Abstract
Background
Gut microbiota alterations have been reported in hospitalized COVID-19 patients, with reduced alpha diversity and altered microbiota composition related to respiratory failure. However, data regarding gut microbiota and mortality are scarce.
Methods
Rectal swabs for gut microbiota analyses were collected within 48 h after hospital admission (baseline; n = 123) and three-month post-admission (n = 50) in a subset of patients included in the Norwegian SARS-CoV2 cohort study. Samples were analysed by sequencing the 16S rRNA gene. Gut microbiota diversity and composition at baseline were assessed in relation to need for intensive care unit (ICU) admission during hospitalization. The primary objective was to investigate whether the ICU-related gut microbiota was associated with 60-day mortality.
Results
Gut microbiota diversity (Shannon index) at baseline was lower in COVID-19 patients requiring ICU admission during hospitalization than in those managed in general wards. A dysbiosis index representing a balance of enriched and reduced taxa in ICU compared with ward patients, including decreased abundance of butyrate-producing microbes and enrichment of a partly oral bacterial flora, was associated with need of ICU admission independent of antibiotic use, dexamethasone use, chronic pulmonary disease, PO2/FiO2 ratio, C-reactive protein, neutrophil counts or creatinine levels (adjusted p < 0.001). The ICU-related dysbiosis index at baseline correlated with systemic inflammation and was associated with 60-day mortality in univariate analyses (Hazard ratio 3.70 [2.00–8.6], p < 0.001), as well as after separate adjustment for covariates. At the three-month follow-up, the dysbiosis index remained elevated in ICU patients compared with ward patients (adjusted p = 0.007).
Conclusions
Although our data should be regarded as exploratory due to low number of clinical end points, they suggest that gut microbiota alterations during hospitalization could be related to poor prognosis after severe COVID-19. Larger studies of gut involvement during COVID-19 in relation to long-term clinical outcome are warranted.
Trial registration NCT04381819. Retrospectively registered May 11, 2020.
Similar content being viewed by others
Introduction
Although SARS-CoV-2 primarily infects the respiratory tract, mounting evidence suggests that also the gastrointestinal (GI) tract is involved in the pathogenesis of COVID-19 [1]. SARS-CoV-2 infects human enterocytes and replicates in the gut mucosa [2], and viral entry receptors including angiotensin converting enzyme-2 (ACE-2) and several membrane-bound serine proteases are expressed in intestinal epithelial cells [3]. In a longitudinal study, viral shedding from faeces was detected in nearly 50% of patients during acute infection and in 3.8% of patients after 7-month follow-up [4].
Gastrointestinal symptoms are frequently occurring in severe COVID-19 patients, and a meta-analysis has suggested that patients with gastrointestinal involvement had a higher risk of severe disease [5]. It has also been hypothesized that the gut microbiota could be a mediator of host inflammatory immune responses during COVID-19, thereby contributing to the pronounced systemic inflammation observed in patients requiring hospitalization [6, 7].
Patients hospitalized with COVID-19 exhibit an altered gut microbiota composition compared to uninfected controls [8] and also compared to patients admitted with seasonal influenza [9]. Gut microbiota alterations, including reduced bacterial alpha diversity and changes in microbial composition, have been found to be related to disease severity, including acute respiratory failure and need of ICU admission (reviewed in [10]). We recently reported that the gut microbiota composition remained altered three months after hospitalization and was associated with persistent pulmonary pathology [11].
It has been hypothesized that COVID-related gut microbiota alterations (dysbiosis) could promote long-term clinical outcome [12]. A recent study of critically ill COVID-19 patients based on selective bacterial cultures and subsequent sequencing reported that higher concentrations of opportunistic pathogens in the oropharyngeal and intestinal compartments were independently associated with 90-day mortality [13]. However, data on sequencing-based gut microbiota dysbiosis and mortality are lacking. In the present substudy from the longitudinal Norwegian SARS-CoV2 cohort, we assessed gut microbiota alterations from samples collected within 48 h after hospitalization in relation to need for ICU admission and investigated whether an ICU-related dysbiosis was associated with 60-day mortality.
