Abstract
Background
Both critically ill patients with coronavirus disease 2019 (COVID-19) and patients receiving extracorporeal membrane oxygenation (ECMO) support exhibit a high incidence of healthcare-associated infections (HAI). However, data on incidence, microbiology, resistance patterns, and the impact of HAI on outcomes in patients receiving ECMO for severe COVID-19 remain limited. We aimed to report HAI incidence and microbiology in patients receiving ECMO for severe COVID-19 and to evaluate the impact of ECMO-associated infections (ECMO-AI) on in-hospital mortality.
Methods
For this study, we analyzed data from 701 patients included in the ECMOSARS registry which included COVID-19 patients supported by ECMO in France.
Results
Among 602 analyzed patients for whom HAI and hospital mortality data were available, 214 (36%) had ECMO-AI, resulting in an incidence rate of 27 ECMO-AI per 1000 ECMO days at risk. Of these, 154 patients had bloodstream infection (BSI) and 117 patients had ventilator-associated pneumonia (VAP). The responsible microorganisms were Enterobacteriaceae (34% for BSI and 48% for VAP), Enterococcus species (25% and 6%, respectively) and non-fermenting Gram-negative bacilli (13% and 20%, respectively). Fungal infections were also observed (10% for BSI and 3% for VAP), as were multidrug-resistant organisms (21% and 15%, respectively). Using a Cox multistate model, ECMO-AI were not found associated with hospital death (HR = 1.00 95% CI [0.79–1.26], p = 0.986).
Conclusions
In a nationwide cohort of COVID-19 patients receiving ECMO support, we observed a high incidence of ECMO-AI. ECMO-AI were not found associated with hospital death.
Trial registration number NCT04397588 (May 21, 2020).
Similar content being viewed by others
Background
Healthcare-associated infections (HAI) are frequent in patients receiving extracorporeal membrane oxygenation (ECMO) support [1, 2]. Likewise, critically ill patients with coronavirus disease 2019 (COVID-19) have a higher incidence of HAI compared to non-COVID-19 critically ill patients or those admitted to intensive care unit (ICU) before the pandemic[3,4,5]. Both ECMO support and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) induce immune alterations that may increase the susceptibility to HAI [6, 7]. A recent European multicenter study reported high incidences of ventilator-associated pneumonia (VAP) and bloodstream infections (BSI) in COVID-19 patients on ECMO [8]. Yet, data on microbiology, resistance patterns, and its impact on the outcomes in patients receiving ECMO for severe COVID-19 remain limited [9]. The primary objective of this prospective multicenter cohort study was to report the incidence and microbiology of HAI in patients receiving ECMO for severe COVID-19. The secondary objective was to evaluate the impact of ECMO associated infections (ECMO-AI) on patient outcomes. We hypothesized that the incidence of ECMO-AI would be high and associated with worse outcomes in patients receiving ECMO for severe COVID-19.
Methods
Data collection
The French national Extracorporeal Membrane Oxygenation for Respiratory Failure and/or Heart failure related to Severe Acute Respiratory Syndrome-Coronavirus 2 (ECMOSARS) registry recruited all COVID-19 patients supported by ECMO (Veno-Venous (VV) or Veno-Arterial (VA)) between April 2020 and March 2022 (ClinicalTrials.gov Identifier: NCT04397588) [10]. The registry has been approved by the university hospital of Rennes ethics committee (n° 20.43). According to the French legislation, written consent was waived because of the observational design of the study that does not imply any modification of existing diagnostic or therapeutic strategies. After information, only non-opposition of patients or their legal representative was obtained for use of the data. The data collection methodology has been previously reported [10,11,12]. Briefly, data were collected by research assistants from each patient’s medical record using an electronic case report form. Automatic checks were generated for missing or incoherent data, and additional consistency tests were performed by data managers. Collected data included patient characteristics and comorbidities, management of COVID-related acute respiratory distress syndrome before ECMO cannulation, patient characteristics at ECMO cannulation and the day after, therapeutics, complications and patient outcomes on ECMO. Patient and ECMO management was at the discretion of each center (see Additional file 1: Table S1 for the definition of the main variables). The strategies for HAI prevention were left to the discretion of each ICU. Center experience was classified in two groups according to their experience in ECMO management before the pandemic: centers that managed more than 30 ECMO patients (≥ 30) annually were considered high volume, and those that managed fewer than 30 ECMO patients (< 30) annually were considered low volume [13].
Outcomes
Our primary outcome was HAI incidence while on ECMO (ECMO-AI). Secondary outcomes were incidences of VAP and BSI, ECMO-AI microbiology and antimicrobial resistance, ECMO-free days within 90 days of cannulation, ventilatory-free days within 90 days of cannulation, and in-hospital death.
