Abstract
Rationale
The COVID-19 pandemic disrupted non-COVID critical care trials globally as intensive care units (ICUs) prioritized patient care and COVID-specific research. The international randomized controlled trial CYCLE (Critical Care Cycling to Improve Lower Extremity Strength) was forced to halt recruitment at all sites in March 2020, creating immediate challenges. We applied the CONSERVE (CONSORT and SPIRIT Extension for RCTs Revised in Extenuating Circumstance) statement as a framework to report the impact of the pandemic on CYCLE and describe our mitigation approaches.
Methods
On March 23, 2020, the CYCLE Methods Centre distributed a standardized email to determine the number of patients still in-hospital and those requiring imminent 90-day endpoint assessments. We assessed protocol fidelity by documenting attempts to provide the in-hospital randomized intervention (cycling or routine physiotherapy) and collect the primary outcome (physical function 3-days post-ICU discharge) and 90-day outcomes. We advised sites to prioritize data for the study’s primary outcome. We sought feedback on pandemic barriers related to trial procedures.
Results
Our main Methods Centre mitigation strategies included identifying patients at risk for protocol deviations, communicating early and frequently with sites, developing standardized internal tools focused on high-risk points in the protocol for monitoring patient progress, data entry, and validation, and providing guidance to conduct some research activities remotely. For study sites, our strategies included determining how institutional pandemic research policies applied to CYCLE, communicating with the Methods Centre about capacity to continue any part of the research, and developing contingency plans to ensure the protocol was delivered as intended. From 15 active sites (12 Canada, 2 US, 1 Australia), 5 patients were still receiving the study intervention in ICUs, 6 required primary outcomes, and 17 required 90-day assessments. With these mitigation strategies, we attempted 100% of ICU interventions, 83% of primary outcomes, and 100% of 90-day assessments per our protocol.
Conclusions
We retained all enrolled patients with minimal missing data using several time-sensitive strategies. Although CONSERVE recommends reporting only major modifications incurred by extenuating circumstances, we suggest that it also provides a helpful framework for reporting mitigation strategies with the goal of improving research transparency and trial management.
Trial registration
NCT03471247. Registered on March 20, 2018.
Similar content being viewed by others
Background
The novel coronavirus, SARS-CoV-2, first identified in Wuhan, China, in late December 2019 led to the World Health Organization (WHO) declaring a global pandemic on March 11, 2020. Concerns about personal protective equipment (PPE) supply and already strained health human resources challenged healthcare systems to minimize the demands on available resources, thus impacting the ability to conduct non-COVID-related research with patients. The anticipation of sharp increases in COVID-19 cases and hospitalizations raised further concerns about the availability and capacity to care for increased numbers of patients, the need for redeployment of research staff to meet clinical needs and/or prioritize COVID-related research, and mandates to transition to remote work.
COVID-19 imposed extenuating circumstances on clinical trials beyond the control of study investigators, sponsors, or funders. The CONSERVE (CONSORT and SPIRIT Extension for RCTs Revised in Extenuating Circumstance) 2021 statement was developed to extend the CONSORT (Consolidated Standards of Reporting Trials) [1, 2] and SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) [3] reporting guidelines to ensure the quality, completeness, and transparency of important protocol modifications due to extenuating circumstances for trials and trial protocols [4]. This guidance document encourages the research community to report how extenuating circumstances were managed, examine their overall impact, and take these modifications into account when interpreting trial results. Herein we report use of the CONSERVE-CONSORT Extension [4] as a framework to describe the CYCLE RCT (Critical Care Cycling to Improve Lower Extremity Strength; NCT03471247) study management during the first seven months of the pandemic. The CYCLE trial is currently underway.
