Abstract
Background
Left heart failure (HF) is characterized by an elevation in left-sided filling pressures, causing symptoms of dyspnea, impairing exercise capacity, and leading to pulmonary venous congestion and secondary pulmonary hypertension (PH). There is an increased incidence of PH associated with left heart disease, particularly with heart failure with preserved ejection fraction (HFpEF-PH). Treatment possibilities in HFpEF-PH are non-specific and very limited, thus additional pharmacological and non-pharmacological therapeutic strategies are needed. Various types of exercise-based rehabilitation programs have been shown to improve exercise capacity and quality of life (QoL) of HF and PH patients. However, no study focused on exercise training in the population of HFpEF-PH. This study is designed to investigate whether a standardized low-intensity exercise and respiratory training program is safe and may improve exercise capacity, QoL, hemodynamics, diastolic function, and biomarkers in patients with HFpEF-PH.
Methods
A total of 90 stable patients with HFpEF-PH (World Health Organization functional class II–IV) will be randomized (1:1) to receive a 15-week specialized low-intensity rehabilitation program, including exercise and respiratory therapy and mental gait training, with an in-hospital start, or standard care alone. The primary endpoint of the study is a change in 6-min walk test distance; secondary endpoints are changes in peak exercise oxygen uptake, QoL, echocardiographic parameters, prognostic biomarkers, and safety parameters.
Discussion
To date, no study has investigated the safety and efficacy of exercising specifically in the HFpEF-PH population. We believe that a randomized controlled multicenter trial, which protocol we are sharing in this article, will add important knowledge about the potential utility of a specialized low-intensity exercise and respiratory training program for HFpEF-PH and will be valuable in finding optimal treatment strategies for these patients.
Trial registration
ClinicalTrials.gov NCT05464238. July 19, 2022.
Similar content being viewed by others
Background
Pulmonary hypertension (PH) associated with left heart disease (LHD-PH) is a growing health problem with high morbidity and mortality [1,2,3]. Among the various PH groups, LHD-PH is the most common form and accounts for 50–80% of all cases [1, 4,5,6,7,8]. The estimated prevalence of PH in HF varies depending on the method of pulmonary arterial pressure (PAP) measurement, the definition of PH, the populations studied, and the type of HF. In heart failure with reduced ejection fraction (HFrEF), PH frequency is 40–75%, as assessed by right heart catheterization (RHC) [6, 9,10,11]. The precise prevalence of PH associated with heart failure with preserved ejection fraction (HFpEF-PH) is still unclear. Most of the data are based on echocardiographic signs, where PH prevalence in HFpEF ranges between 52 and 83% [12, 13]. In the invasive hemodynamic assessment study, among 618 HFpEF patients, 355 (57.4%) were diagnosed with PH, and 75 (21.1%) of them had combined post- and pre-capillary PH (CpcPH) [11].
Any type of left HF is characterized by an elevation in left-sided filling pressures, causing symptoms of dyspnea [14], impairing exercise capacity [15], and leading to pulmonary venous congestion and secondary post-capillary PH. Across the spectrum of LHD, increased PAP and pulmonary vascular resistance (PVR) are related to higher disease burden and worse outcomes [16,17,18].
Targeted medication therapy for pulmonary arterial hypertension (PAH) and chronic thromboembolic pulmonary hypertension (CTEPH), including drugs interfering with the endothelin, nitric oxide, and prostacyclin pathways, has evolved progressively in the last decades, with increasing evidence for efficacy [1, 19, 20]. However, these drugs are not recommended in patients with LHD-PH [1, 3]. Conventional HF treatments (medical/interventional) currently remain the only therapies for these patients [1, 4, 21]. Although HF syndrome covers both, HFrEF and HFpEF, these disorders have some differences in pathophysiology, clinical characteristics, hemodynamics, cardiopulmonary interaction, and response to therapy [22,23,24]. While pharmacological treatments are well-established in HFrEF, the same strategies could not be convincingly proven to be effective in HFpEF [21] with the recent exception of sodium-glucose cotransporter-2 (SGLT2) inhibitors case [25, 26].
In patients with HFpEF and HFpEF-PH medication therapy options remain limited—SGLT2 inhibitors, diuretics, and treatment of comorbidities are recommended [1, 21, 25, 26]. Therefore, there is a high need for additional therapeutic strategies to improve symptoms, exercise capacity, health-related quality of life (QoL), and prognosis in these patients.
The ESC/ERS 2022 guidelines recommend complex treatment of PAH, consisting of disease-targeted and supportive medical therapy, together with non-pharmacological general measures, including supervised exercise training [1], but there are no evidence-based recommendations for the exercise therapy of LHD-PH.
Different exercise-based rehabilitation programs have already been shown to improve the physical capacity and health-related QoL of PH patients [27,28,29,30,31,32,33]. Most of the previous trials enrolled PAH and CTEPH patients only, excluding post-capillary PH, which is pathognomonic for LHD-PH. Standardized low-intensity exercise and respiratory training programs also demonstrated an increase in exercise capacity, lower limb muscle strength, health-related QoL, and hemodynamics in PAH and CTEPH patients; LHD-PH was an exclusion criterion in all previous studies [30, 31, 33,34,35,36].
