Abstract
Background
Latin American and Hispanic women are less likely to develop breast cancer (BC) than women of European descent. Observational studies have found an inverse relationship between the individual proportion of Native American ancestry and BC risk. Here, we use ancestry-informative markers to rule out potential confounding of this relationship, estimating the confounder-free effect of Native American ancestry on BC risk.
Methods and study population
We used the informativeness for assignment measure to select robust instrumental variables for the individual proportion of Native American ancestry. We then conducted separate Mendelian randomization (MR) analyses based on 1401 Colombian women, most of them from the central Andean regions of Cundinamarca and Huila, and 1366 Mexican women from Mexico City, Monterrey and Veracruz, supplemented by sensitivity and stratified analyses.
Results
The proportion of Colombian Native American ancestry showed a putatively causal protective effect on BC risk (inverse variance-weighted odds ratio [OR] = 0.974 per 1% increase in ancestry proportion, 95% confidence interval [CI] 0.970–0.978, p = 3.1 × 10–40). The corresponding OR for Mexican Native American ancestry was 0.988 (95% CI 0.987–0.990, p = 1.4 × 10–44). Stratified analyses revealed a stronger association between Native American ancestry and familial BC (Colombian women: OR = 0.958, 95% CI 0.952–0.964; Mexican women: OR = 0.973, 95% CI 0.969–0.978), and stronger protective effects on oestrogen receptor (ER)-positive BC than on ER-negative and triple-negative BC.
Conclusions
The present results point to an unconfounded protective effect of Native American ancestry on BC risk in both Colombian and Mexican women which appears to be stronger for familial and ER-positive BC. These findings provide a rationale for personalised prevention programmes that take genetic ancestry into account, as well as for future admixture mapping studies.
Similar content being viewed by others
Introduction
Breast cancer (BC) is a major public health concern, as it is the most commonly diagnosed cancer among women worldwide and the leading cause of cancer death [1]. BC is a complex trait with multiple established genetic and non-genetic, risk and protective factors influencing disease development.
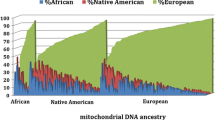
Latin American women and Latinas are ethnically diverse [2,3,4,5,6,7,8]. Their genomes are made up of chromosomal segments of Native American, European and African origin admixed in different proportions within and between countries of South America, the Caribbean, and Mexico, depending on the original peoples and the specific local history of European settlement and the slave trade [9,10,11,12,13,14,15,16]. In Mexico, individual Native American proportions are generally highest in the center and south of the country, European percentages are highest in the north, and the African contribution to the Mexican genome is generally limited, with the exception of some coastal regions. In Colombia, Native American proportions are particularly high in the east and southwest of the country, central areas show generally high percentages of European ancestry, and proportions of African ancestry increase in coastal regions, especially along the Pacific [17].
Differences in the risk of various diseases, including different types of cancer, according to the individual proportion of Native American, European and African genetic ancestry have recently moved into focus [18, 19]. For example, prostate cancer is more common in black men than in white men, and genome-wide association studies have identified variants at 8q24 that account for a large proportion of the excess risk of prostate cancer in black men [20]. The relative proportion of European versus Native American ancestry has been associated with BC risk in US Latinas and in Mexican and Colombian women. Women with a high proportion of Native American ancestry have a lower risk of BC than those with a high proportion of European ancestry [21,22,23,24,25]. The reported protective effects of Native American ancestry take into account statistically established risk factors such as oral contraceptive use, parity, age at first full-term pregnancy, age at menarche and breastfeeding, but at least part of the association could be attributed to as yet unknown confounding factors, which may be specific to Latin American and Hispanic women, and to measurement errors in the adjustment variables (e.g., accurate information on socio-economic status is difficult to obtain). The origin of the negative association between Native American ancestry and BC risk—are confounding factors, e.g. higher parity or lower income of women with a high percentage of Native American ancestry, responsible for this association?—has important implications for BC prevention and research.
Genetic variants (e.g. single-nucleotide polymorphisms [SNPs]) can be used as instrumental variables (IVs) to assess the confounding-free effect of an exposure of interest (in this study, the individual proportion of Native American ancestry) on a given outcome (in the present study, BC development) [26]. The alleles of the SNPs used as instruments for the proportion of Native American ancestry are randomly allocated during meiosis, mimicking a trial randomized by nature and resulting in effect estimates that are less influenced by potential confounders than those from observational studies [27]. Instrumental variable analyses on the relationship between the individual proportion of Native American ancestry and BC risk would facilitate the distinction between correlation and confounder-free association, allowing prioritisation of unconfounded associations for more efficient prevention and providing the basis for further analysis to better understand the non-genetic and genetic mechanisms leading to BC development.