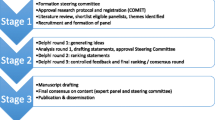
CYCLE is an international multicenter randomized controlled trial (RCT) examining in-bed cycling in critically ill, mechanically ventilated adults (target N = 360). CYCLE involves a complex in-hospital rehabilitation intervention provided in the ICU and relies on a multidisciplinary team of frontline healthcare providers and research personnel to implement the protocol. Patients are randomized to either 30-minutes of daily in-bed cycling and routine physical rehabilitation (PR) or routine PR alone, delivered by ICU physical and occupational therapists (hereafter called “interventionists”) 5 days per week until ICU discharge or 28 days, whichever comes first. Physical outcome measures are administered at 4 time points through the index ICU and hospital admission; the primary outcome is the Physical Function ICU Test (scored) [5], a performance-based physical function measure assessed at 3-days post-ICU discharge by acute care therapists (physical and occupational therapists, and therapy assistants, hereafter called “assessors”) blinded to treatment allocation. Patient-reported outcomes, administered by research coordinators (RCs), are assessed at 3 time points through the index ICU and hospital admission and at 90-days post-randomization. Figure 1 outlines the study schema. Since study initiation in 2016, CYCLE has been enrolling patients in 17 sites in 3 countries (Canada, USA, Australia) and 2 languages (English and French). Further information about the protocol is located at https://clinicaltrials.gov/ct2/show/NCT03471247, and a protocol paper is in preparation. The CYCLE Methods Centre, comprised of the Principal Investigator, lead research coordinators, and research assistants, is based at St. Joseph’s Healthcare (Hamilton, Canada), the primary CYCLE study site.
With the global pandemic declaration, CYCLE recruitment was interrupted. At the time of the interruption, the CYCLE trial was actively enrolling patients and conducting follow-up assessments. The Methods Centre personnel were also preparing for a pre-planned 180-patient interim analysis (half of the target 360-patient enrollment). Immediately following interruption, the Methods Centre identified 3 main impacts to CYCLE’s internal validity, including (1) in-hospital randomized intervention delivery (cycling and routine PR), (2) obtaining in-hospital primary outcome data, and (3) accurate, timely data entry and validation for patient safety monitoring in preparation for the pending interim analysis. Our aims were to honor our research commitment to patients enrolled before the pandemic, optimize cohort retention, minimize missing data, and continue to conduct the trial where ever it was feasible and safe. This report describes the CYCLE trial management Methods Centre response to the pandemic up to September 30, 2020.
Methods
The CYCLE Methods Centre developed several risk mitigation strategies to minimize impact of the COVID pandemic on the internal validity of the CYCLE RCT and report these using the framework of the CONSERVE-CONSORT Extension guidance [4]. The CONSERVE-CONSORT checklist can be found in Additional File 1: Appendix 1. To account for randomized patients (item 13: participant flow—number of participants randomized, losses and exclusions after randomization), we first developed structured communication using a standardized email (Additional File 1: Appendix 2) to determine (1) patient status and identify patients at risk of not receiving the allocated intervention, those pending primary outcome assessment, and 90-day assessments scheduled to occur by April 30, 2020, and (2) site staffing and availability (i.e., interventionists, assessors, and RCs for tracking patients, coordinating blinded outcomes assessments, and administering patient-reported outcome measures in-hospital and at the 90-day follow-up).
We developed internal Methods Centre communications to track patients, data progress, and personnel (research and clinical) across sites with the goals of providing support and guidance as required. We used these same communication strategies to reactivate sites when non-COVID-19 research resumed in some centers in late Spring 2020.
To track protocol fidelity, we focused on attempts to conduct study procedures, allowing us to discern pre-specified reasons for not completing a study procedure from reasons imposed by the pandemic. An “attempt” included any time an interventionist, assessor, or RC tried to deliver the intervention, collect the physical function or patient-reported assessments, or collect the 90-day assessments, as per study protocol. An attempt may or may not have resulted in successful conduct of the planned task. For example, if a patient was too sick to receive the assigned intervention, this was consistent with our protocol and therefore not considered a protocol deviation. If a task was not attempted due to pandemic-related factors (e.g., lack of staffing, PPE supply), we classified this as deviation from the initial protocol and documented specific reasons.
