Abstract
Background
It is unclear if the impact of frailty on mortality differs between patients with viral pneumonitis due to COVID-19 or other causes. We aimed to determine if a difference exists between patients with and without COVID-19 pneumonitis.
Methods
This multicentre, retrospective, cohort study using the Australian and New Zealand Intensive Care Society Adult Patient Database included patients aged ≥ 16 years admitted to 153 ICUs between 01/012020 and 12/31/2021 with admission diagnostic codes for viral pneumonia or acute respiratory distress syndrome, and Clinical Frailty Scale (CFS). The primary outcome was hospital mortality.
Results
A total of 4620 patients were studied, and 3077 (66.6%) had COVID-19. The patients with COVID-19 were younger (median [IQR] 57.0 [44.7–68.3] vs. 66.1 [52.0–76.2]; p < 0.001) and less frail (median [IQR] CFS 3 [2–4] vs. 4 [3–5]; p < 0.001) than non-COVID-19 patients. The overall hospital mortality was similar between the patients with and without COVID-19 (14.7% vs. 14.9%; p = 0.82). Frailty alone as a predictor of mortality showed only moderate discrimination in differentiating survivors from those who died but was similar between patients with and without COVID-19 (AUROC 0.68 vs. 0.66; p = 0.42). Increasing frailty scores were associated with hospital mortality, after adjusting for Australian and New Zealand Risk of Death score and sex. However, the effect of frailty was similar in patients with and without COVID-19 (OR = 1.29; 95% CI: 1.19–1.41 vs. OR = 1.24; 95% CI: 1.11–1.37).
Conclusion
The presence of frailty was an independent risk factor for mortality. However, the impact of frailty on outcomes was similar in COVID-19 patients compared to other causes of viral pneumonitis.
Graphical Abstract

Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had a devastating global impact. The clinical spectrum ranges widely from asymptomatic to severe respiratory failure, multiorgan failure, and death [1, 2]. Evidence suggests that older people with frailty are unequally affected [3], and that higher degrees of frailty along with cumulative comorbidities are linked with higher mortality in patients with COVID-19 [3,4,5,6,7].
Healthcare in many parts of the world has been severely strained due to insufficient intensive care unit (ICU) beds and workforce capacity [8]. This pressure resulted in triage systems to maximize efficient resource use [9,10,11,12,13,14]. Frailty assessment tools, such as the Clinical Frailty Scale (CFS), have been proposed as an adjunct to age-based criteria for critical care triage decisions (The National Institute for Health and Care Excellence, NICE triage guidelines) [15]. This guideline suggested that patients older than 65 years with a CFS score ≥ 5 might not benefit from ICU admission [10, 12, 16] and such patients were encouraged to establish goals of care documentation [9, 12, 13, 17]. Despite this, frail patients with COVID-19 were admitted to ICU and had greater mortality but spent relatively fewer days in ICU compared with non-frail patients [18].
Pre-pandemic, patients with frailty were also common among patients admitted to ICU. These patients had more than double the risk of death and functional dependence than patients without frailty [19,20,21]. A study in Australia and New Zealand found that a third of non-COVID-19 patients admitted to the ICU with pneumonia were frail and were associated with poor outcomes [22]. Frail patients with COVID-19 had a higher case fatality rate. It is, however, unclear if the impact of frailty on outcomes differs between patients with and without COVID-19. With the geographic isolation and very strict public health measures, the Australian and New Zealand healthcare system was not overwhelmed in 2020 [23], allowing improved access to ICU earlier to all patients, including those with frailty. This was, however, not the case in 2021 when a higher volume of cases put significant strain on the healthcare system in parts of Australia [24]. Consequently, we hypothesized that the presence of frailty in patients admitted to ICU with COVID-19 would be associated with worse outcomes than in patients with other “non-COVID-19” causes of viral pneumonitis. We aimed to determine whether the impact of frailty differed between patients with viral pneumonitis due to COVID-19 or other causes. Australia and New Zealand were uniquely placed to test this hypothesis because our health systems were not stretched as they were in other parts of the world and resource issues are less of a confounder.
Methods
Study design and setting
This was a retrospective multicentre cohort study, which analysed ICU admissions reported to the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) between 1 January 2020 and 31 December 2021.
ANZICS-APD
The ANZICS-APD is a binational database that prospectively collects high-quality de-identified patient information, including demographics (such as age and sex), chronic health status, physiological and biochemical variables within the first 24 h of admission required for the Acute Physiology and Chronic Health Evaluation (APACHE)-III-j and IV illness severity scores and Australian and New Zealand Risk of Death (ANZROD), as well as ICU and hospital outcomes. Each patient is allocated a single diagnosis which reflects the primary cause of admission to ICU using the ANZICS modification of the APACHE-IV diagnosis coding system [25].
Patient identification
Adult patients (age ≥ 16 years), with a documented CFS score, admitted to Australian and New Zealand ICUs with an ICU admission diagnosis of Viral Pneumonia or Acute Respiratory Distress Syndrome (ARDS) were included. Patients were further classified using a subcode of “suspected or confirmed pandemic infection” to indicate which were highly likely to have COVID-19 (Additional file 2: Table S1). Readmission episodes during the same hospitalization and admissions for organ donation or palliative care were excluded, as were patients with no primary outcome (hospital mortality) listed.