With these objectives in mind, we preselected ancestry-informative markers (AIMs) in reference panels of Native American, European and African ancestry using the informativeness for assignment measure [28]. We then selected valid IVs in Colombian and Mexican women separately that were robustly associated with the proportion of Native American ancestry (relevance assumption), not associated with potential confounders (independence assumption) and not directly associated with outcome (exclusion restriction assumption). Next, we performed two-sample Mendelian randomization (MR) analyses, which we complemented with sensitivity analyses and analyses stratified by age at diagnosis, family history and BC hormone receptor status. Population stratification, usually a limitation in genetic association studies, was our exposure of interest, with an atypically high proportion of variance explained by the IVs used (between 7 and 39%).
Results
Figure 1 depicts the usual directed acyclic graph of MR adapted to the present study. Increasing individual proportions of Native American ancestry have been linked to decreasing BC risk, but this association may be attributed to some degree to unknown confounders and non-random measurement error in known confounders (e.g. socio-economic status), motivating the use of AIMs as instrumental variables to assess the unconfounded effect of the proportion of Native American ancestry on BC risk.
Figure 2 represents the analyses conducted from AIM pre-selection to the two-sample MR analyses. The left part of the flowchart shows some intermediate results based on Colombian women, while the right part refers to the analyses in Mexican women. The ancestry reference panels in the primary analyses included 107 Iberians from Spain (IBS) and 108 Yorubans from Ibadan, Nigeria (YRI) from the 1000 Genomes Project, complemented with 29 Native Americans from Colombia (nine Inga, five Arhuaco, four Embera, three Kogi and three Waunana described by Reich et al. and five Piapoco individuals from the Human Genome Diversity Project [HGDP]) or 177 Native Americans from Mexico (49 Maya, 43 Zapotec, 30 Pima, 25 Tepehuano, 17 Mixe, five Mixtec, one Yaqui and one Purepecha described by Reich et al. and four Maya and one Pima from the HGDP) [29, 30]. Relying on the informativeness for assignment measure, we preselected 36,403 AIMs for Colombian women and 32,835 AIMs for Mexican women. Among the preselected markers, 623 were robustly associated (p < 5 × 10–8) with the proportion of Native American ancestry among Colombian female controls; the corresponding number in Mexican female controls was 6118. Downstream phenome-wide association analyses (PheWAS, using a p-value threshold of 5 × 10–8) and linkage disequilibrium (LD) pruning (r2 > 0.01) resulted in 121 preliminary IVs for the subsequent Colombian analyses and 150 IVs for the subsequent Mexican analyses. We then complemented age-adjusted summary statistics on the association between the IVs and the proportion of Native American ancestry with age-adjusted summary statistics on the association between the IVs and BC risk based on BC patients and controls to perform radial MR and exclude potentially outlying instruments (p < 0.1). Finally, 98 and 134 IVs were utilised to investigate the confounder-free effect of the proportions of Colombian and Mexican Native American ancestry on BC risk.
Figure 3 represents the first versus the second, and the first versus the third genetic principal components, along with the reference panels of Native American, European and African ancestry. The first three principal components explained a genetic variance of 4.07%, 1.34% and 0.18% in Colombian women and 5.89%, 2.00% and 0.26% for Mexican women, respectively. The first principal component distinguished between African and non-African ancestry in both admixed Colombian women (panel A) and admixed Mexican women (panel B). The second principal component distinguished between European and Native American ancestry. The third principal component separated three subtypes of Native American ancestry in Mexican women: the group of Native American reference individuals most similar to the study population (M1) included 115 individuals (49 Maya, 43 Zapotec, 17 Mixe, five Mixtec and one Purepecha).
Scatter plots of first versus second, and first versus third genetic principal components (PC) of study participants (crosses: BC patients, circles: population-based controls) and reference panels of African, European and Native American ancestry (represented by triangles; M1 includes Maya, Mixe, Mixtec, Purepecha and Zapotec, M2 includes Tepehuano and Yaqui, and M3 includes Pima individuals); panel A: Colombian study, panel B: Mexican study
Table 1 shows the results for Colombian women, while the corresponding results based on Mexican women are summarised in Table 2. The 98 IVs utilised for two-sample MR in Colombian women explained a cumulative variance of 7.1% in the proportion of Native American ancestry (F-statistic = 55.57). The p-value of Cochran’s Q statistic (p > 0.99) revealed no instrument heterogeneity as an indicator of pleiotropy, the MR-Egger intercept (p = 0.60) was consistent with no horizontal pleiotropy, and departing instruments were not evident in scatter and funnel plots (Fig. 4, panels A and B), prompting the use of inverse variance-weighted (IVW) odds ratios (ORs) for the primary analyses. The cumulative variance explained by the 134 IVs used for the Mexican analyses amounted to 38.5% (F-statistic = 412.29), which is an atypically high proportion in Mendelian randomization studies. After inspection of the p-value of Cochran’s Q statistic (p > 0.99), the MR-Egger intercept (p = 0.66) and the scatter and funnel plots (Fig. 4, panels C and D), we also decided to use the IVW OR for the primary Mendelian randomization analyses in Mexican women.