Our study focuses on four metrics we deemed critical to study internal validity. The first three related to participant flow (CONSERVE item 13). We documented the following attempts: in the hospital, randomized intervention delivery in the ICU and collection of the primary physical function outcome at 3 days following ICU discharge; post-hospital discharge, 90-day assessments scheduled up to April 30, 2020, within the prescribed timeframe (i.e., from 83–120 days post-randomization). We chose randomized intervention delivery as a measure of protocol fidelity and the primary outcome because of its highest importance among all other outcomes. We selected the April 30 timeline based on 2 factors: (1) initial reports planned for lockdowns of only 2-weeks duration and (2) allowing time for the Methods Centre to develop processes for ongoing remote data collection should lockdowns persist. The final metric, related to statistical methods (CONSERVE item 12), was timely data collection and entry to ensure completion of the interim analysis.
We analyzed all data descriptively and present figures where relevant.
Results
By February 21, 2020, CYCLE had trained 17 sites and enrolled 50% of the 360-patient target, triggering the initiation of a planned 180-patient interim analysis. On March 17, 2020, the province of Ontario (home to the main research ethics board for CYCLE) declared a provincial state of emergency. At this time, 197 (54.7%) patients had been enrolled, and all actively enrolling sites (15 of 17 sites, including 12 academic and 3 community) were forced to pause recruitment into any non-COVID studies, including CYCLE. Figure 2 is a timeline of key events, both globally and related to the CYCLE trial. For patients already enrolled, study procedures continued according to each institution’s policy.
Site characteristics
Research personnel at all sites were required to work from home; at all but one site, interventionists and assessors were permitted to complete in-hospital activities for enrolled patients. Among the 15 active sites, we identified 26 unique patients (13.2% of total CYCLE cohort) still actively on the study protocol: 10 patients in hospital (5 patients still receiving study intervention in the ICU, 6 requiring primary outcome assessment), and 17 requiring 90-day follow-up assessments by April 30, 2020. Table 1 details progression through the protocol by site for these 26 patients. Figure 3 summarizes the activities of all CYCLE sites and the Methods Centre from January to September 30, 2020.
Participant flow—intervention delivery
Five study patients were in ICU requiring the intervention; for all 5 patients, the allocated interventions were attempted at least once during the remainder of their respective intervention periods. Table 2 shows the number of attempted intervention days compared to the number completed, with reasons not done.
Participant flow—outcome assessments
Of the 10 study patients in hospital, 6 were pending primary outcome at 3-days post-ICU, and 5/6 (83%) were attempted. The primary outcome for one patient was not attempted due to an institutional policy prohibiting research staff from being on-site. Of 17 patients pending their 90-day follow-up assessments, 100% were attempted. Table 2 shows the number of attempted, successful, and missed outcomes, with reasons.
RCs identified 2 concerns for completing the 90-day follow-up assessments due to institutional directives to work remotely: (1) patient confidentiality (i.e., potential for identifying documentation in the homes of research personnel rather than in secured offices) and (2) research staff privacy (i.e., using personal phones to conduct follow-ups). In response, we developed a written guidance document to protect patient and research staff privacy and ensure data confidentiality (Additional file 1: Appendix 3).
Statistical analysis—data entry and validation
For research staff working from home, the Methods Centre provided guidance for how to access and use the database remotely. The Methods Centre provided one-on-one support for data entry and cleaning. Working with sites, we validated data for the first 180-patients and the interim analysis was completed on-time in September 2020.
Recruitment—site reactivation
Using a similar communication strategy to the start of the pandemic, we developed a standardized reactivation email template that each site completed before resuming screening and enrolment (Additional file 1: Appendix 4). Through this template, we sought to ensure there was sufficient interventionist, assessor, and research personnel capacity to optimize protocol fidelity in the moment and through potential future waves. We also advised sites to exclude ICU patients with COVID-19 because of the unknown risks of disease transmission via bike equipment surfaces, strained therapy resources (i.e., due to increased clinical responsibilities to care for patients with COVID-19, or staff unable to work because of illness or quarantine), and PPE supply concerns. Figure 4 depicts the CYCLE enrollment graph from study initiation to the end of September 2020. By September 30, 2020, 10 sites (67%) had been reactivated, though recruitment was slower than pre-pandemic. With the commencement of the second wave in Fall 2020, 1 site was paused again at the direction of local leadership.
