Abstract
Background
The objective of this study was to investigate the effects of Anethum graveolens (dill) powder supplementation on glycemic control, lipid profile, some antioxidants and inflammatory markers, and gastrointestinal symptoms in patients with type 2 diabetes.
Materials and methods
In this study, 42 patients with type 2 diabetes were randomly allocated to intervention and control groups and received either 3 g/day dill powder or placebo (3 capsules/day, 1 g each). Fasting blood sugar, insulin, homeostatic model assessment of insulin resistance, lipid profile, high-sensitivity C-reactive protein, total antioxidant capacity, malondialdehyde and gastrointestinal symptoms were measured in all of the subjects at baseline and postintervention.
Results
The dill powder supplementation significantly decreased the mean serum levels of insulin, homeostatic model assessment of insulin resistance, low-density lipoprotein cholesterol, total cholesterol and malondialdehyde in the intervention group in comparison with the baseline measurements (P < 0.05). Furthermore, the mean serum levels of high-density lipoprotein and total antioxidant capacity were significantly increased in the intervention group in comparison with the baseline measurement (P < 0.05). Colonic motility disorder was the only gastrointestinal symptom whose frequency was significantly reduced by supplementation (P = 0.01). The mean changes in insulin, low-density lipoprotein cholesterol, total cholesterol and malondialdehyde were significantly lower in the intervention group than in the control group (P < 0.05). In addition, the mean changes in high-density lipoprotein were significantly higher in the intervention group than in the control group (P < 0.05).
Conclusion
Dill powder supplementation can be effective in controlling the glycemic, lipid, stress oxidative and gastrointestinal symptoms in patients with type 2 diabetes.
Trial registration
Iran Clinical Trials Registry: IRCT20120704010181N12. Registered on 12 May 2018.
Similar content being viewed by others
Introduction
Diabetes is a public health problem that affected 285 million adults in 2010. That number is expected to rise to 439 million—or 7.7% of all adults—by 2030 [1]. In Iran, it has been estimated that 8% of the adult population has diabetes [2]. Major characteristics of type 2 diabetes mellitus (T2DM) are obesity, impaired insulin action, insulin secretory dysfunction and increased endogenous glucose output [3]. Increased free fatty acid flux secondary to insulin resistance is associated with diabetic dyslipidemia, including high plasma triglyceride concentration and low high-density lipoprotein cholesterol (HDL-C) concentration [4]. Inflammatory cytokines contribute to T2DM occurrence by affecting β cell function, which, in turn, promotes the long-term complications of diabetes by intensifying hyperglycemia [5]. Increased glucose uptake by endothelial cells under hyperglycemic conditions also leads to the increased production of free radicals, which decreases antioxidant levels [6]. It is commonly reported that patients with T2DM also encounter gastrointestinal complications, including gastroesophageal reflux disease, gastroparesis, enteropathy, nonalcoholic fatty liver disease and glycogenic hepatopathy [7].
Anethum graveolens L (commonly referred to as dill) is a herb commonly used both as a remedy and as a spice [8]. It grows in the Mediterranean region, in Europe, in central and southern Asia, and in the southeastern region of Iran [9]. A. graveolens leaves are a source of minerals, proteins and fibers [10]. A. graveolens oils are also a source of antioxidants and have antimicrobial and antispasmodic properties [11]. In traditional herbal medicine, A. graveolens is used to treat gastrointestinal ailments such as indigestion and flatulence [12]. A. graveolens has been shown to have anticancer, antimicrobial, antigastric irritation, anti-inflammatory and antioxidant properties [13]. In diabetic models, the administration of different extractions of A. graveolens seed had antioxidant, hypolipidemic and hypoglycemic effects [14].
Earlier studies have reported inconsistent findings regarding the protective effects of A. graveolens on the lipid profile and insulin resistance in patients with metabolic syndrome [15, 16]. Randomized clinical trials showed that A. graveolens reduced total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) but did not change triglyceride or HDL-C levels in patients with T2DM [17]. It has also been reported that A. graveolens could have beneficial effects on some inflammatory biomarkers [18] and controversial effects on glucose and insulin [18, 19]. Given the inconclusive results related to glycemic, lipid and inflammatory profiles, it is not clear whether A. graveolens helps to increase antioxidants or improve gastrointestinal symptoms. Therefore, the present study was designed to examine the effects of A. graveolens powder on the serum levels of glycemic parameters, lipid profile, some antioxidants, inflammatory markers and gastrointestinal symptoms in patients with T2DM.