We found evidence of a putatively causal protective effect of Colombian Native American ancestry on BC risk (IVW OR = 0.974 per 1% increase in ancestry proportion, 95% confidence interval [CI] 0.970–0.978, p = 3.1 × 10–40). This estimate can also be interpreted as a 2.6% decrease in BC risk (95% CI 2.2–3%) per each 1% increase in the proportion of Native American ancestry (median 42% and interquartile range 36%-49% in Colombian female controls). MR results based on Mexican women also pointed to a protective effect of Native American ancestry on BC risk (IVW OR 0.988, 95% CI 0.987–0.990, p = 1.4 × 10–44). The median and interquartile range of the proportion of Native American ancestry were 65% and 54%-79% in Mexican control women, respectively.
Table 1 also shows the results of sensitivity analyses for Colombian women. The MR-Egger regression estimate (OR = 0.983, 95% CI 0.950–1.017) was consistent (overlapping 95% CI), and the weighted median estimate (OR = 0.975, 95% CI 0.969–0.980, p = 0.33) was virtually identical to the IVW OR (see also the regression lines on Fig. 4, panel A). To assess the influence on the results of the reference panel of Native American ancestry, we replaced the original 29 Native Americans from Colombia with 57 unrelated Native Americans from the HGDP (21 Maya, 13 Pima, 11 Karitiana, seven Piapoco and five Surui, see Additional file 1: Fig. 1) [31]. The use of Native Americans from the HGDP for calculation of ancestry proportions reduced the explained variance (from 7.1%-6.6%) and increased the p-value (to p = 6.1 × 10–37), but resulted in practically identical IVW OR estimates.
Stratified analyses in Colombian women suggested stronger protective effects of the proportion of Native American ancestry among women with a family history of BC and/or ovarian cancer (4.2% decrease in BC risk per 1% increase in proportion of Native American ancestry, 95% CI 3.6%-4.8%, p = 2.0 × 10–41), and on ER-positive BC (IVW OR = 0.968) versus ER-negative BC (IVW OR = 0.988) or triple-negative BC (IVW OR = 0.993; non-overlapping 95% CIs with ER-positive BC).
The results of the sensitivity analyses based on the Mexican women are shown in Table 2. As in the Colombian analyses, the IVW, MR-Egger and weighted median estimates were consistent (overlapping 95% CIs and very similar regression lines on Fig. 4, panel C). To examine the impact of the large variance explained by the IVs on the results, we reduced the number of IVs to 17, resulting in a similar explained variance as in the Colombian analyses (8.4%), but the IVW estimates barely changed (from OR = 0.988 to OR = 0.990). Neither the use of Native Americans from the HGDP nor the use of a subset of 115 Native Americans from Mexico (49 Maya, 43 Zapotec, 17 Mixe, five Mixtec and one Purepecha) as the reference panels for estimation of Native American ancestry proportions affected the IVW OR estimates.
Stratified analyses in Mexican women confirmed the stronger protective effect of Native American ancestry against familial BC found in Colombian women (2.7% decrease in familial BC risk compared with 1.2% decrease in overall BC risk per 1% increase in the proportion of Native American ancestry). Also in agreement with the Colombian results, the protective effect was stronger against ER-positive BC (IVW OR = 0.989) than against ER-negative BC (IVW OR = 1.004) or triple-negative BC (IVW OR = 1.004; non-overlapping 95% CIs and associated p < 2.2 × 10–16 with ER-positive BC).
Interestingly, most IVs (Colombian: 96%, Mexican: 97%) used as instrumental variables were population-specific, but differences between causal effect estimates based on common and population-specific markers did not reach statistical significance (overlapping 95% confidence intervals). For example, the IVW OR based on the four joint Colombian and Mexican IVs was 0.969 (95% CI 0.949–0.988) compared to 0.974 (95% CI 0.970–0.978) based on the 94 Colombia-specific IVs.
Discussion
An inverse relationship between the individual proportion of Native American ancestry and BC risk has been previously reported in observational studies, but the role of confounding factors in this association remains unclear, and the standard approach of statistical adjustment is limited by (1) potentially large, non-random measurement errors in the adjustment variables (e.g. income and access to BC screening) and (2) the impossibility of taking into account as yet unknown risk factors. Using specific AIMs for Colombian and Mexican women as instrumental variables, we assessed the unconfounded effect of Native American ancestry on BC risk and found a confounder-free protective effect in both populations: each 1% increase in the proportion of Native American ancestry represented a 2.6% reduction in BC risk for Colombian women and a 1.2% risk reduction for Mexican women. Given the large variability in ancestry proportions in the populations investigated, these results are clinically relevant: they translate into expected differences in BC risk of (49–36) × 2.6 = 33.8% between Colombian women in the first and third ancestry quartiles—the corresponding BC risk difference for Mexican women was (79–54) × 1.2 = 30%. Extensive sensitivity analyses considering alternative reference panels of Native American ancestry, and different MR methods confirmed the protective association and its magnitude. Stratified analyses revealed stronger effects for familial BC, adding plausibility to our findings.