In Tables 3 and 4, we summarize key tips we learned for Methods Centres and study sites, respectively to optimize cohort retention under extenuating circumstances.
Discussion
Optimizing participant flow, cohort retention, and continuing with timely data entry and validation while assuring the safety of patients, interventionists, assessors, and research personnel were our primary goals in navigating the CYCLE trial through the COVID-19 pandemic. Our implementation priorities were driven by patients’ progress in the protocol at the beginning of the pandemic. Throughout the COVID-19 pandemic, we learned important lessons and implemented crucial processes to ensure research integrity, and patient and staff safety. In this report, we documented our approaches to address extenuating circumstances and patient retention for a complex rehabilitation intervention in critically ill patients requiring multiple personnel with distinct research and clinical roles, which will enrich the interpretation of the trial results. Moreover, lessons learned may help Methods Centres and sites navigate extenuating circumstances, such as the COVID-19 pandemic. In addition, these strategies may support future capacity-building efforts in rehabilitation science and enhance the rigor and quality of clinical trials outside of extenuating circumstances.
At the start of the pandemic, researchers expressed many concerns about the conduct of non-COVID-19 clinical trials. Members of our group collaboratively developed guidelines for continuing or restarting non-pandemic focused research [6] as many clinical trials were interrupted or halted by the pandemic [7]. A myriad of challenges from these interruptions have included lost treatment opportunities for patients [8, 9], threatened trial equipment supply chains [9], missed medication doses in vulnerable populations [10], uncertainties about re-starting trials [11], and challenges with data integrity and interpretability due to intercurrent complications (e.g., unavailable study drug, treatment discontinuation due to COVID-19 illness, and missing data) [12,13,14]. Few publications have described specific trial experiences in the context of the current pandemic. Shiely et al. reported management of 8 commercial clinical trials of investigational medicinal products during COVID-19 [15], underscoring challenges related to site communication, intervention delivery, participant retention, and data collection. For example, these investigators implemented protocol modifications to optimize intervention delivery away from in-hospital to home settings (e.g., to administer medication infusions to immunocompromised patients), and outcome assessments from in-person to telephone follow-ups. The authors also shifted from paper to electronic case report forms to facilitate remote collection and entry. However, not all trial interventions or outcomes assessments can pivot to virtual platforms or in-home visits, either due to the intervention and outcomes themselves, or the target population; for example, in-bed cycling with critically ill patients must be delivered in-person in the ICU and performance-based outcome measures cannot occur virtually.
Changing the modes of intervention delivery and outcome assessment may affect the internal validity of the study. For example, transitioning from in-person to telephone outcomes may alter the psychometric properties of a measure. In contrast, changes to the mode of data collection from paper to electronic case report forms are less likely to negatively impact internal validity, though this change should still be documented. Finally, pausing recruitment and enrolment to ensure participant and personnel safety may not have significant impacts on the scientific rigor of studies in progress, but will extend the duration of planned enrolment, and associated costs [16]. Notwithstanding, investigators will need to assess whether the trial management strategies implemented due to extenuating circumstances such as the COVID-19 pandemic affect the validity of trial results. For example, we collected 3 out of the 6 patients requiring primary outcome assessments. While our initial sample size calculation estimated that we needed to enroll 360 patients after accounting for ICU mortality and missing data, we plan to re-evaluate the effect of the pandemic in terms of the scope of any additional missing primary outcome data on the overall trial cohort as we develop our final statistical analysis plan.