Methods
Patients and clinical outcomes
Study participants were recruited from the Norwegian SARS-CoV-2 study (NCT04381819), a multicentre cohort study of COVID-19 patients admitted to five Norwegian hospitals, conducted as part of an International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) WHO Clinical Characterization Protocol study, as previously described [14]. Participants aged ≥ 18 years and admitted to hospital with PCR-confirmed SARS-2-CoV-2 infection were eligible for inclusion and were included from March 9, 2020, until December 15, 2020. The study was approved by the Committee for Medical Research Ethics Region South-East Norway (approval no. 106624). All participants gave informed consent prior to inclusion, either directly or through a legally authorized representative. Gut microbiota alterations were assessed in relation to need for treatment at ICU/high-dependency unit during hospitalization, and the primary end point was 60-day post-admission all-cause mortality [14].
Gut microbiota analyses
Rectal swabs were sampled within 48 h after admission and three-month post-admission, stored in a stabilizing transportation medium (soluble Amies, Thermo Scientific™) and frozen at − 80 °C until analysis. Faecal DNA was extracted using the QIAamp PowerFecal®Pro DNA Kit (Qiagen, Germany), with slight modifications. Briefly, 700 µL of faecal material was pelleted and homogenized in 800 µL of kit solution CD1 using a bead-beating homogenizer (2 × 60 s at 5.5 ms, 20 °C) and further processed according to the manufacturer’s protocol. Libraries for 16S rRNA amplicon sequencing were generated as previously described [11]. Briefly, the hypervariable regions V3 and V4 of the 16S rRNA gene were amplified using dual-indexed universal primers 319F (forward) and 806R (reverse), and Phusion High-Fidelity PCR Master Mix with HF buffer (Thermo Fisher Scientific, USA). The PCR products were cleaned and normalized using a SequalPrep Normalization Plate Kit (Thermo Fisher Scientific, USA). Quality control and quantification of the pooled libraries were performed using an Agilent Bioanalyzer (Agilent Technologies, USA) and Kapa Library Quantification Kit (Kapa Biosystems, London, UK). Sequencing was performed at the Norwegian Sequencing Centre (Oslo, Norway) using the Illumina MiSeq platform and v3 kit (Illumina, San Diego, CA, USA), allowing for 300 base pair paired-end reads.
Sequence processing and bioinformatics
Paired-end reads containing Illumina Universal Adapters or PhiX were discarded using bbduk version 38.90 (https://sourceforge.net/projects/bbmap/) and the remaining reads were demultiplexed using cutadapt version 3.5 [15]. Trimming of indexes, heterogeneity spacers and primers was also done with cutadapt (parameters: -e 0.1 –overlap 20 –discard-untrimmed -m 250) and the paired-end reads were subsequently quality trimmed and merged using bbmerge version 38.90 [16]. The merged contigs were trimmed to 400 bp and denoised to ASVs (Amplicon Sequence Variants) with deblur in Qiime2 version 2022.2 [17]. Taxonomic classification of ASVs was done in Qiime2 using a naïve Bayes classifier [18] trained on the V3-V4 region of a preclustered version (99% sequence similarity) of the Silva database version 138 [19]. ASVs from mitochondria, chloroplast or lacking taxonomic annotation on order level were removed. Filtering of contaminants was done with the R package microDecon based on four negative control samples. A de-novo phylogenetic tree was built in Qiime2 based on the remaining ASVs. Differential abundance analysis was performed on genera present in at least 10% of patients. Gut microbiota alpha diversity was assessed by Shannon diversity index, performed on a rarefied (subsampled) dataset with an ASV count of 5144 per sample.
Statistical analyses
Patient characteristics were compared using Student's t test or Mann–Whitney U-test depending on the distribution or chi-square for continuous and categorical variables, respectively. We first characterized gut microbiota alterations in relation to need for ICU treatment during hospitalization. Based on the differences (Table 1) between ward and ICU patients, and due to limited number of patients in the ICU group, we constructed a propensity score using logistic regression for adjustment purposes. Age was also included in the score due to near significant differences between groups. As several biochemical markers may reflect similar processes, C-reactive protein (CRP), neutrophil counts and creatinine were used in the propensity score. Similarly, we chose the PO2/FiO2 ratio over variables reflecting use of oxygen therapy. PO2/FiO2 is defined as the ratio between the partial pressure of oxygen in blood (PaO2) and fraction of inspired oxygen the patient is receiving (FiO2). All together, the propensity score consisted of age, use of dexamethasone or antibiotics, chronic pulmonary disease, PO2/FiO2 ratio, neutrophil counts, CRP and creatinine.