Data extraction
Data included patient demographics (age, sex, comorbidities, ethnicity, ICU admission source, smoking status), obesity status (body mass index ≥ 30 kg/m2; data collected as patient’s height and weight in ANZICS-APD) CFS, ICU organ supports (need for mechanical ventilation, non-invasive ventilation, vasopressors, tracheostomy, extracorporeal membrane oxygenation [ECMO] and/or renal replacement therapies), treatment limitation order, the incidence of delirium (developed during the current ICU admission), ICU and hospital mortality, and respective length of stays. Treatment limitation was defined as that medical treatment would be constrained by either patient wishes or medical futility but does not necessarily imply that the patient was expected to die during this ICU admission.
Frailty assessment
Frailty was measured with a modified version of the Canadian Study of Health and Aging Clinical Frailty Scale, which categorizes patients as non-frail (1 = very fit; 2 = well; 3 = managing well; 4 = vulnerable) or frail (5 = mild; 6 = moderate; 7 = severe; 8 = very severe) [26]. Terminally ill patients usually scored 9 on the CFS, and are instead scored in the ANZICS-APD on their level of frailty. This measurement has been validated among critically ill patients [19, 20] with good inter-rater reliability [19, 27, 28], and reported to be correlated with the other comprehensive frailty scales [29, 30]. In the ANZICS-APD, the CFS is modified to eight categories without a CFS-9 (terminally ill) [31]. The CFS represented the patient’s status in the two months preceding ICU admission [31]. For this study, we further grouped CFS scores according to five groups, CFS-1–3, CFS-4, CFS-5, CFS-6, and CFS-7–8 as reported in recent studies [32, 33]. The CFS was assigned by trained data collectors working in ICU, including junior doctors, nurses, and administrative staff, based on the patient’s level of physical function in the two months preceding ICU admission [25].
Exposure and confounding variables
The exposure variable was frailty status based on CFS categories in patients with and without COVID-19. The confounding variables were illness severity (measured with ANZROD), and sex.
Study aims and outcomes
We aimed to investigate whether the impact of frailty on mortality differed between patients with COVID-19 pneumonia and other aetiologies of viral pneumonia. The primary outcome was hospital mortality. Secondary outcomes included ICU mortality, ICU, and hospital length of stays and discharge destination.
Subgroup analysis
Predefined subgroup analyses based on biological sex, age (≥ 65 years), and those needing mechanical ventilation were performed.
Statistical analysis
The group comparisons between patients with and without COVID-19 were made using chi-square tests for proportions, student t tests for normally distributed data, and Mann–Whitney U or Kruskal–Wallis tests for nonparametric data depending on the number of categories examined. Data are reported as frequencies (%), means (standard deviations [SD]), or medians (interquartile range [IQR] 25–75%), respectively. Illness severity was determined using ANZROD, a highly discriminatory, locally derived, and well-calibrated mortality prediction model used for benchmarking ICU performance in Australia and New Zealand which combines age, chronic illnesses, acute physiological disturbance, and diagnosis [34, 35]. The association of CFS with hospital mortality in patients with and without COVID-19 was investigated using multivariable logistic regression with results reported as odds ratio (OR) and 95% confidence interval (CI). Model discrimination was assessed using the area under the receiver operating characteristic (AUROC) plots with the comparison between models assessed using chi-square tests [36]. Sensitivity subgroup analyses were performed which separately examined patients admitted in 2020 and 2021 (when there was a higher burden of COVID-19 admissions). Collinearity between ANZROD and CFS was assessed with variance inflation factor. Analyses were performed using SPSS software (version 27), and a two-sided p value of < 0.05 was used to indicate statistical significance.
Results
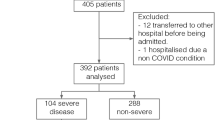
During the study period, a total of 5735 patients were admitted to 153 Australian and New Zealand ICUs with admission diagnoses of either viral pneumonia or ARDS that were reported to the ANZICS-APD. Of these, 4620 patients had a documented CFS and were included in the study. There were no differences in age, sex, the proportion of treatment limitations, or hospitalization prior to ICU or pre-ICU hours between the 4620 patients and 1115 patients without a documented CFS. However, a lower proportion of those with missing frailty data had COVID-19 and these patients had higher illness severity scores (Additional file 2: Table S2).
Baseline characteristics are presented in Table 1. Patients with COVID-19 were younger (median age 57.0 [IQR 44.7–68.3] vs. 66.1 [IQR 52.0–76.2]; p < 0.001) and less frail (median CFS 3 [IQR 2–4] vs. 4 [IQR 3–5]; p < 0.001), than patients without COVID-19. A higher proportion of patients with COVID-19 were male (61.3% vs. 51.3%; p < 0.001). Patients with COVID-19 had lower APACHE-III scores and less frequently had chronic comorbidities such as respiratory, cardiovascular, renal, liver, immunosuppressive conditions, and metastatic cancer, but were more likely to be obese and have delirium, than patients without COVID-19. Admissions to ICU following a rapid response team review were less frequent for patients with COVID-19 (36.2% vs. 39.3%; p = 0.045). More patients with COVID-19 were receipt of mechanical ventilation, tracheostomies, ECMO therapies, and vasoactive agents, whereas fewer patients were receipt of non-invasive ventilation or renal replacement therapy than patients without COVID-19 (Additional file 1: Fig. S1). Further categorization by age and CFS categories is provided in Additional file 1: Fig. S2 and Additional file 2: Tables S3a and S3b.