Properly designed exercise interventions for HF patients demonstrated improvement in physical capacity, health-related QoL, and risk reduction of all-cause and HF hospitalizations [37,38,39,40,41,42]. Although HFrEF patients were predominant in the largest HF exercise training trials, several systematic reviews and meta-analyses have focused specifically on HFpEF, and confirmed the positive impact of exercising on functional capacity in HFpEF, as indicated by improved peak oxygen uptake (VO2peak), 6-min walk test distance (6-MWD), and health-related QoL [42,43,44,45,46,47]. The number of HFpEF-PH patients in previous HFpEF exercise training trials remains unclear [48], and none of the previous studies focused specifically on HFpEF-PH.
This study is sought to investigate whether a standardized exercise training program is safe and tolerable and may improve exercise capacity, quality of life, hemodynamics, diastolic dysfunction, and biomarkers in patients with HFpEF-PH. We used the SPIRIT Checklist when writing our manuscript [49].
Methods/design
Study design
This study is designed as a prospective, randomized (1:1 randomization), controlled, parallel-group, superiority, multicenter trial in patients with invasively confirmed HFpEF-PH.
The total duration of the study is planned for 3 years (Q1 2023 to Q4 2025). The follow-up of individual subjects will be performed until the last patient’s last visit. The study is registered on ClinicalTrials.gov (identifier—NCT05464238). A summary of the protocol is provided in Table 1.
Randomization and blinding
The distribution of patients to the different groups will be performed by block randomization. Group allocation will be provided in sealed envelopes, which will be prepared for each participating center by the study coordinator at Heidelberg University. Blocks for block randomization will be medium size to allow a balanced randomization sequence over time. Sites that only include a very small amount of patients may lead to a minimally unbalanced patient number. Block sizes will be the same for all centers, leading to several randomization/allocation blocks in high recruiting centers. Upon inclusion, the participants will be randomly designated to the intervention (training) or conventional (control) group. Allocation concealment will be ensured, as envelopes will not be unsealed until the patient has been recruited into the trial.
The participation in this rehabilitation program is voluntary. Participants may terminate their participation at any time.
According to the eligibility criteria, the patient should be receiving optimized and ≥ 1 month of stable treatment before inclusion in the study. Thus, we expect that the need for medication changes during the 15-week follow-up period will be minimal. However, the dosage of diuretics is permitted to be changed, and other pharmacological and non-pharmacological treatments will not be prohibited, if the treating physicians decide this to be clinically necessary. Participation in another interventional study is prohibited during the 15-week follow-up period.
Cardiologists, pulmonologists, and PH experts, blinded to the patients’ allocation groups, will perform and interpret examination tests (6-min walking test, cardiopulmonary exercise test, echocardiography, right heart catheterization, cardiac magnetic resonance imaging). Study data analytics will also be blinded to the patients’ allocation groups until the entire analysis has been completed.
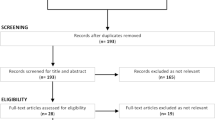
Population sampling
Candidate patients will be selected from European pulmonary hypertension centers (a list of study sites can be found at ClinicalTrials.gov), which will be continuously updated. To achieve an adequate number of enrolled participants, healthcare professionals at involved European PH centers, as well as national associations of PH patients, will be informed about the ongoing study and the opportunity to take part in it. The diagnosis of HFpEF-PH will be established according to the ESC/ERS guidelines [1, 3, 21]. Patients will be screened before their baseline visit regarding the inclusion and exclusion criteria (days − 28 to − 1) (Table 2). After 15 weeks, patients of the control group will be offered to participate in the training program (waiting-group design). All patients will visit the clinic for pre-study screening on days − 28 to − 1 (visit [V] 1), at baseline (BL) at day 1 (V2), and week 15 (V4).
Interventions
Training
The training will be based on the specialized low-intensity rehabilitation program, including exercise and respiratory therapy and mental gait training, which has been previously described [32, 35, 50, 51].
The initial phase of exercise training will be closely monitored, as it will be held in hospital for approximately 3 weeks period and later will be continued for further 12 weeks at home. In-hospital stays will be arranged country-specific, and hospitalization times may range. The rehabilitation program will comprise interval ergometer training (20 min 5 days per week), dumbbell training of single muscle groups (30 min 5 days a week), respiratory therapy (30 min 5 days per week), mental training and guided walks (individually, at least two times a week), and conventional elements, such as massages, relaxation, lectures, and patient education.
Individual training adjustment will be performed according to clinical assessments at baseline and follow-up and the patient’s subjective perception throughout the program. Training intensity will be started at 40–50% of the maximal patient’s workload, reached during the cardiopulmonary exercise test at baseline, and will be increased within the in-hospital period, trying to achieve the maximal baseline workload (maintaining 60–80% of the peak heart rate and avoiding desaturation < 90%). Overexertion must be strictly avoided. In order to ensure safety and adherence, every workout will be supervised by a physiotherapist during an in-hospital phase. Before leaving the hospital, each patient will receive individualized written recommendations on how to continue exercising at home. The patient will be asked to document daily trainings (intensity, duration, pulse rate, blood pressure, adverse events), which will be discussed at the follow-up visits.