Differential abundance analysis was performed in baseline samples with ANCOM-BC2 [20] between ICU and ward patients. An ICU-related dysbiosis index representing a balance of enriched and reduced taxa in baseline faecal samples from ICU compared with ward patients was calculated by using the selbal algorithm (in R), which takes the compositional nature of microbiota data into account. Both the Shannon diversity index and ICU-related dysbiosis index were compared by linear regression adjusting for the propensity score. The distribution of Shannon diversity and ICU-related dysbiosis index are shown in Additional file 1: Fig. S1. The dysbiosis index showed a normal distribution but Shannon diversity was somewhat right skewed. However, log or log(x + 1) transformation rendered the variable more skewed and it was therefore used non-transformed.
We next investigated the association between the ICU-related dysbiosis index and 60-day all-cause mortality by receiver operating characteristic (ROC) analysis and Kaplan–Meier analysis (tertiles). The modulation of the association between dysbiosis index (as continuous variable) and mortality was further assessed in cox regression adjusting separately for covariates with trend level differences between survivors and non-survivors (Table 1) as well as for the ICU propensity score.
Statistical analysis was performed with IBM SPSS statistics package (version 27.0.0.0) and R: A language and environment for statistical computing (version 4.2.2).
Results
Baseline characteristics
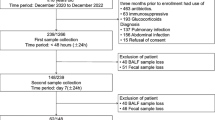
As shown in Table 1, patients were predominantly male, and 28 out of 123 participants were treated in the ICU during hospitalization. ICU patients were on average five years older than ward patients, with higher prevalence of pre-existing pulmonary disease, higher levels of systemic inflammatory markers and more often receiving antibiotics and dexamethasone treatment. Eleven participants (8.9%) died within 60 days of inclusion, and all of these were ICU patients, as shown in the flow chart (Fig. 1).
Reduced alpha diversity and altered gut microbiota composition in ICU patients
As depicted in Fig. 2A, gut microbiota diversity assessed by Shannon diversity index at baseline was trend level lower (p = 0.077) in COVID-19 patients requiring ICU during hospitalization compared to ward patients in analysis adjusting for the ICU propensity score (see methods, statistical analysis, for definition). Shannon diversity was not significantly different in patients treated or not treated with dexamethasone or antibiotics (Additional file 1: Table S1). ICU patients also had an altered gut microbiota composition, with increased relative abundance of Pyramidobacter and Eremococcus, and reduced abundance of Collinsella and Eubacterium ventriosum group (Volcano plot, Fig. 2B).
Gut microbiota alterations within 48 h after hospital admission in COVID-19 patients admitted to ICU (n = 28) compared to ward patients (n = 95). A Tukey plots showing reduced Shannon diversity index in ICU patients with adjusted p value (ICU propensity score, see statistical methods), B Volcano plot visualizing differentially abundant bacterial genera (from ANCOM-BC2) based on effect size (x-axis) and p values (y-axis) in relation to ICU status, C Tukey plot showing dysbiosis index for ICU vs. ward patients with adjusted p value (ICU propensity score, see statistical methods), D Correlations between dysbiosis index, degree of respiratory distress (p/PF-ratio) and inflammatory markers
Dysbiosis index characterizing ICU patients independent of relevant confounders
For further analyses, we generated an ICU-related dysbiosis index based on the R package Selbal for selecting bacterial taxa distinguishing ICU from ward patients [21]. The following taxa were identified as enriched in ICU patients: Pyramidobacter, Eremococcus, Ruminococcaceae;g_uncultured, Rothia, Intestinibacter, Olsenella, Fournierella, and Eubacterium eligens group. The following taxa were reduced: Oscillospiraceae family, Eubacterium ventriosum group, Fastidiosipila, Christensenellaceae;g__uncultured, Roseburia, Alloprevotella, Terrisporobacter, Incertae_Sedis;g__uncultured, Eubacterium siraeum group, and Howardella. The index is defined as the difference between the arithmetic means of the log-transformed abundances in these two groups of taxa [21]. Only genera present in at least 20% of samples were considered for inclusion in the index. As shown in Fig. 2C, this index was associated with need of ICU (p < 0.001) independent of the ICU propensity score.