The authors of CONSERVE 2021 define extenuating circumstances as, “Unavoidable situations that prompt modifications to a trial. These are not usually under the control of study investigators, sponsors, or funders.” [4] CONSERVE, which recommends reporting details about trial modifications, how the modifications are important, the potential impacts of modifications, and a timeline, suggests this extension only be used when the extenuating circumstances result in important modifications that could have a potentially meaningful effect on a study’s research question, ethics, internal validity and generalizability, feasibility, or analytical methods and statistical power [4]. In March 2020, the duration and impact of the circumstances imposed by the pandemic were unknown. To honor our commitment to enrolled patients and to continue to advance our research agenda in the midst of unknown circumstances, we recognized that a systematic evaluation of our study processes was needed to determine which, if any, would require modifications and how to effectively mitigate potential pandemic impacts. For example, we elected not to enroll patients with COVID-19 for infection control concerns and the possibility of transmitting the virus through the equipment; furthermore, strained therapy resources could impair trial fidelity. We focused on mitigating the impact of the pandemic to patients already enrolled in the trial. The pandemic pause in enrollment has resulted in delayed recruitment leading to a later trial closure date, although randomization has restarted. Clinically, given the emerging evidence on Long COVID outcomes, future studies of ICU rehabilitation in patients with COVID-19 will be critical, but this discussion is beyond the scope of this study.
After careful evaluation, we did not make important modifications to the CYCLE intervention or outcomes assessments and conducted our interim analysis as planned. However, we did implement extensive mitigation strategies to protect participant flow and statistical analyses. For these reasons, we suggest the use of the CONSERVE reporting guidance for all trials that experienced extenuating circumstances as defined above—notably, all trials occurring during the COVID-19 pandemic. This is supported by CONSERVE authors [4] who state that while it was intended to capture important modifications, there may be opportunity to enhance reporting within a broader context. Understanding how trialists implement and evaluate mitigation strategies and their rationale for any important modifications will help future trialists respond and adjust to other unforeseen circumstances causing research disruptions. Given the known gap in evidence for trial management [17], the universal implementation of CONSERVE 2021 reporting in all instances of extenuating circumstances will enhance transparency in reporting and decision-making. In Fig. 5, we outline the stages in a study at which CONSERVE 2021 could be applied.
Strengths and limitations
Strengths of this study include focus on the conduct of an international multi-center trial of a complex rehabilitation intervention in acute care during the pandemic. We addressed key issues of data integrity, data completeness, and research ethics using the CONSERVE 2021 statement as a reporting framework for our trial in-progress. We reported our specific Methods Centre processes in the context of the COVID-19 pandemic, including practical examples and resources which could be generalizable to other complex interventions or studies including remote telephone follow-up. Our report also has limitations. First, it is focused on one trial underway in the ICU setting with follow-up in-hospital and beyond. Second, it does not address other parts of CONSERVE 2021, such as changing recruitment strategies or statistical analysis plans due to extenuating circumstances.
Conclusions
The pandemic has been a catalyst to identify guiding principles and develop contingency plans and mitigating strategies to optimize study recruitment, retention, fidelity and reporting in the face of unintended interruptions. Despite a complete pause in enrolment in this rehabilitation trial and an immediate transition to working from home for many research personnel, data integrity was maintained, the interim analysis was completed, and the study has since resumed enrolment at 10 of 15 sites.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUS:
-
Australia
- Ax:
-
Assessment
- CAN:
-
Canada
- CONSERVE:
-
CONSORT and SPIRIT Extension for RCTs Revised in Extenuating Circumstances
- CONSORT:
-
Consolidated Standards of Reporting Trials
- D:
-
Day
- D/C:
-
Discharge
- HCW:
-
Healthcare worker
- ICU:
-
Intensive care unit
- LTCHs:
-
Long-term care homes
- MC:
-
Methods Centre
- MV:
-
Mechanical ventilation
- ON:
-
Ontario
- PPE:
-
Personal protective equipment
- PR:
-
Physical rehabilitation
- PT:
-
Physiotherapy
- QC:
-
Quebec
- RC:
-
Research coordinator
- REB:
-
Research Ethics Board
- RCT:
-
Randomized controlled trial
- SDM:
-
Substitute decision maker
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- USA:
-
United States of America
- WHO:
-
World Health Organization
References
Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148(4):295–309. https://doi.org/10.7326/0003-4819-148-4-200802190-00008 148/4/295 [pii][published Online First: Epub Date]|.
Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869.
Chan AW, Tetzlaff JM, Gotzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. https://doi.org/10.1136/bmj.e7586 [published Online First: Epub Date]|.
Orkin AM, Gill PJ, Ghersi D, et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA. 2021. https://doi.org/10.1001/jama.2021.9941 [published Online First: Epub Date]|.
Denehy L, de Morton NA, Skinner EH, et al. A physical function test for use in the intensive care unit: validity, responsiveness, and predictive utility of the physical function ICU test (scored). Phys Ther. 2013;93(12):1636–45. https://doi.org/10.2522/ptj.20120310 [published Online First: Epub Date]|.
Cook DJ, Kho ME, Duan EH, et al. Principles guiding nonpandemic critical care research during a pandemic. Crit Care Med. 2020;48(10):1403–10. https://doi.org/10.1097/CCM.0000000000004538 [published Online First: Epub Date]|.
Duffett M, Cook DJ, Strong G, Lee JH, Kho ME. The effect of COVID-19 on critical care research during the first year of the pandemic: a prospective longitudinal multinational survey. medRxiv. 2021:2020.10.21.20216945. https://doi.org/10.1101/2020.10.21.20216945 [published Online First: Epub Date]|.
Peyrin-Biroulet L, Ananthakrishnan AN. Clinical research and trials-a “nonessential” victim of the COVID-19 pandemic? Am J Gastroenterol. 2020;115(6):946–7.
van Dorn A. COVID-19 and readjusting clinical trials. Lancet. 2020;396(10250):523–4. https://doi.org/10.1016/S0140-6736(20)31787-6 [published Online First: Epub Date]|.
Weinberg MS, Patrick RE, Schwab NA, et al. Clinical trials and tribulations in the COVID-19 era. Am J Geriatr Psychiatry. 2020;28(9):913–20. https://doi.org/10.1016/j.jagp.2020.05.016 [published Online First: Epub Date]|.
Mitchell EJ, Ahmed K, Breeman S, et al. It is unprecedented: trial management during the COVID-19 pandemic and beyond. Trials. 2020;21(1):1–7.
Akacha M, Branson J, Bretz F, et al. Challenges in assessing the impact of the COVID-19 pandemic on the integrity and interpretability of clinical trials. Stat Biopharm Res. 2020;12(4):419–26.
Meyer RD, Ratitch B, Wolbers M, et al. Statistical issues and recommendations for clinical trials conducted during the COVID-19 pandemic. Stat Biopharm Res. 2020;12(4):399–411.
Kunz CU, Jörgens S, Bretz F, et al. Clinical trials impacted by the COVID-19 pandemic: adaptive designs to the rescue? Stat Biopharm Res. 2020;12(4):461–77.
Shiely F, Foley J, Stone A, et al. Managing clinical trials during COVID-19: experience from a clinical research facility. Trials. 2021;22(1):62. https://doi.org/10.1186/s13063-020-05004-8 [published Online First: Epub Date]|.
US Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic: guidance for industry, investigators, and institutional review boards [Updated on April 16, 2020]. United States Food and Drug Administration; 2020.
Treweek S, Littleford R. Trial management- building the evidence base for decision-making. Trials. 2018;19(1):11. https://doi.org/10.1186/s13063-017-2322-8 [published Online First: Epub Date]|.