Primary outcome
Overall hospital mortality was similar between patients with and without COVID-19 (14.7% [441/3006] vs. 14.9% [280/1541]; p = 0.82). Higher hospital mortality was observed in COVID-19 patients compared to those without COVID-19 at equivalent frailty levels (p = 0.024; Fig. 1; Additional file 2: Table S4). Frailty was assessed using CFS as a continuous variable, increasing frailty scores were associated with mortality, after adjusting for ANZROD and sex. This effect was similar in patients with and without COVID-19 (OR = 1.29; 95% CI: 1.19–1.41 vs. OR = 1.24; 95% CI: 1.11–1.37; Table 2).
Frailty alone as a predictor of mortality showed only moderate discrimination in differentiating survivors from those who died. This effect was similar between patients with and without COVID-19 (AUROC 0.68 vs. 0.66; p = 0.42, Fig. 2). After adjusting for baseline illness severity (ANZROD) and sex, higher frailty scores were independently associated with mortality in patients with and without COVID-19. The presence of frailty (assessed as CFS categories) added little to the discriminatory capacity of the logistic regression model to predict death which already included ANZROD and sex (Fig. 1). The impact of frailty on mortality prediction was also no different between patients with and without COVID-19 (AUROC 0.80 vs. 0.81; p = 0.82; Fig. 2).
Secondary outcomes
The unadjusted ICU mortality rates were higher only for non-frail patients with COVID-19 for CFS categories CFS-1–3 (8.6% vs. 5.8%; p = 0.023) and CFS-4 (17.1% vs. 8.9%; p < 0.001), compared to patients without COVID-19 (Additional file 2: Table S5). Patients with COVID-19 had a longer median length of stay in ICU than patients without COVID-19 (5.0 [IQR 2.1–10.9] vs. 3.0 [IQR 1.6–5.6] days; p < 0.001; Additional file 1: Fig. S3), especially for CFS categories CFS-1–3, CFS-4, and CFS-5. The median hospital length of stay was no different for patients with COVID-19 (12.9 [IQR 7.4–21.7] vs. 10.1 [IQR 5.4–18.8] days; p < 0.001) for CFS categories, than those without COVID-19 (p = 0.91). The ICU readmissions were lower in patients with COVID-19 for CFS categories CFS-1–3, CFS-4, and CFS-6, than in those without COVID-19 (p < 0.001). Overall, the patients with COVID-19 were less likely to be discharged home or to a nursing home, when compared to patients without COVID-19 (both p < 0.001) respectively.
Subgroup analysis
Biological sex
More than half the patients were male (58.0%). A higher proportion of male patients had COVID-29 (70.4% vs. 61.3%; Additional file 2: Tables S5 and S6). The raw hospital mortality was higher for both male and female patients with COVID-19 for all CFS categories when compared to patients without COVID-19 (p < 0.001). Although the increasing frailty scores were associated with mortality, after adjusting for ANZROD, the effect of frailty was similar in both groups (Fig. 3; Additional file 2: Table S11).
Hospital mortality according to Clinical Frailty Scale (CFS) categories for patients with (red) and without (black) COVID-19: a male sex, b female sex, c ≥ 65 years of age, and d those needing mechanical ventilation. The top panel is unadjusted hospital mortality, while the bottom panel is adjusted analysis. Biological sex was adjusted only for ANZROD, while others are adjusted for ANZROD and sex
Patients ≥ 65 years
Of the 1861, a lower proportion of patients with COVID-19 were ≥ 65 years, than those without COVID-19 (33.6% vs. 53.7%). Their median age was similar between the 2 groups (Additional file 2: Table S7). When compared to patients without COVID-19, the unadjusted hospital mortality was higher for patients with COVID-19 across all CFS categories, (p < 0.001). In patients aged ≥ 65 years, although the increasing frailty scores were associated with mortality, after adjusting for ANZROD and sex, the effect of frailty was similar in patients with and without COVID-19 (Fig. 3; Additional file 2: Table S11).
Patients needing mechanical ventilation
A total of 1642 patients (35.5%) were mechanically ventilated. Although more patients with COVID-19 received mechanical ventilation overall, (42.7% vs. 21.3%; Additional file 2: Table S8), the number of patients with frailty was lower than those without COVID-19 (9.5% vs. 24.1%). The raw mortality was higher for patients with COVID-19 for CFS categories CFS-1–3, CFS-4, and CFS-7–8, when compared to patients without COVID-19 (p < 0.001). Although the increasing frailty scores were associated with mortality, after adjusting for ANZROD and sex, the effect of frailty was similar in patients with and without COVID-19 (Fig. 3; Additional file 2: Table S11).
Patients admitted in 2020
Of the 1163 patients (25.2%) admitted, 38.1% (n = 444) had COVID-19 (Additional file 2: Table S9). The raw hospital mortality was higher for patients with COVID-19 for all CFS categories except CFS-7–8 when compared to patients without COVID-19 (p < 0.001). Despite the increasing frailty scores were associated with mortality, after adjusting for ANZROD and sex, the effect of frailty was similar in both groups (Additional file 1: Fig. S4; Additional file 2: Table S11).
Patients admitted in 2021
Of the 3457 patients (74.8%) admitted, 85.1% (n = 2942) were patients with COVID-19 (Additional file 2: Table S9). Of these, most were non-frail (75.2%, 2212/2942) when compared to patients without COVID-19 (69.4%, 675/972). The raw hospital mortality was higher for patients with COVID-19 for all CFS categories (p < 0.001). Although the increasing frailty scores were associated with mortality, after adjusting for ANZROD and sex, the effect of frailty was similar in patients with and without COVID-19 (Fig. 3; Additional file 2: Table S10).
