Abstract
Background
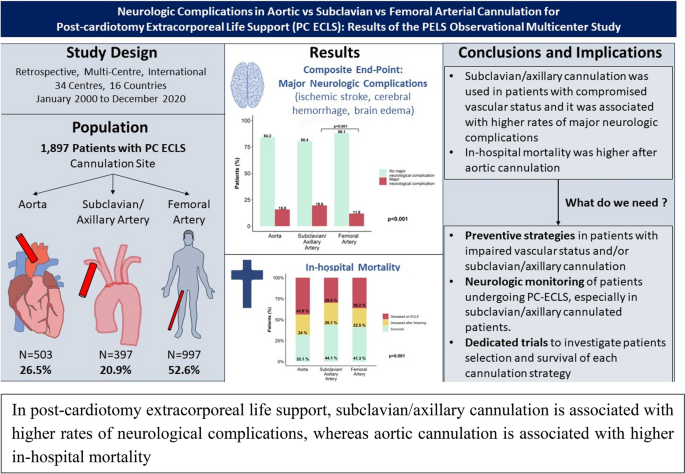
Cerebral perfusion may change depending on arterial cannulation site and may affect the incidence of neurologic adverse events in post-cardiotomy extracorporeal life support (ECLS). The current study compares patients' neurologic outcomes with three commonly used arterial cannulation strategies (aortic vs. subclavian/axillary vs. femoral artery) to evaluate if each ECLS configuration is associated with different rates of neurologic complications.
Methods
This retrospective, multicenter (34 centers), observational study included adults requiring post-cardiotomy ECLS between January 2000 and December 2020 present in the Post-Cardiotomy Extracorporeal Life Support (PELS) Study database. Patients with Aortic, Subclavian/Axillary and Femoral cannulation were compared on the incidence of a composite neurological end-point (ischemic stroke, cerebral hemorrhage, brain edema). Secondary outcomes were overall in-hospital mortality, neurologic complications as cause of in-hospital death, and post-operative minor neurologic complications (seizures). Association between cannulation and neurological outcomes were investigated through linear mixed-effects models.
Results
This study included 1897 patients comprising 26.5% Aortic (n = 503), 20.9% Subclavian/Axillary (n = 397) and 52.6% Femoral (n = 997) cannulations. The Subclavian/Axillary group featured a more frequent history of hypertension, smoking, diabetes, previous myocardial infarction, dialysis, peripheral artery disease and previous stroke. Neuro-monitoring was used infrequently in all groups. Major neurologic complications were more frequent in Subclavian/Axillary (Aortic: n = 79, 15.8%; Subclavian/Axillary: n = 78, 19.6%; Femoral: n = 118, 11.9%; p < 0.001) also after mixed-effects model adjustment (OR 1.53 [95% CI 1.02–2.31], p = 0.041). Seizures were more common in Subclavian/Axillary (n = 13, 3.4%) than Aortic (n = 9, 1.8%) and Femoral cannulation (n = 12, 1.3%, p = 0.036). In-hospital mortality was higher after Aortic cannulation (Aortic: n = 344, 68.4%, Subclavian/Axillary: n = 223, 56.2%, Femoral: n = 587, 58.9%, p < 0.001), as shown by Kaplan–Meier curves. Anyhow, neurologic cause of death (Aortic: n = 12, 3.9%, Subclavian/Axillary: n = 14, 6.6%, Femoral: n = 28, 5.0%, p = 0.433) was similar.
Conclusions
In this analysis of the PELS Study, Subclavian/Axillary cannulation was associated with higher rates of major neurologic complications and seizures. In-hospital mortality was higher after Aortic cannulation, despite no significant differences in incidence of neurological cause of death in these patients. These results encourage vigilance for neurologic complications and neuromonitoring use in patients on ECLS, especially with Subclavian/Axillary cannulation.
Graphical abstract
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Extracorporeal life support (ECLS) represents a strategy of temporary mechanical circulatory support for refractory post-cardiotomy (PC) cardiogenic shock [1, 2]. ECLS has gained an important role in perioperative care, especially in patients with high-risk profiles undergoing complex cardiac surgical procedures [3]. Nonetheless, morbidity and mortality in such patients are consistently high, with minimal evidence available on long-term and functional outcomes [3, 4]. Particularly, data regarding patients’ neurological outcomes and association with different cannulation approaches in PC-ECLS are lacking and urgently needed to understand the pathophysiology of these complications, monitor and prevent them [5,6,7]. Since cerebral perfusion patterns during ECLS may be different depending on the arterial cannulation site (antegrade vs. retrograde flow in ascending or descending aorta), the baseline vascular condition or hypoxia, the choice of the return site could potentially lead to a different likelihood of neurologic complications. Nevertheless, evidence on this topic is scarce [8] and the assessment of cerebral autoregulation in relation to cannulation settings or ECLS patient’s characteristics is complex. Moreover, little evidence addressing the relationship between the return cannulation site and neurologic injury exists to inform our cannulation strategy in PC-ECLS patients. In this study, we hypothesize that different ECLS cannulation strategies are associated with different rates of major neurological outcomes including stroke, cerebral bleeding and brain edema. We aim to compare patients' neurologic outcomes in three commonly used ECLS arterial cannulation sites: aortic vs subclavian/axillary vs femoral artery.
