Abstract
Background
Based on the molecular expression of cancer cells, molecular subtypes of breast cancer have been applied to classify patients for predicting clinical outcomes and prognosis. However, further evidence is needed regarding the influence of molecular subtypes on the efficacy of radiotherapy (RT) after breast-conserving surgery (BCS), particularly in a population-based context. Hence, the present study employed a propensity-score-matched cohort design to investigate the potential role of molecular subtypes in stratifying patient outcomes for post-BCS RT and to identify the specific clinical benefits that may emerge.
Methods
From 2006 to 2019, the present study included 59,502 breast cancer patients who underwent BCS from the Taiwan National Health Insurance Research Database. Propensity scores were utilized to match confounding variables between patients with and without RT within each subtype of breast cancer, namely luminal A, luminal B/HER2-negative, luminal B/HER2-positive, basal-like, and HER2-enriched ones. Several clinical outcomes were assessed, in terms of local recurrence (LR), regional recurrence (RR), distant metastasis (DM), disease-free survival (DFS), and overall survival (OS).
Results
After post-BCS RT, patients with luminal A and luminal B/HER2-positive breast cancers exhibited a decrease in LR (adjusted hazard ratio [aHR] = 0.18, p < 0.0001; and, 0.24, p = 0.0049, respectively). Furthermore, reduced RR and improved DFS were observed in patients with luminal A (aHR = 0.15, p = 0.0004; and 0.29, p < 0.0001), luminal B/HER2-negative (aHR = 0.06, p = 0.0093; and, 0.46, p = 0.028), and luminal B/HER2-positive (aHR = 0.14, p = 0.01; and, 0.38, p < 0.0001) breast cancers. Notably, OS benefits were found in patients with luminal A (aHR = 0.62, p = 0.002), luminal B/HER2-negative (aHR = 0.30, p < 0.0001), basal-like (aHR = 0.40, p < 0.0001), and HER2-enriched (aHR = 0.50, p = 0.03), but not luminal B/HER2-positive diseases. Remarkably, when considering DM, luminal A patients who received RT demonstrated a lower cumulative incidence of DM than those without RT (p = 0.02).
Conclusion
In patients with luminal A breast cancer who undergo BCS, RT could decrease the likelihood of tumor metastasis. After RT, the tumor’s hormone receptor status may predict tumor control regarding LR, RR, and DFS. Besides, the HER2 status of luminal breast cancer patients may serve as an additional predictor of OS after post-BCS RT. However, further prospective studies are required to validate these findings.
Similar content being viewed by others
Introduction
Breast-conserving therapy, comprising breast-conserving surgery (BCS) followed by radiotherapy (RT), is a standard approach in treating patients with early-stage breast cancer [1]. Post-BCS RT has been proven effective in preventing tumor recurrence by promoting cell apoptosis and inhibiting cell cycle progression [2,3,4]. Numerous studies have shown improved clinical outcomes in post-BCS RT patients [5,6,7]. However, the benefits of RT may vary among postoperative patients, possibly due to the biological heterogeneity of breast tumors [8].
The diverse nature of breast tumors at the molecular level leads to variations in the presentation of breast cancer. Through the use of immunohistochemistry (IHC) staining and fluorescence in situ hybridization (FISH) analyses, the main molecular subtypes of breast cancer were identified, as follows: luminal A (Hormone receptor-positive/Human Epidermal Growth factor Receptor-2 negative; HR+/HER2−), luminal B (HR+/HER2+and HR+/HER2−), basal-like (HR−/HER2−), and HER2-enriched (HR−/HER2 +) [9]. Different subtypes of breast cancer have been found to have varying prognoses depending on the treatments applied [8, 10, 11]. However, previous studies have presented contradictory and incomplete findings regarding the role of molecular subtypes in the outcomes of postoperative RT. For example, while one study showed a slight benefit of RT in luminal A breast cancer patients [12], another study did not find such benefits [13]. Furthermore, there is limited information on the benefits of post-BCS RT for patients with different molecular subtypes, particular from population-based evidence. It is important to note that previous studies have had limitations in their research methodology, as they failed to account for potential confounding factors such as the surgical approach [14, 15] and risk factors associated with specific breast cancer subtypes [16,17,18]. These factors have been shown to impact clinical outcomes [19, 20] and should be considered for future research.
