Abstract
Background
Re-intubation secondary to post-extubation respiratory failure in post-operative patients is associated with increased patient morbidity and mortality. Non-invasive respiratory support (NRS) alternative to conventional oxygen therapy (COT), i.e., high-flow nasal oxygen, continuous positive airway pressure, and non-invasive ventilation (NIV), has been proposed to prevent or treat post-extubation respiratory failure. Aim of the present study is assessing the effects of NRS application, compared to COT, on the re-intubation rate (primary outcome), and time to re-intubation, incidence of nosocomial pneumonia, patient discomfort, intensive care unit (ICU) and hospital length of stay, and mortality (secondary outcomes) in adult patients extubated after surgery.
Methods
A systematic review and network meta-analysis of randomized and non-randomized controlled trials. A search from Medline, Embase, Scopus, Cochrane Central Register of Controlled Trials, and Web of Science from inception until February 2, 2024 was performed.
Results
Thirty-three studies (11,292 patients) were included. Among all NRS modalities, only NIV reduced the re-intubation rate, compared to COT (odds ratio 0.49, 95% confidence interval 0.28; 0.87, p = 0.015, I2 = 60.5%, low certainty of evidence). In particular, this effect was observed in patients receiving NIV for treatment, while not for prevention, of post-extubation respiratory failure, and in patients at high, while not low, risk of post-extubation respiratory failure. NIV reduced the rate of nosocomial pneumonia, ICU length of stay, and ICU, hospital, and long-term mortality, while not worsening patient discomfort.
Conclusions
In post-operative patients receiving NRS after extubation, NIV reduced the rate of re-intubation, compared to COT, when used for treatment of post-extubation respiratory failure and in patients at high risk of post-extubation respiratory failure.
Similar content being viewed by others
Background
Re-intubation consequent to post-extubation respiratory failure in post-operative patients who underwent general anesthesia occurs in a relevant number of patients, i.e., 2.1% (range 0.2–33%) of 370,617 patients included in a recent meta-analysis [1]. The observed variability depends on a variety of factors including underlying disease, comorbidities, and type of surgery and anesthesia [1,2,3]. Post-operative re-intubation is associated with increased morbidity, mortality, and healthcare costs [3,4,5].
To prevent or treat post-extubation respiratory failure, forms of non-invasive respiratory support (NRS) alternative to conventional oxygen therapy (COT) have been proposed, i.e., high-flow nasal oxygen (HFNO), continuous positive airway pressure (CPAP), and bilevel non-invasive ventilation (NIV). These techniques aim at maintaining adequate gas exchanges, while reducing patient’s work of breathing [6, 7], and improving airway secretion clearance [8].
The 2017 European Respiratory Society (ERS)/American Thoracic Society (ATS) clinical practice guidelines recommend the use of NIV/CPAP, over COT, for both treating and preventing post-extubation respiratory failure after surgery (conditional recommendation, moderate certainty of evidence) [9]. Moreover, the 2022 ERS guidelines recommend the use of either COT or HFNO in post-operative patients at low risk of respiratory complications, and either HFNO or NIV in post-operative patients at high risk of respiratory complications (both conditional recommendations with low certainty of evidence) [10].
The aims of the present systematic review and network meta-analysis of randomized and non-randomized controlled trials are assessments of the effect of NRS application, as compared to COT, on the rate of re-intubation (primary outcome), and time to re-intubation, incidence of nosocomial pneumonia, patient discomfort, ICU and hospital length of stay, and ICU, hospital, and long-term mortality (secondary outcomes), in adult patients extubated after surgery. Additional subgroup analyses, for the rate of re-intubation only, aim to compare, as opposed to COT, the efficacy of NRS (1) for the prevention or treatment of post-operative respiratory failure after extubation; (2) for supra-diaphragmatic or infra-diaphragmatic surgery; (3) for patients at high or low risk of post-operative respiratory failure; and (4) for patients transferred to the intensive care unit (ICU) or out of the ICU, i.e., post-anesthesia care units or wards, after surgery.
Methods
Reporting of this systematic review and meta-analysis conforms to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) Statement extension for network meta-analysis (Additional file 1: Supplementary Digital Content [SDC] 1) [11]. The review protocol was registered in PROSPERO (CRD42022377859), an international prospective register of systematic reviews, on Dec 30, 2022.
Literature search
An electronic search of Medline, Embase, Scopus, Cochrane Central Register of Controlled Trials, and Web of Science from inception until February 2, 2024 was performed with no language restrictions. In addition, a research-in-progress database (ClinicalTrials.gov), grey literature (OpenGrey), and all references of included articles and related reviews and guidelines were searched. Abstracts and conference proceedings were excluded. Controlled vocabulary terms (when available), text words, and keywords were variably combined with blocks of terms per concept: (“non-invasive respiratory support”) AND (“extubation” OR “weaning”) AND (“surgery” OR “general anesthesia”). MEDLINE and Scopus search strategies were adapted for searches in other databases and are reported in SDC 2.
Study selection
All studies meeting the following Participants, Interventions, Comparisons, Outcomes, and Study design (PICOS) question were included: participants were adult patients admitted to ICU or non-ICU settings and extubated after surgery; the intervention was any NRS modality; the comparison was COT or another NRS modality; the primary outcome was all-cause re-intubation at any time-point, whereas the time to re-intubation, the incidence of nosocomial pneumonia and patient discomfort, ICU and hospital length of stay, and ICU, hospital, and long-term mortality were secondary outcomes; and eligible study designs were randomized controlled trials (RCTs) or non-randomized controlled studies. Studies not comparing at least two different NRS modalities or COT, studies investigating NRS or COT before surgery, and studies assessing NRS to facilitate early weaning from invasive mechanical ventilation were excluded. Moreover, studies exclusively on patients undergoing self-extubation or requiring palliative care and studies with cross-over design were omitted. Search results were merged and duplicate records of the same report were removed. The remaining studies were stored using Microsoft Excel software (Microsoft Corporation, Redmond, WA, USA).