Definitions
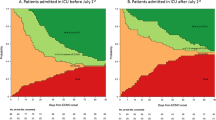
ECMO-AI included both VAP and BSI. An infection was classified as ECMO-AI if it developed during the ECMO run, was diagnosed 48 h or more after ICU admission and was not incubating upon admission. Diagnosis was made by treating physician. Within each subtype of ECMO-AI (VAP or BSI), only the first event was recorded. BSI was defined by a positive blood culture occurring 48 h or more after admission. For common skin contaminants, confirmation required two positive blood cultures drawn from separate puncture site [14]. The diagnosis of VAP was considered in patients ventilated for 48 h or more, and up to 48 h after extubation. The criteria for the diagnosis of VAP followed the current French guidelines [15]. Microorganisms identified as the cause of infection were categorized as multidrug-resistant organisms (MDRO) based on the European Society of Clinical Microbiology and Infectious Disease definition [16]. The first epidemic wave (up to July 1st, 2020) was distinguished from the subsequent waves (from July 1st, 2020, to March 31, 2022).
Study design and population
For the present study, we analyzed all consecutive patients included in the registry with available data on acquired infections and hospital mortality. The analysis followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Statistical analysis
A statistical analysis plan was made prior to accessing the data. No a priori statistical power calculation was conducted. Categorical variables were expressed as number (percentage) and continuous variables as median and interquartile range. When appropriate, the chi-square test and the Fisher’s exact test were used to compare categorical variables. The Mann–Whitney U test and the Wilcoxon test were used to compare continuous variables. Multiple imputations were used to replace missing data. Missing data were assumed to be missing at random and were dealt using “MICE” R package using Monte Carlo Markov chained equations to generate a dataset without missing values. The variable selected to predict missing values was those available before exposure to the risk of HAI (outcome variables not included). To evaluate the association between ECMO-AI and in-hospital mortality, we performed survival analyses using a multivariable proportional Cox model. Given that ECMO-AI developed during follow-up and was not present at cannulation, a multistate model was constructed [17]. As a result, patients who developed an ECMO-AI were included twice. First, they were included in the group without ECMO-AI from cannulation to the onset of ECMO-AI. Then, they were censored from this group and included in the ECMO-AI group from the onset of ECMO-AI to discharge or death. Confounders entered in the multivariable model were defined a priori based on the existing ECMO and COVID-19 literature. All confounders that are associated with both ECMO-AI and death were included in the multivariable analysis. The set of potential confounders sufficient for adjustment was: center case volume, epidemic wave (first vs subsequent), age, diabetes, chronic respiratory failure, chronic kidney disease, malignancy (solid cancer or hemopathy), use of steroids before ECMO, use of non-steroidal anti-inflammatory drugs before ECMO, septic shock, antibiotic before cannulation, selective digestive decontamination, SOFA score at cannulation, type of ECMO support (VA vs VV), delay from hospitalization to ECMO cannulation. All tests were two-sided, and p < 0.05 was considered statistically significant.
Results
Study population
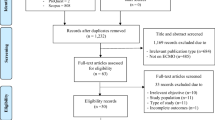
Among the 47 participating ICUs, 701 patients were included in 41 ICUs in the registry at the time of database lock. Of these, 6 patients had missing data concerning ECMO-AI and an additional 93 had missing survival data, leaving a total of 602 patients available for analysis (Fig. 1). Most patients (73%) were admitted during first epidemic wave (Table 1). The median age was 55 (46–61) years. Patients were intubated for a median of 5 (2–8) days before cannulation, 541/599 patients (90%) underwent prone positioning and 565/595 patients (95%) received neuromuscular blocking agents before cannulation. The median PaO2/FiO2 ratio before cannulation was 63 (54–77) mmHg. Additionally, 432/477 (91%) received antibiotics before ECMO initiation and 15 (2%) received selective digestive decontamination before ECMO initiation in 4 ICUs. Most ECMO were veno-venous (550/602, 91%). Superior–inferior vena cava was the most common site of cannulation (515/602, 86%), mostly through femoro-jugular access (493/602, 82%).
ECMO-associated infections
Overall, 214/602 patients (36%) experienced at least one ECMO-AI event. The incidence rate of ECMO-AI was 27 per 1000 ECMO days at risk (Fig. 2). VAP was diagnosed in 117 patients (incidence rate of 12 per 1000 ECMO days at risk) and BSI in 154 patients (incidence rate of 15 per 1000 ECMO days at risk). Additionally, 57/214 (27%) patients presented with both VAP and BSI. The time from cannulation to ECMO-AI was notably shorter for BSI compared to VAP, with medians of 4 (0–9) days and 5 (2–11) days, respectively (p = 0.017). The causative microorganisms are reported by infection site in Table 2 and Additional file 1: Figure S1. The main causative agents were Enterobacteriaceae (34% for BSI and 48% for VAP), Enterococcus species (25% and 6%, respectively) and non-fermenting Gram-negative bacilli (13% and 20%, respectively). Fungal infections were also noteworthy, with incidences of 10% for BSI and 3% for VAP. MDRO accounted for 21% and 15% of infections for BSI and VAP, respectively. The proportion of extended-spectrum beta-lactamase (ESBL) was 4% and 7%, respectively, and the proportion of methicillin-resistant Staphylococcus aureus (MRSA) was 3% and 3% respectively.