The OR estimated in this study for Colombian women (0.974 per 1% increase in Native American ancestry proportion, 95% CI 0.970–0.978) was similar to the OR adjusted for age, family history of BC, oral contraceptive use, menopausal status combined with postmenopausal hormone therapy use, body mass index, smoking status, parity, age at first full-term pregnancy and breastfeeding (OR = 0.976, 95% CI 0.969–0.983) previously reported in an observational study [23]. The study population investigated in the present study (714 BC patients and 687 matched female controls) largely overlapped with the population examined in the earlier observational study (722 BC patients and 622 matched female controls), which relied on targeted genotyping of 30 AIMs for ancestry estimation. As shown in Fig. 3, increasing proportions of Native American ancestry generally correspond to decreasing proportions of European ancestry in Latin American women, and European ancestry has previously been associated with increased BC risk among Mexicans and US Hispanics [21, 22]. Stratified analyses revealed a stronger protective effect of Native American ancestry against familial BC and ER-positive BC for both Colombian and Mexican women, which has important implications for BC prevention: As the negative association between Native American ancestry and BC risk previously found in observational studies appears to be free of confounding factors, taking into account the individual proportion of Native American ancestry could improve the effectiveness of current prevention strategies by, for example, defining the optimal ancestry-specific age for starting BC screening [32].
Based on 2107 BC cases and 2587 unaffected controls of Hispanic/Native American origin living in the United States and Mexico, Fejerman et al. examined the interaction between hormonal and lifestyle risk factors, and 10 BC susceptibility variants [33]. The authors found a correlation between Native American ancestry, hormone replacement use, and breastfeeding behaviour. They concluded that genetic ancestry in admixed populations may reflect not only population-specific differences in genetic susceptibility, but also differences in environmental exposures that, together with genetic factors, may influence BC risk. Hynes et al. also examined the interaction between established risk factors and genetic ancestry on BC risk among women from the USA and Mexico in the Breast Cancer Health Disparities Study [24]. They found that the inverse relationship between Native American ancestry and BC risk was only slightly attenuated when adjusted for known risk factors and concluded that established BC risk factors may be less relevant for women with a high proportion of Native American ancestry. Consistent with our findings, previous studies on the association between genetic ancestry and BC risk in Latin American populations have found differences in BC subtypes by ancestry. Rey-Vargas et al. reported a higher proportion of Native American ancestry in Colombian patients with ER+ /HER2+ (45%) than in ER + /HER2− (40%) breast tumours, and Marker et al. demonstrated a higher risk of HER2 + BC with increasing proportions of Native American ancestry in Colombian, Mexican and Peruvian women [34, 35]. The novelty of the present study lay in the use of instrumental variable analysis to identify and quantify the confounding-free effect of Native American ancestry on the risk of overall BC and BC subtypes.
The relatively low number of women investigated in the separate Colombian and Mexican analyses was a limitation of this study. On the other hand, the association found in previous observational studies was strong and the explained variance in the proportion of Native American ancestry was uncharacteristically high for instrumental variable analysis, especially in the Mexican substudy (38.5%), which translates into relatively high statistical power: Using the online tool provided by Brion et al., taking into account the available sample sizes and explained variances, and assuming a true OR of 0.72 per standard deviation of the proportion of Native American ancestry, as reported in the earlier study by Torres et al., the present study had a statistical power of 97% for the Mexican analyses (type I error rate of 5%) [23, 36]. Furthermore, sensitivity analyses for the Mexican substudy, in which we reduced the number of IVs to achieve an explained variance similar to the Colombian substudy, had little effect on the estimated ORs.
In addition to low statistical power, pleiotropy is an important limitation of MR studies. Since first-order inverse variance weights keep the type I error rate under the causal null, we calculated Cochran’s Q statistic using first-order weights to detect heterogeneity, which often reflects pleiotropy; visually inspected scatter and funnel plots; performed MR-Egger regression to detect potential bias attributable to horizontal pleiotropy; and used radial MR to detect potentially outlying IVs. The use of alternative reference panels of Native American ancestry to preselect ancestry informative markers in both Colombian and Mexican women, and the utilisation of a more specific reference panel in the Mexican analyses hardly influenced the estimated ORs (Table 2). The Colombians and Mexicans included in the less specific reference panels of Native American ancestry are genetically more similar to other Native Americans than to Europeans and Africans, but the general recommendation is to use reference panels that are genetically as close as possible to the study population.
The present findings, which support an unconfounded relationship between the proportion of Native American ancestry and BC risk—without the need for all BC risk factors to be known, accurately measured and statistically adjusted for—may pave the way for further admixture mapping studies that complement the successful identification of a novel BC susceptibility region on 6q25 by Fejermann et al., possibly in combination with subsequent association testing. Note that the genome-wide significance level for admixture mapping is much higher than for association mapping [37, 38]. From an implementation perspective, recruiting study women from regions with a high average proportion of Native American ancestry would increase the statistical power of admixture mapping.