Data collection
Eight researchers (EP, CP, TAG, SF, FMC, FM, GP, GC) were split into four couples, each analyzing the same number of overall identified citations. Specifically, each member of the couple independently screened the titles and abstracts of assigned papers and retrieved the full texts of potentially relevant reports. Reasons for exclusions were detailed and excluded full texts were listed (SDC 3). Eight researchers (MN, NC, CLT, VG, CSc, CSi, SC, FM) were split into four couples, each analyzing the same number of eligible full texts. Specifically, each member of the couple independently assessed the full text of the assigned papers. Data from included studies were recorded using a Microsoft Excel specific report form. Four researchers (TP, AB, NS, FZ) independently verified all extracted data for accuracy. Any disagreements on both study selection and data extraction were resolved by referral to other authors (ADC, PN), if necessary. The following information was collected: first author, year of the study, type of surgery, inclusion and exclusion criteria, patient age and gender, risk of post-operative respiratory failure, clinical setting, NRS application for prevention or treatment, and primary and secondary outcomes.
Quality and certainty of evidence assessment
Eight researchers (EP, CP, TAG, SF, FM, GP, CSc, CSi) were split into four couples and assessed the risk of bias of the same number of included studies. Specifically, each member of the couple independently evaluated the quality of included RCTs and non-RCTs by using the Risk of Bias (RoB) 2 and the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) assessment tools, respectively. The RoB2 examines five domains of bias: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. The study-level risk of bias is expressed on a three-grade scale, i.e., low risk of bias, high risk of bias or some concerns [12]. The ROBINS-I considers seven domains of bias: confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes, and selection of the reported result. The study-level risk of bias is described on a four-grade scale, i.e., low, moderate, serious, and critical risk of bias [13]. Disagreements were resolved by discussion with other authors (TP, PN), if necessary.
The Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach, addressing the domains of risk of bias, inconsistency, indirectness, publication bias, intransitivity, incoherence, and imprecision, was used to assess the certainty of evidence related to the each of the outcomes [14] Imprecision for each comparison was incorporated only at the network level, not at the level of the direct or indirect estimate. The most recent GRADE guidance on imprecision rating using a minimally contextualized approach was applied [15]. A partially contextualized approach was used to evaluate the magnitudes of the intervention effects [16].
Sensitivity analyses
For the primary outcome only, a pre-planned sensitivity analysis to assess the effect on study findings of excluding RCTs at high risk of bias and non-RCTs at serious or critical risk of bias was conducted. In addition, several post-hoc sensitivity analyses were performed to assess the robustness of results after (1) excluding those studies comparing COT with a sequential combination of NRS modalities, i.e., two NRS strategies applied in sequence; (2) considering only one NRS setting at a time in those studies investigating two different HFNO flow rates or two different NIV interfaces; (3) excluding those studies requiring the application of a continuity correction, in case no events were observed in the intervention groups (see paragraph 2.7 “Statistical Analysis”); and (4) considering in the same group those studies comparing either CPAP or NIV to COT.
Subgroup analyses
For the primary outcome only, pre-planned subgroup analyses were performed according to the following subgroups: (1) prophylactic NRS, i.e., applied immediately after extubation, versus therapeutic NRS, i.e., applied only after evidence of respiratory deterioration; (2) patients at high versus low risk of post-operative respiratory failure, as defined in the individual study; (3) studies including more than 90% of patients undergoing supra-diaphragmatic surgery versus studies including more than 90% of patients undergoing infra-diaphragmatic surgery; and (4) studies enrolling more than 90% of patients admitted to the ICU after surgery versus studies enrolling less than 10% of patients admitted to the ICU after surgery. Subgroup analyses were also performed after considering those studies comparing either CPAP or NIV to COT in the same group (see paragraph 2.5 “Sensitivity Analyses”).
Statistical analysis
Conventional pairwise meta-analyses were performed using a random-effects model to account for between-study heterogeneity [17]. The treatment effect for dichotomous outcomes was analyzed with the Mantel–Haenszel method and expressed as odds ratio (OR) with 95% confidence interval (CI). The treatment effect for continuous outcomes was analyzed with the inverse variance method and expressed as standardized mean difference (SMD) with 95% CI. Whenever necessary, we converted reported median and interquartile range to estimated mean and standard deviation (SD) using Wan’s method [18]. When no events were observed in any of the groups in an individual study, a fixed value of 1 was added as a continuity correction to the cells corresponding to the number of events [17]. Statistical heterogeneity for the outcomes among studies was assessed using the chi-squared test and I2 statistic. Heterogeneity was defined as follows: low for I2 < 25%, moderate for I2 25–50%, and high for I2 > 50% [17].
Availability of evidence, transitivity assumption, intra-network connectivity, and network coherence were considered to assess the feasibility of conducting a network meta-analysis [19]. The following variables were included as potential moderators in a Bayesian network meta-regression to evaluate whether the transitivity assumption was satisfied [20, 21]: prophylactic versus therapeutic NRS; patients at high versus low risk of post-operative respiratory failure; supra-diaphragmatic versus infra-diaphragmatic surgery; and ICU vs. non-ICU setting. Surface under the cumulative ranking curve (SUCRA) scatterplots indicating confidence rectangles were obtained to identify those treatment effects influenced by mediators [22]. Direct and indirect treatment estimates were compared to check for incoherence in the network meta-analyses [23].
We performed frequentist random-effects network meta-analyses [19]. The direct treatment estimates were based on the common between-study variance Tau2 from the network meta-analysis. The indirect estimates were obtained with the Separate Indirect from Direct Evidence and the Separate Indirect from Direct Design Evidence methods [19].
A ranking among treatments was performed based on the frequentist analogue of the SUCRA. The ranking was provided as p-scores, ranging from 0 (minimum) to 1 (maximum) and measuring the mean extent of certainty that a NRS modality is better than the competing modalities [19].
Publication bias was assessed by visually inspecting a funnel plot for potential asymmetry and Egger’s test was applied when more than 10 studies were available for a specific outcome [24].
All analyses were performed with Review Manager version 5.3 (Nordic Cochrane Centre, Cochrane Collaboration) and R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria) with the “netmeta” package for frequentist network meta-analyses and the “rnmamod” package for Bayesian network meta-regression. For all analyses, two-sided p values < 0.05 were considered significant.