Methods
The multicenter, retrospective observational Post-cardiotomy Extracorporeal Life Support (PELS) study enrolled consecutive patients supported with ECLS in the post-operative phase (ClinicalTrials.gov: NCT03857217) in 34 centers from 16 countries. Adults (≥ 18 years old) were included if they underwent veno-arterial (V-A) ECLS implantation during or after cardiac surgery between January 2000 and December 2020. For the present analysis, we compared three cannulation strategies analyzing preoperative, intra-operative and post-operatory characteristics, neurologic complications and in-hospital mortality (Supplementary Table 1 and 2). Exclusion criteria were veno-venous configuration, mixed cannulations, pulmonary artery cannulation, and cannulation sites unknown (Supplementary Fig. 1).
The current study was conducted in accordance with the Declaration of Helsinki. Institutional Review Board (IRB) approval was acquired in all centers based on the IRB-approval of the coordinating center (METC-2018–0788). The need for informed consent was waived due to the observational character of the study, the emergency of the performed procedure, and the de-identification of shared data. Study was performed following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (Appendix) [9].
Data collection and outcomes
Data were collected centrally according to data-sharing agreements between participating centers [3]. Demographics, pre-operative clinical, procedural characteristics, ECLS details, in-hospital morbidity and mortality, and post-discharge survival were included in a dedicated form (data.castoredc.com). Follow-up data were collected through the review of the most recent medical records or contact with patients at discretion of the treating center. The primary outcome was a composite end-point of major neurologic complications (ischemic stroke, cerebral hemorrhage, brain edema). Secondary outcomes included seizures, all-cause in-hospital mortality, neurologic complication as cause of in-hospital mortality and mortality at follow-up after hospital discharge.
Statistical analysis
The full cohort was categorized into three study groups based on arterial cannulation site (ascending aorta, subclavian/axillary artery, femoral artery). Missing data analysis (Supplementary Table 2) was conducted with the mice: Multivariate Imputation by Chained Equations (MICE) R package [10]. Missing data patterns were investigated and were identified as missing completely at random (MCAR). Descriptive statistics were conducted on available data only and no imputations were performed for this purpose. Normality was tested for continuous variables. Continuous variables were reported as median and interquartile range (IQR) and analyzed with Mann Whitney U-test. Chi-square Test and Fisher’s Exact Test were used to compare group differences for categorical variables expressed as count (percentage). In case of significant differences between groups, post-hoc comparisons were performed and adjusted by the Bonferroni correction for multiple tests (Supplementary Table 3). A p-value < 0.05 was considered statistically significant. Survival was investigated with the Kaplan–Meier method and comparisons were performed with Log-rank test. Based on the possible variations in ECLS management over the study period and the confounding factors represented by cardiac arrest, previous stroke, previous transient ischemic attack, peripheral artery disease (PAD), two sensitivity analysis were performed after exclusion of patients who received post-cardiotomy ECLS before 2010 (2010–2020 cohort) and those with the abovementioned conditions. To estimate the associations between type of cannulation (reference group: femoral cannulation) and composite end-point of major neurological complications, we conducted a mixed-effects multivariable logistic regression, using the lme4: Linear Mixed-Effects Models using 'Eigen' and S4 R package [11]. The random effect was used to account for dependency of observations due to clustering in centers and in years. We first estimated a crude model, which was subsequently adjusted for sets of variables deemed potential confounders for the association with the outcome: Model 1, crude model with variable “Arterial cannulation site”; Model 2, arterial cannulation site, PAD; Model 3, arterial cannulation site, PAD, stroke; Model 4, arterial cannulation site, PAD, stroke, interaction stroke*PAD; Model 5, arterial cannulation site, PAD, stroke, hypertension, dialysis, diabetes, preoperative cardiac arrest; Model 6, arterial cannulation site, PAD, stroke, hypertension, dialysis, diabetes, preoperative cardiac arrest, emergency surgery, coronary artery bypass graft (CABG), aortic surgery, cardiopulmonary bypass (CPB) time; Model 7, arterial cannulation site, PAD, stroke, hypertension, dialysis, diabetes, preoperative cardiac arrest, emergency surgery, CABG, aortic surgery, CPB time, implant timing, cardiac arrest as indication for ECLS. Data were merged and analyzed using SPSS 26.0 (IBM, New York, USA), and R 4.4.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline, surgical, and ECLS characteristics
Overall, 1897 PC-ECLS patients were included in the current study: 503 patients (26.5%) underwent aortic, 397 (20.9%) subclavian/axillary and 997 (52.6%) femoral cannulation (Table 1). Each center enrolled a median value of 24 patients per center (Supplementary Fig. 2). A history of hypertension (p < 0.001), smoking (p = 0.013), diabetes (p = 0.002), previous stroke (p = 0.007), previous myocardial infarction (p = 0.002), and dialysis (p = 0.041) was more frequent in the subclavian/axillary cannulation group (Table 1 and Supplementary Table 3). PAD was less frequent in femoral cannulation (n = 99, 9.9%), compared to aortic (n = 96, 19.1%) and subclavian/axillary cannulation (n = 86, 21.7%; p < 0.001; Table 1 and Supplementary Table 3). A higher rate of pre-operative cardiac arrest was observed in subclavian/axillary cannulation (p = 0.005). Emergency surgery occurred less frequently before femoral cannulation (p < 0.001) and CABG was more frequent in subclavian/axillary and aortic than femoral cannulation (p < 0.001, Table 2). Cardiopulmonary bypass (CPB) time was longer in aortic (215 min [IQR 143–294 min]) and subclavian/axillary (218 min [IQR 161–307 min]) groups, compared to femoral cannulation (192 min [IQR 129–272 min], p < 0.001, Table 2 and Supplementary Table 3).