In summary, in this first instrumental variable analysis of the confounding-free association between Native American ancestry and BC risk in genetically admixed Colombian and Mexican women, we found a protective unconfounded effect, which was stronger for familial and ER-positive BC. Confounder-free associations are generally more relevant than observational correlations, which could be attributed to unknown or known confounding factors that are potentially unmeasurable or systematically mismeasured, and the findings of the present study provide more refined information on the potential of accounting for ethnic differences (in this case, Native American ancestry) in disease prevention (in this case, BC). The methodology applied in this investigation can be used to distinguish between confounded and unconfounded effects of genetic ancestry on other disease outcomes, contributing to understand and hopefully also reduce health disparities, and also to obtain more accurate information for future admixture mapping studies. From a more applied point of view, the present results provide strong evidence for a putatively causal effect of the proportion of Native American ancestry on BC risk, which may have direct implications for the design of more effective BC prevention strategies for Latin American women and Latinas.
Material and methods
Study populations
We used individual-level data from two previous studies contributing to the Breast Cancer Association Consortium (BCAC): The Colombian Breast Cancer Case–Control (COL-BCCC) study as described in [23, 39] and the Mexican Cancér de Mama (CAMA) study as described in [22, 40,41,42]. In brief, Colombian cases were women with a BC diagnosis after 01/01/2004 recruited between 03/2007 and 02/2011 in hospitals from Bogota, Neiva and Villavicencio, which mainly attend women from the central Andean regions of Cundinamarca and Huila. Controls were healthy, unrelated women from the same regions who participated in the Colombian National Pap smear programme and did not report a family history of breast cancer or any other type of cancer in two generations. Mexican BC patients were recruited between 01/2004 and 12/2007 in hospitals from Mexico City, Monterrey and Veracruz. Eligible cases were women with a new BC diagnosis without previous treatment who were not pregnant. Controls were matched to cases according to 5-year age groups, membership to health care institution and place of residence. In both studies, additional information was collected using health questionnaires and genomic DNA was extracted from peripheral blood. Genotypes in BCAC were determined using the Illumina custom array OncoArray [43]. Genotype and phenotype data were available from 687 Colombian BC patients (and 714 matched female controls) and from 709 Mexican BC patients (and 657 matched female controls).
The following reference panels of individuals of Native American ancestry were used for preselection of ancestry-informative markers: (1) primary Colombian analyses: 29 Colombian Native Americans (nine Inga, five Arhuaco, four Embera, three Kogi and three Waunana described by Reich et al. [30] and five Piapoco individuals from the HGDP [31]); (2) primary Mexican analyses: 177 Mexican Native Americans (49 Maya, 43 Zapotec, 30 Pima, 25 Tepehuano, 17 Mixe, five Mixtec, one Yaqui and one Purepecha described by Reich et al. [30] and four Maya and one Pima from the HGDP [31]); (3) secondary analyses, Colombian and Mexican I: 57 Native Americans from the HGDP [31] (seven Piapoco, 11 Karitiana, 21 Maya, 13 Pima, five Surui; and (4) secondary analyses, Mexican II: 115 Mexican Native Americans (49 Maya, 43 Zapotec, 17 Mixe, 5 Mixtec and one Purepecha) described by Reich et al. [30].
Methods
The study was performed in parallel in a Colombian and a Mexican study population. For each population independently, we first preselected ancestry-informative markers (AIMs) as instrumental variables (IVs) to assess the confounding-free association between the proportion of Native American ancestry and BC risk. Further sensitivity analyses and stratified analyses by characteristics in BC patients completed this study.
Mendelian randomization (MR) relies on the random assortment of genetic variants during meiosis, yielding a random distribution of alleles in the study population. Given the parental genotypes in an admixed population, the alleles of AIMs are randomly assigned at meiosis, mimicking a trial randomized by nature. We therefore first preselected genetic variants by using a method to determine the amount of information that multiallelic variants provide about individual ancestry composition, the so-called informativeness for assignment measure In [28]. For each genetic variant with j = 1, 2 possible alleles and for i = 1,…,K subpopulations we calculated:
where pj denotes the average frequency of allele j in all K subpopulations, pij the average frequency of allele j in subpopulation i, Q the (random) assignment of an individual to a subpopulation, and J the (random) genotype of one of the two alleles of an individual. The higher the In-value the more information about ancestry composition is provided by a genetic variant. We used the reference panels described above to calculate the In-value considering two populations at a time (Native American and European, Native American and African). We then preselected the 20,000 genetic variants with the highest In-value for each comparison and retained the variants that were present in at least one comparison as preselected markers of Native American ancestry.