In the present study, we employed the Taiwan National Health Insurance Research Database (TNHIRD) to examine the effects of different breast cancer subtypes on clinical outcomes in patients who underwent post-BCS RT. We conducted a propensity-score-matched cohort design to investigate this topic comprehensively. The main goal was to explore whether there were notable variations in the clinical benefits of post-BCS RT across various molecular subtypes of breast cancer.
Materials and methods
Database
The present study analyzed clinical information from the TNHIRD. This database is extensive and includes comprehensive clinical information for over 99% of the population in Taiwan. The database undergoes strict and regular evaluation by the National Health Insurance Administration (NHIA) [19].
Study population
The present study included female patients diagnosed with breast cancer from 2006 to 2019. The patients were selected based on the International Classification of Disease coding criteria, ninth revision, Clinical Modification (ICD-9-CM), with a breast cancer diagnosis (ICD-9-CM code 174.0–174.9). To ensure the accuracy of the data, we combined the breast cancer diagnostic code from ICD-9-CM with the registry code for patients with catastrophic illnesses. This approach allowed us to confirm that the selected data corresponded to actual records of breast cancer cases.
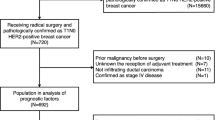
Inclusion criteria were as follows: adult patients aged 20–80 who underwent BCS, had clinical stages ranging from stage 0 to stage IV with a follow-up period of more than one year after breast cancer treatment. To compare the outcomes, eligible patients who underwent BCS were divided into two groups using propensity score matching: those who received RT and those who did not. Furthermore, we categorized the patients into five molecular breast cancer subtypes within each group, as shown in Fig. 1.
Table 1 shows the criteria of breast cancer subtypes, according to the St. Gallen International Expert Consensus [20], as follows: luminal A, luminal B/HER2 negative, luminal B/HER2-positive, basal-like, and HER2-enriched. Because information on Ki-67 was unavailable in the TNHIRD, the histological grade was used as an alternative measure of cell proliferation, as recommended in previous studies [21, 22].
Endpoints
Five clinical outcomes were measured as study endpoints, as follows: local recurrence (LR), regional recurrence (RR), distant metastasis (DM), disease-free survival (DFS), and overall survival (OS). These clinical outcomes were determined based on pathology information or CT/MRI images. The endpoint day was set as the day when the first event occurred. The follow-up time was calculated from the day of primary breast cancer diagnosis to either the day of most recent visit or the event of occurrence.
Statistical analysis
The RT patients were matched in a 1:1 ratio with non-RT patients based on several confounding factors, including age, molecular subtypes, clinical and pathological stage, comorbidities, chemotherapy, hormone therapy, target therapy, anti-cancer agents, and socioeconomic status. The patient characteristics and clinical information are summarized in Table 2. The RT and non-RT cohorts were compared within each molecular subtype. We utilized the Fine and Gray's competing-risk regression model to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the time-to-event clinical outcomes. All clinical outcomes were analyzed using multivariate analysis to adjust confounding factors. We used the SAS software to conduct the statistical analysis (version 9.2; SAS, Inc., Cary, NC). A two-sided test with a P-value of less than 0.05 was considered statistically significant.
Results
From 2006 to 2019, 59,502 breast cancer patients who underwent BCS were included. After applying the exclusion criteria (Fig. 1), 57,509 patients met the requirements for further analysis. Through a 1:1 matching, we obtained two cohorts of post-BCS patients: the RT (n = 6582) and non-RT ones (n = 6582; Table 2). Among the specific molecular subtype groups, the numbers of patients with and without RT were as follows: luminal A (n = 2646 and 2607), luminal B/HER2-negative (n = 373 and 396), luminal B/HER2-positive (n = 667 and 705), basal-like (n = 390 and 398), and HER2-enriched breast cancer (n = 382 and 394), respectively.
RT improved LR (aHR, 0.33; 95% CI 0.25–0.44; p < 0.0001), RR (aHR, 0.29; 95% CI 0.19–0.43; p < 0.0001), DM (aHR, 0.81; 95% CI 0.66–0.99; p < 0.05), DFS (aHR, 0.50; 95% CI 0.43–0.58; p < 0.0001), and OS (aHR, 0.51; 95% CI 0.45–0.58; p < 0.0001).