Most common indication for ECLS was failure to wean from cardiopulmonary bypass which was more common in the subclavian/axillary group compared to others (p < 0.001) (Table 3). Active left ventricular unloading strategies were applied in 205 patients (49.6%) in aortic, 43 patients (15.0%) in subclavian/axillary and 237 patients (27.4%) in femoral cannulation (p < 0.001). Patients were supported on ECLS for a median of 120 h (IQR, 56–206 h) in aortic, 116 h (IQR, 69–182 h) in subclavian/axillary and 116 h (IQR, 52–192 h) in femoral group (p = 0.557). Number of units of post-operatively transfused erythrocyte concentrates was similar in all groups (Supplementary Table 4).
Neurological outcomes and associated variables
The composite end-point of major neurological complications was differently distributed between subclavian/axillary (n = 78, 19.6%), aortic (n = 79, 15.8%) and femoral cannulation (n = 118, 11.9%, p < 0.001) with subclavian/axillary cannulation showing a higher rate of events compared to femoral cannulation (p = 0.001; Fig. 1). Cerebral hemorrhage (aortic: n = 16, 3.2%; subclavian/axillary: n = 22, 5.9%; femoral: n = 21, 2.3%, p = 0.004) and stroke (aortic: n = 59, 11.8%; subclavian/axillary: n = 63, 15.9%; femoral: n = 80, 8.1%, p < 0.001) were more frequent in patients cannulated with subclavian/axillary approach. Seizures were more common in subclavian/axillary (n = 13, 3.4%) compared to aortic (n = 9, 1.8%) and femoral cannulation (n = 12, 1.3%, p = 0.036). No difference between groups was observed in cerebral hemorrhage severity (p = 0.051) and stroke severity (p = 0.197, Table 4). Neuro-monitoring was used very infrequently (Table 5). Regression models with random effects for centers and years, subclavian/axillary cannulation was associated with higher risk of neurological complications (OR 1.50 [95% CI 1.05–2.15], p = 0.027), also after adjustment for peripheral artery disease, stroke, hypertension, dialysis, diabetes, preoperative cardiac arrest, emergency surgery, CABG, aortic surgery, CPB time, implant timing, cardiac arrest as indication for ECLS (OR 1.53 [95% CI 1.02–2.31], p = 0.041; Table 6).
Secondary outcomes
Intensive care unit stay was longer in subclavian/axillary than aortic or femoral cannulation (p < 0.001, Table 4), with a higher in-hospital mortality in the aortic group (aortic: n = 344, 68.4%; subclavian/axillary: n = 223, 56.2%; femoral: n = 587, 58.9%; p < 0.001, Fig. 2 and Supplementary Table 3), also confirmed by Kaplan–Meier curves (Fig. 3). More patients deceased during ECLS support in the aortic cannulation group (n = 217, 43.8%) compared to subclavian/axillary (n = 103, 29.9%) and femoral groups (n = 360, 36.3%, p < 0.001 Supplementary Table 3). No differences were found in main causes of in-hospital death between groups (p = 0.433). Median Follow-up time was 11 days for in-hospital deaths (IQR: 4–22) and 885 days for hospital survivors (IQR: 91–1916).
Sensitivity analysis
In the sensitivity analysis excluding patients supported before 2010 (Supplementary Tables 5–8), we confirmed the same distribution of the primary outcome and in-hospital mortality observed in the main analysis (Supplementary Fig. 3–5). In the sensitivity analysis excluding patients who suffered previous stroke, previous transient ischemic attack, peripheral vessel disease or with cardiac arrest during hospital stay (Supplementary Tables 9–12), the composite neurological end-point occurred more frequently in the subclavian/axillary group (aortic: n = 48, 15.6%; subclavian/axillary: n = 38, 18.0%; femoral: n = 62, 9.2%; p = 0.001; Supplementary Fig. 6). In-hospital mortality remained higher in the aortic cannulation group (aortic: n = 215, 69.8%; subclavian/axillary: n = 103, 48.8%; femoral: n = 370, 56.3%; p < 0.001; Supplementary Fig. 7–8).
Discussion
This study investigated neurological complications in one of the largest cohorts of PC-ECLS patients. The study has four main findings. First, femoral cannulation remains the most used cannulation approach (53%), while subclavian/axillary cannulation (21%) and aortic cannulation (26%) are less used. Second, we found that patients with subclavian/axillary cannulation had worse baseline vascular conditions as shown by higher prevalence of previous stroke, previous myocardial infarction, dialysis, preoperative cardiac arrest and peripheral artery disease. Third, we showed that the composite outcome of neurological complications occurred in almost 20% of patients cannulated with subclavian/axillary, compared to 12–16% of patients cannulated with femoral and aortic approach. Finally, we found higher in-hospital mortality in the aortic group, despite the lower incidence of neurological complications, confirmed by two sensitivity analyses after exclusion of patients supported before 2010 and those with cardiac arrest, stroke, previous transient ischemic attack, peripheral vessel disease.
Overall neurological complications occur in almost 20% of V-A ECLS patients as reported by literature [12]. However, it is still difficult to identify which patient might develop such a complication, its relationship with cerebral autoregulation, its predicted severity, or whether a specific ECLS setting may be related to more neurological events. Moreover, effective strategies to prevent such complications or monitor their early onset are urgently needed to improve PC-ECLS outcomes. Literature supports the hypothesis that cerebral perfusion during ECLS might be influenced by the arterial cannulation site, but whether this could influence neurologic complications is still unknown [13, 14]. Arterial cannulation approach may significantly vary, as demonstrated by this analysis of the PC-ECLS population, with femoral cannulation used in 52.6% of patients, subclavian/axillary cannulation in 20.9% and aortic cannulation used in 26.5% of patients. Femoral cannulation remains the preferred cannulation strategy in PC-ECLS [15], but its superiority in terms of fewer brain embolization events compared to the central aortic one is still debated, as mechanisms underlying the potential beneficial effects of peripheral cannulation have to be confirmed [16,17,18,19].