ICU-related dysbiosis index in relation to degree of respiratory distress and inflammatory markers
As shown in Fig. 2D, the ICU-related dysbiosis index correlated negatively with the PO2/FiO2 ratio, with lower values reflecting increasing degree of respiratory failure. The dysbiosis index correlated positively with levels of C-reactive protein (CRP) and neutrophil count, and negatively with lymphocyte count. Overall, patients treated with dexamethasone and antibiotics had a higher ICU-related dysbiosis index (Additional file 1: Table S1).
ICU-related dysbiosis index associated with 60-day mortality
During 60-day follow-up, 11 patients died. As shown in Kaplan–Meier plots in Fig. 3, the upper tertile of the dysbiosis index was associated with higher 60-day mortality (p < 0.001). A ROC analysis of the ICU-related dysbiosis index for 60-day mortality revealed an area under curve (AUC) of 0.90 (0.83–0.98), p < 0.001. Cox regression analysis of the dysbiosis index (as a continuous variable) was associated with 60-day mortality in univariate analyses (Hazard ratio 3.70 [2.00–8.6], p < 0.001). Clinical characteristics for survivors and non-survivors are given in Table 1, and adjusting separately for markers that were trend levels different between survivors and non-survivors did not alter this association (Fig. 3C). Adjustment with the ICU propensity score attenuated the association somewhat, but remained significant. Some of the microbes enriched in the ICU-related dysbiosis index, Pyramidobacter and Olsenella, in addition to bacteria previously reported in severe COVID-19, including Veillonellaceae, Bilophila and Escherichia [7] were also enriched in patients with a mortality end point (Fig. 3D).
Association between gut microbiota alterations (dysbiosis) within 48 h after hospital admission and 60-day mortality in hospitalized COVID-19 patients. A ROC analysis of ICU dysbiosis index for 60-day mortality (n = 11). B Kaplan–Meier curve for 60-day mortality according to tertiles of ICU dysbiosis index. C Cox regression analysis of ICU dysbiosis index (as a continuous variable) in univariate analysis (black) and adjustment with covariates (red) one by one that were trend level different between survivors and non-survivors (see Additional file 1: Table S1, as well as ICU propensity score, see statistical methods), D Volcano plot visualizing differentially abundant bacterial genera based on effect size (x-axis) and p values (y-axis) in relation to 60-day mortality
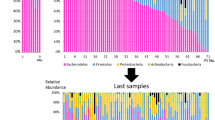
Persistent dysbiosis in ICU patients three-month post-admission
As shown in Fig. 4, the ICU-related dysbiosis index remained significantly elevated in ICU patients (n = 7) compared with ward patients (n = 43) at the three-month follow-up (adjusted p = 0.007), although paired analysis revealed a tendency to reduction in the surviving ICU patients from baseline (p = 0.063). In the whole cohort, the reduction from baseline to 3 months was significant (p < 0.001).
Discussion
In this prospective Norwegian multicentre cohort of hospitalized COVID-19 patients, we assessed gut microbiota alterations in relation to need for ICU admission, and whether an ICU-related dysbiosis was associated with 60-day mortality. Our results can be summarized as follows: (i) Gut microbiota diversity was lower in COVID-19 patients requiring ICU during hospitalization than in ward patients, (ii) ICU patients had an altered gut microbiota composition (dysbiosis), independent of admission demographics that differed with ward patients, as well as antibiotic use, dexamethasone use, pulmonary comorbidities, and inflammatory markers, and (iii) the dysbiosis index was associated with 60-day mortality, also in adjusted analysis.
Several studies have reported gut microbiota alterations during acute COVID-19 and, in particular, in relation to acute respiratory failure and need of ICU [10]. Our finding of reduced microbiota diversity in ICU patients is in line with previous studies [9, 22]. Based on the ICU-related dysbiosis index, we also found that reduced relative abundance of several members of the Lachnospiraceae and Ruminococcaceae families, such as Roseburia and different Eubacterium species, which are known producers of butyrate, distinguished ICU from ward patients, also in line with several previous studies [9, 10, 22]. Butyrate has local immunomodulatory effects in the gut mucosa and is the main energy substrate for enterocytes, and is vital for gut barrier maintenance [23].