Control
Patients in the control group will not receive exercise training and will continue their regular treatment and daily activities for 15 weeks. After 15 weeks, control group patients will be offered to take part in the exercise training program (waiting-group design). In this case, the final assessment of the patient in the control group will also serve as a baseline assessment for a participant in the training group.
Individual withdrawal criteria
The patient will be withdrawn from the study at any time, if he/she wishes to discontinue or if one of the following occurs due to exercise training:
-
➢Signs of acute heart failure
-
➢Syncope
-
➢Symptomatic ventricular tachycardia
-
➢Worsening of WHO functional class
Data collection and management
Each center will receive study-specific case record forms (CRF) to collect the data and enhance data integrity. Information obtained will be pseudonymized. The rules of medical confidentiality and data protection will be followed.
The data will be prospectively collected in every participating center. All findings including clinical and laboratory data will be documented in the patient’s medical record. The center’s principal investigator will be responsible for the patients’ safety, study conduct, and data quality, ensuring that all sections of the database are completed correctly and entries can be verified against source data. The biometrician and trial coordinator, appointed by Thoraxklinik at Heidelberg University Hospital (Core center of the study), will be able to access all (e)CRFs and check for reliability, consistency, and completeness of the data. Based on these checks, queries will be produced combined with the queries generated by visual control. All missing data or inconsistencies will be reported back to the respective recruiting center and will be followed upon completion.
Assessments
Efficacy assessment
Efficacy parameters in both groups will be assessed at baseline and after 15 weeks (mean or median changes from baseline to 15 weeks, comparing changes within trained and control groups as well as mean/median changes between these groups). Patients in the training group will additionally perform the 6-MWD at the end of in-hospital rehabilitation.
The primary endpoint is to determine the effect of standardized exercise and respiratory training on exercise capacity, measured by the mean change of 6-MWD (baseline vs 15 weeks vs control group) in the HFpEF-PH population.
Secondary endpoints include mean/median changes from baseline to 15 weeks of echocardiography parameters, cardiopulmonary exercise testing, World Health Organization (WHO) functional class, measurement of safety parameters, health-related quality of life assessment (SF-36 questionnaire), anxiety and depression assessment (HADS scale), optional right heart catheterization at rest and during exercise, and optional cardiac magnetic resonance imaging (MRI). A detailed description of the evaluative parameters of each test is provided in the following paragraph (the “Procedures” section).
A follow-up interview will be performed by phone at the end of the study (last patient, last visit) to assess safety and compliance and observe survival. The long-term compliance and risk profile of exercise training will be explored to identify risk factors and record adverse events.
The detailed timeline of the study is shown in Fig. 1.
Procedures
Six-minute walking distance (6-MWD) and Borg scale
Blinded to the patients’ allocation groups, investigators will perform a 6-MWD test, according to the ATS guidelines [52]. Before and after the 6-MWD test, heart rate, blood pressure, and oxygen saturation will be measured. If the patient receives supplemental oxygen, the amount of oxygen has to be the same for each test. After the test, 6-MWD and subjective perception of dyspnea, measured by the Borg scale of 10 points, will be determined.
Cardiopulmonary exercise testing (CPET)
Cardiopulmonary exercise testing will be performed to assess peak oxygen uptake (peak VO2), peak VO2/kg, peak workload, heart rate, blood pressure, oxygen saturation, ventilation, ventilatory equivalent for carbon dioxide (VE/VCO2), VO2, and VCO2 at the anaerobic threshold. Investigators will be blinded to the patients’ allocation group.
Echocardiography
Investigators, blinded to the patients’ allocation groups, will perform echocardiography. Two-dimensional, Doppler echocardiography, and three-dimensional (3D) measurements will be conducted. Echocardiography measurements will include sizes of chambers, LV pump function (LV ejection fraction, determined by Simpson biplane method and 3D LV EF), LV diastolic function (E/e′ mean), RV pump function (RV fractional area change (FAC) and 3D RV EF), estimated systolic pulmonary arterial pressure (sPAP), tricuspid annular plane systolic excursion (TAPSE), tricuspid annular peak systolic velocity (TAPSV), global longitudinal RV and LV strain, and size and collapsibility of the inferior vena cava (IVC).sPAP will be estimated by the maximal velocity of tricuspid regurgitation using the Bernoulli formula. Right atrial pressure will be evaluated under consideration of IVC: 3 mmHg if the vena cava < 21 mm (width) and collapses during inspiration > 50%, 8 mmHg if the vena cava is > 21 mm and collapses during inspiration > 50%, and 15 mmHg if the vena cava is > 21 mm and collapses < 50%.