Materials and methods
Study design and participants
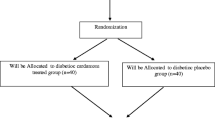
A single-center, randomized, double-blind, placebo-controlled study was conducted with 100 patients with T2DM. The patients were recruited from the endocrinology and metabolism clinics of Golestan Hospital at Ahvaz Jundishapur University of Medical Science in Iran between 2017 and 2018 (Fig. 1).
Inclusion criteria were as follows: the patient has diabetes mellitus; is aged 30–60 years; has gastrointestinal symptoms; has a body mass index (BMI) between 25 and 35 kg/m2; does not have systemic diseases, thyroid disease, or a kidney disorder; is not pregnant or lactating; and is not taking any dietary supplements or antioxidants, immunosuppressants, or anti-inflammatory agents. Exclusion criteria were the patient shows noticeable changes in the dose of medications and treatment of diabetes, refuses to continue participating in the study, or has less than 90% compliance with the dill capsules.
The diagnosis of T2DM was made according to American Diabetes Association guidelines. Patients with fasting blood sugar (FBS) ≥126 mg/dl, 2-h plasma glucose ≥200 mg/dl, or glycated hemoglobin ≥6.5% were diagnosed with diabetes mellitus [20].
Fifty-two patients did not qualify for this study due to not meeting the inclusion criteria, such as gastrointestinal symptoms and not agreeing to participate. Forty-eight patients were randomly assigned to two groups of intervention (n = 24) or placebo (n = 24) for 8 weeks. Randomization was performed using computer-generated random numbers by a third person to reduce bias. The third person generated a random block in blocks of 4. The naming of dill or placebo bottles was performed according to random numbers. Odd or even numbers were allocated randomly to groups A or B. A multipart questionnaire including demographic data (age and sex), anthropometric indices, dietary intake, medication, diabetes duration (in years), physical activity and gastrointestinal symptoms was obtained from the subjects. During each visit, every patient was given dill supplement or placebo for 4 weeks, and throughout these weeks the consumption of supplements or placebo by the patients was ensured through telephone calls or text messages. The compliance of patients was checked by counting the remaining capsules. Patients were excluded from the study if they had consumed less than 90% of the prescribed capsules. All participants were asked not to consume dill in their diet during the study. The protocol of this study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (ethical code IR.AJUMS.REC.1396.623) and this study was registered in the Iranian Registry of Clinical Trials website (IRCT20120704010181N12) which is available at http://irct.ir/user/trial/20288/view. Written informed consent was obtained from all participants.
Supplement and placebo prescription
After confirmation of the A. graveolens (dill) herb by the botanist, dried leaves were milled to powder. Capsules containing 1 g dill powder were provided by the Faculty of Pharmacy, Ahvaz Jundishapur University of Medical Sciences. In this study, starch was used as the placebo. The intervention and control groups received either three capsules of 1 g dill or placebo three times per day after each meal (breakfast, lunch and dinner) for 8 weeks. The placebo and dill capsules were matched in terms of size, taste, color and shape.
Assessment of demographic data, anthropometric indices and food intake
Dietary intake was investigated with a 24-h food recall for 3 days (2 weekdays and 1 weekend day) and dietary intake was analyzed by Nutritionist 4 software specified for Iranian foods. Anthropometric indices (weight, height and BMI) were measured by a trained researcher (nutritionist) at baseline and after the 8-week intervention. Weight (Seca, Germany) was measured while the patients wore light clothing and no shoes at 0.1-kg accuracy. Height was measured using a stadiometer (Seca) with 0.5-cm accuracy without shoes. BMI was calculated (weight in kilograms divided by the square of the height in meters). Physical activity level was evaluated by the Persian form of the International Physical Activity Questionnaire and presented in metabolic equivalent of task (MET) minutes/week. The participants were asked not to change their ordinary dietary intake and physical activity during the intervention.
Assessment of gastrointestinal symptoms
The assessment of gastrointestinal symptoms was performed by questionnaire at the baseline and at the end of the study [21]. This questionnaire included gastrointestinal symptoms such as gastroesophageal reflux, esophageal motility disorders, dyspepsia, gastric motility disorders and colonic motility disorders.