Acknowledgements
The authors are grateful to the following CYCLE Investigators (PI), physiotherapists (PT), occupational therapists (OT), research personnel (research coordinators, RC, research assistants, RA) for helping patients enrolled at the onset of the pandemic continue the protocol with minimal interruption. St. Joseph’s Hamilton Healthcare - Research Personnel: Dr. Jill Rudkowski (PI), France Clarke (RC), Stacey Priest (RA); PTs: Daana Ajami, Frances Garner, Kristy Obrovac, Laura Camposilvan (PT Assistant), Miranda Prince, Wendy Perry, Christine Neilson, Tina Memarzadeh, Tina Murphy, Magda McCaughan, Shivaun Davidson; McMaster Univeristy - Research Personnel: Diane Heels-Ansdell (Statistician), Quazi Ibrahim (Statistical Analyst), and Lisa Buckingham (Database Management); Juravinski Hospital - Research Personnel: Dr. Tim Karachi (PI), Tina Millen (RC), Lauren Locco (RA), Ryan Vaisler (RA), and Alia Khalid (RA); PT: Cortney Armstrong, Tania Brittain, Chris Farley, Leigh-Ann Niven, Gillian Manson, Jessica Temesy, Andrea Galli, Chelsea Hale, Helen Bishop, Jesse Coopman, Shannon Earl (PT Assistant), and Michael Cimcone; Hamilton General Hospital - Research Personnel: Yasmin Sivji (RC), Ellen McDonald (RC), Tracey Reynolds (Admin), Makena Pook (RC), Hassan Kashif (RC), and Lisa Klotz (RA); PT: Anastasia Newman, Elise Loreto, Ivone Ivone, Sarah Lohonyai, Jennifer Duley, Jacqueline Hockridge, Matt McCaffrey, Jessica Pilon-Bignell, Kristina Saric, Sue Mahler, and Melissa Richardson; St. Michael’s Hospital - Research Personnel: Marlene Santos (RC), Gyan Sandhu (RC), Orla Smith (RC), Imrana Khalid (RA), Jennifer Hodder (RA), and Kurtis Salway (RA); PT: Caity Heath, Deanna Feltracco, Kara Morrison, Olivia So, Amber Robertson, Anna Michalski, Meghan Robson, Christine Leger, Diana Horobetz, Natalia Zapata, Sarah Brown, Verity Tulloch, and Rose Lee; Duke University Hospital - Research Personnel: Katherine Sweeney (RC), Brett Koermer (RC/PT), Jennifer Kaisen, (RC) Melissa Minniti (RC), Andreea Podgoreanu (RC), Alicja Szydlowska (Administrator), Anne Davenport (RA), Cara Mariani (RC), Karen Clemons (RC), Stratton Barth (RC), Amanda Beaty (RC), and Gabriel Streisfeld (RC); PT/Rehab: Lane White, Meg Williamson (OT), Sara Dorn, Samantha Hoyle (OT), Michelle Iorio, Kyrsten Spurrier (OT), Grant Bitzer, Hannah McHugh, Melissa Kandel (OT), Tamara Klintworh-Kirk, Karlyn Schiltgen, Grace Ditzenberger (RA/PT student), Anne Kelly, Jessie Poteat (OT), and Karen Bienenstock; Mount Sinai Hospital - Research Personnel: Dr. Sangeeta Mehta (PI), Sumesh Shah (RC); PT: Celine Nathoo, Kristen Baxter, and Nick Bradley; University of Maryland Baltimore - Research Personnel: Olga Kolesnik (RC), Thelma Harrington (RC), Deana Tran (RA), Harsh Patel (RA), Zain Nagaria (RA), and Hassan Haji (RA); PT/Rehab: Chris Wells, Josh Vogel, Mary Hoyt, Katie DiAnthony (OT), Suzanne Dunn (OT), Alaina Bescia, and Eileen Connor; The Ottawa Hospital – Civic Campus - Research Personnel: Rebecca Porteous (RC), Brigette Gomes (RC), Sydney Miezitis (RA), Kaitlyn Montroy (RA), and Liane LeClair (RA); PT: Michelle Cummings, Rose Johnston, Tanya Forward and Sal Patten; The Ottawa Hospital – General Campus - Research Personnel: Irene Watpool (RC) and Heather Langlois (RA); PT: Josee Lamontagne, Karen Saab, Shelley DeRooy and Kristy Steeves; Austin Health - Research Personnel: Ally Macdonell (RC/PT), Sarah Retica (RC), and Ashleigh Donavon (RC); PT: Tom Rollinson, Joleen Rose, Hannah Verspey, Stephanie Biffano, Estelle Kyriacou, Laura Lehany, Lexie Mitris, Rebecca Parsons, Danielle Dunlop, Laura