Outcomes
Crude mortality by microorganism and by infection site is reported in Table 2. The highest mortality rates were observed in patients with non-fermenting Gram-negative bacilli infection (79%) and with Enterococcus species infection (63%). Patients with ECMO-AI had longer ECMO support with a median of 16 (10–27) days, compared to 11 (5–19) days for those without ECMO-AI (p < 0.001) (Additional file 1: Table S2). Further analysis using a Cox multistate model (Additional file 1: Table S3) did not find an association between ECMO-AI and hospital death (HR = 1.00 95% CI [0.79–1.26], p = 0.986).
Sensitivity analyses
We conducted a sensitivity analysis in which only ECMO-AI that developed after 48 h of ECMO run were considered. Patients with ECMO run < 48 h were excluded. We found that 157/546 patients (29%) acquired an ECMO-AI corresponding to an incidence rate of 21 ECMO-AI per 1000 ECMO-days. Outcomes were similar to those reported when considering the complete ECMO run (Additional file 1: Table S4). We also explored the potential for different patterns of early vs late ECMO-AI. We compared early (≤ 5 days from cannulation) and delayed (> 5 days from cannulation) ECMO-AI. Interestingly, there were no differences in microbiology nor in outcomes with respect for ECMO-AI timing (Additional file 1: Tables S5 and S6).
Discussion
This study reported the incidence of ECMO-AI (defined as VAP and BSI during ECMO support) at a nationwide level in a large multicenter cohort of COVID-19 patients supported by ECMO. The main results were as follows. First, the incidence of ECMO-AI was high in this population, with 36% of patients and a rate of 27 ECMO-AI per 1000 ECMO days. Second, Enterobacteriaceae emerged as the main causative microorganisms. Third, we found a high incidence of Enterococcus spp. in BSI. Fourth, the incidence of MRSA and ESBL was low in our cohort. Finally, ECMO-AI were not associated with in-hospital death after multivariable analysis.
The incidence of ECMO-AI is highly variable across published observational studies, including the ELSO registry, ranging from to 9 to 65% [18]. Several factors contribute to this variability: the specific types of HAI considered in the analysis, the definitions employed and the underlying indications for ECMO. Diagnosing HAI on ECMO can be challenging, especially for cannulation site or catheter-associated urinary tract infections. Furthermore, distinguishing between colonization and infection may not always be definitive. Moreover, the mortality attributable to some infections, such as catheter-associated urinary tract infections, might be close to zero [19]. Consequently, the present study focused on the most common ECMO-AI, BSI and VAP, both of which have been shown to be associated with poorer outcomes in critically ill patients [20].
Regarding microbiology, we report here the most extensive description to date of the micro-organisms responsible for ECMO-AI. As observed in previous ECMO case series and in other critical-care settings, Enterobacteriaceae were the main causative microorganisms, found in a third of BSI and almost half of VAP [1, 14, 21, 22]. Enterobacteriaceae also predominated in VAP and BSI in critically COVID-19 patients [2, 3, 5]. Similarly, non-fermenting Gram-negative bacilli were highly represented in VAP (20%) in our cohort, in line with previous publications involving both COVID-19 and non-COVID-19 critically ill patients [1,2,3,4,5].
Strikingly, a high proportion of Enterococcus spp. were reported in BSI cases (25%), which was unexpected. Recently, the international EUROBACT-2 study, encompassing 2,927 hospital-acquired BSI episodes in non-COVID-19 patients, reported 314 Enterococcus spp. infections (11%), much lower than observed in the present study. Regarding non-COVID-19 ECMO patients, previous case series also reported lower proportions of Enterococcus spp. BSI, ranging from 15 to 20% [1, 22]. Several factors may explain this difference. First, Enterococcus spp. was frequently identified in BSI cases in COVID-19 patients, such as reported in Spain (30%), in Italy (25%) or in France (15%) (2, 4, 23). In our cohort, the majority of critically ill COVID-19 patients received antimicrobial agents at admission, primarily cephalosporins, which may have promoted Enterococcus spp. proliferation and subsequent translocation [23, 24]. Furthermore, cross-transmission of Enterococcus spp. has been frequently observed, especially in high-activity ICUs as observed during the pandemic [25]. Notably, this microorganism was only identified in a few cases (6%) of VAP. The implications of Enterococcus respiratory colonization, or even infection, remain controversial, and identification in respiratory sample is usually dismissed as contamination. Finally, MDRO were identified in nearly 20% of ECMO-AI in our cohort, with low levels of MRSA or ESBL. The EUROBACT-2 study reported a similar 22% rate of difficult-to-treat Gram-negative bacteria. However, in this study, the prevalence of resistant Gram-positive bacteria was higher at 37%, compared to 3% in our study [14]. For critically ill COVID-19 patients, another large French cohort reported higher prevalence of MDRO with up to 30% resistance to 3rd Generation Cephalosporin and 17% of ESBL in Enterobacteriaceae and 11% of MRSA [4]. Similarly, an European cohort of COVID-19 critically ill patients found high rates of MDR [26].