The first step to understanding the association of neurological outcomes and cannulation strategy implies an analysis of patients’ characteristics to identify specific risk profiles for adverse events, identify best candidates for each cannulation strategy, and also understand how clinicians currently select patients for each cannulation approach. This study showed that patients who were cannulated with subclavian/axillary approach were characterized by a worse vascular status compared to others. Moreover, a significant amount of them received emergency surgery and experienced cardiogenic shock or cardiac arrest before the operation. This observation suggests that the subclavian/axillary cannulation is preferred in case of worse patient’s vascular status, possibly because the subclavian/axillary artery is more often free from atheromatic disease compared to femoral vessels or ascending aorta [20, 21]. Surprisingly, subclavian/axillary cannulation was not predominantly used in aortic surgery, even though the subclavian/axillary artery is often cannulated to initiate CPB during this type of operation [20]. Aortic surgery is usually associated with higher neurological risks due to the possible disease involvement of neck vessels or the need for a circulatory arrest [16, 22], but interaction between disease extension and ECLS cannulation approach needs further investigations.
CPB time was slightly longer in patients cannulated with subclavian/axillary and aortic approach compared to femoral approach. This could be explained by the higher surgical complexity that characterized the subclavian/axillary group, whose patients underwent two or more procedures in 28% of cases compared to the 16–18% of other groups. A longer CPB time might influence cerebral circulation and neurological outcomes. However, the interaction between CPB time and flow, intra-operative CPB cannulation and ECLS cannulation sites, hemodynamic parameters, and patient’s vascular status is still under-investigated and requires the development of dedicated studies.
Observations from this study demonstrated that the composite neurological end-point including stroke, brain hemorrhage and brain oedema occurs more frequently in subclavian/axillary cannulation, with 6% of patients suffering cerebral hemorrhage and 16% of patients suffering ischemic stroke in the subclavian/axillary group. Also, clinical seizures were more common in subclavian/axillary patients. The adjusted analysis, which accounted for a range of the ECLS-independent confounding factors, demonstrated that the subclavian/axillary cannulation site remained independently associated with increased neurologic complications. This finding underscores the significance of the cannulation strategy in influencing patient outcomes during ECLS and reduces the likelihood that the observed differences were merely due to the subclavian/axillary group being sicker already before the cannulation. Although tracing the pathophysiological mechanism of these events was beyond the scope of this observational study, we can hypothesize an additive effect of baseline cerebral and vascular comorbidities, an intra-operative alteration of the cerebral blood flow, the lack of pulsatility due to ECLS, an altered cerebral autoregulation and the flow pattern determined by the arterial cannulation site. Moreover, an autoregulatory dysfunction may contribute to neurological dysfunction, but how it interacts with ECLS and cannula flow is still unknown [13, 14, 23, 24] and mechanisms of cerebral autoregulation in the specific setting of non-pulsatile blood flow and after different cannulation strategies are still an active research area [8, 19, 21].
To further investigate all these aspects and allow for an early detection of neurological complications, dedicated neurological monitoring strategies during ECLS are advised even if no specific guidelines still exist. PELS study demonstrated that neurologic monitoring (such as near-infrared spectroscopy, transcranial doppler, electroencephalogram and brain computed tomography) is still not routinely used. However, literature suggests that standardized neuromonitoring, when implemented, significantly improves the detection [25, 26] of acute brain injuries in ECLS patients; particularly lack of blood flow monitoring may be associated with increased stroke incidence [27,28,29]. Strong heterogeneity exists also in anticoagulation protocols and unloading strategies that might play an important role in determining thrombotic and hemorrhagic brain events and cardiac recovery [30,31,32]. This study demonstrated a less frequent use of left ventricular unloading strategies in the subclavian/axillary group. Considering the different flow pattern with antegrade flow in the descending aorta, subclavian/axillary cannulation is deemed to be less burdened by left ventricular afterload increase and pulmonary edema. This different hemodynamic pattern might induce a less frequent use of left ventricular unloading strategies [33]. Furthermore, institutional practices and protocols for ECLS management can vary significantly, and some centers may have a “lower threshold” for implementing unloading in patients with femoral or aortic cannulation compared to those with subclavian/axillary approach.
Several studies report in-hospital mortality of patients undergoing PC V-A ECLS around 60% with different variations, depending on weight of surgery, patient’s age and center’s expertise [3, 21, 27, 29, 34,35,36]. Our survival outcomes were also comparable to those presented in the previous studies and reports from the Extracorporeal Life Support Organization (ELSO) registry [21, 37], although variations may be related to the specific characteristics of our patient cohort. This comparison underscores the validity of our results and highlights the importance of considering patient-specific factors when evaluating ECLS outcomes. Our study also confirmed the importance of describing the death timing when reporting on ECLS mortality [38]. For example, we noticed a higher percentage of on-support mortality within the aortic group that significantly contributes the overall higher mortality in this group. This suggests that the inability to wean from ECLS is a critical factor contributing to the increased mortality in the aortic group, likely reflecting a more severe underlying condition or a less favorable response to ECLS support.