The numbers 0, 1 and 2 indicate the severity of gastrointestinal symptoms, where 0 = the patient did not have gastrointestinal symptoms, 1 = the patient had occasional gastrointestinal symptoms, and 2 = the patient had permanent gastrointestinal problems.
Biochemical assays
Fasting blood samples (5 ml) were collected from all participants at the beginning and end of the study and were immediately centrifuged (3000×g, 10 min, 4°C). Blood samples were poured into anticoagulant tubes to extract serum samples and were sent to the laboratory in cool boxes. All samples were stored at −70°C until biochemical analyses. Serum glucose, triglyceride (TG), HDL and TC was measured by standard enzymatic methods using the Pars Azmoun kit (Tehran, Iran). Serum insulin was measured by a human insulin enzyme-linked immunosorbent assay kit (Monobind Inc.). Insulin resistance was estimated according to the homeostatic model assessment of insulin resistance (HOMA-IR), calculated as: HOMA-IR = fasting concentrations of glucose (mg/dl) × fasting insulin (μU/ml) / 405 [22]. The Friedewald formula was used for the calculation of LDL-C [23]:
LDL-C (mg/dl) = TC (mg/dl) − HDL-C (mg/dl) − TG (mg/dl)/5, where TG/5 is used to represent very-low-density lipoprotein cholesterol.
Serum markers of oxidative stress such as total antioxidant capacity (TAC) and malondialdehyde (MDA) were measured by reliable spectrophotometric methods using Zell Bio GmbH kit (Germany). Serum levels of high-sensitivity C-reactive protein (hs-CRP) were measured by enzyme-linked immunosorbent assay kits (Monobind Inc.).
Outcomes
In this study, LDL-C was considered as the primary outcome. The secondary measurement outcomes were glycemic parameters, other factors of the lipid profile, some antioxidant and inflammatory markers, and gastrointestinal symptoms.
Statistical analysis
The sample size (95% confidence interval and 80% power) was computed according to the study of Mobasseri et al. [17] and considering LDL-C as the main outcome. Sample size was 21 subjects for each group; 24 subjects were computed in each group allowing for 10% withdrawal. All statistical analyses was performed using SPSS 25. All data were reported as means with standard deviations for quantitative variables or number and percentage for qualitative variables. The normality of the distribution of the data was checked using the Kolmogorov–Smirnov test. A paired sample t test was used to compare the results within groups postintervention. An independent sample t test was performed to compare the results between the two groups (placebo and intervention). Furthermore, an independent t test was used to identify differences between the two groups at the end of the study. The mean changes in variables were calculated using the mean differences of data before and after the study. Analysis of covariance was used to identify any differences between the two groups at the end of the study, adjusting for baseline values and covariates. Furthermore, a chi-squared test was used for statistical analysis of qualitative variables. P values less than 0.05 were considered statistically significant in all analyses.
Results
Baseline characteristics of the subjects, anthropometric parameters and dietary intake
Overall, 42 patients with T2DM (intervention group, n = 21; control group, n = 21) completed the study over 8 weeks. The mean age of patients in the intervention and control groups was 50.66 ± 8.22 and 50.42 ± 8.61 years, respectively. No significant differences (P ≥ 0.05) were observed in demographic and anthropometric characteristics, duration of diabetes, physical activity or medications between the two groups at baseline (Table 1). No significant differences were observed between the two groups for dietary intake including energy, macronutrients or micronutrients such as antioxidant vitamins C and E at baseline and after the intervention (P ≥ 0.05) (Table 2).
Glycemic control
The results of this study showed that no significant differences were observed in FBS, insulin and HOMA-IR between the two groups at baseline (P ≥ 0.05). It was demonstrated that 8 weeks consumption of dill powder significantly decreased the mean serum levels of insulin and HOMA-IR in the intervention group by the end of the study in comparison with the baseline (insulin: 13.27 ± 3.8 vs 10.54 ± 4.51 μU/ml, respectively; P = 0.004; HOMA-IR: 4.88 ± 2.37 vs 3.86 ± 2.32, respectively; P = 0.039). Furthermore, the insulin levels decreased to a greater extent in the intervention group between the start and the end of the study than in the control group (−2.7 ± 3.83 vs 0.50 ± 4.36, respectively; P = 0.015). Analysis of covariance showed that, after adjusting for confounding factors (age, duration of disease, changes in BMI, dietary intake of energy, macronutrients, vitamin A, C and E, and physical activity), the mean changes in insulin were not significantly lower in the intervention group in comparison with the control group after the intervention (Table 3).