Montgomery, Tess O’Dea, Chris Ramlu, Caitlin Devanny, and Kylie Graham; Hôpital du Sacré-Cœur de Montréal - Research Personnel: Virginie Williams (RC), Julia Lainer Palacos (RA), and Mathilde Duplaix (RA); PTs: Genevieve Beauchamp-Vien, Xavier Bernet, Jennifer Bessette, Josianne Charbonneau, Huy-Thanh Bach, and Marianne Denommee; Hôpital Fleurimont – Sherbrooke - Research Personnel: Marilene Ladouceur (RC), Joannie Marchand (RC), Elaine Carbonneau (RC), Liné Côté (RC), Marie-Pier Bouchard (RA), and Marie Michelle-Watt (Admin); PT: Christine Lafonde, Pascale Girard, Nicole Marquis, Chantal Guillenette, and Cindy Lessard; Kingston Health Sciences Centre - Research Personnel: Miranda Hunt (RC), Tracy Boyd (RC), Michaela Hanley (RA), Donna Leybourne (Administrator), and Kimberley Smith (Administrator); PT: Mimi Anderson, Al MacVicar, Alyssa Whelan, Ashley Bridgen, Stephanie Bryan, Diane Challis, Susan Surca, Ashley Woodroffe-McClintock, and Angela Romero (PT Assistant); London Health Sciences Centre- Victoria Hospital - Research Personnel: Eileen Campbell (RC), Athena Ovsenek (RA), and Rebecca Rondinelli (RA); PT: Jennifer Curry, Kristen Abercrombie, Christine Smit, Lori Vantfoort, Michele Isenor, Tania Larsen, Erin Blackwell-Knowles, Jennifer Jackson, and Maciej Prajs; Niagara Health – St. Catharines Site - Research Personnel: Lisa Patterson (RC), Mercedes Camargo-Penuela (RC), Laurie Sadowski (RA), and Jane Jomy (RA); PT: Christina Carile, Daniel Aranda, Angie Dueck, Kathleen Reardon, Jennifer Wager, and Liz Bitzer; Hôpital Hôtel-Dieu de Lévis - Research Personnel: Estel Duquet-Deblois (RC), Julien Le Beller (RC), Rosalie Beaudoin (RA), Erik Celikovic (RA), and Alexandre Pepin (RA); PT: Karen Bolduc, Mylene Rochon, Stephane Guilbault, Claudia Hamel, and Isabelle Robitaille.
Funding
The CYCLE trial is funded by a Canadian Institutes of Health Research operating grant (PJT-155919) and a Canada Foundation for Innovation (228975) for study equipment. Dr. Michelle Kho and Dr. Deborah Cook are each funded by a Canada Research Chair. Dr. Julie Reid is funded by a Canadian Frailty Network Interdisciplinary Fellowship. The funders had no role in the conduct, analysis, interpretation, or reporting of this work.
Author information
Authors and Affiliations
Consortia
Contributions
Substantial contributions to conception or design: MEK, JCR, DJC, FL, LT. Acquisition, analysis, or interpretation of the data: JCR, AM, GS, LK, HO, MEK, DJC. Drafting the work: JCR, MEK. Critical revisions for important intellectual content: all authors. Final approval of the version submitted for publication: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Hamilton Integrated Research Ethics Board (HiREB) for all Hamilton study sites, by Clinical Trials Ontario for all Ontario, Canada study sites, and by all other sites’ local ethics committees. Participation in this study is voluntary and participants provide informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
CONSERVE-CONSORT Extension checklist. Appendix 2. Site communication template. Appendix 3. Working From Home – Conducting CYCLE Follow-up Phone Calls Remotely. Appendix 4. Site restart communication template and planning template.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reid, J.C., Molloy, A., Strong, G. et al. Research interrupted: applying the CONSERVE 2021 Statement to a randomized trial of rehabilitation during critical illness affected by the COVID-19 pandemic. Trials 23, 735 (2022). https://doi.org/10.1186/s13063-022-06640-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-022-06640-y