Interestingly, the ICU-related dysbiosis index also consisted of increased relative abundance of several microbes with partial affinity to the oral microbiome, including Pyramidobacter, Olsenella and Rothia. In particular, Rothia species have been found in increased abundance in several previous gut microbiota studies [9, 24,25,26] and, in one study, enriched both in the oral and gut microbiota of hospitalized COVID-19 patients [24]. Whether this dysbiosis is a consequence of viral replication in the oral cavity and/or gut mucosa [2], disrupted mucosal immunology paving the way for opportunistic pathogens, the inflammatory response or other factors [10], cannot be determined from our data. Of note, the dysbiosis index correlated with the degree of respiratory distress and markers of systemic inflammation, in line with previous studies [10]. Furthermore, data from animal models have shown that oxygen therapy could promote dysbiosis in airways and the gut that could contribute to oxygen-induced lung injury [27]. Hence, both respiratory distress and oxygen therapy itself could potentially contribute to a gut-lung axis.
Our study expands the current literature by reporting a potential link between ICU-related microbiota alterations and 60 days mortality, in line with a recent study showing an association between day-90 mortality and higher concentrations of opportunistic pathogens in the oropharyngeal and intestinal compartments of critically ill patients [13]. Of note, our data should be interpreted with caution, as our sample size was not powered for multivariate adjustment. Still, the association between dysbiosis and 60-day mortality was not weakened after separate adjustment for relevant covariates including age, comorbidities, kidney function and inflammatory markers. Treatment with dexamethasone and antibiotics attenuated the association somewhat, as these were strongly associated with 60-day mortality. For this reason, the strongest attenuation of the association between dysbiosis and 60-day mortality was seen with the ICU propensity score reflecting several parameters strongly associated with poor prognosis (e.g. dexamethasone, antibiotics and P/F-ratio).
Some of the microbes being enriched in ICU patients, including Pyramidobacter and Olsenella, also had increased relative abundance in patients who died during the first 60 days. In a previous work, enhanced gut microbiota levels of Pyramidobacter correlated with circulating IL-6 levels, an upstream regulator of the pro-inflammatory response in severe COVID-19 disease, and predictor of disease progression in frail adults [14] while enriched Olsenella were detected in the lung microbiota of COVID-19 patients [15].
60-day mortality was also associated with increased abundance of Veillonellaceae, Bilophila and Escherichia, known pathogens that have been reported increased in previous studies of hospitalized COVID-19 patients [10]. Of interest, Veillonella was reported enriched in both oral and faecal samples of patients with COVID-19 and was also detected in high concentration in bronchoalveolar lavage samples [28]. The oral microbiota is altered in COVID-19 patients [28, 29] and has been proposed as a potential reservoir of pulmonary co-infections, as well as contributing to a disturbed gut microbiota with potential for microbial translocation to the systemic circulation [10]. Studies of selective decontamination of the oral cavity and upper GI tract have shown promise in reducing in-hospital mortality in ICU patients receiving mechanical ventilation [30, 31]. Our data, in light of the overall literature [10], suggest that such strategies could also be relevant in future intervention trials of critical COVID-19 patients.
Although rectal swabs were collected within 48 h after hospital admission, different treatment modalities could have contributed to gut microbiota differences between ICU and ward patients. Even short courses of antibiotics may alter the gut microbiota composition, and in particular, anti-anaerobic antibiotics have been shown to increase mortality in ICU patients, possibly due to effect on gut and airway microbiota [32]. Also dexamethasone could impact the gut microbiota composition and has been reported to interfere with gut permeability [33]. Furthermore, the enrichment of a partly oral bacterial flora in the gut microbiota of ICU patients could potentially also be explained by factors such as mechanical ventilation, nasogastric feeding tubes and parenteral nutrition [34].
Whatever contributing factors, the dysbiosis index remained elevated in ICU patients compared with ward patients also at the three-month follow-up. Previous studies, including data from our own group, have shown that gut microbiota alterations can persist long-term after hospitalization and are associated with persisting pulmonary symptoms and low-grade inflammation [10, 11]. Future studies should investigate whether persistent microbiota alterations after severe COVID could affect long-term clinical outcome, including long-COVID [35].