Lipid profile
At baseline, there were no significant differences in the mean serum levels of TG, TC, LDL-C and HDL between the two groups (P > 0.05). The dill powder supplementation significantly increased the mean serum levels of HDL in the intervention group in comparison with baseline (44.80 ± 9.89 vs 41.85 ± 11.68 mg/dl, respectively; P = 0.007). Furthermore, the mean changes in serum levels of HDL were significantly higher in the intervention group compared to the control group (2.59 ± 4.51 vs −1.38 ± 4.60 mg/dl, respectively; P = 0.004). Even after adjusting for confounding factors, there was a significant difference in the mean change in HDL-C between the two groups (P = 0.04). In the intervention group, the mean serum levels of LDL-C and TC were significantly decreased postintervention (LDL-C: 81.00 ± 34.79 to 71.23 ± 26.63 mg/dl, respectively; P = 0.029; TC: 160.28 ± 38.26 to 149.23 ± 26.7 mg/dl, respectively; P = 0.03). Furthermore, the serum levels of LDL-C decreased to a greater extent in the intervention group between the start and the end of the study than in the control group (−9.76 ± 19.08 vs 3.09 ± 14.07 mg/dl, respectively; P = 0.017). After adjusting for confounding factors, there was a significant difference in mean change in LDL-C and TC between two groups (P = 0.04 and P = 0.033, respectively). However, no significant changes were observed in the mean serum levels of TG after the intervention (P ≥ 0.05) (Table 3).
Antioxidant and inflammatory markers
According to the analysis, there were no significant differences in the mean serum levels of hs-CRP, MDA and TAC between the intervention and control groups at baseline (P ≥ 0.05). The results of the present study showed that in the intervention group the mean MDA was reduced significantly postintervention in comparison with baseline (3.34 ± 2.05 to 2.22 ± 1.57 μM, respectively; P = 0.034). At the end of study, there was a significant difference in the mean changes in MDA between the intervention and control groups both without and with adjusting for confounding factors (−1.11 ± 2.24 vs 0.33 ± 1.62 μM, respectively; P = 0.021 vs P = 0.013, respectively). Within-group comparison in the intervention group showed that the mean serum levels of TAC significantly increased after 8 weeks of supplementation (0.19 ± 0.05 to 0.25 ± 0.09 mM, respectively; p = 0.025). In addition, after the supplementation, the mean serum levels of TAC were significantly higher in the intervention group in comparison with the control group (0.25 ± 0.09 vs 0.16 ± 0.06 mg/dl, respectively; P = 0.001). This result for TAC was also observed after adjusting for confounding factors (P = 0.004). No significant difference was observed for hs-CRP within and between the two groups (P ≥ 0.05) (Table 4).
Gastrointestinal symptoms
Based on the results presented in Table 5, supplementation with dill failed to reduce the frequency of gastrointestinal symptoms such as gastroesophageal reflux, esophageal motility, dyspepsia and gastric motility disorders in comparison with the baseline measurements (P ≥ 0.05). Amongst all the symptoms, only colonic motility disorders had their frequency significantly reduced by supplementation (P = 0.01), and this decrease was more notable in patients with severe gastrointestinal problems. In the control group, meanwhile, there was no significant reduction in the frequency of gastrointestinal symptoms (P ≥ 0.05).
Safety, adverse effects and monitoring data
A Data Monitoring Committee supervised this study to detect any possible side effects and to report to the ethics committee of Ahvaz Jundishapur University of Medical Sciences. However, no significant side effects from dill administration were reported in this study.
Discussion
This study revealed that 8 weeks of supplementation with 3 g/day A. graveolens reduced serum insulin and HOMA-IR. Moreover, A. graveolens might significantly reduce the serum levels of LDL and TC and enhance HDL when compared to a placebo condition. Patients in the intervention group had low MDA and TAC; however, no significant changes were observed for the serum levels of hs-CRP. In terms of gastrointestinal symptoms, only colonic motility disorders decreased.