RT provided the most advantage in reducing rates of LR (66%) and RR (72%), surpassing a 50% reduction. Subsequently, it exhibited reduction rates of 48% in DFS and 46% in OS. Although the reduction rate of DM (19%) was the lowest, post-BCS patients still experienced statistically significant benefits from RT (aHR = 0.81, p < 0.05; Table 3).
Table 4 presents the variations in prognosis after RT among five molecular subtypes of breast cancer. After adjusting confounding factors, we observed RT improved LR in luminal A (aHR = 0.18, p < 0.0001) and luminal B/HER2-positive breast cancers (aHR = 0.24, p = 0.0049). Furthermore, RT improved RR and DFS in luminal A (aHR = 0.15, p = 0.0004 and 0.29, p < 0.0001), luminal B/HER2-negative (aHR = 0.06, p = 0.0093 and 0.46, p = 0.028), and luminal B/HER2-positive breast cancers (aHR = 0.14, p = 0.01 and 0.38, p < 0.0001), respectively.
The analysis also revealed OS benefits in both luminal and non-luminal breast cancers, including luminal A (aHR = 0.62, p = 0.002), luminal B/HER2-negative (aHR = 0.30, p < 0.0001), Basal-like (aHR = 0.40, p < 0.0001), and HER2-enriched (aHR = 0.50, p = 0.03), except for luminal B/HER2-positive breast cancers. Besides, a lower cumulative incidence of DM was observed only in the group of luminal A breast cancer patients with RT than those without RT (p = 0.02).
The luminal breast cancer (hormone receptor-positive; HR+) generally showed positive outcomes in terms of LR, RR, and DFS after post-BCS RT (aHR = 0.20, 0.17, and 0.35, respectively). However, non-luminal breast cancer (hormone receptor-negative; HR−) did not exhibit the same benefits (aHR = 0.78, 0.48, and 0.77, respectively; Fig. 2). We also observed that the HR+and HR− groups benefited from post-BCS RT regarding OS (aHR = 0.56 and 0.42). However, the risk of DM did not noticeably decrease after RT in either group (aHR = 0.73 and 0.99, respectively).
Furthermore, we observed RT patients a lower cumulative incidence of LR than non-RT patients in the luminal A (p < 0.0001), luminal B/HER2-negative (p = 0.02), and luminal B/HER2-positive breast cancer groups (p = 0.005; Fig. 3). Subsequently, a resulting increased DFS was observed, with higher rates in the luminal A (p < 0.0001), luminal B/HER2-negative (p = 0.01), and luminal B/HER2-positive breast cancer groups (p < 0.0001; Fig. 6). Regarding the cumulative incidence of RR (Fig. 4), patients benefited from RT were in the luminal A (p < 0.0001) and luminal B/HER2-positive breast cancer groups (p = 0.01). Considering OS (Fig. 7), patients benefited from RT were in the luminal A (p < 0.0001), luminal B/HER2-negative breast cancer (p < 0.0001), Basal-like (p = 0.0003), and HER2-enriched breast cancer groups (p = 0.02).
When compared with non-RT patients, a lower cumulative incidence of DM was only observed in RT patients in the luminal A breast cancer group (p = 0.02; Fig. 5). We further examined the incidences of DM between the RT and non-RT cohorts for each molecular subtype group among post-BCS patients (Table 5).
Discussion
The present study investigated how different molecular subtypes of breast cancer affect clinical outcomes after post-BCS RT. In general, post-BCS RT reduced the risks of LR, RR, and DM and prolonged DFS and OS rates in breast cancer patients. However, we discovered that not all molecular subtypes derived equal benefits from RT, and the advantages of RT were not consistent across all clinical outcomes. Our findings suggest that the intrinsic molecular subtypes of breast cancer can influence the clinical outcomes following RT in different ways, as follows. First, RT patients with luminal breast cancer experienced significant benefits, including lower risks of LR and RR and prolonged DFS. Conversely, patients with non-luminal breast cancer showed limited advantages in these clinical outcomes (Table 4 and Figs. 2, 3, 4, and 6). Second, whether the breast cancer was classified as luminal or non-luminal, post-BCS patients benefited from RT regarding extended OS. However, patients with HR+/HER2+breast cancer did not experience the same benefits (Table 4, Figs. 2 and 7). Third, regarding the observation of DM risk, RT was beneficial in reducing the probability of tumor metastasis after BCS only for patients with luminal A breast cancer (Table 4, Figs. 2 and 5).