Discussion
Summary of key findings
This multicentre retrospective observational study that compared viral pneumonia patients with and without COVID-19 admitted to ICU in Australia and New Zealand revealed that: firstly, the mortality increased with increasing frailty, but the impact of frailty was similar in patients with and without COVID-19 pneumonitis. Secondly, patients with COVID-19 were less frail and younger than patients without COVID-19. Thirdly, the CFS independently predicted hospital mortality in both patients with and without COVID-19 pneumonitis but had a low discriminatory capacity. Fourthly, only one in ten patients with frailty with COVID-19 received mechanical ventilation. Finally, the mortality was higher in patients ≥ 65 years of age and those requiring mechanical ventilation, especially with increasing frailty.
Relationship to previous findings
There were few studies that compared outcomes of COVID-19 with influenza patients. These studies showed the overall hospital mortality; the need for ICU admission and mechanical ventilation was substantially higher in patients with COVID-19 [37,38,39]. However, none of these studies specifically investigated the association of frailty on clinically important outcomes. A recent study compared the characteristics and outcomes of very old patients with frailty with COVID-19 with historical controls and found that patients with COVID-19 were relatively less frail and had lower illness severity scores [40]. Our study was the first to compare critically ill patients with frailty, with and without COVID-19 pneumonitis, during the same period.
Our key study finding was that although the risk of death increased with frailty, the impact of frailty on hospital mortality was comparable between patients with and without COVID-19 pneumonitis. It is important to note that the Australian experience of the COVID-19 pandemic has differed from that internationally [41]. Our mortality rates were considerably lower than in other parts of the world. Importantly, we observed that the patients with COVID-19 were not only younger and less frail but also the overall proportion of patients with frailty was smaller when compared with those without COVID-19. Our study findings were, however, similar to a recent study that found that patients with COVID-19 were relatively less frail and had lower illness severity scores [40]. There was a higher proportion of patients with frailty in the non-COVID-19 group. Although outcomes in patients with frailty are bad [20, 22], the outcomes related to COVID-19 pneumonitis are worse. These two factors trade off against each other, explaining why the overall hospital mortality was similar between the two groups.
It is well established that higher degrees of frailty have been associated with poor outcomes and higher mortality rates during and after ICU admission [42, 43]. Similarly, we observed that hospital mortality increased with increasing frailty in both patients with and without COVID-19. A recent large prospective multinational study (COVIP) identified that frailty was independently associated with lower survival [11]. Our study found that although the CFS independently predicted hospital mortality, it had a low discriminatory capacity. Furthermore, the CFS was unable to clinically improve upon the predictability provided by baseline patient illness severity.
Patients with frailty were associated with lower use of mechanical ventilation [11, 44]. A recent systematic review observed that patients with frailty with COVID-19 were less commonly admitted to ICU or receive mechanical ventilation [45]. However, among those admitted to the ICU, almost two-thirds of patients with frailty with COVID-19 died in the hospital, with a greater risk of death for those receiving mechanical ventilation, when compared with patients without frailty [44]. Hospital mortality was relatively lower in these patients when compared to the published literature [11, 40, 44,45,46]. We observed that only 10% of patients with frailty with COVID-19 needed mechanical ventilation, which was lower than recently published in patients with COVID-19 [40, 45]. However, although the hospital mortality was higher, it was comparable in patients without COVID-19. This may indicate that frailty status was adopted as one of the triaging factors to screen patients for ICU admission and/or appropriate critical care interventions. These in turn may reinforce the importance of prudent selection and appropriate management of older patients with frailty amidst the pandemic, as previously observed [45].
Australia and New Zealand’s healthcare system was not as overwhelmed as other parts of the world in 2020. However, the impact was much greater in 2021. At the peak in October, 55% of all public ICU beds in Victoria and almost 40% of all public ICU beds in New South Wales were occupied by patients with COVID-19 [47]. This caused a significant strain in the healthcare system in late 2021 in both states, which was also associated with a deterioration in the risk-adjusted outcomes of COVID-19 patients [47, 48].
The inclusion period of 2 years encompassed patients from several different waves that also witnessed changes in treatment and the introduction of vaccinations. The rates of COVID-19 vaccine administration steadily increased since the rollout in February 2021. The vaccinations were initially prioritized in Victoria and New South Wales, which had the highest case numbers. At the end of the study period, > 90% of all eligible people had received the first dose Australia wide and > 84% received their second dose [49]. Further improvements in the outcomes in these patients are likely with increased uptake of vaccinations. However, despite vaccinations, public health measures to mitigate this pandemic, and new treatment options, COVID-19 may continue to severely impact frail older and vulnerable patients.
Study implications
Our study found that frailty independently predicted mortality in both patients with and without COVID-19 pneumonitis, but the impact of frailty was similar in patients with and without COVID-19 pneumonitis. This implies that, regardless of COVID-19 status, the patients’ care was no different. This may at least in part reflect that Australia and New Zealand have evaded the magnitude of the pandemic that has overwhelmed healthcare systems in many parts of the world. Moreover, the intensive care resource availability is owing to stringent public health measures in Australia and New Zealand. Our study has demonstrated that more patients with COVID-19 admitted to ICU had CFS scores between 1 and 3. It is possible that the intensive care teams were more selective in admitting frail patients with COVID-19 into their ICUs.