These findings are in line with those of several interventional studies confirming the benefits of A. graveolens in improving T2DM and metabolic syndrome [14, 16]. The significant reduction in HOMA-IR and serum levels of insulin indicates that A. graveolens has a role to play in reducing insulin resistance. Similar beneficial effects of A. graveolens on glycemic control have been reported previously. Supplementation of patients with T2DM with 3.3 g/day of A. graveolens powder for 8 weeks could significantly reduce levels of insulin [17]. After 6 weeks of supplementation with 1.5 g/day of dill powder tablets, serum levels of FBS were significantly reduced in patients with T2DM [19].
Although Payahoo et al. [18] found a significant decrease in serum levels of insulin, no significant effect was observed for HOMA-IR, which could be due to the reduced levels of FBS in diabetic patients. High antioxidant content (i.e., vitamin C, polyphenols and carotenoids) in A. graveolens neutralizes reactive oxygen species and thus plays a role in repairing β cell function and insulin secretion [24, 25].
In this study, serum concentrations of LDL-C and TC decreased, while HDL-C increased significantly at the end of the study. No significant change was seen for serum levels of TG. In agreement with our study, Rashidlamir et al. [26] showed that aerobic training with the use of 2.7 g/day A. graveolens resulted in increased HDL and a decreased LDL to HDL ratio in diabetic women compared with the control group; findings for TC, meanwhile, were not statistically significant. In contrast, supplementation with 650 mg A. graveolens tablets twice daily increased the serum levels of TG in patients with hyperlipidemia, but no significant changes were seen in TC or LDL [15].
The treatment of hyperlipidemic patients with 1 g/day A. graveolens powder for 4 weeks resulted in a significant reduction in the levels of TC, TG, LDL and very-low-density lipoprotein when compared to patients treated with 20 mg/day lovastatin tablets. However, no significant change was observed in the serum levels of HDL [27].
The exact mechanism of the lipid-lowering effects of A. graveolens is not yet determined. However, it may relate to the decreased absorption of cholesterol by binding to bile acids, the inhibition of cholesterol and fatty acid synthesis through the suppression of acetyl-CoA carboxylase and HMG-COA reductase activity, and the stimulation of cholesterol clearance by increasing LDL receptors [28,29,30].
In this study, patients who received 3 g/day A. graveolens had lower levels of MDA and higher levels of TAC than patients in the control group, both in crude and adjusted models. MDA is a product of lipid peroxidation and is recognized as an atherogenic agent. Patients with elevated levels of MDA are more susceptible to atherosclerosis, diabetes and other metabolic disorders [31].
Findings from animal studies showed that the administration of different fractions of A. graveolens to animals on a high-fat diet decreased their MDA levels and increased the activities of antioxidant enzymes, including superoxide dismutase and catalase. It also increases the levels of glutathione, thus playing a key role in scavenging reactive oxygen species [32]. Hamsters treated with A. graveolens extracts or tablets exhibited a significant increase in TAC levels when compared to those on a high-cholesterol diet [33]. A. graveolens is composed of a variety of antioxidants, such as flavonoids that are capable of scavenging free radicals [34]. The enhanced levels of antioxidant activity in response to A. graveolens might be due to the content of polyphenols and flavonoids. It is possible that normal levels of antioxidants protect individuals against several chronic diseases [35].
We observed a nonsignificant decrease in serum levels of hs-CRP after supplementation with A. graveolens. The fact that an increase in bodyweight is an indicator of inflammation [36] could be why a nonsignificant reduction in serum levels of hs-CRP was observed in our study. The anti-inflammatory effects of different forms of A. graveolens have been shown in several animal studies [37,38,39]. Payahoo et al. [18] found a significant decrease in the serum levels of inflammatory biomarkers—including hs-CRP, interleukin-6 and tumor necrosis factor—after 8 weeks of supplementation with 3.3 g dill powder.
In terms of gastrointestinal symptoms, we observed a significant decrease only in colonic motility disorders. It is reported that the most prevalent symptoms among patients with diabetes are colonic motility disorders, which increase with age [21]. The prevalence of gastrointestinal symptoms is positively associated with the duration of diabetes [21, 40]. Patients included in the current study had a mean age of 50 years and a mean disease duration of 8 years—both of which are relatively high. This could be a reason for the observed findings in this regard. Earlier animal models show that A. graveolens extract is a potent relaxant of contractions in rat ileum and has antisecretory and antiulcer capabilities as it relates to HCl- and ethanol-induced stomach lesions [41, 42].