In the era of precision medicine, the application of molecular classification of breast cancer is developing actively. The influence of diverse breast cancer subtypes on prognosis and treatment response is highly valued [23, 24]. When considering RT for postoperative breast cancer patients, clinical factors such as tumor stage, lymph node invasion, and surgical margin play a crucial role. However, advancements in molecular biotechnology have revealed the heterogeneity within breast tumors, leading to the recognition of the clinical significance of classifying breast cancer into intrinsic subtypes [25]. Our study suggested that molecular subtypes have a predictive role in determining the clinical benefits of post-BCS RT. This information can be valuable for clinicians in developing personalized cancer therapies.
Breast tumors vary in their response to treatment [26], and the effectiveness of RT in improving clinical outcomes may depend on the different gene expression patterns of these tumors [21]. When compared with hormone receptor-negative (HR−) tumors, our findings revealed that RT improved LR, RR, and DFS in hormone receptor-positive (HR+) tumors. This finding suggests that the hormone receptor status can be a predictive marker for tumor control following RT. [27]
Studies have shown that luminal breast cancer generally has more favorable outcomes after RT compared to non-luminal breast cancer [8, 21, 28, 29], and distinct biological processes have been identified that impact prognosis and treatment response in estrogen receptor-positive (ER-positive) and estrogen receptor-negative (ER-negative) breast cancers [30]. Furthermore, previous research has proposed different levels of sensitivity to radiation in individual breast cancer subtypes, suggesting that the differences in prognosis between luminal and non-luminal breast cancers may be attributed to significantly enhanced radiosensitivity in luminal breast cancer. In contrast, HER2-enriched [8] and basal-like breast cancers exhibit strong resistance to radiation [31]. The estrogen receptor has been found to interact with the androgen receptor, further enhancing the radiosensitivity of breast tumors [32]. Inhibiting estrogen receptor signaling has also been shown to increase the sensitivity of ER-positive tumors to radiation [33]. Additionally, clinical studies have pointed out the association between poor prognosis and radioresistance in HER2-overexpressing and triple-negative breast tumors [27, 34].
Emerging evidence has shed light on potential mechanisms contributing to the robust radioresistance observed in HER2-enriched breast cancer. These mechanisms include the HER2-NF-kappaB-HER2 loop, which mediates radiation-induced adaptive resistance [34], as well as the Fak-mediated pathway, which enhances radiosensitization in HER2-overexpressing breast cancer [35, 36]. Furthermore, the involvement of microRNA (miRNA) in the regulatory mechanism of triple-negative breast tumors has been discovered. For instance, high expression of MiR27a has been found to play a crucial role in regulating the radiosensitivity of triple-negative breast cancer cells [37, 38].
Notably, while significant tumor control was observed in HR+cancer patients after RT, our analysis revealed that an improved OS was found only in HR+/HER2-, not HR+/HER2+tumors. This finding suggests that HER2 status may further predict the benefits of OS after RT in patients with luminal breast cancer. Even in patients who underwent postmastectomy radiotherapy (PMRT), as studied previously [27], OS benefits from RT were observed solely among those with hormone receptor-positive and HER2-negative breast cancers (including two HR+subtypes) [27]. The resistance of HER2-overexpressing tumors to radiation may affect the OS benefits, even in cases with good prognostic markers for luminal breast cancer (HR +). Moreover, the extent of radioresistance may vary among different cell types of HER2-positive tumors, as previous studies have proposed the existence of inherent radiosensitivity differences in HER2-overexpressing tumor cells, which should be considered in conventional RT approaches [39].