Interestingly, we found a high incidence of fungal infection in our population, a proportion much higher than previously described in non-COVID-19 ECMO patients [27].
ECMO-AI were not found associated with mortality in our cohort, in line with previous study which reported that HAI do not modify outcome in the most severe patients such as those with ECMO support [28]. Interestingly, ECMO-AI were associated with length of ECMO support, length of mechanical ventilation and length of ICU stay in bivariate analysis. This is likely related in part to the duration of exposure, i.e., longer ECMO exposure creates more opportunities for ECMO-AI. The other potential effect is that ECMO-AI may delay decannulation or extubation and prolong ICU stays.
Our study has several strengths. First, our cohort is one of the largest samples of COVID-19 patients supported by ECMO, providing detailed microbiological data on ECMO-HAI. Second, the participating centers cover a majority of the available ECMO sites in France. Third, the multicenter design facilitates the generalizability of our findings. Finally, the database's quality was regularly assessed by dedicated data managers.
However, there are limitations to consider. Despite wide representation, not all French ECMO centers were included, potentially introducing selection bias. Further, being an observational study, this study might be subject to information bias. The absence of specific HAI prevention recommendations might result in variations in the prevention practice across the ICUs. Additionally, as mentioned above, we focused on VAP and BSI and we do not provide information on catheter-related urinary tract infections or cannulation site infections. Moreover, the source of BSI was not recorded in our database. As both ECMO cannulation itself and patient illness severity at cannulation contribute to the development of ECMO-AI, we classified as ECMO-AI any infection occurring during the entire ECMO run. However, alternative definitions exist in the literature, which consider different exposure periods for ECMO-AI [29]. Finally, most of our patients (75%) were included during the first wave of the pandemic in a context of work overload and bed shortage which may have resulted in difficulties to maintain adequate preventive measures.
Conclusions
In conclusion, our study demonstrated a high incidence of ECMO-AI in a nationwide multicenter cohort of patients with severe COVID-19 supported with ECMO. Enterobacteriaceae were the main causative microorganisms, with low rates of ESBL and MRSA. ECMO-AI were not found associated with in-hospital mortality.
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- BSI:
-
Bloodstream Infections
- BMI:
-
Body mass index
- COVID-19:
-
Coronavirus disease 2019
- ESBL:
-
Extended-spectrum beta-lactamase
- ECMO:
-
Extracorporeal membrane oxygenation
- ECMO-AI:
-
ECMO-associated infections
- HAI:
-
Healthcare associated infections
- IRR:
-
Incidence rate ratio
- MDRO:
-
Multidrug-resistant organisms
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SOFA:
-
Sequential organ failure assessment
- VAP:
-
Ventilator-associated pneumonia
- VA-ECMO:
-
Veno-arterial ECMO
- VV-ECMO:
-
Veno-venous ECMO
References
Schmidt M, Bréchot N, Hariri S, Guiguet M, Luyt CE, Makri R, et al. Nosocomial Infections in adult cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation. Clin Infect Dis. 2012;55:1633–41.
Grasselli G, Scaravilli V, Bella SD, Biffi S, Bombino M, Patroniti N, et al. Nosocomial infections during extracorporeal membrane oxygenation. Crit Care Med. 2017;45:1726–33.
Vacheron C-H, Lepape A, Savey A, Machut A, Timsit JF, Vanhems P, et al. Increased incidence of ventilator-acquired pneumonia in coronavirus disease 2019 patients: a multicentric cohort study*. Crit Care Med. 2022;50:449–59.
Lepape A, Machut A, Bretonnière C, Friggeri A, Vacheron C-H, Savey A, et al. Effect of SARS-CoV-2 infection and pandemic period on healthcare-associated infections acquired in intensive care units. Clin Microbiol Infect. 2023;29:530–6.
Rouzé A, Martin-Loeches I, Povoa P, Makris D, Artigas A, Bouchereau M, et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intensiv Care Med. 2021;47:188–98.
Frerou A, Lesouhaitier M, Gregoire M, Uhel F, Gacouin A, Reizine F, et al. Venoarterial extracorporeal membrane oxygenation induces early immune alterations. Crit Care. 2021;25:9.
