc Natl Acad Sci USA. 2009;106:17841–6.
Dormont L, Mulatier M, Carrasco D, Cohuet A. Mosquito attractants. J Chem Ecol. 2021;47:351–93.
Cheon SY, Song J. The association between hepatic encephalopathy and diabetic encephalopathy: the brain-liver axis. Int J Mol Sci. 2021;22:463.
de-Cleva R, Cardia L, Vieira-Gadducci A, Greve JM, Santo MA. Lactate can be a marker of metabolic syndrome in severe obesity? Arq Bras Cir Dig [Internet]. 2021;34. Available from: https://doi.org/10.1590/0102-672020210001e1579.
Alawad AO, Merghani TH, Ballal MA. Resting metabolic rate in obese diabetic and obese non-diabetic subjects and its relation to glycaemic control. BMC Res Notes [Internet]. 2013;6. Available from: https://doi.org/10.1186/1756-0500-6-382.
Samaddar S, Marnin L, Butler LR, Pedra JHF. Immunometabolism in arthropod vectors: redefining interspecies relationships. Trends Parasitol. 2020;36:807–15.
Galenza A, Foley E. Immunometabolism: insights from the drosophila model. Dev Comp Immunol. 2019;94:22–34.
Acknowledgements
We thank Jaciara Miranda Freire for insect rearing. We thank Prof Marcelo Bozza for donating AG129 mice.
Funding
This work was supported by grants from the Instituto Serrapilheira, Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro, and Conselho Nacional de Desenvolvimento Científico e Tecnológico.
Author information
Authors and Affiliations
Contributions
AM: Formal analysis, Investigation, Data curation, Writing—Review and Editing. MP: Investigation, Writing—Review and Editing. MS: Formal analysis, Investigation, Data curation. ECB: Formal analysis, Investigation, Data curation, Writing—Review and Editing. CLO: Investigation, Writing—Review and Editing. ABWN: Investigation, Writing—Review and Editing. NCK: Investigation. JP: Investigation, Writing—Review and Editing. IR: Methodology, Writing—Review and Editing. GOPS: Methodology, Writing—Review and Editing. GA: Methodology, Writing—Review and Editing. PZ: Conceptualization, Methodology, Formal analysis, Resources, Writing—Review and Editing. MSP: Conceptualization, Methodology, Formal analysis, Resources, Writing—Review and Editing, Supervision, Funding acquisition. FMG: Conceptualization, Methodology, Formal analysis, Resources, Data curation, Writing—Original Draft, Supervision, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experiments were performed according to the criteria approved by the Animal Care and Use Committee from the Health Sciences Center of the Federal University of Rio de Janeiro under the document CEUA/CCS/UFRJ 087/20.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. Diet composition. Table S2. Primer list. Figure S1. Mice were fed with either a CHOW or HSHF diet for 20 weeks. Over the course of the experiment, metabolic syndrome was followed by tracking weight gain, glucose, and insulin sensitivity. Then, Aedes mosquitoes were allowed to feed on anesthetized mice, and whole-body relative expression levels of A fatty acid synthase I, B LSD1, C LSD2, D pyruvate kinase, E glycogen synthase, and F PINK1 were measured by qRT-PCR 1 and 4 days pbm. Sugar-fed (SF) mosquitoes were used as a baseline for gene expression. Four biological replicates were prepared using independent mosquito hatches and dietary protocols. A Unpaired t-test and B–F one-way ANOVA followed by Tukey’s multiple comparison tests were performed. ns: non-significant, *P < 0.05. Figure S2. Mice were fed with either a CHOW or HSHF diet for 20 weeks. Over the course of the experiment, metabolic syndrome was followed by tracking weight gain, glucose, and insulin sensitivity. Then, Aedes mosquitoes were allowed to feed on anesthetized mice, and whole-body relative expression levels of A 16S, B catalase, C glutathione peroxidase, and D oxidation resistance 1 (A–D). Sugar-fed (SF) mosquitoes were used as a baseline for gene expression. Four biological replicates were prepared using independent mosquito hatches and dietary protocols. One-way ANOVA followed by Tukey’s multiple comparison tests was performed. ns: non-significant.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Menezes, A., Peixoto, M., Silva, M. et al. Western diet consumption by host vertebrate promotes altered gene expression on Aedes aegypti reducing its lifespan and increasing fertility following blood feeding. Parasites Vectors 17, 12 (2024). https://doi.org/10.1186/s13071-023-06095-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-023-06095-3