Invasive hemodynamic assessment (optional)
Hemodynamic parameters will be determined by right heart catheterization according to the current guidelines. Invasively measured parameters will include right atrial pressure, mean pulmonary arterial pressure (mPAP), and pulmonary artery wedge pressure (PAWP). Cardiac output (CO) will be estimated by the thermodilution method. Pulmonary vascular resistance (PVR) and cardiac index (CI) will be calculated. The values will be based on two to three measurements at one time point. Hemodynamics will be measured at rest and optionally during exercise with a supine bicycle ergometer. Investigators will be blinded to the patients’ allocation group.
Cardiac MRI (optional)
Investigators who will be blinded to the clinical data and group assignment will evaluate cardiac MRI. MRI measurements will include LV and RV mass, area, volumes and function (regional and global), diastolic function assessment (mitral-pulmonary flows), atrial size and function (left atrial strain and strain rate), T1 mapping/extracellular volume, and the pulmonary artery to aorta ratio.
Laboratory parameters
The N-terminal prohormone of brain natriuretic peptide (NTproBNP) will be assessed at baseline and after the 15-week follow-up period. Routine laboratory parameters determined according to the standards of the clinic (hemoglobin, glucose, creatinine, potassium, iron) will be collected as safety parameters.
Patient-reported outcomes
Quality of life will be assessed with the 36-Item Short Form Health Survey (SF-36) [53]. The questionnaire includes two main scores with physical component and emotional component scales and eight subscales. A higher score indicates a better QoL. Anxiety and depression will be assessed using the Hospital Anxiety and Depression Scale (HADS) [54]. The HADS comprises seven questions for anxiety and seven questions for depression. Scores of less than 7 indicate non-anxiety or non-depression. The higher the score, the more pronounced anxiety or depression is. Both questionnaires will be in the respective language of the country.
Risks assessment
Adverse reactions/adverse events and serious adverse reactions/serious adverse events will be documented throughout the trial.
Statistical considerations and analyses
Sample size calculation
To estimate the effect of exercise training on 6-MWD, 90 patients are expected to be enrolled, who either receive exercise training or continue their daily lifestyle for 15 weeks. The sample size was calculated by the G*Power 3.1 program according to the results of previous studies on 6-MWD. Based on previous data and the inclusion criteria, we expect a clinically significant mean increase of 35 m with a standard deviation of the difference of 50 m. If the true treatment effect is a difference of at least 35 m with an equal standard deviation of the difference of 50 m, the two-sided Student’s t-test at an alpha level of 0.05 has a power of 85%, if 38 patients for each group are included. To account for a possible 15% dropout rate, we will include 45 patients in each group—90 patients in total.
Statistical analysis
The data from all centers will be pooled. If sample sizes allow, center effects on the primary and secondary outcomes will be analyzed.
Descriptive statistics will be displayed by treatment and control groups corrected for the active treatment group, including the usual location and scale statistics (mean, median, standard deviation, standard error, first and third quartiles, minimum, and maximum) and 95% confidence limits of the mean and median. Frequency tables for qualitative data will be provided. As an unbalanced distribution of baseline characteristics may not be completely excluded, baseline clinical parameters including patient risks and prognostic implications will be analyzed and compared between the groups.
The primary efficacy analysis will be based on an analysis of variance with the baseline values as a covariate (ANCOVA). This analysis provides a power advantage over the standard two-sided Student’s t-test leading to a statistical power of 85% or more. If the preconditions for ANCOVA are not met, a t-test with robust variance estimation (Welch test) will be used. Secondary endpoints will be analyzed by comparison of the mean changes between baseline and 15 weeks in the two groups (training vs control group) adjusted for the baseline value (ANCOVA or Wilcoxon rank sum test for non-parametric data). Categorical data will be analyzed by the McNemar test or chi-square test as appropriate. Exploratory data analysis of follow-up will be conducted by descriptive statistics and comparing baseline values and follow-up examinations. In case of ≤ 20% of missing values of a variable, a multiple imputation strategy will be used and analyzed as sensitivity analysis for data interpretation. The primary analysis set is the intention-to-treat analysis population (all patients randomized into the study). As a sensitivity analysis, the per-protocol population will be analyzed (all patients actually taking part in the study). Patients not fulfilling the inclusion criteria will be excluded in a separate sensitivity analysis using the per-protocol set.
Patient characteristics and efficacy parameters (secondary and exploratory endpoints) will be analyzed at baseline and 15 weeks. The values for each respective group will be displayed as mean ± standard deviation or mean ± standard error of the mean. Changes from baseline to 15 weeks will be analyzed by robust Student’s t-test (Welch test). Frequency data will be displayed as n and %. This data will be analyzed by the chi-square test and McNemar test. By means of correlation and regression analysis, the influence of different factors on the training effect will be investigated. P-values < 0.05 will be considered significant.
Discussion
Increases in pulmonary arterial pressure and pulmonary vascular resistance in HFpEF are related to a higher disease burden and a worse outcome [16, 55]. As treatment possibilities in HFpEF-PH are very limited and non-specific [1, 21, 25, 26], additional pharmacological and non-pharmacological therapeutic strategies are needed.