Reizine F, Lesouhaitier M, Gregoire M, Pinceaux K, Gacouin A, Maamar A, et al. SARS-CoV-2-Induced ARDS associates with MDSC expansion, lymphocyte dysfunction, and arginine shortage. J Clin Immunol. 2021;41:515–25.
Schmidt M, Hajage D, Landoll M, Pequignot B, Langouet E, Amalric M, et al. Comparative outcomes of extracorporeal membrane oxygenation for COVID-19 delivered in experienced European centres during successive SARS-CoV-2 variant outbreaks (ECMO-SURGES): an international, multicentre, retrospective cohort study. Lancet Respir Med. 2023;11:163–75.
Luyt C-E, Sahnoun T, Gautier M, Vidal P, Burrel S, de Chambrun MP, et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: a retrospective cohort study. Ann Intensiv Care. 2020;10:158.
Nesseler N, Fadel G, Mansour A, Para M, Falcoz P-E, Mongardon N, et al. Extracorporeal membrane oxygenation for respiratory failure related to COVID-19: a nationwide cohort study. Anesthesiology. 2022;136:732–48.
Massart N, Guervilly C, Mansour A, Porto A, Flécher E, Esvan M, et al. Impact of prone position in COVID-19 patients on extracorporeal membrane oxygenation*. Crit Care Med. 2023;51:36–46.
Mansour A, Flecher E, Schmidt M, Rozec B, Gouin-Thibault I, Esvan M, et al. Bleeding and thrombotic events in patients with severe COVID-19 supported with extracorporeal membrane oxygenation: a nationwide cohort study. Intensiv Care Med. 2022;48:1039–52.
Lebreton G, Schmidt M, Ponnaiah M, Folliguet T, Para M, Guihaire J, et al. Extracorporeal membrane oxygenation network organisation and clinical outcomes during the COVID-19 pandemic in Greater Paris, France: a multicentre cohort study. Lancet Respir Med. 2021;9:851–62.
Tabah A, Koulenti D, Laupland K, Misset B, Valles J, de Carvalho FB, et al. Characteristics and determinants of outcome of hospital-acquired bloodstream infections in intensive care units: the EUROBACT international cohort study. Intensiv Care Med. 2012;38:1930–45.
Leone M, Bouadma L, Bouhemad B, Brissaud O, Dauger S, Gibot S, et al. Hospital-acquired pneumonia in ICU. Anaesth Crit Care Pain Med. 2018;37:83–98.
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Escolano S, Golmard J, Korinek A, Mallet A. A multi-state model for evolution of intensive care unit patients: prediction of nosocomial infections and deaths. Stat Med. 2000;19:3465–82.
Abrams D, Grasselli G, Schmidt M, Mueller T, Brodie D. ECLS-associated infections in adults: what we know and what we don’t yet know. Intensiv Care Med. 2020;46:182–91.
Clec’h C, Schwebel C, Français A, Toledano D, Fosse J-P, Garrouste-Orgeas M, et al. Does catheter-associated urinary tract infection increase mortality in critically patient? Infect Control Hosp Epidemiology. 2007;28:1367–73.
Lambert M-L, Suetens C, Savey A, Palomar M, Hiesmayr M, Morales I, et al. Clinical outcomes of health-care-associated infections and antimicrobial resistance in patients admitted to European intensive-care units: a cohort study. Lancet Infect Dis. 2011;11:30–8.
Martin-Loeches I, Povoa P, Rodríguez A, Curcio D, Suarez D, Mira J-P, et al. Incidence and prognosis of ventilator-associated tracheobronchitis (TAVeM): a multicentre, prospective, observational study. Lancet Respir Med. 2015;3:859–68.
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ, et al. Infections acquired by adults who receive extracorporeal membrane oxygenation risk factors and outcome. Infect Control Hosp Epidemiology. 2013;34:24–30.
Bonten MJ, Gaillard CA, van Tiel FH, van der Geest S, Stobberingh EE. Colonization and infection with Enterococcus faecalis in intensive care units: the role of antimicrobial agents. Antimicrob Agents Chemother. 1995;39:2783–6.
Pultz NJ, Stiefel U, Subramanyan S, Helfand MS, Donskey CJ. Mechanisms by which anaerobic microbiota inhibit the establishment in mice of intestinal colonization by vancomycin-resistant enterococcus. J Infect Dis. 2005;191:949–56.
Lund B, Agvald-Öhman C, Hultberg A, Edlund C. Frequent transmission of enterococcal strains between mechanically ventilated patients treated at an intensive care unit. J Clin Microbiol. 2002;40:2084–8.
Abelenda-Alonso G, Rombauts A, Gudiol C, Oriol I, Simonetti A, Coloma A, et al. Immunomodulatory therapy, risk factors and outcomes of hospital-acquired bloodstream infection in patients with severe COVID-19 pneumonia: a Spanish case–control matched multicentre study (BACTCOVID). Clin Microbiol Infect. 2021;27:1685–92.
de Roux Q, Botterel F, Lepeule R, Taccone FS, Langeron O, Mongardon N. Candida bloodstream infection under veno-arterial ECMO therapy. Crit Care. 2019;23:314.
Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13:665–71.
Peña-López Y, Machado MC, Rello J. Infection in ECMO patients: changes in epidemiology, diagnosis and prevention. Anaesth Crit Care Pain Med. 2024;43: 101319.
Acknowledgements
The ECMOSARS registry has been endorsed by the French society of thoracic and cardio-vascular surgery (Société Française de Chirurgie Thoracique et Cardio-Vasculaire, SFCTCV), the French society of thoracic and cardio-vascular critical care and anesthesia (Anesthésie-Réanimation Coeur-Thorax-Vaisseaux, ARCOTHOVA) and the French society of anesthesiology and critical care medicine (Société Française d’Anesthésie-Réanimation, SFAR) research network. ECMOSARS investigators: Olivier Fouquet M.D., Ph.D., University Hospital of Angers, Professor, collected data, provided and cared for study patients. Marc Pierrot, M.D., University Hospital of Angers, collected data, provided and cared for study patients. Sidney Chocron, M.D., Ph.D., University Hospital of Besançon, Professor, collected data, provided and cared for study patients. Guillaume Flicoteaux, M.D., University Hospital of Besançon, collected data, provided and cared for study patients. Philippe Mauriat, M.D., University Hospital of Bordeaux, critically reviewed the study proposal. Alexandre Ouattara, M.D., Ph.D., University Hospital of Bordeaux, collected data, provided and cared for study patients. Hadrien Roze, M.D., University Hospital of Bordeaux, collected data, provided and cared for study patients. Olivier Huet, M.D., Ph.D., University Hospital of Brest, Professor, collected data, provided and cared for study patients. Marc-Olivier Fischer, M.D., Ph.D., University Hospital of Caen, Professor, collected data, provided and cared for study patients. Claire Alessandri, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Raphel Bellaïche M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Ophélie Constant, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Quentin De Roux, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. André LY, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Arnaud Meffert, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Jean-Claude MERLE, M.D., APHP University Hospital Henri Mondor, Créteil. provided and cared for study patients. Lucile Picard, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Elena Skripkina, M.D, APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Thierry Folliguet, M.D., Ph.D., APHP University Hospital Henri Mondor, Créteil, Professor, provided and cared for study patients. Antonio Fiore, M.D., APHP University Hospital Henri Mondor, Créteil, provided and cared for study patients. Nicolas D'ostrevy, M.D., University Hospital of Clermont-Ferrand, collected data, provided and cared for study patients. Marie-Catherine Morgan, M.D., University Hospital of Dijon, collected data, provided and cared for study patients. Maxime Nguyen, M.D., University Hospital of Dijon, collected data, provided and cared for study patients. Nicolas Terzi, M.D., Ph.D., University Hospital of Grenoble, Professor, collected data, provided and cared for study patients. Dr Gwenhaël Colin, Vendée Hospital, La Roche-sur-Yon, collected data, provided and cared for study patients. Olivier Fabre, Hospital of Lens, collected data, provided and cared for study patients. Arash Astaneh, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Justin Issard, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Elie Fadel, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, collected data, provided and cared for study patients. Dominique Fabre, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Antoine GIRAULT, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Julien Guihaire, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Iolande Ion, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Jean Baptiste Menager, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Delphine Mitilian, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Olaf Mercier, M.D., Ph.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, collected data, provided and cared for study patients. François Stephan, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, Professor, collected data, provided and cared for study patients. Jacques Thes, M.D., Marie-Lannelongue Hospital, Le Plessis-Robinson, collected data, provided and cared for study patients. Jerôme Jouan, M.D., University Hospital of Limoges, collected data, provided and cared for study patients. Thibault Duburcq, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Valentin Loobuyck, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Mouhammed Moussa, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Sabrina Manganiello, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Agnes Mugnier, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Natacha Rousse, M.D., University Hospital of Lille, collected data, provided and cared for study patients. Olivier Desebbe, M.D., Clinique de la Sauvegarde, Lyon, collected data, provided and cared for study patients. Jean-Luc Fellahi, M.D., Ph.D., Hospices civils de Lyon, Professor, critically reviewed the study proposal, provided and cared for study patients. Roland Henaine, M.D., Ph.D., Hospices civils de Lyon, Professor, critically reviewed the study proposal, provided and cared for study patients. Matteo Pozzi, M.D, Hospices civils de Lyon, collected data, provided and cared for study patients. Jean-Christophe RICHARD, M.D., Ph.D., Hospices civils de Lyon, Professor, collected data, provided and cared for study patients, Zakaria Riad, M.D., Hospices civils de Lyon, collected data, provided and cared for study patients. Christophe Guervilly, M.D., North