To the best of our knowledge, this is the first human study investigating the effects of A. graveolens on gastrointestinal symptoms. The major strength of this study was its design as a well-controlled, double-blind clinical trial that controlled for several main confounding factors in different models.
However, there are some limitations to our study. First, this is a single-dose trial, thus preventing any dose-effect associations. It remains unclear whether larger or smaller doses could introduce a stronger clinical effect. Second, the narrow range of inclusion criteria led to unrepresentative samples, therefore limiting the generalizability of the study results to all patients with diabetes. Third, only the data of subjects who completed the study were analyzed; the data of those who were excluded were not measured.
Conclusion
This study highlights the beneficial effects of A. graveolens on insulin resistance, LDL and HDL cholesterol, TC, antioxidant levels and some gastrointestinal symptoms in comparison with a placebo during 8 weeks of supplementation. Further studies are needed to determine molecular levels and to clarify the role of A. graveolens in the treatment of diabetes complications.
Availability of data and materials
The results will not be available before publishing.
Abbreviations
- BMI:
-
Body mass index
- FBS:
-
Fasting blood sugar
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- hs-CRP:
-
High-sensitivity C-reactive protein
- LDL-C:
-
Low-density lipoprotein cholesterol
- MDA:
-
Malondialdehyde
- T2DM:
-
Type 2 diabetes mellitus
- TAC:
-
Total antioxidant capacity
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14 PubMed PMID: 19896746. Epub 2009/11/10.
Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, et al. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: national survey of risk factors for non-communicable diseases of Iran. Diabetes Care. 2008;31(1):96–8 PubMed PMID: 17921357. Epub 2007/10/09.
Rosal MC, Borg A, Bodenlos JS, Tellez T, Ockene IS. Awareness of diabetes risk factors and prevention strategies among a sample of low-income Latinos with no known diagnosis of diabetes. Diabetes Educ. 2011;37(1):47–55 PubMed PMID: 21220363. Epub 2011/01/12.
Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5(3):150–9 PubMed PMID: 19229235. Epub 2009/02/21.
Lontchi-Yimagou E, Sobngwi E, Matsha TE, Kengne AP. Diabetes mellitus and inflammation. Curr Diab Rep. 2013;13(3):435–44 PubMed PMID: 23494755. Epub 2013/03/16.
Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005;115(5):1111–9 PubMed PMID: 15864338.
Krishnan B, Babu S, Walker J, Walker AB, Pappachan JM. Gastrointestinal complications of diabetes mellitus. World J Diabetes. 2013;4(3):51–63 PubMed PMID: 23772273. Epub 2013/06/15.
Saleh-E-In MM, Sultana N, Rahim MM, Ahsan MA, Bhuiyan MNH, Hossain MN, et al. Chemical composition and pharmacological significance of Anethum sowa L. root. BMC Complement Altern Med. 2017;17(1):127 PubMed PMID: 28231789.
Mozaffarian VA. Dictionary of Iranian plant names. Tehran: Farhang Moaser Publications; 1995. p. 44.
Rekha MNYA, Dharmesh S, Chauhan AS, Ramteke RS. Evaluation of antioxidant properties of dry soup mix extracts containing dill (Anethum sowa L.) leaf. Food Bioprocess Technol. 2010;3:441–9.
Singh G, Maurya S, De Lampasona M, Catalan C. Chemical constituents, antimicrobial investigations, and antioxidative potentials of Anethum graveolens L. essential oil and acetone extract: Part 52. J Food Sci. 2005;70(4):M208–M15.
Thomson PDR Staff. PDR for herbal medicines. 3rd ed. Thomson PDR; 2004.
Oshaghi EA, Khodadadi I, Tavilani H, Goodarzi MT. Effect of dill tablet (Anethum graveolens L) on antioxidant status and biochemical factors on carbon tetrachloride-induced liver damage on rat. Int J Appl Basic Med Res. 2016;6(2):111.
Goodarzi MT, Khodadadi I, Tavilani H, Abbasi Oshaghi E. The role of Anethum graveolens L. (dill) in the management of diabetes. J Trop Med. 2016;2016:1098916 PubMed PMID: 27829842. Pubmed Central PMCID: PMC5088306. Epub 2016/11/11.