Remarkably, a lower cumulative incidence rate of DM was observed after RT in patients with luminal A breast cancer. This finding is consistent with previous studies [29, 40]. Furthermore, HER2-overexpression has been linked to radioresistance and epithelial-to-mesenchymal transition in breast cancer stem cells [41, 42], which are crucial for tumor invasion, migration, and metastatic outgrowth [43]. Taken together, these characteristics of different breast tumor subtypes may contribute to a high likelihood of metastasis even after RT, but there is still a slightly favorable outcome observed after RT in luminal A (HR+/HER2-) breast tumors.
The present study discovered a significant increase in OS rates among RT patients. This finding indicates that the benefits of OS from post-BCS RT extend beyond just the luminal subtypes and apply to basal-like and HER2-enriched breast cancers. The lack of tumor control in basal-like and HER2-enriched breast cancers did not diminish the OS benefits of post-BCS RT, suggesting that RT has a robust effect on prolonging survival in post-BCS patients [5, 44, 45]. It is a proven fact that post-BCS RT has noticeable positive effects on breast cancer patients, with both breast-cancer-specific survival and OS significantly improved even in elderly patients (age ≥ 70 years) [44]. Furthermore, the benefits of RT on OS were not dependent on irradiation volume, as similar benefits were observed in patients who underwent accelerated partial breast irradiation and those who received whole breast RT [46]. Despite the favorable outcomes associated with post-BCS RT, there remains uncertainty regarding the relationship between molecular subtypes of breast cancer and the benefits of OS from RT due to conflicting previous research [8, 28, 47]. While one study demonstrated a significantly lower 3-year OS rate among patients with the HER2-enriched subtype than those with the luminal subtype [28], another 5-year follow-up study found no differences among molecular subtypes [47].
It should be noted that the influences on the benefits of OS from RT can be multifactorial, including factors such as surgical approach, [14, 15, 48] tumor stage, [49, 50] anti-cancer drug, [51, 52] and age [53], all of which need to be considered when evaluating the impact of molecular subtypes of breast cancer on the clinical benefits of radiotherapy. Therefore, further clinical studies are required to develop a factorial model that incorporates the benefits of overall survival from radiotherapy in molecular subtypes of breast cancer. The present study utilized propensity-score-based matching to control for confounding variables between patients with and without RT, revealing distinct survival benefits from RT in post-BCS patients. Although non-luminal subtypes are recognized as prognostic indicators of breast cancer associated with shorter overall survival [11, 21, 54], the benefits of OS from post-BCS RT should not be disregarded for these subtypes.
The present study has several limitations. Firstly, although the study employed a propensity-score-matched design, it cannot definitively establish a cause-and-effect relationship between breast cancer subtypes and post-RT outcomes due to its retrospective study nature. Secondly, some studies have separately explored the clinical outcomes of RT in pre- [55] and post-menopausal [56] breast cancer patients. However, the correlation between the benefits of RT and menopause status appears to be minimal, as similar clinical outcomes were observed in both groups of patients [57]. Additionally, other factors were not assessed in our study, such as the family history of malignant tumors, lymphovascular invasion [58], physical activity [59, 60], and circulating tumor cell status [61]. These factors could potentially influence the clinical outcomes after RT, despite our efforts to adjust and control for confounding variables.
Remarkably, we should discuss that the present study included BCS patients without RT, which is not the standard care of the current guideline. Among the 57,509 qualified post-BCS patients, we deleted 4648 patients who had no clear tumor stages. In the remaining 52,861 patients, 44,847 RT patients and 8014 non-RT patients were matched with a 1:1 ratio. Therefore, the number of post-BCS patients without RT was accounted for 15.1% of the total number. In the real-world setting, several reasons may result in patients and their families choosing diversely from the standard of care, such as the fear of RT side effects, elderly, economic status, significant comorbidities (e.g., stroke, severe dementia, end-stage renal disease, or heart failure), or other personal factors. Presenting the actual status in a real-world setting is one of the central values of the population-based study. Thus, we co-present the RT and non-RT patients (but match-paired them) instead of excluding the non-RT patients from the present analysis.
Conclusion
The response of tumors to RT in luminal breast cancer can be predicted by the hormone receptor status, in terms of LR, RR, and DSF. Additionally, HER2 status may serve as an additional predictor for OS following post-BCS RT. The impact of RT in reducing the likelihood of tumor spread after BCS is potentially significant for patients with luminal A breast cancer. However, the lack of tumor control in basal-like and HER2-enriched breast cancers does not affect the OS benefits derived from post-BCS RT.