Hospital, APHM, Marseille, collected data, provided and cared for study patients. Sami Hraiech, M.D., North Hospital, APHM, Marseille, collected data, provided and cared for study patients. Laurent Papazian, M.D., Ph.D., North Hospital, APHM, Marseille, Professor, collected data, provided and cared for study patients. Matthias Castanier, M.D., European Hospital, Marseille, collected data, provided and cared for study patients. Charles Chanavaz, M.D., Clairval Hospital, Marseille, collected data, provided and cared for study patients. Cyril Cadoz, M.D., Regional Hospital of Metz-Thionville, provided and cared for study patients. Sebastien Gette, M.D., Regional Hospital of Metz-Thionville, provided and cared for study patients. Guillaume Louis, M.D., Regional Hospital of Metz-Thionville, provided and cared for study patients. Erick Portocarrero, M.D., Regional Hospital of Metz-Thionville, provided and cared for study patients. Philippe Gaudard, M.D., Ph.D, Univeristy Hospiyal of Montpellier, collected data, provided and cared for study patients. Kais Brini, M.D., Institut Mutualiste Montsouris, Paris, collected data, provided and cared for study patients. Nicolas Bischoff, M.D., Emile Muller Hospital, Mulhouse, collected data, provided and cared for study patients. Antoine Kimmoun, M.D., Ph.D., University Hospital of Nancy, Professor, collected data, provided and cared for study patients. Bruno Levy, M.D., Ph.D., University Hospital of Nancy, Professor, collected data, provided and cared for study patients. Mathieu MATTEI, M.D., University Hospital of Nancy, collected data, provided and cared for study patients. Pierre Perez, M.D., University Hospital of Nancy, collected data, provided and cared for study patients. Alexandre Bourdiol, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Yannick Hourmant, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Pierre-Joachim Mahé, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Bertrand Rozec, M.D., Ph.D., University Hospital of Nantes, collected data, provided and cared for study patients. Mickaël Vourc’h, M.D., University Hospital of Nantes, collected data, provided and cared for study patients. Stéphane Aubert, M.D., Ambroise Paré Hospital, Neuilly-sur-Seine, collected data, provided and cared for study patients. Florian Bazalgette, M.D., University hospital of Nîmes, collected data, provided and cared for study patients. Claire Roger, M.D., University hospital of Nîmes, collected data, provided and cared for study patients. Pierre Jaquet, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Brice Lortat-Jacob, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Pierre Mordant, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Patrick Nataf, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Juliette Patrier, M.D., Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Sophie Provenchere, M.D., Ph.D., Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Morgan Roué, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Romain Sonneville, M.D., Ph.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, Professor, provided and cared for study patients. Alexy Tran-Dinh, M.D., Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Paul-Henri Wicky, M.D., APHP, Hôpital Bichat-Claude Bernard, Paris University Hospital, provided and cared for study patients. Charles Al Zreibi, M.D., APHP Hôpital Européen Georges Pompidou—Paris University Hospital, collected data, provided and cared for study patients. Bernard Cholley, M.D., Ph.D., APHP Hôpital Européen Georges Pompidou—Paris University Hospital, Professor, collected data, provided and cared for study patients. Yannis Guyonvarch, M.D., APHP Hôpital Européen Georges Pompidou—Paris University Hospital, collected data, provided and cared for study patients. Sophie Hamada, M.D., APHP Hôpital Européen Georges Pompidou—Paris University Hospital, collected data, provided and cared for study patients. Claudio Barbanti, M.D., APHP Necker, Paris University Hospital, collected data, provided and cared for study patients. Astrid Bertier, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital, collected data, provided and cared for study patients. Anatole Harrois, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital, collected data, provided and cared for study patients. Jordi Matiello, M.D., APHP Le Kremlin-Bicêtre, Paris University Hospital, collected data, provided and cared for study patients. Thomas Kerforne, M.D., University Hospital of Poitiers, collected data, provided and cared for study patients. Corentin Lacroix, M.D., University Hospital of Poitiers, collected data, provided and cared for study patients. Nicolas Brechot, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Alain Combes, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Juliette Chommeloux, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Jean Michel Constantin, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Cosimo D’alessandro, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Pierre Demondion, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Alexandre Demoule, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Martin Dres, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Guillaume Fadel, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Muriel Fartoukh, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Guillaume Hekimian, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Charles Juvin, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Pascal Leprince, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. David Levy, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Charles Edouard Luyt, M.D., Ph.