To select valid IVs among the preselected AIMs, we selected genetic variants that were (1) robustly associated with the investigated exposure (individual proportion of Native American ancestry), (2) not associated with potential confounders, and (3) in linkage equilibrium with one another. To fulfil (1), we used the software ADMIXTURE, version 1.3.0, for supervised estimation of individual proportions of Native American ancestry using the reference panels described above [44] and retained preselected markers with a probability value for the association with the proportion of Native American ancestry lower than 5 × 10–8. To fulfil (2), we performed a PheWAS and excluded markers associated with the following phenotypes provided by MR Base: menopause, pregnancy outcomes, tobacco or cigarette smoking, alcohol consumption, educational level, contraceptives, hormone-replacement therapy, diabetes, body circumferences and breast cancer [45]. To fulfil (3), we calculated the explained variance in the proportion of Native American ancestry using the formula 36:
where β denotes the additive genetic effect and MAF denotes the allele frequency. For markers in linkage disequilibrium, which we separately identified in the 714 Colombian and the 657 Mexican female controls using the R package ‘genetics’ [46], we retained the marker with the highest explained variance. The cumulative variance explained was then calculated by adding the variances explained by all retained markers.
To visually inspect and subsequently exclude outlying IVs in the main analyses, as well as in the sensitivity and stratified analyses, we first used summary statistics adjusted for age of the association between the IVs and the exposure of interest (Native American ancestry proportion), and of the association between the IVs and the investigated outcome (BC), based on the control females as sample 1, and the BC patients and matched control females as sample 2. After performing radial MR using the R package ‘RadialMR’ [47], non-excluded markers were used as IVs to perform two-sample MR analyses using the R-version of MR-Base [45]. We also calculated Cochran’s Q statistic using inverse variance weights to preclude heterogeneity, which may indicate violation of the IV assumptions.
To complement the main results, we performed sensitivity analyses and stratified analyses. Sensitivity analyses included the calculation of weighted median estimates and MR-Egger regression to test for directional pleiotropy. To examine the possible impact of less specific reference panels, we reran the analyses with ancestry proportions estimated by replacing the primary reference individuals for Colombian and Mexican Native American ancestry with reference individuals for general Native American ancestry. The influence of a more specific reference panel was assessed by visually inspecting the principal component plots of the Mexican study population and then re-estimating the ancestry proportions only with those reference individuals genetically most similar to the study Mexican BC patients and matched controls. Genetic principal components were estimated for Colombian and Mexican study participants separately, using the respective reference panels and the eigenstrat function [48]. Additionally, we repeated the analyses limiting the number of IVs, so that the explained variance in the Mexican study was similar to the explained variance in the Colombian study. Finally, we performed stratified analyses considering only patients diagnosed before the age of 46 years, patients with a family history of breast and/or ovarian cancer, and patients affected by oestrogen-receptor (ER) positive or negative tumours, or by triple-negative BC (negative for ER, progesterone receptor, and human epidermal growth factor receptor 2).
Availability of data and materials
The source code to reproduce all the results and the necessary input files with the summary association statistics are available at www.biometrie.uni-heidelberg.de/StatisticalGenetics/Software_and_Data.
References
Bray F, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Carvajal-Carmona LG, et al. Genetic demography of Antioquia (Colombia) and the Central Valley of Costa Rica. Hum Genet. 2003;112:534–41.
Dipierri JE, et al. Paternal directional mating in two Amerindian subpopulations located at different altitudes in Northwestern Argentina. Hum Biol. 1998;70:1001–10.
González-Andrade F, Sánchez D, González-Solórzano J, Gascón S, Martínez-Jarreta B. Sex-specific genetic admixture of mestizos, Amerindian Kichwas, and Afro-Ecuadorans from Ecuador. Hum Biol. 2007;79:51–77.
Green LD, Derr JN, Knight A. mtDNA affinities of the peoples of north-central Mexico. Am J Hum Genet. 2000;66:989–98.
Marrero AR, et al. Pre- and post-Columbian gene and cultural continuity: the case of the gaucho from southern Brazil. Hum Hered. 2007;64:160–71.
Mendizabal I, et al. Genetic origin, admixture, and asymmetry in maternal and paternal human lineages in Cuba. BMC Evol Biol. 2008;8:213.
Sans M, et al. unequal contributions of male and female gene pools from parental populations in the African descendants of the city of Melo. Uruguay Am J Phys Anthropol. 2002;118:33–44.
Bryc K, et al. Genome-wide patterns of population structure and admixture among Hispanic/Latino populations. Proc Natl Acad Sci USA. 2010;107:8954–61.
Klimentidis YC, Miller GF, Shriver MD. Genetic admixture, self-reported ethnicity, self-estimated admixture, and skin pigmentation among Hispanics and native Americans. Am J Phys Anthropol. 2009;138:375–83.
Moreno-Estrada A, et al. Reconstructing the population genetic history of the caribbean. PLoS Genet. 2013;9:e1003925.