Results
Study selection, characteristics, and quality
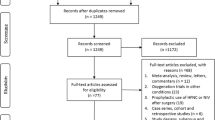
The study selection flow-chart is shown in Fig. 1.
We identified 4594 unique citations and assessed the full text of 73 articles for eligibility. Of these, 28 RCTs (9099 patients) [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52] and five non-RCTs (2193 patients) [53,54,55,56,57] were included in the systematic review.
The characteristics of the included studies are reported in SDC 4. Studies were published between 1997 and 2022. Study populations ranged from 20 to 4793 patients and 4285 (38%) subjects were females. Twenty-three studies (70%) were performed in the ICU, while three (9%) outside of the ICU, and 6 (18%) in a mixed setting. One study did not specify the clinical setting [32]. One study included 8% of patients admitted to the ward or high-dependency unit after surgery and was considered in the ICU group [25].
COT was administered in 5056 patients (45%), CPAP in 3130 (28%), NIV in 1814 (16%), and HFNO in 1292 (11%). NRS was used for prevention of post-operative respiratory failure after extubation in 20 studies (61%) and for treatment in 11 (33%). One study did not specify the indication for NRS [53] and another one included patients receiving either prophylactic or therapeutic NRS [45].
Only two studies (6%) investigated the use of a sequential combination of COT and CPAP [35, 51]. Therefore, these studies were not considered as a separate node of treatment. One study tested two different HFNO flow rates [46] and another tested two different NIV interfaces [49]. For two studies, the application of continuity correction was required [29, 48]. Twelve studies (36%), including 1613 patients (14%), compared COT to HFNO, 9 (27%), 5955 patients (53%), compared COT to CPAP, 9 (27%), 2574 patients (23%), compared COT to NIV, two (6%), 959 patients (8%), compared HFNO to NIV, and one (3%), 191 patients (2%), CPAP to NIV.
The risk of bias assessments are shown in Fig. 2 and SDC 5.
Risk of bias assessment figures for randomized (A) and non-randomized (B) controlled trials. For randomized controlled trials, green, yellow, and red circles indicate low risk of bias, some concerns, and high risk of bias, respectively. For non-randomized controlled trials, green, yellow, red, and grey circles indicate low, moderate, serious, and critical risk of bias, respectively
Among the RCTs, five studies (18%) were considered to be at high risk of bias, 16 (57%) arose some concerns, and 7 (25%) were considered to be at low risk of bias. Among the non-RCTs, three studies (60%) were considered at critical risk of bias, while two (40%) at serious risk of bias.
The presence of publication bias was strongly suspected from the visual inspection of the funnel plot for the following outcomes: nosocomial pneumonia, discomfort, ICU length of stay, and hospital length of stay (SDC 6). Egger’s test confirmed the occurrence of publication bias for nosocomial pneumonia (p = 0.021), ICU length of stay (p = 0.050), and hospital length of stay (p = 0.042).
As described in SDC7, SUCRA scatterplots indicated an overall consistency of the NMA with respect to the considered mediators. Only NIV treatment indicated a potential inconsistency, i.e., 50% relative overestimation when accounting for the mediation effect of prophylactic respiratory support.
As reported in SDC 8, from the comparison of direct and indirect evidence of the impact of the interventions on primary and secondary outcomes, no serious incoherence was detected.
GRADE assessment is reported in SDC 9. Overall, the certainty of evidence was rated down to low or very low for most outcomes and comparisons because of concerns related to risk of bias, publication bias, and imprecision.
Primary and secondary outcomes
Eighteen studies reported on the incidence of nosocomial pneumonia, 9 on discomfort, 22 and 18 on ICU and hospital length of stay, respectively, 7 and 20 on ICU and hospital mortality, respectively, and 5 on long-term mortality. Since only one study provided data on the timing of re-intubation, this variable could not be included in the meta-analyses.
Table 1 details network estimates evaluating the impact of the interventions on primary and secondary outcomes in the overall patient population. Figure 3 depicts the forest plots for primary and secondary outcomes in the overall patient population. Forest plots of pairwise comparisons of the effect of non-invasive respiratory support on the primary outcome are reported in SDC 10. SDC 11 depicts network diagrams for primary and secondary outcomes in the overall patient population. SDC 12 reports network estimates evaluating the impact of the interventions on the primary outcome in sensitivity analyses and patient subgroups. SDC 13 details the p-scores of the interventions for primary and secondary outcomes in the overall patient population, in sensitivity analyses, and in patient subgroups.
Forest plots of the effect of non-invasive respiratory support on primary and secondary outcomes. Abbreviations: COT conventional oxygen therapy; NRS non-invasive respiratory support; OR odds ratio; CI confidence interval; CPAP continuous positive airway pressure; NIV non-invasive ventilation; HFNO high-flow nasal oxygen; ICU intensive care unit; SMD standardized mean difference
As detailed in Table 1 and Fig. 3, only NIV reduced the rate of re-intubation, compared to COT (OR 0.49, 95% CI 0.28; 0.87, p = 0.015, I2 = 60.5%, low certainty of evidence). No differences were found between HFNO and CPAP, HFNO and NIV, and CPAP and NIV.
As depicted in Fig. 3, compared to COT, (1) only NIV was associated with a lower rate of nosocomial pneumonia (OR 0.55, 95% CI 0.33; 0.90, p = 0.019, I2 = 31%, low certainty of evidence); (2) both CPAP (SMD − 1.39, 95% CI − 2.04; − 0.73, p < 0.001, I2 = 84.1%, very low certainty of evidence) and NIV (SMD − 0.78, 95% CI − 1.49; − 0.06, p = 0.033, I2 = 84.1%, very low certainty of evidence) were associated with a shorter ICU length of stay, while only CPAP (SMD − 2.58, 95% CI − 3.99; − 1.17, p < 0.001, I2 = 92.7%, very low certainty) reduced hospital length of stay; and 3) only NIV reduced ICU (OR 0.39, 95% CI 0.17; 0.90, p = 0.027, I2 = 0%, moderate certainty of evidence), hospital (OR 0.51, 95% CI 0.34; 0.74, p = 0.001, I2 = 0%, low certainty of evidence), and long-term mortality (OR 0.56, 95% CI 0.32; 0.97, p = 0.039, I2 = 0%, moderate certainty of evidence). Finally, patient discomfort was similar for all interventions.