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, Professor, collected data, provided and cared for study patients. Marc PINETON DE CHAMBRUN, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Thibaut Schoell, M.D., APHP, Sorbonne Université, Hôpital Pitié–Salpêtrière, Paris, France, collected data, provided and cared for study patients. Pierre Fillâtre, M.D., Ph.D., Hospital of Saint-Brieuc, Collected data, provided and cared for study patients. Nicolas Massart, M.D., Hospital of Saint-Brieuc, Collected data, provided and cared for study patients. Roxane NICOLAS, M.D., University Hospital of Saint-Etienne, collected data, provided and cared for study patients. Maud Jonas, M.D., Saint-Nazaire Hospital, collected data, provided and cared for study patients. Charles VIDAL, M.D., University Hospital of Saint-Denis, La Réunion, collected data, provided and cared for study patients. Nicolas Allou, M.D., University Hospital of Saint-Denis, La Réunion, collected data, provided and cared for study patients, Salvatore Muccio, M.D., University Hospital of Reims, collected data, provided and cared for study patients. Dario Di Perna, M.D., University Hospital of Reims, collected data, provided and cared for study patients. Vito-Giovanni Ruggieri, M.D., Ph.D., University Hospital of Reims, collected data, provided and cared for study patients. Bruno Mourvillier, M.D., Ph.D., University Hospital of Reims, Professor, collected data, provided and cared for study patients. Amedeo Anselmi, M.D., Ph.D., University Hospital of Rennes, provided and cared for study patients. Karl Bounader, M.D., University Hospital of Rennes, provided and cared for study patients. Yoann Launey, M.D., Ph.D., University Hospital of Rennes, provided and cared for study patients. Thomas Lebouvier, M.D., University Hospital of Rennes, provided and cared for study patients. Alessandro Parasido, University Hospital of Rennes, provided and cared for study patients. Florian Reizine, M.D., University Hospital of Rennes, provided and cared for study patients. Maxime Esvan, MSc, University Hospital of Rennes, participated to performed the statistical analysis. Philippe Seguin, M.D., Ph.D., University Hospital of Rennes, Professor, provided and cared for study patients. Emmanuel Besnier, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Dorothée Carpentier, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Thomas Clavier, M.D., University Hospital of Rouen, collected data, provided and cared for study patients. Anne Olland, M.D., Ph.D., University Hospital of Strasbourg, Professor, collected data, provided and cared for study patients. Marion Villard, M.D., University Hospital of Strasbourg, collected data, provided and cared for study patients. Fanny Bounes, M.D., University Hospital of Toulouse, collected data, provided and cared for study patients. François Labaste, M.D., Ph.D., University Hospital of Toulouse, Professor, collected data, provided and cared for study patients. Vincent Minville, M.D., Ph.D., University Hospital of Toulouse, Professor, collected data, provided and cared for study patients. Antoine Guillon, M.D., University Hospital of Tours, collected data, provided and cared for study patients. Yannick Fedun, M.D., Bretagne Atlantique Hospital, Vannes, collected data, provided and cared for study patients.
Funding
This work was supported by a grant from the university hospital of Rennes (Appel à projets CFTR2) and by a grant from the French society of thoracic and cardio-vascular surgery (Société française de chirurgie thoracique et cardio-vasculaire, Bourse Marc Laskar).
Author information
Authors and Affiliations
Consortia
Contributions
NN, AM, CF, EF, AV, NMa substantially contributed to the conception and design of the work. NN, AM, MP, AP, PEF, NMo, AB, LGC, PGG, FL, EB, GLB, NMa, EF, AV contributed to acquisition of data for the work. NN, AM, MS, PGG, JTR, NMa contributed to analysis and interpretation of data for the work. All authors contributed to drafting the article or revising it critically for important intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ECMOSARS registry has been approved by the university hospital of Rennes ethics committee (n° 20.43). After information, non-opposition of patients or their legal representative was obtained for use of the data.
Competing interests
Nicolas NESSELER declares no competing interests. Alexandre MANSOUR received payments made to his institution from i-SEP for consulting fees, and from LFB, Viatris, Aguettant and Pfizer for lecture fees. Matthieu SCHMIDT received consultancy fees from Getinge, Xenios FMC and Drager. Claire FOUGEROU declares no competing interests. James T. ROSS declares no competing interests. Alizée PORTO declares no competing interests. Marylou PARA declares no competing interests. Pierre-Emmanuel FALCOZ declares no competing interests. Nicolas MONGARDON received consultant fees from Amomed and Baxter. Guillaume LEBRETON reports lecture fees from Livanova and Abiomed. Antoine BEURTON declares no competing interests. Lucie GAIDE-CHEVRONNAY declares no competing interests. Erwan FLECHER declares no competing interests. André VINCENTELLI declares no competing interests. Nicolas MASSART declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
of Healthcare-associated infections in patients with severe COVID-19 supported with extracorporeal membrane oxygenation: a nationwide cohort study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nesseler, N., Mansour, A., Schmidt, M. et al. Healthcare-associated infections in patients with severe COVID-19 supported with extracorporeal membrane oxygenation: a nationwide cohort study. Crit Care 28, 54 (2024). https://doi.org/10.1186/s13054-024-04832-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04832-3