There are no evidence-based recommendations for the exercise therapy of PH-HFpEF, but taking into consideration the positive impact of exercise training both in PAH and HFpEF, we could expect it to be beneficial in HFpEF-PH as well. However, this hypothesis requires dedicated research, as HFpEF-PH patients differ in hemodynamics and exercise intolerance, compared with HFpEF without PH [56]. The safety, tolerability, and effectiveness of exercising in this specific population were never evaluated so far—most of PH training studies excluded patients with post-capillary PH, and HFpEF trials usually did not focus on right heart and pulmonary circulation [33, 48].
The intervention that we are planning to investigate is a standardized low-intensity rehabilitation program, including exercise and respiratory therapy and mental gait training, which has already demonstrated its safety and effectiveness for PAH and CTEPH patients in several trials, including randomized multicenter study in eleven centers across ten European countries [30, 32, 35, 36, 50, 51].
We believe that randomized controlled multicenter trial, which protocol we are sharing in this article, will add important knowledge about the potential utility of a standardized exercise training program for HFpEF-PH and will be valuable in finding optimal treatment strategies for these severely ill patients.
Trial status
Protocol version number and date: version 1.0, 5 December 2019.
Start date of recruitment 2023 Q1.
Estimated primary completion date 2025 Q4.
Availability of data and materials
Only researchers that are directly involved in the study will have access to the final dataset.
Abbreviations
- 6-MWD:
-
6-Min walk test distance
- CI:
-
Cardiac index
- CO:
-
Cardiac output
- CpcPH:
-
Combined post- and pre-capillary pulmonary hypertension
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- DLCO:
-
Diffusing capacity for carbon monoxide
- ERS:
-
European Respiratory Society
- ESC:
-
European Society of Cardiology
- FEV1:
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- HADS:
-
Hospital Anxiety and Depression Scale
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- LVEDP:
-
Left ventricular end diastolic pressure
- mPAP:
-
Mean pulmonary arterial pressure
- MRI:
-
Magnetic resonance imaging
- PAH:
-
Pulmonary arterial hypertension
- PAP:
-
Pulmonary arterial pressure
- PCWP:
-
Pulmonary capillary wedge pressure
- PH:
-
Pulmonary hypertension
- PH–LHD:
-
Pulmonary hypertension associated with left heart disease
- PVR:
-
Pulmonary vascular resistance
- QoL:
-
Quality of life
- RCT:
-
Randomized controlled trial
- RHC:
-
Right heart catheterization
- SF-36:
-
36-Item Short Form Health Survey
- SGLT2:
-
Sodium-glucose cotransporter-2
- sPAP:
-
Systolic pulmonary artery pressure
- VE/VCO2 :
-
Ventilatory equivalent for carbon dioxide
- VE/VCO2 slope:
-
Ventilatory equivalent for carbon dioxide
- VO2 :
-
Oxygen uptake
- WHO:
-
World Health Organization
- WU:
-
Wood units
References
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS, Escribano-Subias P, Ferrari P, Ferreira DS, Ghofrani HA, Giannakoulas G, Kiely DG, Mayer E, Meszaros G, Nagavci B, Olsson KM, Pepke-Zaba J, Quint JK, Rådegran G, Simonneau G, Sitbon O, Tonia T, Toshner M, Vachiery JL, Vonk Noordegraaf A, Delcroix M, Rosenkranz S; ESC/ERS Scientific Document Group. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2023;61(1):2200879. https://doi.org/10.1183/13993003.00879-2022.
Vachiéry J-L, Adir Y, Barberà JA, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62:D100-108. https://doi.org/10.1016/j.jacc.2013.10.033.
Vachiéry J-L, Tedford RJ, Rosenkranz S, et al. Pulmonary hypertension due to left heart disease. Eur Respir J. 2019;53:1801897. https://doi.org/10.1183/13993003.01897-2018.
Galiè N, Humbert M, Vachiery J-L, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Rev Espanola Cardiol Engl Ed. 2016;69:177. https://doi.org/10.1016/j.rec.2016.01.002.
Rosenkranz S. Pulmonary hypertension 2015: current definitions, terminology, and novel treatment options. Clin Res Cardiol Off J Ger Card Soc. 2015;104:197–207. https://doi.org/10.1007/s00392-014-0765-4.
Rosenkranz S, Gibbs JSR, Wachter R, et al. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37:942–54. https://doi.org/10.1093/eurheartj/ehv512.
Hoeper MM, Humbert M, Souza R, et al. A global view of pulmonary hypertension. Lancet Respir Med. 2016;4:306–22. https://doi.org/10.1016/S2213-2600(15)00543-3.
Rosenkranz S, Lang IM, Blindt R, et al. Pulmonary hypertension associated with left heart disease: updated recommendations of the Cologne Consensus Conference 2018. Int J Cardiol. 2018;272S:53–62. https://doi.org/10.1016/j.ijcard.2018.08.080.
Miller WL, Grill DE, Borlaug BA. Clinical features, hemodynamics, and outcomes of pulmonary hypertension due to chronic heart failure with reduced ejection fraction: pulmonary hypertension and heart failure. JACC Heart Fail. 2013;1:290–9. https://doi.org/10.1016/j.jchf.2013.05.001.
Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37:183–8. https://doi.org/10.1016/s0735-1097(00)01102-5.