Strengths and limitations
Our study has several notable strengths. Firstly, the multicentre design, incorporating high-quality data Australia and New Zealand wide, as well as a larger sample size than many other studies. Secondly, the CFS, which is the most used frailty assessment tool for critically ill patients. Thirdly, we incorporated pre-specified several secondary analyses, to assess the impact of frailty on several important patient-centred ICU outcomes. To our knowledge, this is the only study to compare the impact of frailty among patients with and without COVID-19 pneumonitis. There are a few limitations to this study. Firstly, the retrospective study design meant that data collection was reliant on existing datasets and medical records. Secondly, despite the ANZICS-APD being recognized as a high-quality clinical registry dataset, the effect of data coding inaccuracy on the study findings could not be assessed. Thirdly, in the absence of having linkage to infection notification data and without site-based auditing of diagnostic coding over the pandemic, we cannot be certain about the degree of misclassification, if any. Fourthly, the CFS was adopted in the assessment of frailty in ICUs across Australia and New Zealand. Despite being an attractive tool to distinguish the different grades of frailty, the reliability of a single assessment tool may be inadequate, especially when it comes to justifying the rationing of medical treatment. Fifthly, the patients with COVID-19 admitted to the ICUs with an alternate diagnosis could have been missed. Sixthly, we do not have any information regarding the number of patients that were referred for ICU admission and denied ICU admission, or the COVID-19 pandemic may have led to an increased presentation of COVID-19 to the ICUs, while non-COVID-19 patients had a transient reduction in hospital presentations as well as ICU admissions. Seventhly, although some evidence suggests that CFS is a major determinant of long-term mortality in patients with COVID-19, we only reported on hospital mortality, as the ANZICS-APD only captured hospital-based outcomes. Finally, the Australia and New Zealand healthcare system has been very fortunate with the magnitude of COVID-19 infections being largely under control, and therefore, the results may not be generalizable in resource-constrained healthcare systems.
Conclusion
This multicentre retrospective study that compared viral pneumonitis in patients with and without COVID-19 admitted to ICU in Australia and New Zealand found that patients with COVID-19 were younger and less frail than patients without COVID-19. The frailty independently predicted hospital mortality in both patients with and without COVID-19 pneumonitis but had low discriminatory capacity. The impact of frailty, however, was no different in patients with and without COVID-19.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available as these are linked from three registries (ANZICS, VAED, and VDI), but are available from the corresponding author upon reasonable request.
Abbreviations
- ANZ:
-
Australia and New Zealand
- ANZICS:
-
Australia and New Zealand Intensive Care Society
- ANZROD:
-
Australia and New Zealand Risk of Death
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- APD:
-
Adult Patient Database
- AUROC:
-
Area under the receiver operating characteristic
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus disease 2019
- CFS:
-
Clinical Frailty Scale
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- LOS:
-
Length of stay
- MI:
-
Myocardial infarction
- n:
-
Number
- OR:
-
Odds ratio
- RRT:
-
Renal replacement therapy
- SD:
-
Standard deviation
References
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
He F, Deng Y, Li W. Coronavirus disease 2019: What we know? J Med Virol. 2020;92(7):719–25.
Hagg S, Jylhava J, Wang Y, Xu H, Metzner C, Annetorp M, Garcia-Ptacek S, Khedri M, Bostrom AM, Kadir A, et al. Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc. 2020;21(11):1555–9.
Davis P, Gibson R, Wright E, Bryan A, Ingram J, Lee RP, Godwin J, Evans T, Burleigh E, Wishart S, et al. Atypical presentations in the hospitalised older adult testing positive for SARS-CoV-2: a retrospective observational study in Glasgow, Scotland. Scott Med J. 2020;66:89–97.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Kramer DB, Lo B, Dickert NW. CPR in the Covid-19 Era: an ethical framework. N Engl J Med. 2020;383(2): e6.
Chase J. Caring for frail older adults during COVID-19: integrating public health ethics into clinical practice. J Am Geriatr Soc. 2020;68(8):1666–70.
Hubbard RE, Maier AB, Hilmer SN, Naganathan V, Etherton-Beer C, Rockwood K. Frailty in the face of COVID-19. Age Ageing. 2020;49(4):499–500.
Jung C, Flaatten H, Fjølner J, Bruno RR, Wernly B, Artigas A, Bollen Pinto B, Schefold JC, Wolff G, Kelm M, et al. The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care. 2021;25(1):149.
Lewis EG, Breckons M, Lee RP, Dotchin C, Walker R. Rationing care by frailty during the COVID-19 pandemic. Age Ageing. 2021;50(1):7–10.
O’Mara LSS, Orkaby AR, Ouchi K, Bernacki R. A framework to triage older adults with Covid-19 to provide patient-centered care. NEJM Catalyst. 2020;1:1–11.
Straw S, McGinlay M, Drozd M, Slater TA, Cowley A, Kamalathasan S, Maxwell N, Bird RA, Koshy AO, Prica M, et al. Advanced care planning during the COVID-19 pandemic: ceiling of care decisions and their implications for observational data. BMC Palliat Care. 2021;20(1):10.
National Institute for Health and Care Excellence: COVID-19 rapid guideline: critical care in adults. 2020.
Smithard DG, Abdelhameed N, Han T, Pieris A. Age, frailty, resuscitation and intensive care: with reference to COVID-19. Geriatrics (Basel). 2021;6(2):36.