Sensitivity analyses
As reported in Additional file 1: Supplementary Table 9 in SDC 12, compared to COT, the application of NIV significantly reduced the rate of re-intubation also when excluding (1) RCTs at high risk of bias and non-RCTs at serious or critical risk of bias; (2) studies investigating a sequential combination of NRS modalities; and (3) studies requiring the application of continuity correction. Moreover, considering only one setting in one study investigating two different HFNO flow rates and in another one using two different NIV interfaces did not change the results relative to the primary outcome.
None of the other NRS modalities were found to significantly reduce the risk of re-intubation, when compared to COT, after the performance of sensitivity analyses.
Finally, considering in the same group those studies comparing either CPAP or NIV to COT identified a significant association between the application of CPAP/NIV, compared to COT, and the rate of re-intubation (OR 0.50, 95% CI 0.32–0.78, p = 0.003, I2 = 61.3%).
Subgroup analyses
As shown in Additional file 1: Supplementary Table 10 and Supplementary Fig. 3 in SDC 12, compared with COT, NIV was effective in reducing the risk of re-intubation only when applied for treatment (OR 0.23, 95% CI 0.09; 0.58, p = 0.002, I2 = 70.2%) and in high-risk patients (OR 0.36, 95% CI 0.14; 0.93, p = 0.034, I2 = 51.3%). This effect of NIV was observed only in patients admitted to the ICU (OR 0.48, 95% CI 0.25; 0.91, p = 0.024, I2 = 68.8%). Notably, however, no study has investigated the effect of NIV outside of the ICU. No difference in the risk of re-intubation was observed between any NRS modality and COT in supra-diaphragmatic versus infra-diaphragmatic surgery.
As reported in Additional file 1: Supplementary Table 11 and Supplementary Fig. 4 in SDC 12, subgroup analyses performed after the inclusion of those studies comparing either CPAP or NIV to COT in the same group identified a significant association of the application of CPAP/NIV, compared to COT, with a reduced rate of re-intubation only when used as treatment (OR 0.25, 95% CI 0.11; 0.60, p = 0.002, I2 = 70.1%), in the ICU (OR 0.45, 95% CI 0.24; 0.82, p = 0.009, I2 = 69.2%), and in both patients at high (OR 0.39, 95% CI 0.17; 0.90, p = 0.027, I2 = 45.2%) and low (OR 0.53, 95% CI 0.30; 0.96, p = 0.035, I2 = 68.2%) risk of post-operative respiratory failure.
Discussion
This systematic review and network meta-analysis including 11,292 adult patients from 33 studies found that in post-operative patients receiving NRS after extubation for post-extubation respiratory failure, the risk of re-intubation was significantly reduced by NIV, as opposed to COT. In particular, this effect was observed in the following subgroups: (1) patients receiving NIV for treatment, while not for prevention, of post- extubation respiratory failure, (2) patients at high, while not low, risk of post-operative respiratory failure, (3) and ICU patients (no data available for out-of-ICU patients). In addition, in the overall patient population, NIV reduced the rate of nosocomial pneumonia, ICU length of stay, and ICU, hospital, and long-term mortality. Moreover, compared to COT, NIV did not worsen patient discomfort. Neither HFNO nor CPAP, compared to COT, significantly improved outcomes, except for the reduction in the ICU and hospital length of stay conferred by CPAP.
The 2022 ERS clinical practice guidelines on the application of HFNO in acute respiratory failure suggest the use of either COT or HFNO in post-operative patients at low risk of respiratory complications [10]. Our data confirm that COT and HFNO were equally effective in reducing the rate of re-intubation in low-risk patients and we also found CPAP and NIV, when considered separately, not to confer any improvement, compared to COT, in this patient subgroup. The same guidelines suggest, based on a single RCT not considering COT [45], that HFNO and NIV are equally effective in patients at high risk of respiratory complications [10]. Our data confirm this indication, since HFNO and NIV resulted in similar re-intubation rates in high-risk patients. Nonetheless, our network meta-analysis compared COT to each of the three NRS modalities and revealed that only NIV significantly decreased the rate of re-intubation in this subgroup of post-operative patients.
The 2017 ERS/ATS clinical practice guidelines on the application of NIV/CPAP for acute respiratory failure suggest the use of NIV/CPAP, rather than COT, for treating or preventing post-operative acute respiratory failure because of the improvement in the rate of re-intubation, nosocomial pneumonia, and mortality [9]. Furthermore, the 2020 European Society of Anesthesiology (ESA) and European Society of Intensive Care Medicine (ESICM) guidelines indicate either NIV or CPAP, over COT, to prevent re-intubation (weak recommendation, moderate certainty of evidence) and nosocomial pneumonia (weak recommendation, high‐quality evidence) and NIV rather than COT (weak recommendation, low certainty of evidence) to reduce mortality in the peri‐operative/peri-procedural hypoxemic patient [58]. Our results are in keeping with these indications in the general post-operative patient population. Noteworthy, however, in the present study only NIV was effective, compared to COT, in reducing the rate of re-intubation, nosocomial pneumonia, and mortality in the overall patient population, while CPAP only reduced ICU and hospital length of stay.
The 2017 ERS/ATS guidelines also suggest NIV should not be used for treatment of established post-extubation respiratory failure in unselected critically ill patients [9]. This recommendation does not appear to be in keeping with our results. Worth reminding, however, quite few post-operative patients, i.e., 50 patients (17% of the overall population) from two studies [59, 60], were included in the analysis leading to that guideline statement, while our network meta-analysis included data from 11,292 post-operative patients. It is important to note that atelectasis is the most frequent pulmonary complication after general anesthesia [61], occurring in approximately 90% of patients intraoperatively and potentially persisting for several days after abdominal surgery [62]. The mechanisms contributing to post-operative atelectasis [63] are readily reversible by the application of NIV [6], which explains the benefit provided by NIV observed in our study. This hypothesis is consistent with previous studies showing NIV to be effective, compared to standard treatment, when used immediately after early extubation in surgical patients with the purpose of shortening the duration of invasive mechanical ventilation [64].