Our study has several limitations, in particular the limited number of patients that died within 60 days, as well as the low number of ICU patients at 3-month follow-up. A formal sample size calculation was not performed, partly because there are no standardized methods for sample size calculations in microbiota studies, and the sample size was not powered for multivariate adjustment. In addition, the study lacks an independent replication cohort, and this should therefore be regarded as exploratory. Furthermore, an observational study cannot draw any conclusions regarding causation, and several factors including comorbidities, disease severity and treatment modalities could have contributed to our findings. Dietary habits before admission and nutritional support during hospitalization are potential contributors to a distorted gut microbiome, and lack of food frequency questionnaires and other data on nutrition is another limitation.
In addition, patients were included before occurrence of the current omicron strains and with a much lower vaccination coverage in the population. Hence, our findings cannot be directly extrapolated to the current epidemiological situation, as omicron strains have been shown to have lower replication in lung and gut cells compared to delta variants [36]. Our study also has obvious strengths, being one of the largest studies with microbiota sampling during acute COVID-19, repeated microbiota sampling at long-term follow-up, as well as mortality end points up to day 60.
In conclusion, our data, although exploratory, provide evidence that gut microbiota alterations detected within 48 h after hospital admission could be related to poor prognosis after severe COVID-19. To clarify the clinical impact of these findings, larger studies of gut involvement during COVID-19 in relation to long-term clinical outcome, including patients infected with current omicron variants, are warranted.
Availability of data and materials
Regarding data sharing, Norwegian institutional data privacy regulations prohibit deposition of individual level data to public repositories. Participant written consent also does not cover public sharing of data for use for unknown purposes. However, upon contact with Marius Trøseid (marius.troseid@medisin.uio.no) or Thor Ueland (thor.ueland@medisin.uio.no), an institutional data transfer agreement can be established, and data shared if the aims of data use are covered by ethical approval and patient consent. The procedure will involve an update to the ethical approval as well as review by legal departments at both institutions, and the process will typically take 1 to 2 months from initial contact. Data will be shared via a secure online procedure.
References
Galanopoulos M, Gkeros F, Doukatas A, et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. 2020;26(31):4579–88. https://doi.org/10.3748/wjg.v26.i31.4579.
Lamers MM, Beumer J, van der Vaart J, et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369(6499):50–4. https://doi.org/10.1126/science.abc1669.
Zang R, Gomez Castro MF, McCune BT, et al. TMPRSS2 and TMPRSS4 promote SARS-CoV-2 infection of human small intestinal enterocytes. Sci Immunol. 2020. https://doi.org/10.1126/sciimmunol.abc3582.
Natarajan A, Zlitni S, Brooks EF, et al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med (N Y). 2022;3(6):371–87. https://doi.org/10.1016/j.medj.2022.04.001.
Mao R, Qiu Y, He JS, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667–78. https://doi.org/10.1016/s2468-1253(20)30126-6.
Ferreira C, Viana SD, Reis F. Gut microbiota dysbiosis-immune hyperresponse-inflammation triad in coronavirus disease 2019 (COVID-19): impact of pharmacological and nutraceutical approaches. Microorganisms. 2020. https://doi.org/10.3390/microorganisms8101514.
Vignesh R, Swathirajan CR, Tun ZH, et al. Could Perturbation of Gut Microbiota Possibly Exacerbate the Severity of COVID-19 via Cytokine Storm? Front Immunol. 2020;11:607734. https://doi.org/10.3389/fimmu.2020.607734.
Zuo T, Zhang F, Lui GCY, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. 2020;159(3):944-55.e8. https://doi.org/10.1053/j.gastro.2020.05.048.
Gu S, Chen Y, Wu Z, et al. Alterations of the gut microbiota in patients with coronavirus disease 2019 or H1N1 influenza. Clin Infect Dis. 2020;71(10):2669–78. https://doi.org/10.1093/cid/ciaa709.
Lau RI, Zhang F, Liu Q, et al. Gut microbiota in COVID-19: key microbial changes, potential mechanisms and clinical applications. Nat Rev Gastroenterol Hepatol. 2022. https://doi.org/10.1038/s41575-022-00698-4.