Moreno-Estrada A, et al. The genetics of Mexico recapitulates native American substructure and affects biomedical traits. Science. 2014;344:1280–5.
Sans M. Admixture studies in Latin America: from the 20th to the 21st century. 72:155–177 (2000).
Seldin MF, et al. Argentine population genetic structure: large variance in Amerindian contribution. Am J Phys Anthropol. 2007;132:455–62.
Silva-Zolezzi I, et al. Analysis of genomic diversity in Mexican Mestizo populations to develop genomic medicine in Mexico. Proc Natl Acad Sci U S A. 2009;106:8611–6.
Wang S, et al. Geographic patterns of genome admixture in Latin American Mestizos. PLoS Genet. 2008;4:e1000037.
Ruiz-Linares A, et al. Admixture in Latin America: geographic structure, phenotypic diversity and self-perception of ancestry based on 7342 individuals. PLoS Genet. 2014;10:e1004572.
Bryc K, Durand EY, Macpherson JM, Reich D, Mountain JL. The genetic ancestry of African Americans, Latinos, and European Americans across the United States. Am J Hum Genet. 2015;96:37–53.
Conomos MP, et al. Genetic diversity and association studies in US Hispanic/Latino populations: applications in the Hispanic community health study/study of Latinos. Am J Hum Genet. 2016;98:165–84.
Han Y, et al. Prostate cancer susceptibility in men of African ancestry at 8q24. J Natl Cancer Inst. 2016;108:djv431.
Fejerman L, et al. Genetic ancestry and risk of breast cancer among U.S. Latinas. Cancer Res. 2008;68:9723–8.
Fejerman L, et al. European ancestry is positively associated with breast cancer risk in Mexican women. Cancer Epidemiol Biomark Prev. 2010;19:1074–82.
Torres D, et al. Interaction between genetic ancestry and common breast cancer susceptibility variants in Colombian women. Int J Cancer. 2019;144:2181–91.
Hines LM, et al. The interaction between genetic ancestry and breast cancer risk factors among hispanic women: the breast cancer health disparities study. Cancer Epidemiol Biomark Prev. 2017;26:692–701.
Slattery ML, et al. Genetic variation in genes involved in hormones, inflammation and energetic factors and breast cancer risk in an admixed population. Carcinogenesis. 2012;33:1512–21.
Smith GD, Ebrahim S. ‘Mendelian randomization’: Can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22.
Ebrahim S, Davey Smith G. Mendelian randomization: Can genetic epidemiology help redress the failures of observational epidemiology? Hum Genet. 2008;123:15–33.
Rosenberg NA, Li LM, Ward R, Pritchard JK. Informativeness of genetic markers for inference of ancestry. Am J Hum Genet. 2003;73:1402–22.
The 1000 Genomes Project Consortium. A global reference for human genetic variation. Nature. 526:68–74 (2015).
Reich D, et al. Reconstructing native American population history. Nature. 2012;488:370–4.
Cavalli-Sforza LL. The human genome diversity project: past, present and future. Nat Rev Genet. 2005;6:333–40.
Chen T, Kharazmi E, Fallah M. Race and ethnicity-adjusted age recommendation for initiating breast cancer screening. JAMA Netw open. 2023;6:e238893.
Fejerman L, et al. Interaction between common breast cancer susceptibility variants, genetic ancestry, and nongenetic risk factors in Hispanic women. Cancer Epidemiol Biomark Prev. 2015;24:1731–8.
Rey-Vargas L, et al. Association of genetic ancestry with HER2, GRB7 AND estrogen receptor expression among Colombian women with breast cancer. Front Oncol. 2022;12:989761.
Marker KM, et al. Human epidermal growth factor receptor 2 (HER2) positive breast cancer is associated with indigenous American ancestry in Latin American women. Cancer Res. 2020;80:1893–901.
Brion MJA, Shakhbazov K, Visscher PM. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 2013;42:1497–501.
Horimoto ARVR, Xue D, Thornton TA, Blue EE. Admixture mapping reveals the association between Native American ancestry at 3q13.11 and reduced risk of Alzheimer’s disease in Caribbean Hispanics. Alzheimer’s Res Ther. 2021;13:122
Fejerman L, et al. Admixture mapping identifies a locus on 6q25 associated with breast cancer risk in US Latinas. Hum Mol Genet. 2012;21:1907–17.
Torres D, et al. Prevalence and penetrance of BRCA1 and BRCA2 germline mutations in Colombian breast cancer patients. Sci Rep. 2017;7:4713.
Ángeles-Llerenas A, et al. Moderate physical activity and breast cancer risk: the effect of menopausal status. Cancer Causes Control. 2010;21:577–86.
Torres-Mejía G, et al. Moderate-intensity physical activity ameliorates the breast cancer risk in diabetic women. Diabetes Care. 2012;35:2500–2.
Murillo-Zamora E, et al. Association between rs2981582 polymorphism in the FGFR2 Gene and the risk of breast cancer in mexican women. Arch Med Res. 2013;44:459–66.