Our results are in keeping with a network meta-analysis, overall including nine RCTs and 1865 patients at high-risk for or with established postoperative respiratory failure, concluding that, in comparison with COT, NIV/CPAP is associated with reduced re-intubation and mortality, while HFNO was associated with reduced re-intubation only [65]. Different from this previous study, however, we separated the effects of NIV and CPAP and included a much larger patient cohort.
A recent network meta-analysis including unselected critically ill patients found, in a subgroup of 2259 post-surgical patients, that, compared to COT, NIV/CPAP, combining both the prophylactic and therapeutic use, reduced the rate of re-intubation, while HFNO did not [66]. Our sensitivity analysis considering either CPAP or NIV, as opposed to COT, confirmed these findings in a much larger patient population (8529 patients). When considering CPAP and NIV separately, however, only NIV was beneficial.
The results of our sensitivity analysis are in accordance with those of a recent meta-analysis, including 5614 patients from four studies considering only upper abdominal surgery, which reported that post-operative prophylactic NIV/CPAP does not reduce the rate of re-intubation [67]. Nonetheless, our study also demonstrated that NIV/CPAP reduces the risk of re-intubation when used for the treatment of overt post-extubation respiratory failure.
In a recent network meta-analysis including only RCTs performed in the ICU, we found that prophylactic HFNO, while not NIV/CPAP, reduced the rate of re-intubation, as opposed to COT, in a subgroup of 544 post-operative patients from 5 RCTs [68]. Worth remarking, however, in the present work we also included non-RCTs, and out-of-ICU studies, overall resulting in 11,292 patients from 33 investigations, which definitely explains the different findings of the two network meta-analyses.
Finally, another recent meta-analysis, including 38 RCTs (9782 patients), did not report preventative post-operative non-invasive respiratory support, overall including CPAP, NIV, and HFNO, to reduce the occurrence of re-intubation, compared with usual care [69]. Notwithstanding, we considered NRS strategies separately and also included non-RCTs.
Our study has some strengths, including the use of a reproducible and comprehensive literature search strategy, comprising clinical trials and grey literature, the duplicate independent citation review, data extraction, and quality assessment, the inclusion of a large number of patients from different countries, the use of Bayesian network meta-regression to test several covariates as potential effect modifiers, and the use of multiple sensitivity analyses to assess the robustness of our results. Several limitations must also be mentioned. First, studies investigating the occurrence of all-cause re-intubation at any point during hospital stay were included, given the lack of a universally accepted definition for the timing of extubation failure. Therefore, we could not differentiate among different etiologies of respiratory failure following post-operative extubation. Second, intransitivity may have arisen from the inclusion of studies published over a 25 years period [19]; nonetheless, we did not detect significant intransitivity during our GRADE assessment. Third, low or very low certainty of evidence was attributed to most outcomes and comparisons, thus limiting the confidence in our findings. Indeed, some outcomes were characterized by high heterogeneity, possibly related to different outcome definitions among studies, variable criteria for re-intubation, and heterogeneous clinical settings and patient populations. For example, the results on patient comfort were rather surprising and need to be confirmed by further studies. Notwithstanding, our subgroup analyses partially explained this heterogeneity, indicating the scenarios where NRS may be of greater benefit over COT, while our network meta-regression did not identify further relevant sources of heterogeneity. Fourth, only nine of the included studies (27%) enrolled more than 100 patients per group, potentially introducing small-study effect biases [24]. Fifth, patients were classified at high risk of post-operative respiratory failure as defined in the original studies, in the absence of a universally applicable definition. Sixth, the inclusion of non-randomized trials may increase the risk of bias and violate the exchangeability assumption of network meta-analyses [70]. However, non-randomized studies complement some of the limitations of RCTs, increasing the generalizability of the findings, and improving network density [70]. Finally, multiple subgroup and sensitivity analyses increased the chance of type 1 error [71].
Conclusions
In patients extubated after surgery and receiving NRS, compared to COT, only NIV reduced the rate of re-intubation and nosocomial pneumonia, and improved hospital and long-term mortality, without worsening patient discomfort. In contrast, CPAP and HFNO did not significantly improve outcomes. Therapeutic, while not prophylactic, NIV decreased the rate of re-intubation and NIV was beneficial in patients at high, rather than low, risk of post-operative respiratory failure.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NRS:
-
Non-invasive respiratory support
- COT:
-
Conventional oxygen therapy
- HFNO:
-
High-flow nasal oxygen
- CPAP:
-
Continuous positive airway pressure
- NIV:
-
Non-invasive ventilation
- ERS:
-
European respiratory society
- ATS:
-
American thoracic society
- ICU:
-
Intensive care unit
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
- SDC:
-
Supplementary digital content
- PICOS:
-
Participants, interventions, comparisons, outcomes, and study design
- RCT:
-
Randomized controlled trials
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SMD:
-
Standardized mean difference
- MD:
-
Mean difference
- SUCRA:
-
Surface under the cumulative ranking curve
- RoB:
-
Risk of bias
- ROBINS-I:
-
Risk of bias in non-randomized studies of interventions
References
Xie Z, Liu J, Yang Z, Tang L, Wang S, Du Y, et al. Risk factors for post-operative planned reintubation in patients after general anesthesia: a systematic review and meta-analysis. Front Med. 2022;9:839070. https://doi.org/10.3389/fmed.2022.839070.
Rujirojindakul P, Geater AF, McNeil EB, Vasinanukorn P, Prathep S, Asim W, et al. Risk factors for reintubation in the post-anaesthetic care unit: a case–control study. Br J Anaesth. 2012;109:636–42. https://doi.org/10.1093/bja/aes226.
Acheampong D, Guerrier S, Lavarias V, Pechman D, Mills C, Inabnet W, et al. Unplanned postoperative reintubation following general and vascular surgical procedures: outcomes and risk factors. Ann Med Surg. 2018;33:40–3. https://doi.org/10.1016/j.amsu.2018.08.013.
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–7. https://doi.org/10.1016/j.jamcollsurg.2004.05.276.