Availability of data and materials
Data used in this study are from TNHIRD, and this database is owned by the government. The information contained within the database was authorized for research purposes by the Health and Welfare Data Science Center (HWDC), Ministry of Health and Welfare, Taiwan. The raw data from the TNHIRD is available to the research community; however, the data must be analyzed within the HWDC after the study proposal is approved (https://dep.mohw.gov.tw/dos/np-2497-113.html). The raw data can only be dealt with in this data science center, and cannot be released according to the legal restriction of Data Science Center, Ministry of Health and Welfare, Taiwan. The website of Data Science Center, Ministry of Health and Welfare, Taiwan is as follows: https://dep.mohw.gov.tw/dos/cp-5283-63826-113.html. The confidentiality assurances were addressed by the data regulations of the HWDC. The study protocol, analytic methods, and statistical programming codes are available from the corresponding author on reasonable request.
References
Network NCC. NCCN clinical practice guidelines in oncology. Breast Cancer Version 4. 2022.
Abdulkarim B, Deutsch E. Endothelial-cell apoptosis and tumor response to radiotherapy. Lancet Oncol. 2004;5(1):9.
Roa W, Zhang X, Guo L, et al. Gold nanoparticles sensitize radiotherapy of prostate cancer cells by regulation of the cell cycle. Nanotechnology. 2009;20(37): 375101.
Li MY, Liu JQ, Chen DP, et al. Radiotherapy induces cell cycle arrest and cell apoptosis in nasopharyngeal carcinoma via the ATM and Smad pathways. Cancer Biol Ther. 2017;18(9):681–93.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Fisher B, Anderson S, Redmond CK, et al. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995;333(22):1456–61.
Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: a meta-analysis of individual patient data for 10,801 women in 17 randomized trials. Lancet (London, England). 2011;378(9804):1707–16.
He L, Lv Y, Song Y, et al. The prognosis comparison of different molecular subtypes of breast tumors after radiotherapy and the intrinsic reasons for their distinct radiosensitivity. Cancer Manag Res. 2019;11:5765–75.
Society AC. Breast cancer facts & figures 2022–2024. 2022.
Perou CM, Sørlie T, Eisen MB, et al. Molecular portraits of human breast tumors. Nature. 2000;406(6797):747–52.
Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci. 2001;98(19):10869–74.
Liu FF, Shi W, Done SJ, et al. Identification of a low-risk luminal a breast cancer cohort that may not benefit from breast radiotherapy. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(18):2035–40.
Wang J, Luo J, Jin K, et al. Biological subtype predicts locoregional recurrence after postmastectomy radiotherapy in Chinese breast cancer patients. Cancer Med. 2020;9(7):2427–34.
de Boniface J, Szulkin R, Johansson ALV. Survival after breast conservation vs mastectomy adjusted for comorbidity and socioeconomic status: a swedish national 6-year follow-up of 48 986 women. JAMA Surg. 2021;156(7):628–37.
Chu QD, Hsieh MC, Lyons JM, et al. 10-year survival after breast-conserving surgery compared with mastectomy in louisiana women with early-stage breast cancer: a population-based study. J Am Coll Surg. 2021;232(4):607–21.
Yang XR, Chang-Claude J, Goode EL, et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst. 2011;103(3):250–63.
Barnard ME, Boeke CE, Tamimi RM. Established breast cancer risk factors and risk of intrinsic tumor subtypes. Biochem Biophys Acta. 2015;1856(1):73–85.
Nattenmüller CJ, Kriegsmann M, Sookthai D, et al. Obesity as a risk factor for subtypes of breast cancer: results from a prospective cohort study. BMC Cancer. 2018;18(1):616.
Cheng TM. Taiwan’s new national health insurance program: genesis and experience so far. Health Aff (Project Hope). 2003;22(3):61–76.
Goldhirsch A, Wood WC, Coates AS, et al. Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol Off J Eur Soc Med Oncol. 2011;22(8):1736–47.
Johnson KS, Conant EF, Soo MS. Molecular subtypes of breast cancer: a review for breast radiologists. J Breast Imaging. 2020;3(1):12–24.
von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(15):1796–804.