Gerges M, Gerges C, Pistritto A-M, et al. Pulmonary hypertension in heart failure. Epidemiology, right ventricular function, and survival. Am J Respir Crit Care Med. 2015;192:1234–46. https://doi.org/10.1164/rccm.201503-0529OC.
Lam CSP, Roger VL, Rodeheffer RJ, et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53:1119–26. https://doi.org/10.1016/j.jacc.2008.11.051.
Leung CC, Moondra V, Catherwood E, Andrus BW. Prevalence and risk factors of pulmonary hypertension in patients with elevated pulmonary venous pressure and preserved ejection fraction. Am J Cardiol. 2010;106:284–6. https://doi.org/10.1016/j.amjcard.2010.02.039.
Obokata M, Olson TP, Reddy YNV, et al. Haemodynamics, dyspnoea, and pulmonary reserve in heart failure with preserved ejection fraction. Eur Heart J. 2018;39:2810–21. https://doi.org/10.1093/eurheartj/ehy268.
Reddy YNV, Olson TP, Obokata M, et al. Hemodynamic correlates and diagnostic role of cardiopulmonary exercise testing in heart failure with preserved ejection fraction. JACC Heart Fail. 2018;6:665–75. https://doi.org/10.1016/j.jchf.2018.03.003.
Maron BA, Brittain EL, Hess E, et al. Pulmonary vascular resistance and clinical outcomes in patients with pulmonary hypertension: a retrospective cohort study. Lancet Respir Med. 2020;8:873–84. https://doi.org/10.1016/S2213-2600(20)30317-9.
Bermejo J, González-Mansilla A, Mombiela T, et al. Persistent pulmonary hypertension in corrected valvular heart disease: hemodynamic insights and long-term survival. J Am Heart Assoc. 2021;10:e019949. https://doi.org/10.1161/JAHA.120.019949.
Caravita S, Dewachter C, Soranna D, et al. Haemodynamics to predict outcome in pulmonary hypertension due to left heart disease: a meta-analysis. Eur Respir J. 2018;51:1702427. https://doi.org/10.1183/13993003.02427-2017.
Galiè N, Manes A, Negro L, et al. A meta-analysis of randomized controlled trials in pulmonary arterial hypertension. Eur Heart J. 2009;30:394–403. https://doi.org/10.1093/eurheartj/ehp022.
Galiè N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J. 2019;53:1801889. https://doi.org/10.1183/13993003.01889-2018.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726. https://doi.org/10.1093/eurheartj/ehab368.
Guazzi M, Ghio S, Adir Y. Pulmonary hypertension in HFpEF and HFrEF: JACC review topic of the week. J Am Coll Cardiol. 2020;76:1102–11. https://doi.org/10.1016/j.jacc.2020.06.069.
Loai S, Cheng H-LM. Heart failure with preserved ejection fraction: the missing pieces in diagnostic imaging. Heart Fail Rev. 2020;25:305–19. https://doi.org/10.1007/s10741-019-09836-8.
Del Buono MG, Iannaccone G, Scacciavillani R, et al. Heart failure with preserved ejection fraction diagnosis and treatment: an updated review of the evidence. Prog Cardiovasc Dis. 2020;63:570–84. https://doi.org/10.1016/j.pcad.2020.04.011.
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61. https://doi.org/10.1056/NEJMoa2107038.
Solomon SD, McMurray JJV, Claggett B, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Desai AS, Jhund PS, Belohlavek J, Chiang CE, Borleffs CJW, Comin-Colet J, Dobreanu D, Drozdz J, Fang JC, Alcocer-Gamba MA, Al Habeeb W, Han Y, Cabrera Honorio JW, Janssens SP, Katova T, Kitakaze M, Merkely B, O'Meara E, Saraiva JFK, Tereshchenko SN, Thierer J, Vaduganathan M, Vardeny O, Verma S, Pham VN, Wilderäng U, Zaozerska N, Bachus E, Lindholm D, Petersson M, Langkilde AM; DELIVER Trial Committees and Investigators. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N Engl J Med. 2022;387(12):1089-98. https://doi.org/10.1056/NEJMoa2206286.
Buys R, Avila A, Cornelissen VA. Exercise training improves physical fitness in patients with pulmonary arterial hypertension: a systematic review and meta-analysis of controlled trials. BMC Pulm Med. 2015;15:40. https://doi.org/10.1186/s12890-015-0031-1.
Yuan P, Yuan X-T, Sun X-Y, et al. Exercise training for pulmonary hypertension: a systematic review and meta-analysis. Int J Cardiol. 2015;178:142–6. https://doi.org/10.1016/j.ijcard.2014.10.161.
Morris NR, Kermeen FD, Holland AE. Exercise-based rehabilitation programmes for pulmonary hypertension. Cochrane Database Syst Rev. 2017;1:CD011285. https://doi.org/10.1002/14651858.CD011285.pub2.