Vestad B, Ueland T, Lerum TV, et al. Respiratory dysfunction three months after severe COVID-19 is associated with gut microbiota alterations. J Intern Med. 2022;291(6):801–12. https://doi.org/10.1111/joim.13458.
Rocchi G, Giovanetti M, Benedetti F, et al. Gut microbiota and COVID-19: potential implications for disease severity. Pathogens. 2022. https://doi.org/10.3390/pathogens11091050.
Patrier J, Villageois-Tran K, Szychowiak P, et al. Oropharyngeal and intestinal concentrations of opportunistic pathogens are independently associated with death of SARS-CoV-2 critically ill adults. Crit Care. 2022;26(1):300. https://doi.org/10.1186/s13054-022-04164-0.
Trøseid M, Dahl TB, Holter JC, et al. Persistent T-cell exhaustion in relation to prolonged pulmonary pathology and death after severe COVID-19: results from two Norwegian cohort studies. J Intern Med. 2022;292(5):816–28. https://doi.org/10.1111/joim.13549.
Kechin A, Boyarskikh U, Kel A, et al. cutPrimers: a new tool for accurate cutting of primers from reads of targeted next generation sequencing. J Comput Biol. 2017;24(11):1138–43. https://doi.org/10.1089/cmb.2017.0096.
Bushnell B, Rood J, Singer E. BBMerge - accurate paired shotgun read merging via overlap. PLoS ONE. 2017;12(10):e0185056. https://doi.org/10.1371/journal.pone.0185056.
Bolyen E, Rideout JR, Dillon MR, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37(8):852–7. https://doi.org/10.1038/s41587-019-0209-9.
Bokulich NA, Kaehler BD, Rideout JR, et al. Optimizing taxonomic classification of marker-gene amplicon sequences with QIIME 2’s q2-feature-classifier plugin. Microbiome. 2018;6(1):90. https://doi.org/10.1186/s40168-018-0470-z.
Quast C, Pruesse E, Yilmaz P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41(Data issue):D590–6. https://doi.org/10.1093/nar/gks1219.
Lin H, Peddada SD. Analysis of compositions of microbiomes with bias correction. Nat Commun. 2020;11(1):3514. https://doi.org/10.1038/s41467-020-17041-7.
Rivera-Pinto J, Egozcue JJ, Pawlowsky-Glahn V, et al. Balances: a new perspective for microbiome analysis. mSystems. 2018. https://doi.org/10.1128/mSystems.00053-18.
Gaibani P, D’Amico F, Bartoletti M, et al. The gut microbiota of critically Ill patients with COVID-19. Front Cell Infect Microbiol. 2021;11:670424. https://doi.org/10.3389/fcimb.2021.670424.
Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504(7480):446–50. https://doi.org/10.1038/nature12721.
Wu Y, Cheng X, Jiang G, et al. Altered oral and gut microbiota and its association with SARS-CoV-2 viral load in COVID-19 patients during hospitalization. NPJ Biofilms Microbiomes. 2021;7(1):61. https://doi.org/10.1038/s41522-021-00232-5.
Tao W, Zhang G, Wang X, et al. Analysis of the intestinal microbiota in COVID-19 patients and its correlation with the inflammatory factor IL-18. Med Microecol. 2020;5:100023. https://doi.org/10.1016/j.medmic.2020.100023.
Rafiqul Islam SM, Foysal MJ, Hoque MN, et al. Dysbiosis of oral and gut microbiomes in SARS-CoV-2 infected patients in bangladesh: elucidating the role of opportunistic gut microbes. Front Med. 2022;9:821777. https://doi.org/10.3389/fmed.2022.821777.
Ashley SL, Sjoding MW, Popova AP, et al. Lung and gut microbiota are altered by hyperoxia and contribute to oxygen-induced lung injury in mice. Sci Transl Med. 2020. https://doi.org/10.1126/scitranslmed.aau9959.
Ma S, Zhang F, Zhou F, et al. Metagenomic analysis reveals oropharyngeal microbiota alterations in patients with COVID-19. Signal Transduct Target Ther. 2021;6(1):191. https://doi.org/10.1038/s41392-021-00614-3.