Kojuri J, Vosoughi AR, Akrami M. Effects of Anethum graveolens and garlic on lipid profile in hyperlipidemic patients. Lipids Health Dis. 2007;6(1):5.
Mansouri M, Nayebi N, Hasani-Ranjbar S, Taheri E, Larijani B. The effect of 12 weeks Anethum graveolens (dill) on metabolic markers in patients with metabolic syndrome; a randomized double blind controlled trial. DARU J Pharm Sci. 2012;20(1):47.
Mobasseri M, Payahoo L, Ostadrahimi A, Khaje Bishak Y, Asghari Jafarabadi M, Mahluji S. Anethum graveolens supplementation improves insulin sensitivity and lipid abnormality in type 2 diabetic patients. J Pharm Sci. 2014;20(2):40–5.
Payahoo L, Khaje-Bishak Y, Mobasseri M, Ostadrahimi A, Asghari-Jafarabadi M. The effects of Anethum graveolens L supplementation on the insulin resistance and inflammatory biomarkers in patients with type 2 diabetes. JIMS. 2015;32(320):2473–83.
Sargolzari MS, Mansouri A, Shahdadi H, Masinaei Nezhad N, Poodineh Moghadam M. The effect of dill tablet on the level of fasting blood sugar in patients with type II diabetes. J Diabetes Nurs. 2017;5(2):86–94.
Ta S. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81.
Shahbazian H, Hashemi SJ, Arghideh M, Fardad F, Latifi SM. Prevalence of gastrointestinal symptoms in type 2 diabetic patients and its association with glycemic control and duration of diabetes. Iran J Endocrinol Metab. 2012;13(5):459–66.
Fujii H, Imajo K, Yoneda M, Nakahara T, Hyogo H, Takahashi H, et al. HOMA-IR: An independent predictor of advanced liver fibrosis innondiabetic non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2019;34(8):1390–5.
Moravej Aleali A, Amani R, Shahbazian H, Namjooyan F, Latifi SM, Cheraghian B. The effect of hydroalcoholic Saffron (Crocus sativus L.) extract on fasting plasma glucose, HbA1c, lipid profile, liver, and renal function tests in patients with type 2 diabetes mellitus: A randomized double-blind clinical trial. Phytother Res. 2019;33(6):1648–57.
Agte VV, Tarwadi KV, Mengale S, Chiplonkar SA. Potential of traditionally cooked green leafy vegetables as natural sources for supplementation of eight micronutrients in vegetarian diets. J Food Compos Anal. 2000;13(6):885–91.
Madani H, Ahmady Mahmoodabady N, Vahdati A. Effects of hydroalchoholic extract of Anethum graveolens (dill) on plasma glucose an lipid levels in diabetes induced rats. Iran J Diabetes Metab. 2005;5(2):109–16.
Rashidlamir A, Gholamian S, Javaheri AH, Dastani M. The effect of 4-weeks aerobic training according with the usage of Anethum graveolens on blood sugar and lipoproteins profile of diabetic women. Ann Biol Res. 2012;3(9):4313–9.
Sahib AS, Mohammad IH, AlGareeb A. Effects of Anethum graveolens leaf powder on lipid profile in hyperlipidemic patients. Spatula DD. 2012;2(3):153–8.
Yazdanparast R, Bahramikia S. Evaluation of the effect of Anethum graveolens L. crude extracts on serum lipids and lipoproteins profiles in hypercholesterolaemic rats. DARU J Pharm Sci. 2008;16(2):88–94.
Piri M, Shahin M, Oryan S. The effects of Anethum on plasma lipid and lipoprotein in normal and diabetic rats fed high fat diets. J Shahrekord Univ Med Sci. 2010;11(4):15–25.
Haghighi B, Kharazizadeh M, Attar M. Possible involvement of hepatic phosphatidate phosphohydrolase in the mechanisms of actions of certain antilipemic drugs in rats. J. Iran J Pharm Res. 2010;6(4):273–8.
Bakhtiari A, Hajian-Tilaki K, Omidvar S, Nasiri Amiri F. Association of lipid peroxidation and antioxidant status with metabolic syndrome in Iranian healthy elderly women. Biomed Rep. 2017;7(4):331–6 PubMed PMID: 28928971. Epub 2017/08/09.