Iwamoto T, Kajiwara Y, Zhu Y, et al. Biomarkers of neoadjuvant/adjuvant chemotherapy for breast cancer. Chin Clin Oncol. 2020;9(3):27.
Rouzier R, Perou CM, Symmans WF, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res Off J Am Assoc Cancer Res. 2005;11(16):5678–85.
Allott EH, Cohen SM, Geradts J, et al. Performance of three-biomarker immunohistochemistry for intrinsic breast cancer subtyping in the AMBER consortium. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2016;25(3):470–8.
Tavassoli FAS, Stuart J. Pathology of the breast. New York: Elsevier; 1992.
Kyndi M, Sørensen FB, Knudsen H, et al. Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(9):1419–26.
Wadasadawala T, Mondal M, Paul SN, et al. Should molecular subtype be recommended as one of the selection criteria for accelerated partial breast irradiation? Preliminary results from an Asian cohort. J Contemp Brachytherapy. 2018;10(1):47–57.
Nguyen PL, Taghian AG, Katz MS, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(14):2373–8.
Iwamoto T, Bianchini G, Booser D, et al. Gene pathways associated with prognosis and chemotherapy sensitivity in molecular subtypes of breast cancer. J Natl Cancer Inst. 2011;103(3):264–72.
He MY, Rancoule C, Rehailia-Blanchard A, et al. Radiotherapy in triple-negative breast cancer: current situation and upcoming strategies. Crit Rev Oncol Hematol. 2018;131:96–101.
Michmerhuizen AR, Lerner LM, Ward C, et al. Androgen and estrogen receptor co-expression determines the efficacy of hormone receptor-mediated radiosensitization in breast cancer. Br J Cancer. 2022;127(5):927–36.
Michmerhuizen AR, Lerner LM, Pesch AM, et al. Estrogen receptor inhibition mediates radiosensitization of ER-positive breast cancer models. NPJ Breast Cancer. 2022;8(1):31.
Cao N, Li S, Wang Z, et al. NF-kappaB-mediated HER2 overexpression in radiation-adaptive resistance. Radiat Res. 2009;171(1):9–21.
Wilson C, Nicholes K, Bustos D, et al. Overcoming EMT-associated resistance to anti-cancer drugs via Src/FAK pathway inhibition. Oncotarget. 2014;5(17):7328–41.
Hou J, Zhou Z, Chen X, et al. HER2 reduces breast cancer radiosensitivity by activating focal adhesion kinase in vitro and in vivo. Oncotarget. 2016;7(29):45186–98.
Ren YQ, Fu F, Han J. MiR-27a modulates radiosensitivity of triple-negative breast cancer (TNBC) cells by targeting CDC27. Med Sci Monit Int Med J Exp Clin Res. 2015;21:1297–303.
Yang F, Zhang W, Shen Y, et al. Identification of dysregulated microRNAs in triple-negative breast cancer (review). Int J Oncol. 2015;46(3):927–32.
Steffen AC, Göstring L, Tolmachev V, et al. Differences in radiosensitivity between three HER2 overexpressing cell lines. Eur J Nucl Med Mol Imaging. 2008;35(6):1179–91.
Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–502.
Giordano A, Gao H, Anfossi S, et al. Epithelial-mesenchymal transition and stem cell markers in patients with HER2-positive metastatic breast cancer. Mol Cancer Ther. 2012;11(11):2526–34.
Arias-Romero LE, Villamar-Cruz O, Huang M, et al. Pak1 kinase links ErbB2 to β-catenin in the transformation of breast epithelial cells. Can Res. 2013;73(12):3671–82.
Yeung KT, Yang J. Epithelial-mesenchymal transition in tumor metastasis. Mol Oncol. 2017;11(1):28–39.
Yang SP, Tan LL, Zhou P, et al. The addition of radiotherapy to breast-conserving surgery improves survival for elderly patients with early breast cancer. Front Oncol. 2022;12: 917054.
Shigematsu N, Takeda A, Sanuki N, et al. Radiation therapy after breast-conserving surgery. Radiat Med. 2006;24(5):388–404.
Hickey BE, Lehman M. Partial breast irradiation versus whole breast radiotherapy for early breast cancer. Cochrane Database Syst Rev. 2021;8(8):CD007077.