This finding opens the discussion on the fate of ECLS patients with neurological damage. Previous studies showed that patients on V-A ECLS support experiencing neurological complications had an increased in-hospital mortality, by a factor of 2–3 [13, 39,40,41]. Moreover, severe neurological damage could be a reason to withdraw the support. However, neurological complications remain limited in the ECLS population, and they seem not to be the main driver of mortality [39]. Therefore, these complications, especially the "minor" ones, should not push toward support withdrawal.
The observation that neurologic complications were not the primary cause of mortality in our cohort may be partly explained by the extended period required for neurologic recovery. Clinical teams may be inclined to continue ECLS support while awaiting potential neurologic improvement, as early withdrawal could preclude recovery that may take days to weeks to become evident. This approach emphasizes the importance of patient-specific management and multimodal neurologic monitoring to guide decision-making during ECLS support.
As clinical experience accumulates and ECLS becomes more widely used, focused research on neurological monitoring and management of neurological complications are imperative to improve early and long-term outcomes. Particularly, it is warranted to evaluate if improving neurological monitoring, anticoagulation protocols, neurological targeted therapy, prognostication, and follow-up, may mitigate incidence and severity of neurological complications in all patients, and especially in those with bad vascular status and/or subclavian cannulation. Since we included patients from different centers and countries, our results may be applicable to a large variety of patients treated with PC-ECLS.
Strengths and limitations
PELS is observational by nature, so causal inference is not possible, and it was not designed to specifically investigate vascular diseases (i.e. carotid stenosis) and neurological outcomes with dedicated tools [12, 16, 41]. Details about CPB cannulation strategies during the index operation or timing (on ECLS, before or after ECLS) of neurological complications were not available, preventing any deeper causal investigation. Moreover, specific data on ECLS selection criteria, protocols, anticoagulation and weaning strategies, cannulation technique and personnel (surgical vs percutaneous) are not captured by the database and could therefore not be included in this study. Similarly, intraoperative and postoperative hemodynamic parameters, oxygen delivery and hypoxia, cerebral autoregulation influencing factors, coagulation parameters, anesthesia management protocols, vasopressors and inotropes usage, reasons for withdrawal of ECLS support, post-discharge quality of life, functional status, re-hospitalization events after discharge and follow-up specific data. As previously mentioned, sicker patients with compromised vascular status more frequently received subclavian/axillary. Therefore, we cannot rule out the effects of confounding by severity and indication which is the main limiting factor of this analysis. While we used models to adjust for these confounding variables, we recognize that these adjustments cannot fully eliminate all biases. Since the observational nature of PELS study, we also cannot infer on relations between other complications (acute kidney injury, pneumonia, acute respiratory distress syndrome, embolism, and arrhythmia, etc.) more common after subclavian/axillary, and neurological complications. Furthermore, we had no access to long-term functional status of these patients, therefore additional studies are warranted in this respect. Participation to the PELS study was on a voluntary basis and centers received no funding for this study. Thus, we cannot exclude that some centers did not provide all available data or included all consecutive patients due to lack of resources, despite the actions taken to support a comprehensive and granular data collection (Supplementary Fig. 2). Indeed, we encountered some missing data, especially regarding severity of stroke or cerebral hemorrhage and vasospasm (Supplementary Table 2). Caution should be applied in the interpretation of data regarding post-operative transfusions due to a high percentage of missing data (n = 918/1897, 48.4%), especially in the subclavian/axillary group. Nevertheless, external validity of our study is supported by the large cohort, the use of linear mixed-effects models including center and year as random effects, and the international participation.
Conclusions
In this cohort of the PC-ECLS Study, subclavian/axillary cannulation was used in patients with compromised vascular status, and it was associated with higher rates of major neurologic complications and seizure, especially compared to femoral cannulation. In-hospital mortality was higher after aortic cannulation, despite no significant differences in incidence of neurological cause of death in these patients. These results focus attention on the application of preventive strategies in patients with impaired vascular status and/or subclavian/axillary cannulation, encouraging dedicated prospective trials. Eventually, this study suggests the need for an adequate neurologic monitoring of patients undergoing PC-ECLS, especially in subclavian/axillary cannulated patients.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- CABG:
-
Coronary artery bypass surgery
- CPB:
-
Cardiopulmonary bypass
- ECLS:
-
Extracorporeal life support
- IQR:
-
Interquartile range
- IRB:
-
Institutional review board
- NYHA:
-
New York Heart Association
- PAD:
-
Peripheral artery disease
- PC-ECLS:
-
Post-cardiotomy extracorporeal life support
- PC:
-
Post-cardiotomy
- V-A:
-
Veno-arterial
References
Lorusso R, Shekar K, MacLaren G, et al. ELSO interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. Asaio J. 2021;67(8):827–44. https://doi.org/10.1097/mat.0000000000001510.
Lorusso R, Whitman G, Milojevic M, et al. 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. J Thorac Cardiovasc Surg. 2021;161(4):1287–331. https://doi.org/10.1016/j.jtcvs.2020.09.045.
Mariani S, Heuts S, van Bussel BCT, et al. Patient and management variables associated with survival after postcardiotomy extracorporeal membrane oxygenation in adults: The PELS-1 Multicenter Cohort Study. J Am Heart Assoc. 2023;12(14):e029609. https://doi.org/10.1161/jaha.123.029609.
Mariani S, van Bussel BCT, Ravaux JM, et al. Variables associated with in-hospital and postdischarge outcomes after postcardiotomy extracorporeal membrane oxygenation: Netherlands Heart Registration Cohort. J Thorac Cardiovasc Surg. 2023;165(3):1127-1137.e14. https://doi.org/10.1016/j.jtcvs.2022.08.024.