Michailidou K, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551:92–4.
Alexander DH, Novembre J, Lange K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 2009;19:1655–64.
Hemani G, et al. The MR-base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408.
Warnes GR. The genetics package—utilities for handling genetic data. R News. 2003;3:9–13.
Bowden J, et al. Improving the visualization, interpretation and analysis of two-sample summary data Mendelian randomization via the radial plot and radial regression. Int J Epidemiol. 2018;47:1264–78.
Patterson N, Price AL, Reich D. Population structure and eigenanalysis. PLoS Genet. 2006;2:2074–93.
Acknowledgements
The CAMA study would like to thank CONACyT for the financial support provided for this work and all physicians responsible for the project in the different participating hospitals: Dr. Germán Castelazo (IMSS, Ciudad de México, DF), Dr. Sinhué Barroso Bravo (IMSS, Ciudad de México, DF), Dr. Fernando Mainero Ratchelous (IMSS, Ciudad de México, DF), Dr. Joaquín Zarco Méndez (ISSSTE, Ciudad de México, DF), Dr. Edelmiro Pérez Rodríguez (Hospital Universitario, Monterrey, Nuevo León), Dr. Jesús Pablo Esparza Cano (IMSS, Monterrey, Nuevo León), Dr. Heriberto Fabela (IMSS, Monterrey, Nuevo León), Dr. Fausto Hernández Morales (ISSSTE, Veracruz, Veracruz), Dr. Pedro Coronel Brizio (CECAN SS, Xalapa, Veracruz) and Dr. Vicente A. Saldaña Quiroz (IMSS, Veracruz, Veracruz). COLBCCC thanks all patients, the physicians Justo G. Olaya, Mauricio Tawil, Lilian Torregrosa, Elias Quintero, Sebastian Quintero, Claudia Ramírez, José J. Caicedo and Jose F. Robledo, and the technician Michael Gilbert for their contributions and commitment to this study.
Funding
Open Access funding enabled and organized by Projekt DEAL. BCAC is funded by the European Union’s Horizon 2020 Research and Innovation Programme (Grant Numbers 634935 and 633784 for BRIDGES and B-CAST respectively) and by the PERSPECTIVE I&I project, funded by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research, the Ministère de l’Économie et de l'Innovation du Québec through Genome Québec, and the Quebec Breast Cancer Foundation. The EU Horizon 2020 Research and Innovation Programme funding source had no role in study design, data collection, data analysis, data interpretation or writing of the report. Additional funding for BCAC is provided via the Confluence project, which is funded with intramural funds from the National Cancer Institute Intramural Research Program, National Institutes of Health. Genotyping of the OncoArray was funded by the NIH Grant U19 CA148065, Cancer Research UK Grant C1287/A16563 and the PERSPECTIVE project supported by the Government of Canada through Genome Canada, the Canadian Institutes of Health Research (Grant GPH-129344), the Ministère de l’Économie, Science et Innovation du Québec through Genome Québec and the PSRSIIRI-701 grant, and the Quebec Breast Cancer Foundation. The CAMA study was funded by Consejo Nacional de Ciencia y Tecnología (CONACyT) (SALUD-2002-C01-7462). Sample collection and processing was funded in part by grants from the National Cancer Institute (NCI R01CA120120 and K24CA169004). COLBCCC was supported by the German Cancer Research Center (DKFZ), Heidelberg, Germany. Diana Torres was in part supported by a postdoctoral fellowship from the Alexander von Humboldt Foundation.
Author information
Authors and Affiliations
Contributions
JLB developed the main conceptual idea. LZ performed the statistical genetic analysis and wrote the original draft under the supervision of JLB and UH, DT, IB, MG, GTM, JD, MKB and QW were involved in data generation and curation. MKB provided critical feedback and MG provided technical assistance. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Colombian Breast Cancer Case–Control (COL-BCCC) study and the Mexican Cancér de Mama (CAMA) study were conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving human subjects were approved by the institutional review boards of the Pontificia Universidad Javeriana in Bogotá, Colombia and the Mexican National Institute of Public Health, respectively. Written informed consent was obtained from all study participants in advance of data and sample retrieval.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. 1.
Scatter plots of first versus second, and first versus third genetic principal components (PC) of study participants (crosses: BC patients, circles: population-based controls) and reference panels of African, European and Native American ancestry (reference individuals represented by triangles; Native Americans from the Human Genome Diversity Project, N1: Karitiana, N2: Surui, N3: Piapoco, N4: Maya, N5: Pima); panel A: Colombian study, panel B: Mexican study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zollner, L., Torres, D., Briceno, I. et al. Native American ancestry and breast cancer risk in Colombian and Mexican women: ruling out potential confounding through ancestry-informative markers. Breast Cancer Res 25, 111 (2023). https://doi.org/10.1186/s13058-023-01713-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-023-01713-5