Wilkinson JB, Shah C, Amin M, et al. Outcomes according to breast cancer subtype in patients treated with accelerated partial breast irradiation. Clin Breast Cancer. 2017;17(1):55–60.
Lan XW, Wen G, He Z, et al. Comparison of long-term results between radiotherapy after breast-conserving surgery and postmastectomy radiotherapy in stage T1–2N1M0 breast cancer. Cancer Manag Res. 2019;11:6477–87.
Xiang W, Wu C, Wu H, et al. Survival comparisons between breast conservation surgery and mastectomy followed by postoperative radiotherapy in stage I–III breast cancer patients: analysis of the surveillance, epidemiology, and end results (Seer) Program database. Curr Oncol (Toronto, Ont). 2022;29(8):5731–47.
Kim YJ, Kim SS, Ahn SD, et al. The role of postoperative radiotherapy after primary tumor resection in patients with de novo stage IV breast cancer. Asia Pac J Clin Oncol. 2021;17(6):495–505.
Lv S, Wang Y, Sun T, et al. Overall Survival benefit from trastuzumab-based treatment in HER2-positive metastatic breast cancer: a retrospective analysis. Oncol Res Treat. 2018;41(7–8):450–5.
Kerr AJ, Dodwell D, McGale P, et al. Adjuvant and neoadjuvant breast cancer treatments: a systematic review of their effects on mortality. Cancer Treat Rev. 2022;105: 102375.
Punglia RS, Kuntz KM, Lee JH, et al. Radiation therapy plus tamoxifen versus tamoxifen alone after breast-conserving surgery in postmenopausal women with stage I breast cancer: a decision analysis. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21(12):2260–7.
Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci. 2003;100(14):8418–23.
Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337(14):956–62.
Overgaard M, Jensen MB, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomized trial. Lancet (London, England). 1999;353(9165):1641–8.
Mok TS, Kwan WH, Yeo WM, et al. Clinical outcomes of postoperative locoregional radiotherapy in pre-menopausal and post-menopausal Chinese women with breast cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2000;54(3):201–8.
Li C, Wang J, Mo M, et al. Outcomes in patients with pT3N0M0 breast cancer with and without postmastectomy radiotherapy. Cancer Manag Res. 2021;13:3889–99.
Collado Chazarra P, Santiñá VM. Influence of physical activity on radiotherapy-treated breast cancer patients: a systematic review. J Healthc Qual Res. 2022. https://doi.org/10.1016/j.jhqr.2022.05.008.
Cannioto RA, Hutson A, Dighe S, et al. Physical activity before, during, and after chemotherapy for high-risk breast cancer: relationships with survival. J Natl Cancer Inst. 2021;113(1):54–63.
Goodman CR, Seagle BL, Friedl TWP, et al. Association of circulating tumor cell status with benefit of radiotherapy and survival in early-stage breast cancer. JAMA Oncol. 2018;4(8): e180163.
Funding
The present study is supported by a research grant from the Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (DTCRD107-I-08, TCMF-A 111-10, TCMF-A 112-04). The funder is not involved in the study design, analysis, and publication decision.
Author information
Authors and Affiliations
Contributions
HYL, SKH, WYC and HJY conceived and designed the study, with input from the other authors. MSL, WYC, DWL, LCC, CHC, CHL, SCL, CLH, CHL, and CCY supervised the project. HYL and HJY wrote the first draft of the manuscript. BHY, HJY, and FCH performed the statistical analyses and prepared all figures and tables. All authors interpreted the data and contributed to the writing of the paper. All authors reviewed and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Before conducting the analysis, the study protocol received approval from the Institute Review Board (IRB) of the Dalin Tzu-Chi Hospital, Buddhist Tzu Chi Medical Foundation (Number: B10604007). Due to the nature of the data being de-identified, the IRB waived the requirement for obtaining informed consent from the included patients.
Competing interests
All authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hung, SK., Yang, HJ., Lee, MS. et al. Molecular subtypes of breast cancer predicting clinical benefits of radiotherapy after breast-conserving surgery: a propensity-score-matched cohort study. Breast Cancer Res 25, 149 (2023). https://doi.org/10.1186/s13058-023-01747-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-023-01747-9