Ramachandran SK, Nafiu OO, Ghaferi A, Tremper KK, Shanks A, Kheterpal S. Independent predictors and outcomes of unanticipated early postoperative tracheal intubation after nonemergent, noncardiac surgery. Anesthesiology. 2011;115:44–53. https://doi.org/10.1097/ALN.0b013e31821cf6de.
Jaber S, Chanques G, Jung B, Riou B. Postoperative noninvasive ventilation. Anesthesiology. 2010;112:453–61. https://doi.org/10.1097/ALN.0b013e3181c5e5f2.
D’Cruz RF, Hart N, Kaltsakas G. High-flow therapy: physiological effects and clinical applications. Breathe. 2020;16:200224. https://doi.org/10.1183/20734735.0224-2020.
Chidekel A, Zhu Y, Wang J, Mosko JJ, Rodriguez E, Shaffer TH. The effects of gas humidification with high-flow nasal cannula on cultured human airway epithelial cells. Pulm Med. 2012;2012:1–8. https://doi.org/10.1155/2012/380686.
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426. https://doi.org/10.1183/13993003.02426-2016.
Oczkowski S, Ergan B, Bos L, Chatwin M, Ferrer M, Gregoretti C, et al. ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure. Eur Respir J. 2022;59:2101574. https://doi.org/10.1183/13993003.01574-2021.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. https://doi.org/10.7326/M14-2385.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019. https://doi.org/10.1136/bmj.l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016. https://doi.org/10.1136/bmj.i4919.
Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630–g5630. https://doi.org/10.1136/bmj.g5630.
Zeng L, Brignardello-Petersen R, Hultcrantz M, Mustafa RA, Murad MH, Iorio A, et al. GRADE guidance 34: update on rating imprecision using a minimally contextualized approach. J Clin Epidemiol. 2022;150:216–24. https://doi.org/10.1016/j.jclinepi.2022.07.014.
Brignardello-Petersen R, Izcovich A, Rochwerg B, Florez ID, Hazlewood G, Alhazanni W, et al. GRADE approach to drawing conclusions from a network meta-analysis using a partially contextualised framework. BMJ. 2020. https://doi.org/10.1136/bmj.m3907.
Deeks JJ, Higgins JPT, Altman DG (editors). Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al., editors. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook. Accessed 11 Apr 2023.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G. Undertaking network meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al., editors. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook. Accessed 11 Apr 2023.
Cooper NJ, Sutton AJ, Morris D, Ades AE, Welton NJ. Addressing between-study heterogeneity and inconsistency in mixed treatment comparisons: application to stroke prevention treatments in individuals with non-rheumatic atrial fibrillation. Stat Med. 2009;28:1861–81. https://doi.org/10.1002/sim.3594.
Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Mak. 2013;33:641–56. https://doi.org/10.1177/0272989X12455847.
Salanti G, Ades AE, Ioannidis JPA. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–71. https://doi.org/10.1016/j.jclinepi.2010.03.016.
Brignardello-Petersen R, Mustafa RA, Siemieniuk RAC, Murad MH, Agoritsas T, Izcovich A, GRADE Working Group, et al. GRADE approach to rate the certainty from a network meta-analysis: addressing incoherence. J Clin Epidemiol. 2019;108:77–85. https://doi.org/10.1016/j.jclinepi.2018.11.025.
Page MJ, Higgins JPT, Sterne JAC. Assessing risk of bias due to missing results in a synthesis. In: Higgins JPT, Thomas J, Chandler J, et al., editors. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook. Accessed 11 Apr 2023.
Abrard S, Rineau E, Seegers V, Lebrec N, Sargentini C, Jeanneteau A, et al. Postoperative prophylactic intermittent noninvasive ventilation versus usual postoperative care for patients at high risk of pulmonary complications: a multicentre randomised trial. Br J Anaesth. 2023;130:e160–8. https://doi.org/10.1016/j.bja.2021.11.033.
Antonelli M, Conti G, Bufi M, Costa MG, Lappa A, Rocco M, et al. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA. 2000;283:235. https://doi.org/10.1001/jama.283.2.235.
Auriant I, Jallot A, Hervé P, Cerrina J, Le Roy LF, Fournier JL, et al. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med. 2001;164:1231–5. https://doi.org/10.1164/ajrccm.164.7.2101089.
Böhner H, Kindgen-Milles D, Grust A, Buhl R, Lillotte W-C, Müller BT, et al. Prophylactic nasal continuous positive airway pressure after major vascular surgery: results of a prospective randomized trial. Langenbeck’s Arch Surg. 2002;387:21–6. https://doi.org/10.1007/s00423-002-0281-2.
Burra V, Putta G, Prasad S, Manjunath V. A prospective study on use of thrive (transnasal humidified rapid insufflation ventilatory exchange) versus conventional nasal oxygenation following extubation of adult cardiac surgical patients. Ann Card Anaesth. 2021;24:353. https://doi.org/10.4103/aca.ACA_16_20.
Corley A, Bull T, Spooner AJ, Barnett AG, Fraser JF. Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI ≥30: a randomised controlled trial. Intensive Care Med. 2015;41:887–94. https://doi.org/10.1007/s00134-015-3765-6.
Futier E, Paugam-Burtz C, Godet T, Khoy-Ear L, Rozencwajg S, OPERA study investigators, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA). Intensive Care Med. 2016;42:1888–98. https://doi.org/10.1007/s00134-016-4594-y.
Gupta SD, Pareek A, Ghose T, Sarkar UK, Mukherjee S, Goswani A, et al. Management of postoperative hypoxaemia in patients following upper abdominal laparoscopic surgery - a comparative study. Indian J Anaesth. 2008;52:185–90.
Hewidy AA, Suliman LA, El Hefnawy E, Hassan AA. Immediate continuous positive airway pressure (CPAP) therapy after sleeve gastrectomy. Egypt J Chest Dis Tuberc. 2016;65:701–6. https://doi.org/10.1016/j.ejcdt.2016.01.012.