Biancari F, Dalén M, Fiore A, et al. Multicenter study on postcardiotomy venoarterial extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2020;159(5):1844-1854.e6. https://doi.org/10.1016/j.jtcvs.2019.06.039.
Meani P, Matteucci M, Jiritano F, et al. Long-term survival and major outcomes in post-cardiotomy extracorporeal membrane oxygenation for adult patients in cardiogenic shock. Ann Cardiothorac Surg. 2019;8(1):116–22. https://doi.org/10.21037/acs.2018.12.04.
Schaefer AK, Riebandt J, Bernardi MH, et al. Fate of patients weaned from post-cardiotomy extracorporeal life support. Eur J Cardiothorac Surg. 2022;61(5):1178–85. https://doi.org/10.1093/ejcts/ezac035.
Caturegli G, Zhang LQ, Mayasi Y, et al. Characterization of cerebral hemodynamics with TCD in patients undergoing VA-ECMO and VV-ECMO: a prospective observational study. Neurocrit Care. 2023;38(2):407–13. https://doi.org/10.1007/s12028-022-01653-6.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67. https://doi.org/10.18637/jss.v045.i03.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. https://doi.org/10.18637/jss.v067.i01.
Shoskes A, Migdady I, Rice C, et al. Brain injury is more common in venoarterial extracorporeal membrane oxygenation than venovenous extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit Care Med. 2020;48(12):1799–808. https://doi.org/10.1097/ccm.0000000000004618.
Mateen FJ, Muralidharan R, Shinohara RT, Parisi JE, Schears GJ, Wijdicks EF. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011;68(12):1543–9. https://doi.org/10.1001/archneurol.2011.209.
Kazmi SO, Sivakumar S, Karakitsos D, Alharthy A, Lazaridis C. Cerebral pathophysiology in extracorporeal membrane oxygenation: pitfalls in daily clinical management. Crit Care Res Pract. 2018;2018:3237810. https://doi.org/10.1155/2018/3237810.
Radakovic D, Hamouda K, Penov K, et al. Central versus peripheral arterial cannulation for veno-arterial extracorporeal membrane oxygenation in post-cardiotomy patients. Asaio J. 2021;67(1):67–73. https://doi.org/10.1097/mat.0000000000001202.
Puthettu M, Vandenberghe S, Demertzis S. Effect of cannulation site on emboli travel during cardiac surgery. J Cardiothorac Surg. 2021. https://doi.org/10.1186/s13019-021-01564-1.
Raffa GM, Kowalewski M, Brodie D, et al. Meta-analysis of peripheral or central extracorporeal membrane oxygenation in postcardiotomy and non-postcardiotomy shock. Ann Thorac Surg. 2019;107(1):311–21. https://doi.org/10.1016/j.athoracsur.2018.05.063.
Mariscalco G, Salsano A, Fiore A, et al. Peripheral versus central extracorporeal membrane oxygenation for postcardiotomy shock: Multicenter registry, systematic review, and meta-analysis. J Thorac Cardiovasc Surg. 2020;160(5):1207-1216.e44. https://doi.org/10.1016/j.jtcvs.2019.10.078.
Lee SI, Lim YS, Park CH, Choi WS, Choi CH. Importance of pulse pressure after extracorporeal cardiopulmonary resuscitation. J Card Surg. 2021;36(8):2743–50. https://doi.org/10.1111/jocs.15614.
Papadopoulos N, Ahmad Ael S, Marinos S, Moritz A, Zierer A. Simple and controlled method to avoid hyperperfusion of the right arm following axillary artery cannulation for extracorporeal membrane oxygenator support. Thorac Cardiovasc Surg. 2013;61(7):581–3. https://doi.org/10.1055/s-0032-1327763.
Kowalewski M, Zieliński K, Brodie D, et al. Venoarterial extracorporeal membrane oxygenation for postcardiotomy shock-analysis of the extracorporeal life support organization registry. Crit Care Med. 2021;49(7):1107–17. https://doi.org/10.1097/ccm.0000000000004922.
Schaefer AK, Distelmaier K, Riebandt J, et al. Access site complications of postcardiotomy extracorporeal life support. J Thorac Cardiovasc Surg. 2022;164(5):1546-1558.e8. https://doi.org/10.1016/j.jtcvs.2021.09.074.
Zhang LQ, Chang H, Kalra A, et al. Continuous monitoring of cerebral autoregulation in adults supported by extracorporeal membrane oxygenation. Neurocrit Care. 2024. https://doi.org/10.1007/s12028-023-01932-w.
Khanduja S, Kim J, Kang JK, et al. Hypoxic-ischemic brain injury in ECMO: pathophysiology, neuromonitoring, and therapeutic opportunities. Cells. 2023. https://doi.org/10.3390/cells12111546.
Lorusso R, Raffa GM, Kowalewski M, et al. Structured review of post-cardiotomy extracorporeal membrane oxygenation: Part 2-pediatric patients. J Heart Lung Transpl. 2019;38(11):1144–61. https://doi.org/10.1016/j.healun.2019.07.004.
Kowalewski M, Raffa G, Zieliński K, et al. Baseline surgical status and short-term mortality after extracorporeal membrane oxygenation for post-cardiotomy shock: a meta-analysis. Perfusion. 2020;35(3):246–54. https://doi.org/10.1177/0267659119865122.
Wang L, Yang F, Wang X, et al. Predicting mortality in patients undergoing VA-ECMO after coronary artery bypass grafting: the REMEMBER score. Crit Care. 2019;23(1):11. https://doi.org/10.1186/s13054-019-2307-y.