Maltese G, Corsonello A, Di Rosa M, Soraci L, Vitale C, Corica F, Lattanzio F. Frailty and COVID-19: a systematic scoping review. J Clin Med. 2020;9(7):2106.
Okahara S, Subramaniam A, Darvall JN, Ueno R, Bailey M, Pilcher DV. The relationship between frailty and mechanical ventilation: a population-based cohort study. Ann Am Thorac Soc. 2021;19:264–71.
Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, Artiuch B, Ibrahim Q, Stollery DE, Rokosh E, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186(2):E95-102.
Darvall JN, Bellomo R, Paul E, Subramaniam A, Santamaria JD, Bagshaw SM, Rai S, Hubbard RE, Pilcher D. Frailty in very old critically ill patients in Australia and New Zealand: a population-based cohort study. Med J Aust. 2019;211(7):318–23.
Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, Sibley S, Rockwood K. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22.
Darvall JN, Bellomo R, Bailey M, Paul E, Young PJ, Rockwood K, Pilcher D. Frailty and outcomes from pneumonia in critical illness: a population-based cohort study. Br J Anaesth. 2020;125(5):730–8.
Chin KL, Ofori-Asenso R, Jordan KA, Jones D, Liew D. Early signs that COVID-19 is being contained in Australia. J Infect. 2020;81(2):318–56.
ANZICS CORE: Report on COVID-19 admissions to Intensive Care in Australia 01 January 2021–31 December 2021. Melbourne; 2022: 15.
APD Data Dictionary ANZICS core—adult patient database https://www.anzics.com.au/wp-content/uploads/2018/08/ANZICS-APD-Dictionary.pdf
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
Bagshaw SM, Stelfox HT, Johnson JA, McDermid RC, Rolfson DB, Tsuyuki RT, Ibrahim Q, Majumdar SR. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med. 2015;43(5):973–82.
Theou O, Pérez-Zepeda MU, van der Valk AM, Searle SD, Howlett SE, Rockwood K. A classification tree to assist with routine scoring of the Clinical Frailty Scale. Age Ageing. 2021;50(4):1406–11.
Tipping CJ, Hodgson CL, Harrold M, Chan T, Holland AE. Frailty in patients with trauma who are critically Ill: a prospective observational study to determine feasibility, concordance, and construct and predictive validity of 2 frailty measures. Phys Ther. 2019;99(8):1089–97.
Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019;52:193–9.
Bagshaw M, Majumdar SR, Rolfson DB, Ibrahim Q, McDermid RC, Stelfox HT. A prospective multicenter cohort study of frailty in younger critically ill patients. Crit Care. 2016;20(1):175.
Aliberti MJR, Szlejf C, Avelino-Silva VI, Suemoto CK, Apolinario D, Dias MB, Garcez FB, Trindade CB, Amaral J, de Melo LR, et al. COVID-19 is not over and age is not enough: using frailty for prognostication in hospitalized patients. J Am Geriatr Soc. 2021;69(5):1116–27.
Aw D, Woodrow L, Ogliari G, Harwood R. Association of frailty with mortality in older inpatients with Covid-19: a cohort study. Age Ageing. 2020;49(6):915–22.
Paul E, Bailey M, Kasza J, Pilcher D. The ANZROD model: better benchmarking of ICU outcomes and detection of outliers. Crit Care Resusc. 2016;18(1):25–36.
Pilcher D, Paul E, Bailey M, Huckson S. The Australian and New Zealand Risk of Death (ANZROD) model: getting mortality prediction right for intensive care units. Crit Care Resusc. 2014;16(1):3–4.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Ludwig M, Jacob J, Basedow F, Andersohn F, Walker J. Clinical outcomes and characteristics of patients hospitalized for Influenza or COVID-19 in Germany. Int J Infect Dis. 2021;103:316–22.
Hernández-Cárdenas C, Lugo-Goytia G, Hernández-García D, Pérez-Padilla R. Comparison of the clinical characteristics and mortality in acute respiratory distress syndrome due to COVID-19 versus due to Influenza A-H1N1pdm09. Med Intensiva Engl Ed. 2021;11:e155044.
Auvinen R, Nohynek H, Syrjänen R, Ollgren J, Kerttula T, Mäntylä J, Ikonen N, Loginov R, Haveri A, Kurkela S, et al. Comparison of the clinical characteristics and outcomes of hospitalized adult COVID-19 and influenza patients—a prospective observational study. Infect Dis (Lond). 2021;53(2):111–21.
Guidet B, Jung C, Flaatten H, Fjolner J, Artigas A, Pinto BB, Schefold JC, Beil M, Sigal S, van Heerden PV, et al. Increased 30-day mortality in very old ICU patients with COVID-19 compared to patients with respiratory failure without COVID-19. Intensive Care Med. 2022;48:435–47.
Tracking outcomes during the COVID-19 pandemic (August 2020)—Divergence within Australia https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/9/Tracking_wellbeing_outcomes_during_the_COVID-19_pandemic_February_to_August_2020.pdf
Hussien H, Nastasa A, Apetrii M, Nistor I, Petrovic M, Covic A. Different aspects of frailty and COVID-19: points to consider in the current pandemic and future ones. BMC Geriatr. 2021;21(1):389.