Miller EH, Annavajhala MK, Chong AM, et al. Oral microbiome alterations and SARS-CoV-2 saliva viral load in patients with COVID-19. Microbiol Spectr. 2021;9(2):e0005521. https://doi.org/10.1128/Spectrum.00055-21.
Hammond NE, Myburgh J, Seppelt I, et al. Association between selective decontamination of the digestive tract and in-hospital mortality in intensive care unit patients receiving mechanical ventilation: a systematic review and meta-analysis. JAMA. 2022;328(19):1922–34. https://doi.org/10.1001/jama.2022.19709.
Myburgh JA, Seppelt IM, Goodman F, et al. Effect of selective decontamination of the digestive tract on hospital mortality in critically Ill patients receiving mechanical ventilation: a randomized clinical trial. JAMA. 2022;328(19):1911–21. https://doi.org/10.1001/jama.2022.17927.
Chanderraj R, Baker JM, Kay SG, et al. In critically ill patients, anti-anaerobic antibiotics increase risk of adverse clinical outcomes. Eur Respir J. 2022. https://doi.org/10.1183/13993003.00910-2022.
Spitz J, Hecht G, Taveras M, et al. The effect of dexamethasone administration on rat intestinal permeability: the role of bacterial adherence. Gastroenterology. 1994;106(1):35–41. https://doi.org/10.1016/s0016-5085(94)94155-6.
Wolff NS, Hugenholtz F, Wiersinga WJ. The emerging role of the microbiota in the ICU. Crit Care. 2018;22(1):78. https://doi.org/10.1186/s13054-018-1999-8.
Liu Q, Mak JWY, Su Q, et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut. 2022;71(3):544–52. https://doi.org/10.1136/gutjnl-2021-325989.
Meng B, Abdullahi A, Ferreira I, et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature. 2022;603(7902):706–14. https://doi.org/10.1038/s41586-022-04474-x.
Acknowledgements
We thank site staff for recruitment and follow-up of participants, and the patients for participating in the trial. Members of the Norwegian SARS-Co-2 study group are listed as follows: Cathrine Austad, Gry Klouman Bekken, Mette Bogen, Anne Hermann, Hanne Opsand, Trude Steinsvik, Bjørn Martin Woll (Vestre Viken Hospital Trust); Erik Egeland Christensen, Susanne Dudman, Kristin Eftestøl, Børre Fevang, Liv Hesstvedt, Marthe Jøntvedt Jørgensen, Elisabeth Toverud Landaas, Andreas Lind, Fredrik Müller, Sarah Nur, Vidar Ormaasen, Frank Olav Pettersen, Else Quist-Paulsen, Dag Henrik Reikvam, Kjerstin Røstad, Linda Skeie, Anne Katrine Steffensen, Birgitte Stiksrud (Oslo University Hospital); Berit Gravrok, Vegard Skogen, Garth Daryl Tylden (University Hospital of North Norway).
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). This study received the following funding: Oslo University Hospital, Research Council of Norway (Grant No 312780), and a philanthropic donation from Vivaldi Invest A/S owned by Jon Stephenson von Tetzchner. The funders had no role in study design, data collection, or decision to publish this article.
Author information
Authors and Affiliations
Consortia
Contributions
MT, JCH, JRH and TU were responsible for the study conception and execution of the present substudy and to secure the financial support. JCH, AMDR, KT, ARH, ABK, LH, AT, SB, KEM and SJ were responsible for the management, coordination, research activity, planning and execution of the Norwegian SARS-CoV-2 study. KH, BV, TS, BKG and JRH were responsible for preparation and analyses of the microbiota samples. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was carried out in accordance with the Helsinki declaration. All participants gave written informed consent, either directly or through a legally authorized representative, to participate in this study. The study was approved by the Regional Committee for Medical and Health Research Ethics in South-Eastern Norway (reference no 106624).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Shannon diversity and ICU-related dysbiosis index according to dexamethasone and antibiotic treatment in hospitalized COVID-19 patients. Fig. S1. Distribution of Shannon diversity and dysbiosis index in hospitalized COVID-19 patients
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Trøseid, M., Holter, J.C., Holm, K. et al. Gut microbiota composition during hospitalization is associated with 60-day mortality after severe COVID-19. Crit Care 27, 69 (2023). https://doi.org/10.1186/s13054-023-04356-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04356-2