Ong CS, Etchill E, Dong J, et al. Neuromonitoring detects brain injury in patients receiving extracorporeal membrane oxygenation support. J Thorac Cardiovasc Surg. 2023;165(6):2104-2110.e1. https://doi.org/10.1016/j.jtcvs.2021.09.063.
Hu RTC, Broad JD, Osawa EA, et al. 30-day outcomes post veno-arterial extra corporeal membrane oxygenation (VA-ECMO) after cardiac surgery and predictors of survival. Heart Lung Circ. 2020;29(8):1217–25. https://doi.org/10.1016/j.hlc.2020.01.009.
Mariani S, Bari G, Ravaux JM, et al. Heterogeneity in clinical practices for post-cardiotomy extracorporeal life support: a pilot survey from the PELS-1 multicenter study. Artif Organs. 2023. https://doi.org/10.1111/aor.14601.
Thomas J, Kostousov V, Teruya J. Bleeding and thrombotic complications in the use of extracorporeal membrane oxygenation. Semin Thromb Hemost. 2018;44(1):20–9. https://doi.org/10.1055/s-0037-1606179.
Olson SR, Murphree CR, Zonies D, et al. Thrombosis and bleeding in extracorporeal membrane oxygenation (ECMO) without anticoagulation: a systematic review. Asaio J. 2021;67(3):290–6. https://doi.org/10.1097/mat.0000000000001230.
Vale JD, Kantor E, Papin G, et al. Femoro-axillary versus femoro-femoral veno-arterial extracorporeal membrane oxygenation for refractory cardiogenic shock: a monocentric retrospective study. Perfusion. 2024. https://doi.org/10.1177/02676591241261330.
Brewer JM, Tran A, Yu J, et al. ECMO after cardiac surgery: a single center study on survival and optimizing outcomes. J Cardiothorac Surg. 2021;16(1):264. https://doi.org/10.1186/s13019-021-01638-0.
Chen F, Wang L, Shao J, Wang H, Hou X, Jia M. Survival following venoarterial extracorporeal membrane oxygenation in postcardiotomy cardiogenic shock adults. Perfusion. 2020;35(8):747–55. https://doi.org/10.1177/0267659120931306.
Biancari F, Dalén M, Fiore A, et al. Gender and the outcome of postcardiotomy veno-arterial extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2022;36(6):1678–85. https://doi.org/10.1053/j.jvca.2021.05.015.
Organization ELS. ELSO Registry 2024 report. Tuesday, May 21, 2024, 2024. https://www.elso.org/registry/internationalsummaryandreports/internationalsummary.aspx
Mariani S, Schaefer AK, van Bussel BCT, et al. On-support and postweaning mortality in postcardiotomy extracorporeal membrane oxygenation. Ann Thorac Surg. 2023;116(5):1079–89. https://doi.org/10.1016/j.athoracsur.2023.05.045.
Cho SM, Farrokh S, Whitman G, Bleck TP, Geocadin RG. Neurocritical care for extracorporeal membrane oxygenation patients. Crit Care Med. 2019;47(12):1773–81. https://doi.org/10.1097/ccm.0000000000004060.
Lorusso R, Gelsomino S, Parise O, et al. Neurologic injury in adults supported with veno-venous extracorporeal membrane oxygenation for respiratory failure: findings from the extracorporeal life support organization database. Crit Care Med. 2017;45(8):1389–97. https://doi.org/10.1097/ccm.0000000000002502.
Risnes I, Wagner K, Nome T, et al. Cerebral outcome in adult patients treated with extracorporeal membrane oxygenation. Ann Thorac Surg. 2006;81(4):1401–6. https://doi.org/10.1016/j.athoracsur.2005.10.008.
Acknowledgements
List of PELS Investigators: Giovanni Chiarini1, Silvia Mariani1,2, Bas C.T. van Bussel4, Samuel Heuts1, Michele Di Mauro1, Dominik Wiedemann5, Anne-Kristin Schaefer5, Luca Conci5, Diyar Saeed6, Jawad Khalil6, Sven Lehmann6, Matteo Pozzi7, Jean-Francois Obadia7, Antonio Loforte8,9, Luca Botta8, Davide Pacini8, Udo Boeken10, Nikolaos Kalampokas10, Robertas Samalavicius11, Agne Jankuviene11, Karl Bounader12, Erwan Flecher12, Xiaotong Hou13, Jeroen J.H. Bunge14,15, Dinis Dos Reis Miranda15, Hergen Buscher16, Kogulan Sriranjan16, Leonardo Salazar17, Bart Meyns18, Daniel Herr19, Michael A Mazzeffi19, Sacha Matteucc20, Marco Di Eusanio20, Sandro Sponga21, Igor Vendramin21, Graeme MacLaren22, Vitaly Sorokin22, Kollengode Ramanathan22, Claudio Russo23, Alessandro Costetti23, Francesco Formica2,24, Pranya Sakiyalak25, Antonio Fiore26, Daniele Camboni27, Chistof Schmid27, Giuseppe Maria Raffa28, Rodrigo Diaz29, Roberto Castillo29, I-wen Wang30, Jae-Seung Jung31, Jan Belohlavek32, Tomas Grus33, Vin Pellegrino34, Giacomo Bianchi35, Marco Solinas35, Matteo Pettinari36, Alessandro Barbone37, José P. Garcia38, Kiran Shekar39, Glenn Whitman40, Roberto Lorusso1.