Rottler M, Ocskay K, Sipos Z, Görbe A, Virág M, Hegyi P, Molnár T, Erőss B, Leiner T, Molnár Z. Clinical Frailty Scale (CFS) indicated frailty is associated with increased in-hospital and 30-day mortality in COVID-19 patients: a systematic review and meta-analysis. Ann Intensive Care. 2022;12(1):17.
Subramaniam A, Anstey C, Curtis JR, Ashwin S, Ponnapa Reddy M, Aliberti MJR, Avelino-Silva TJ, Welch C, Koduri G, Prowle JR, et al. Characteristics and outcomes of patients with frailty admitted to ICU with Coronavirus Disease 2019: an individual patient data meta-analysis. Crit Care Explor. 2022;4(1): e0616.
Subramaniam A, Shekar K, Afroz A, Ashwin S, Billah B, Brown H, Kundi H, Lim ZJ, Ponnapa Reddy M, Curtis JR. Frailty and mortality associations in patients with COVID-19: a systematic review and meta-analysis. Intern Med J. 2022;52:724–39.
Lim ZJ, Subramaniam A, Reddy MP, Blecher G, Kadam U, Afroz A, Billah B, Ashwin S, Kubicki M, Bilotta F, et al. Case fatality rates for COVID-19 patients requiring invasive mechanical ventilation: a meta-analysis. Am J Respir Crit Care Med. 2020;203:54–66.
Pilcher D, Coatsworth NR, Rosenow M, McClure J. A national system for monitoring intensive care unit demand and capacity: the Critical Health Resources Information System (CHRIS). Med J Aust. 2021;214(7):297–8.
ANZICS CORE: Report on COVID-19 admissions to Intensive Care in Australia 01 January 2021–31 December 2021. 2022:12.
Shield OC: COVID-19 vaccine roll-out. In. Edited by Government A. Canberra; 2021.
Acknowledgements
The authors and the ANZICS CORE management committee would like to thank clinicians, data collectors, and researchers at the following contributing sites: Albury Base Hospital, Alfred Hospital, Alice Springs Hospital, Angliss Hospital, Armadale Health Service, Ashford Community Hospital, Auckland City Hospital CV, Auckland City Hospital DCCM, Austin Hospital, Ballarat Health Services, Bankstown-Lidcombe Hospital, Bathurst Base Hospital, Bendigo Health Care Group, Blacktown Hospital, Box Hill Hospital, Buderim Private Hospital, Bunbury Regional Hospital, Bundaberg Base Hospital, Caboolture Hospital, Cabrini Hospital, Cairns Hospital, Calvary Hospital (Canberra), Calvary Mater Newcastle, Calvary Wakefield Hospital (Adelaide), Campbelltown Hospital, Canberra Hospital, Casey Hospital, Central Gippsland Health Service, Christchurch Hospital, Coffs Harbour Health Campus, Concord Hospital (Sydney), Dandenong Hospital, Dubbo Base Hospital, Dunedin Hospital, Epworth Hospital (Richmond), Fairfield Hospital, Fiona Stanley Hospital, Flinders Medical Centre, Flinders Private Hospital, Footscray Hospital, Frankston Hospital, Gold Coast Private Hospital, Gold Coast University Hospital, Gosford Hospital, Gosford Private Hospital, Goulburn Base Hospital, Goulburn Valley Health, Grafton Base Hospital, Greenslopes Private Hospital, Griffith Base Hospital, Hawkes Bay Hospital, Hervey Bay Hospital, Hollywood Private Hospital, Holmesglen Private Hospital, Holy Spirit Northside Hospital, Hornsby Ku-ring-gai Hospital, Hutt Hospital, Ipswich Hospital, John Fawkner Hospital, John Hunter Hospital, Joondalup Health Campus, Kareena Private Hospital, Knox Private Hospital, Latrobe Regional Hospital, Launceston General Hospital, Lingard Private Hospital, Lismore Base Hospital, Liverpool Hospital, Logan Hospital, Lyell McEwin Hospital, Mackay Base Hospital, Macquarie University Private Hospital, Maitland Hospital, Maitland Private Hospital, Manning Rural Referral Hospital, Maroondah Hospital, Mater Adults Hospital (Brisbane), Mater Health Services North Queensland, Mater Private Hospital (Brisbane), Mater Private Hospital (Sydney), Melbourne Private Hospital, Middlemore Hospital, Mildura Base Hospital, Monash Medical Centre (Clayton), Mount Hospital, Mount Isa Hospital, Nelson Hospital, Nepean Hospital, Noosa Hospital, North Shore Hospital, North Shore Private Hospital, North West Regional Hospital (Burnie), Northeast Health Wangaratta, Northern Beaches Hospital, Norwest Private Hospital, Orange Base Hospital, Peninsula Private Hospital, Pindara Private Hospital, Port Macquarie Base Hospital, Prince of Wales Hospital (Sydney), Princess Alexandra Hospital, Queen Elizabeth II Jubilee Hospital, Redcliffe Hospital, Robina Hospital, Rockhampton Hospital, Rockingham General Hospital, Rotorua Hospital, Royal Adelaide Hospital, Royal Brisbane and Women’s Hospital, Royal Darwin Hospital, Royal Melbourne Hospital, Royal North Shore Hospital, Royal Perth Hospital, Royal Prince Alfred Hospital, Ryde Hospital & Community Health Services, Shoalhaven Hospital, Sir Charles Gairdner Hospital, South West Healthcare (Warrnambool), St Andrew’s Hospital (Adelaide), St Andrew’s Hospital Toowoomba, St Andrew’s Private Hospital (Ipswich), St Andrew’s War Memorial Hospital, St George Hospital (Sydney), St George Private Hospital (Sydney), St John of God (Berwick), St John Of God Health Care (Subiaco), St John of God Hospital (Bendigo), St John Of God Hospital (Geelong), St John Of God Hospital (Murdoch), St John of God Midland Public & Private, St Vincent’s Hospital (Melbourne), St Vincent’s Hospital (Sydney), St Vincent’s Hospital (Toowoomba), St Vincent’s Private Hospital Fitzroy, Sunnybank