Grünig E, MacKenzie A, Peacock AJ, Eichstaedt CA, Benjamin N, Nechwatal R, Ulrich S, Saxer S, Bussotti M, Sommaruga M, Ghio S, Gumbiene L, Palevičiūtė E, Jurevičienė E, Cittadini A, Stanziola AA, Marra AM, Kovacs G, Olschewski H, Barberà JA, Blanco I, Spruit MA, Franssen FME, Vonk Noordegraaf A, Reis A, Santos M, Viamonte SG, Demeyer H, Delcroix M, Bossone E, Johnson M. Standardized exercise training is feasible, safe, and effective in pulmonary arterial and chronic thromboembolic pulmonary hypertension: results from a large European multicentre randomized controlled trial. Eur Heart J. 2021;42(23):2284-95. https://doi.org/10.1093/eurheartj/ehaa696.
Nagel C, Benjamin N, Egenlauf B, et al. Effect of supervised training therapy on pulmonary arterial compliance and stroke volume in severe pulmonary arterial hypertension and inoperable or persistent chronic thromboembolic pulmonary hypertension. Respir Int Rev Thorac Dis. 2021;100:369–78. https://doi.org/10.1159/000512316.
Grünig E, Ehlken N, Ghofrani A, et al. Effect of exercise and respiratory training on clinical progression and survival in patients with severe chronic pulmonary hypertension. Respir Int Rev Thorac Dis. 2011;81:394–401. https://doi.org/10.1159/000322475.
Grünig E, Eichstaedt C, Barberà JA, Benjamin N, Blanco I, Bossone E, Cittadini A, Coghlan G, Corris P, D'Alto M, D'Andrea A, Delcroix M, de Man F, Gaine S, Ghio S, Gibbs S, Gumbiene L, Howard LS, Johnson M, Jurevičienė E, Kiely DG, Kovacs G, MacKenzie A, Marra AM, McCaffrey N, McCaughey P, Naeije R, Olschewski H, Pepke-Zaba J, Reis A, Santos M, Saxer S, Tulloh RM, Ulrich S, Vonk Noordegraaf A, Peacock AJ. ERS statement on exercise training and rehabilitation in patients with severe chronic pulmonary hypertension. Eur Respir J. 2019;53(2):1800332. https://doi.org/10.1183/13993003.00332-2018.
de Man FS, Handoko ML, Groepenhoff H, et al. Effects of exercise training in patients with idiopathic pulmonary arterial hypertension. Eur Respir J. 2009;34:669–75. https://doi.org/10.1183/09031936.00027909.
Mereles D, Ehlken N, Kreuscher S, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. 2006;114:1482–9. https://doi.org/10.1161/CIRCULATIONAHA.106.618397.
Ehlken N, Lichtblau M, Klose H, et al. Exercise training improves peak oxygen consumption and haemodynamics in patients with severe pulmonary arterial hypertension and inoperable chronic thrombo-embolic pulmonary hypertension: a prospective, randomized, controlled trial. Eur Heart J. 2016;37:35–44. https://doi.org/10.1093/eurheartj/ehv337.
Taylor RS, Walker S, Smart NA, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: individual participant meta-analysis. J Am Coll Cardiol. 2019;73:1430–43. https://doi.org/10.1016/j.jacc.2018.12.072.
Taylor RS, Walker S, Smart NA, et al. Impact of exercise-based cardiac rehabilitation in patients with heart failure (ExTraMATCH II) on mortality and hospitalisation: an individual patient data meta-analysis of randomised trials. Eur J Heart Fail. 2018;20:1735–43. https://doi.org/10.1002/ejhf.1311.
Taylor RS, Long L, Mordi IR, et al. Exercise-based rehabilitation for heart failure: Cochrane systematic review, meta-analysis, and trial sequential analysis. JACC Heart Fail. 2019;7:691–705. https://doi.org/10.1016/j.jchf.2019.04.023.
Flynn KE, Piña IL, Whellan DJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301:1451–9. https://doi.org/10.1001/jama.2009.457.
Sagar VA, Davies EJ, Briscoe S, et al. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open Heart. 2015;2:e000163. https://doi.org/10.1136/openhrt-2014-000163.
Pandey A, Parashar A, Kumbhani D, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015;8:33–40. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001615.
Chan E, Giallauria F, Vigorito C, Smart NA. Exercise training in heart failure patients with preserved ejection fraction: a systematic review and meta-analysis. Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2016;86:759. https://doi.org/10.4081/monaldi.2016.759.
Dieberg G, Ismail H, Giallauria F. Smart NA (2015) Clinical outcomes and cardiovascular responses to exercise training in heart failure patients with preserved ejection fraction: a systematic review and meta-analysis. J Appl Physiol Bethesda Md. 1985;119:726–33. https://doi.org/10.1152/japplphysiol.00904.2014.
Fukuta H, Goto T, Wakami K, et al. Effects of exercise training on cardiac function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2019;24:535–47. https://doi.org/10.1007/s10741-019-09774-5.
Gomes-Neto M, Durães AR, Conceição LSR, et al. Effect of aerobic exercise on peak oxygen consumption, VE/VCO2 slope, and health-related quality of life in patients with heart failure with preserved left ventricular ejection fraction: a systematic review and meta-analysis. Curr Atheroscler Rep. 2019;21:45. https://doi.org/10.1007/s11883-019-0806-6.