1Cardio-Thoracic Surgery Department, and Cardiovascular Research Institute Maastricht, Maastricht, The Netherlands. 2Cardiac Surgery Unit, San Gerardo Hospital, Monza, Italy 3Universidade de Pernambuco, Pernambuco, Brazil. 4Department of Intensive Care Medicine, and Cardiovascular Research Institute Maastricht, Maastricht, The Netherlands. 5Department of Cardiac Surgery, Medical University of Vienna, Vienna, Austria 6Department of Cardiac Surgery, Leipzig Heart Center, Leipzig, Germany 7Department of Cardiac Surgery, Louis Pradel Cardiologic Hospital, Lyon, France 8Division of Cardiac Surgery, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy. 9University of Turin, Turin, Italy 10Department of Cardiac Surgery, Medical Faculty, Heinrich Heine University, Duesseldorf, Germany. 11II Department of Anesthesiology, Centre of Anesthesia, Intensive Care and Pain management, Vilnius University Hospital Santariskiu Klinikos, Vilnius, Lithuania. 12Division of Cardiothoracic and Vascular Surgery. Pontchaillou University Hospital, Rennes, France. 13Center for Cardiac Intensive Care, Beijing Institute of Heart, Lung, and Blood Vessels Diseases, Beijing Anzhen Hospital, Capital Medical University, Beijing, China. 14Department of cardiology, Erasmus MC, Rotterdam, The Netherlands. 15Department of Intensive Care Adults, Erasmus MC, Rotterdam, The Netherlands. 16Department of Intensive Care Medicine, Center of Applied Medical Research, St Vincent's Hospital, Darlinghurst, NSW, Australia. 17Department of Cardiology, Fundación Cardiovascular de Colombia, Bucaramanga, Colombia. 18Department of Cardiac Surgery, University Hospitals Leuven and Department of Cardiovascular Sciences, University of Leuven, Leuven, Belgium. 19Departments of Medicine and Surgery, University of Maryland, Baltimore, USA. 20SOD Cardiochirurgia Ospedali Riuniti 'Umberto I - Lancisi - Salesi' Università Politecnica delle Marche, Ancona, Italy. 21Division of Cardiac Surgery, Cardiothoracic Department, University Hospital of Udine, Udine, Italy. 22Cardiothoracic Intensive Care Unit, National University Heart Centre, National University Hospital, Singapore, Singapore. 23Cardiac Surgery Unit, Cardiac Thoracic and Vascular Department, Niguarda Hospital, Milan, Italy. 24Department of Medicine and Surgery, University of Parma, Parma, Italy. 25Division of Cardiovascular and Thoracic Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. 26Department of Cardio-Thoracic Surgery, University Hospital Henri-Mondor, Créteil, Paris, France. 27Department of Cardiothoracic Surgery, University Medical Center Regensburg, Regensburg, Germany. 28Department for the Treatment and Study of Cardiothoracic Diseases and Cardiothoracic Transplantation, IRCCS-ISMETT (Istituto Mediterraneo per i Trapianti e Terapie ad Alta Specializzazione), Palermo, Italy. 29ECMO Unit, Departamento de Anestesia, Clínica Las Condes, Las Condes, Santiago, Chile. 30Division of Cardiac Surgery, Memorial Healthcare System, Hollywood, FL 33021, USA. 31Department of Thoracic and Cardiovascular Surgery, Korea University Anam Hospital, Seoul, South Korea. 322nd Department of Internal Medicine, Cardiovascular Medicine General Teaching Hospital and 1st Faculty of Medicine, Charles University in Prague, Prague, Czech Republic. 332nd Department of Cardiovascular Surgery, First Faculty of Medicine, Charles University and General University Hospital in Prague, Prague, Czech Republic. 34Intensive Care Unit, The Alfred Hospital, Melbourne, VIC, Australia. 35Ospedale del Cuore Fondazione Toscana "G. Monasterio", Massa, Italy. 36Department of Cardiovascular Surgery, Ziekenhuis Oost-Limburg, Genk, Belgium. 37Cardiac Surgery Unit, IRCCS Humanitas Research Hospital – Rozzano (MI) – Italy. 38IU Health Advanced Heart & Lung Care, Indiana University Methodist Hospital, Indianapolis, IN, USA. 39Adult Intensive Care Services, The Prince Charles Hospital, Brisbane, Australia. 40Cardiac Intensive Care Unit, Johns Hopkins Hospital, Baltimore, Maryland, USA.
Funding
No financial support for this study was provided.
Author information
Authors and Affiliations
Consortia
Contributions
GC, AS, SM, RL conceived and designed the study. GC and SM conceived and performed the analysis. GC, AS, SM, RL drafted the manuscript. All authors interpreted the results, critically edited the manuscript, approved the final work, and agreed to be accountable for the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board (IRB) approval was required for all centers, based on the IRB-approval of the coordinating center (MUMC + , number: METC-2018-0788, date: December 19th, 2018). The study was registered at ClinicalTrials.gov (trial registration ID: NCT03857217). Need for informed consent was waived based on the retrospective nature of the study, the emergency of the performed procedure, and the pseudonymization of shared data. The current study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
DW: consultant/proctor for Abbott; scientific advisor for Xenios. RL: consultant for Medtronic, Getinge and LivaNova; Advisory Board Member of Eurosets (honoraria paid as research funding). KR: received honoraria from Baxter and Fresenius Ltd for educational lectures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chiarini, G., Mariani, S., Schaefer, AK. et al. Neurologic complications in patients receiving aortic versus subclavian versus femoral arterial cannulation for post-cardiotomy extracorporeal life support: results of the PELS observational multicenter study. Crit Care 28, 265 (2024). https://doi.org/10.1186/s13054-024-05047-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-05047-2