Jaber S, Lescot T, Futier E, Paugam-Burtz C, Seguin P, Ferrandiere M, et al. Effect of noninvasive ventilation on tracheal reintubation among patients with hypoxemic respiratory failure following abdominal surgery: a randomized clinical trial. JAMA. 2016;315:1345. https://doi.org/10.1001/jama.2016.2706.
Kindgen-Milles D, Müller E, Buhl R, Böhner H, Ritter D, Sandmann W, et al. Nasal-continuous positive airway pressure reduces pulmonary morbidity and length of hospital stay following thoracoabdominal aortic surgery. Chest. 2005;128:821–8. https://doi.org/10.1378/chest.128.2.821.
Lockstone J, Parry SM, Denehy L, Robertson IK, Story D, Boden I. Non-invasive positive airway pressure therapy to reduce postoperative lung complications following upper abdominal surgery (NIPPER PLUS): a pilot randomised control trial. Physiotherapy. 2022;117:25–34. https://doi.org/10.1016/j.physio.2022.06.001.
Mazullo Filho JBR, Bonfim VJG, Aquim EE. Noninvasive mechanical ventilation in immediate postoperative cardiac surgery patients. Rev Bras Ter Intensiva. 2010;22:363–8.
Olper L, Bignami E, Di Prima AL, Albini S, Nascimbene S, Cabrini L, et al. Continuous positive airway pressure versus oxygen therapy in the cardiac surgical ward: a randomized trial. J Cardiothorac Vasc Anesth. 2017;31:115–21. https://doi.org/10.1053/j.jvca.2016.08.007.
Parke R, McGuinness S, Dixon R, Jull A. Open-label, phase II study of routine high-flow nasal oxygen therapy in cardiac surgical patients. Br J Anaesth. 2013;111:925–31. https://doi.org/10.1093/bja/aet262.
Pennisi MA, Bello G, Congedo MT, Montini L, Nachira D, Ferretti GM, et al. Early nasal high-flow versus Venturi mask oxygen therapy after lung resection: a randomized trial. Crit Care. 2019;23:68. https://doi.org/10.1186/s13054-019-2361-5.
Pearse R, Ranieri M, Abbott T, Pakats M-L, Piervincenzi E, Patel A, et al. Postoperative continuous positive airway pressure to prevent pneumonia, re-intubation, and death after major abdominal surgery (PRISM): a multicentre, open-label, randomised, phase 3 trial. Lancet Respir Med. 2021;9:1221–30. https://doi.org/10.1016/S2213-2600(21)00089-8.
Sahin M, El H, Akkoç I. Comparison of mask oxygen therapy and high-flow oxygen therapy after cardiopulmonary bypass in obese patients. Can Respir J. 2018;2018:1–7. https://doi.org/10.1155/2018/1039635.
Soliman HAZ, Fikry DM, El-Attar AM, El Hadidy MS. High flow nasal cannula effect on pulmonary complications after major elective upper abdominal surgeries: a randomized control study. Egypt J Anaest. 2022;38:656–64.
Squadrone V, Coha M, Cerutti E, Schellino MM, Biolino P, Occella P, et al. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA. 2005;293:589. https://doi.org/10.1001/jama.293.5.589.
Stéphan F, Barrucand B, Petit P, Rézaiguia-Delclaux S, Médard A, Delannoy B, et al. High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA. 2015;313:2331. https://doi.org/10.1001/jama.2015.5213.
Theologou S, Ischaki E, Zakynthinos SG, Charitos C, Michopanou N, Patsatzis S, et al. High flow oxygen therapy at two initial flow settings versus conventional oxygen therapy in cardiac surgery patients with postextubation hypoxemia: a single-center, unblinded, randomized, controlled trial. J Clin Med. 2021;10:2079. https://doi.org/10.3390/jcm10102079.
Vourc’h M, Nicolet J, Volteau C, Caubert L, Chabbert C, Lepoivre T, et al. High-flow therapy by nasal cannulae versus high-flow face mask in severe hypoxemia after cardiac surgery: a single-center randomized controlled study - the heart flow study. J Cardiothorac Vasc Anesth. 2020;34:157–65. https://doi.org/10.1053/j.jvca.2019.05.039.
Wong DT, Adly E, Ip HYV, Thapar S, Maxted GR, Chung FF. A comparison between the Boussignac™ continuous positive airway pressure mask and the venturi mask in terms of improvement in the PaO2/FiO2 ratio in morbidly obese patients undergoing bariatric surgery: a randomized controlled trial. Can J Anesth J Can Anesth. 2011;58:532–9. https://doi.org/10.1007/s12630-011-9497-3.
Yang Y, Liu N, Sun L, Zhou Y, Yang Y, Shang W, et al. Noninvasive positive-pressure ventilation in treatment of hypoxemia after extubation following type-a aortic dissection. J Cardiothorac Vasc Anesth. 2016;30:1539–44. https://doi.org/10.1053/j.jvca.2016.03.129.
Yu Y, Qian X, Liu C, Zhu C. Effect of high-flow nasal cannula versus conventional oxygen therapy for patients with thoracoscopic lobectomy after extubation. Can Respir J. 2017;2017:1–8. https://doi.org/10.1155/2017/7894631.
Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications. Chest. 2009;135:1252–9. https://doi.org/10.1378/chest.08-1602.
Zhu GF, Wang DJ, Liu S, Jia M, Jia SJ. Efficacy and safety of noninvasive positive pressure ventilation in the treatment of acute respiratory failure after cardiac surgery. Chin Med J. 2013;126:4463–9.
Ishikawa S, Ohtaki A, Takahashi T, Koyano T, Hasegawa Y, Ohki S, et al. Noninvasive nasal mask bipap management for prolonged respiratory failure following cardiovascular surgery. J Cardiac Surg. 1997;12:176–9. https://doi.org/10.1111/j.1540-8191.1997.tb00119.x.
Kurt M, Boeken U, Litmathe J, Feindt P, Gams E. Oxygenation failure after cardiac surgery: early re-intubation versus treatment by nasal continuous positive airway pressure (NCPAP) or non-invasive positive pressure ventilation (NPPV). Monaldi Arch Chest Dis. 2016. https://doi.org/10.4081/monaldi.2008.425.