Taylor RS, Davies EJ, Dalal HM, et al. Effects of exercise training for heart failure with preserved ejection fraction: a systematic review and meta-analysis of comparative studies. Int J Cardiol. 2012;162:6–13. https://doi.org/10.1016/j.ijcard.2012.05.070.
Palevičiūtė E, Šimbelytė T, Eichstaedt CA, Benjamin N, Egenlauf B, Grünig E, Čelutkienė J. The effect of exercise training and physiotherapy on left and right heart function in heart failure with preserved ejection fraction: a systematic literature review. Heart Fail Rev. 2023;28(1):193-206. https://doi.org/10.1007/s10741-022-10259-1.
Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. https://doi.org/10.1136/bmj.e7586.
Grünig E, Lichtblau M, Ehlken N, et al. Safety and efficacy of exercise training in various forms of pulmonary hypertension. Eur Respir J. 2012;40:84–92. https://doi.org/10.1183/09031936.00123711.
Nagel C, Prange F, Guth S, et al. Exercise training improves exercise capacity and quality of life in patients with inoperable or residual chronic thromboembolic pulmonary hypertension. PloS One. 2012;7:e41603. https://doi.org/10.1371/journal.pone.0041603.
Brooks D, Solway S, Gibbons WJ. ATS statement on six-minute walk test. Am J Respir Crit Care Med. 2003;167(9):1287. https://doi.org/10.1164/ajrccm.167.9.950.
McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. https://doi.org/10.1097/00005650-199303000-00006.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Vanderpool RR, Saul M, Nouraie M, et al. Association between hemodynamic markers of pulmonary hypertension and outcomes in heart failure with preserved ejection fraction. JAMA Cardiol. 2018;3:298–306. https://doi.org/10.1001/jamacardio.2018.0128.
Gorter TM, Obokata M, Reddy YNV, et al. Exercise unmasks distinct pathophysiologic features in heart failure with preserved ejection fraction and pulmonary vascular disease. Eur Heart J. 2018;39:2825–35. https://doi.org/10.1093/eurheartj/ehy331.
Acknowledgements
Not applicable.
Dissemination
Study results will be disseminated through publications in peer-reviewed scientific journals, relevant international clinical conferences, and patient societies. The core research center will circulate proposed publication topics to the principal investigators at each center, who will be asked to suggest and justify authorships.
Funding
This research received no specific grant from any funding agency in public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EG is the chief investigator. EG, EP, JČ, NB, and CAE constructed the protocol and study design. EP made the first draft of this manuscript. All authors contributed to the revisions and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Medical Faculty of Heidelberg University, Germany (S-879/2019; Local project ID: 2019-04ET; version 1.0, 5 December 2019). All participating centers will submit the study protocol to their local ethics committees. The study will be carried out following applicable local laws and regulations. Any changes to the protocol that may impact the conduct of the study, may potentiate benefit, or may affect patient’s safety will require formal approval by the local ethics committees.
Trained physicians will discuss the trial aspects with each patient, regarding its characteristics, consequences, potential impact on health issues, and benefit-risk ratio. Patients will have ample time and opportunity to ask questions and will be informed about the right to withdraw from the study at any time without any disadvantage and without having to provide reasons for this decision. Only patients who give their written, informed consent will be included in the study. The patient’s informed consent form is prepared in the native language. If needed for evaluation, it can be provided by the principal investigator of each center. The procedures set out in this protocol pertaining to the organization, evaluation, and documentation of this study will be conducted under Good Clinical Practice (GCP) guidelines and under the principles detailed in the Declaration of Helsinki. The data obtained during the trial will be treated pursuant to the General Data Protection Regulation (GDPR) (EU) 2016/679 and relevant national regulations.
Consent for publication
Not applicable.
Competing interests
E.P. reports speaker honoraria fees from Johnson and Johnson and Medis Pharma outside this work.
J.Č. reports personal fees from AstraZeneca, Boehringer Ingelheim, Pfizer, Bayer, and Novartis outside this work.
E.G. reports research grants and speaker honoraria/consultancy fees from Actelion, Janssen, Bayer, MSD, Merck, and Ferrer and research grants to the institution from Acceleron, Actelion, Bayer, MSD, Janssen, Liquidia, United Therapeutics, and OMT outside the submitted work.
L.G. has received speaker’s fees from Actelion, Johnson & Johnson, and Medis Pharma outside the submitted work.
S.Č. reports honoraria fees from Medtronic, Bostopn Scientific, and Meril outside this work.
T.Š., C.A.E, N.B., E.J., and D.Z. declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Reporting checklist for protocol of a clinical trial.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Palevičiūtė, E., Čelutkienė, J., Šimbelytė, T. et al. Safety and effectiveness of standardized exercise training in patients with pulmonary hypertension associated with heart failure with preserved ejection fraction (TRAIN-HFpEF-PH): study protocol for a randomized controlled multicenter trial. Trials 24, 281 (2023). https://doi.org/10.1186/s13063-023-07297-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-023-07297-x