Hospital, Sunshine Coast University Hospital, Sunshine Coast University Private Hospital, Sunshine Hospital, Sutherland Hospital & Community Health Services, Sydney Adventist Hospital, Tamworth Base Hospital, Tauranga Hospital, The Chris O’Brien Lifehouse, The Northern Hospital, The Prince Charles Hospital, The Queen Elizabeth (Adelaide), The Townsville Hospital, The Valley Private Hospital, The Wesley Hospital, Timaru Hospital, Tweed Heads District Hospital, University Hospital Geelong, Wagga Wagga Base Hospital & District Health, Waikato Hospital, Warringal Private Hospital, Wellington Hospital, Werribee Mercy Hospital, Western District Health Service (Hamilton), Western Hospital (SA), Westmead Hospital, Whangarei Area Hospital, Northland Health Ltd, Wimmera Health Care Group (Horsham), Wollongong Hospital, and Wyong Hospital. This work was performed Australian and New Zealand Intensive Care Research Centre (ANZIC-RC), Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Victoria, Australia.
Funding
No financial support, including any institutional departmental funds, was used for the study.
Author information
Authors and Affiliations
Contributions
AS contributed to conceptualization, methodology, data curation, project administration, formal analysis, writing—original draft, and writing—review and editing. KS and RT were involved in methodology, supervision, and writing—review and editing. CA contributed to supervision and writing—review and editing, and provided software. DP was involved in conceptualization, methodology, supervision, and writing—review and editing. All authors critically reviewed the manuscript and approved the final version before submission. All authors have agreed both be personally accountable for the author’s contributions and ensured questions related to the accuracy or integrity of any part of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental protocols were approved by The Alfred Hospital Ethics Committee (Project No: 176/21) approved this study with a waiver of informed consent. ANZICS Centre for Outcome and Resource Evaluation Management Committee granted access to the ANZICS-APD in accordance with standing protocols. All methods were carried out in accordance with the relevant guidelines and regulations of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
ICU Supports among patients with COVID-19 (red lines) with patients without COVID-19 (black lines), based on CFS score. Standard error bars are 95%-CI. Figure S2 Age comparison based on CFS categories. The CFS categories are denoted by the different stacked colours starting with CFS 1–3 at the bottom up to CFS 7–8 at the top. Figure S3 ICU bed days stratified by Clinical Frailty Scale (CFS) categories for patients with and without COVID-19. The bottom panels demonstrate the median length of stay among ICU survivors and non-survivors. Figure S4 Hospital mortality according to Clinical Frailty Scale (CFS) categories for patients with (red) and without (black) COVID-19 for patients admitted in 2020 (a) and 2021 (b). The top panel is unadjusted hospital mortality, while the bottom panel is adjusted for ANZROD and sex.
Additional file 2: Table S1
Diagnostic codes and subcodes for patients included in the study between 1st January 2020 and 31st December 2021. Table S2 Missing data comparison for patients with and without the CFS scores. Table S3a CFS-1–3, CFS-4, and CFS-5 for patients with COVID-19 admitted to ICU with an admission diagnosis of viral pneumonia or ARDS. Table S3b CFS-6 and CFS-7–8 for patients with COVID-19 admitted to ICU with an admission diagnosis of viral pneumonia or ARDS. Table S4 Comparison of unadjusted outcomes. Standard error bars are 95%-CI. Table S5 Exposure and raw outcomes for male patients (2679 patients [58.0%]; with COVID-19 = 1887 patients; and without COVID-19 = 792 patients). Table S6 Exposure and raw outcomes for female patients (1941 patients [42.0%]; with COVID-19 = 1190 patients; and without COVID-19 = 751 patients). Table S7 Exposure and raw outcomes for patients ≥ 65 years (1861 patients [40.3%]; with COVID-19 = 1033 patients; and without COVID-19 = 828 patients). Table S8 Exposure and raw outcomes in patients needing mechanical ventilation (1642 patients [35.5%]; COVID-19 = 1314 patients; non-COVID-19 = 328 patients). Table S9 Exposure and raw outcomes for patients who were cared for in the year 2020 (1163 patients [25.2%]; with COVID-19 = 444 patients; and without COVID-19 = 719 patients). Table S10 Exposure and raw outcomes for patients who were cared for in the year 2021 (3457 patients [74.8%]; with COVID-19 = 2942 patients; and without COVID-19 = 972 patients). Table S11 Predictors for hospital mortality with the Clinical Frailty Scale (CFS) categories, adjusted for ANZROD and sex.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Subramaniam, A., Shekar, K., Anstey, C. et al. Impact of frailty on clinical outcomes in patients with and without COVID-19 pneumonitis admitted to intensive care units in Australia and New Zealand: a retrospective registry data analysis. Crit Care 26, 301 (2022). https://doi.org/10.1186/s13054-022-04177-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04177-9