Melton N, Lazar JF, Childers WK, Anderson D, Jaik NP, Loran DB, et al. Preventing respiratory failure after cardiac surgery using post-extubation bilevel positive airway pressure therapy. Cureus. 2019. https://doi.org/10.7759/cureus.4236.
Xia M, Li W, Yao J, Jin Y, Du G, Xu Q, et al. A postoperative comparison of high-flow nasal cannula therapy and conventional oxygen therapy for esophageal cancer patients. Ann Palliat Med. 2021;10:2530–9. https://doi.org/10.21037/apm-20-1539.
Yan C, Zhang J, Wu Y, Yao J, Li J, Zhang X, et al. Effect of high-flow nasal cannula for hypoxemia following sun’s procedure in acute aortic dissection type A patients. Front Surg. 2021;8:630624. https://doi.org/10.3389/fsurg.2021.630624.
Leone M, Einav S, Chiumello D, Constantin J-M, De Robertis E, De Gama AM, et al. Guideline contributors. Noninvasive respiratory support in the hypoxaemic peri-operative/periprocedural patient: a joint ESA/ESICM guideline. Intensive Care Med. 2020;46:697–713. https://doi.org/10.1007/s00134-020-05948-0.
Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguía C, González M, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452–60. https://doi.org/10.1056/NEJMoa032736.
Keenan SP, Powers C, McCormack DG, Block G. Noninvasive positive-pressure ventilation for postextubation respiratory distress: a randomized controlled trial. JAMA. 2002;287:3238. https://doi.org/10.1001/jama.287.24.3238.
Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat MS, Rajesh PB, et al. Postoperative pulmonary complications following thoracic surgery: Are there any modifiable risk factors? Thorax. 2010;65:815–8. https://doi.org/10.1136/thx.2009.123083.
Hedenstierna G. Alveolar collapse and closure of airways: regular effects of anaesthesia. Clin Physio Funct Imaging. 2003;23:123–9. https://doi.org/10.1046/j.1475-097X.2003.00483.x.
Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118:317–34. https://doi.org/10.1093/bja/aex002.
Vaschetto R, Longhini F, Persona P, Ori C, Stefani G, Liu S, et al. Early extubation followed by immediate noninvasive ventilation vs. standard extubation in hypoxemic patients: a randomized clinical trial. Intensive Care Med. 2019;45:62–71. https://doi.org/10.1007/s00134-018-5478-0.
Zayed Y, Kheiri B, Barbarawi M, Rashdan L, Gakhal I, Ismail E, et al. Effect of oxygenation modalities among patients with postoperative respiratory failure: a pairwise and network meta-analysis of randomized controlled trials. J Intensive Care. 2020;8:51. https://doi.org/10.1186/s40560-020-00468-x.
Fernando SM, Tran A, Sadeghirad B, Burns KEA, Fan E, Brodie D, et al. Noninvasive respiratory support following extubation in critically ill adults: a systematic review and network meta-analysis. Intensive Care Med. 2022;48:137–47. https://doi.org/10.1007/s00134-021-06581-1.
Lockstone J, Denehy L, Truong D, Whish-Wilson GA, Boden I, Abo S, et al. Prophylactic postoperative noninvasive ventilation in adults undergoing upper abdominal surgery: a systematic review and meta-analysis. Crit Care Med. 2022;50:1522–32. https://doi.org/10.1097/CCM.0000000000005628.
Boscolo A, Pettenuzzo T, Sella N, Zatta M, Salvagno M, Tassone M, et al. Noninvasive respiratory support after extubation: a systematic review and network meta-analysis. Eur Respir Rev. 2023;32:220196. https://doi.org/10.1183/16000617.0196-2022.
Hui S, Fowler AJ, Cashmore RMJ, Fisher TJ, Schlautmann J, Body S, et al. Routine postoperative noninvasive respiratory support and pneumonia after elective surgery: a systematic review and meta-analysis of randomised trials. Br J Anaesth. 2022;128:363–74. https://doi.org/10.1016/j.bja.2021.10.047.
Cameron C, Fireman B, Hutton B, Clifford T, Coyle D, Wells G, et al. Network meta-analysis incorporating randomized controlled trials and non-randomized comparative cohort studies for assessing the safety and effectiveness of medical treatments: challenges and opportunities. Syst Rev. 2015;4:147. https://doi.org/10.1186/s13643-015-0133-0.
Mascha EJ. Alpha, beta, meta: guidelines for assessing power and type I error in meta-analyses. Anesth Analg. 2015;121:1430–3. https://doi.org/10.1213/ANE.0000000000000993.
Acknowledgements
The authors are grateful to Prof. Dario Gregori and Dr. Giulia Lorenzoni, affiliated with the Unit of Biostatistics, Epidemiology, and Public Health of the University of Padua, Italy, for their support in the statistical analysis.
Funding
Open access funding provided by Università degli Studi di Padova.
Author information
Authors and Affiliations
Contributions
TP, AB, PN: conception and design of the study. TP, AB, EP, CP, TAG, SF, FMC, FM, GP, GC, MN, NC, CLT, VG, CSc, CSi, SC, FM, FZ, NS, ADC: acquisition of data, analysis and interpretation of data. PN: interpretation of data. TP, AB, PN: drafting the article. All authors: revising the article critically for important intellectual content. All authors: final approval of the version to be submitted. All authors: agreement to be accountable for all aspects of the research and manuscript. All authors: ensuring that questions related to the accuracy or integrity of any part of the research and manuscript, even ones in which the author was not personally involved, are appropriately investigated, resolved, and communicated (where needed).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Prof. Navalesi’s research lab has received grants/research equipment from Draeger, Intersurgical SPA, and Gilead. Prof. Navalesi receives royalties from Intersurgical SPA for the Helmet Next invention. He has also received speaking fees from Getinge, Mindray, Intersurgical SPA, Gilead, GSK and Draeger. Dr. Zarantonello and Dr. Sella received payments for lecturing from Getinge. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary digital content.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pettenuzzo, T., Boscolo, A., Pistollato, E. et al. Effects of non-invasive respiratory support in post-operative patients: a systematic review and network meta-analysis. Crit Care 28, 152 (2024). https://doi.org/10.1186/s13054-024-04924-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04924-0