Bahramikia S, Yazdanparast R. Efficacy of different fractions of Anethum graveolens leaves on serum lipoproteins and serum and liver oxidative status in experimentally induced hypercholesterolaemic rat models. Am J Chin Med. 2009;37(04):685–99.
Abbasi-Oshaghi E, Khodadadi I, Tavilani H, Mirzaei F, Goodarzi MT. Dill-normalized liver lipid accumulation, oxidative stress, and low-density lipoprotein receptor levels in high cholesterol fed hamsters. ARYA Atheroscler. 2018;14(5):218–24 PubMed PMID: 30783412.
Mateos R, Lecumberri E, Ramos S, Goya L, Bravo L. Determination of malondialdehyde (MDA) by high-performance liquid chromatography in serum and liver as a biomarker for oxidative stress. Application to a rat model for hypercholesterolemia and evaluation of the effect of diets rich in phenolic antioxidants from fruits. J Chromatogr B Anal Technol Biomed Life Sci. 2005;827(1):76–82 PubMed PMID: 16009604. Epub 2005/07/13.
Kaplan M, Aviram M. Oxidized low density lipoprotein: atherogenic and proinflammatory characteristics during macrophage foam cell formation. An inhibitory role for nutritional antioxidants and serum paraoxonase. Clin Chem Lab Med. 1999;37(8):777–87 PubMed PMID: 10536926. Epub 1999/10/28.
Adebayo AH, Abolaji AO, Opata TK, Adegbenro IK. Effects of ethanolic leaf extract of Chrysophyllum albidum G. on biochemical and haematological parameters of albino Wistar rats. Afr J Biotechnol. 2010;9:2145–50.
Valady A, Nasri S, Abbasi N. Anti-inflammatory and analgesic effects of hydroalcoholic extract from the seed of Anethum graveolens L. J Med Plants. 2010;9:130–24.
Naseri M, Mojab F, Khodadoost M. The study of antiinflammatory activity of oil-based dill (Anethum graveolens L.) extract used topically in formalin-induced inflammation male rat paw. Iran J Pharm Res. 2012;11(4):1169–74.
Okuyama T, Matsuda M, Masuda Y, Baba M, Masubuchi H, Adachi M, et al. Studies on cancer bio-chemoprevention of natural resources. X. Inhibitory effect of spices on TPA-enhanced 3H-choline incorporation in phospholipid of C3H10T1/2 cells and on TPA-induced ear edema. Zhonghua Yaoxue Zazhi. 1995;47(5):421–30.
Fujishiro M, Kushiyama A, Yamazaki H, Kaneko S, Koketsu Y, Yamamotoya T, et al. Gastrointestinal symptom prevalence depends on disease duration and gastrointestinal region in type 2 diabetes mellitus. World J Gastroenterol. 2017;23(36):6694–704 PubMed PMID: 29085214. Pubmed Central PMCID: PMC5643290. Epub 2017/11/01.
Naseri MG, Heidari A. Antispasmodic effect of Anethum graveolens fruit extract on rat ileum. Int J Pharmacol. 2007;3:260–4.
Hosseinzadeh H, Karimi GR, Ameri M. Effects of Anethum graveolens L. seed extracts on experimental gastric irritation models in mice. BMC Pharmacol. 2002;2:21 PubMed PMID: 12493079.
Acknowledgements
The present study resulted from the M.Sc. thesis of MS Amoochi. The authors thank the Nutrition and Metabolic Diseases Research Center, Research Center for Diabetes and Endocrinology and Metabolism clinic employees of Golestan Hospital of Ahvaz Jundishapur University of Medical Sciences.
Funding
This study was financially supported by the Vice-Chancellor for Research Affairs of Ahvaz Jundishapur University of Medical Sciences (NRC-9617).
Author information
Authors and Affiliations
Contributions
GAF and FH conceived the idea and designed the study. GAF and MZ collected the data. FH and KAA analyzed and interpreted the results. GAF, FH and FB drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the ethics committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1396.623) in accordance with the Declaration of Helsinki. Each participant will sign an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haidari, F., Zakerkish, M., Borazjani, F. et al. The effects of Anethum graveolens (dill) powder supplementation on clinical and metabolic status in patients with type 2 diabetes. Trials 21, 483 (2020). https://doi.org/10.1186/s13063-020-04401-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-04401-3