Abstract
Aim
To compare the safety and effects of unrestricted visiting policies (UVPs) and restricted visiting policies (RVPs) in intensive care units (ICUs) with respect to outcomes related to delirium, infection, and mortality.
Methods
MEDLINE, Cochrane Library, Embase, Web of Science, CINAHL, CBMdisc, CNKI, Wanfang, and VIP database records generated from their inception to 22 January 2022 were searched. Randomized controlled trials and quasi-experimental studies were included. The main outcomes investigated were delirium, ICU-acquired infection, ICU mortality, and length of ICU stay. Two reviewers independently screened studies, extracted data, and assessed risks of bias. Random‑effects and fixed-effects meta‑analyses were conducted to obtain pooled estimates, due to heterogeneity. Meta-analyses were performed using RevMan 5.3 software. The results were analyzed using odds ratios (ORs), 95% confidence intervals (CIs), and standardized mean differences (SMDs).
Results
Eleven studies including a total of 3741 patients that compared UVPs and RVPs in ICUs were included in the analyses. Random effects modeling indicated that UVPs were associated with a reduced incidence of delirium (OR = 0.4, 95% CI 0.25–0.63, I2 = 71%, p = 0.0005). Fixed-effects modeling indicated that UVPs did not increase the incidences of ICU-acquired infections, including ventilator-associated pneumonia (OR = 0.96, 95% CI 0.71–1.30, I2 = 0%, p = 0.49), catheter-associated urinary tract infection (OR 0.97, 95% CI 0.52–1.80, I2 = 0%, p = 0.55), and catheter-related blood stream infection (OR = 1.15, 95% CI 0.72–1.84, I2 = 0%, p = 0.66), or ICU mortality (OR = 1.03, 95% CI 0.83–1.28, I2 = 49%, p = 0.12). Forest plotting indicated that UVPs could reduce the lengths of ICU stays (SMD = − 0.97, 95% CI − 1.61 to 0.32, p = 0.003).
Conclusion
The current meta-analysis indicates that adopting a UVP may significantly reduce the incidence of delirium in ICU patients, without increasing the risks of ICU-acquired infection or mortality. Further large-scale, multicenter studies are needed to confirm these indications.
Similar content being viewed by others
Introduction
The incidence of infections acquired in intensive care units (ICUs) is 2–5 times that in general wards [1, 2]. They complicate the regular hospitalization process, and are a major therapeutic issue that can compromise patients’ medical conditions (sometimes resulting in mortality), prolong treatment periods, and increase hospitalization costs [1, 3, 4]. Ventilator‑associated pneumonia (VAP), catheter-related blood stream infections (CRBSIs), and catheter-associated urinary tract infections (CAUTIs) are the most frequent ICU‑acquired infections. The estimated rate of mortality attributable to VAP is approximately 10%, with higher mortality rates in surgical ICU patients and patients with mid‑range severity scores at admission [4]. Restricted visiting policies (RVPs) may reduce the risk of infection in the vulnerable population of ICU patients [5,6,7]. Most ICUs have RVPs that define the number of visitors, visiting times, and other factors based on a unified hospital management policy and their ICU’s characteristics [8]. As more hospitals consider the benefits of family involvement in ICU holistic patient care, however, more ICUs are beginning to explore the advantages and disadvantages of adopting an unrestricted visiting policy (UVP) [9,10,11]. Growing evidence suggests that UVP implementation has positive effects on critical patient outcomes. Specifically, it can reduce the incidences of delirium, anxiety, and depression, and improve the satisfaction of patients and their families, without increasing the incidences of ICU-related infections or mortality [10,11,12,13]. Internationally restrictions on visitation in adult ICUs are common, with wide variability of reported policies [14].
Delirium is a substantial problem in critically ill patients, and it occurs in up to 83% of mechanically ventilated patients [15]. It is a well-recognized independent factor that is potentially detrimental to ICU patient outcomes [15,16,17]. It is associated with increases in mechanical ventilation time, prolonged ICU stays, and increased risks of falling and unplanned extubation. It is also associated with long-term cognitive impairment and increased mortality [16,17,18]. The types of visitations to ICUs can be categorized in several ways. RVPs do not meet the mental needs of patients and their families, and are a significant cause of patient suffering [10, 19, 20]. The risk of delirium in critically ill patients without family visits is increased by more than threefold, suggesting that family involvement can help prevent delirium in critically ill patients [21, 22]. Due to cultural variability and the unique treatment environment of ICUs, however, more than 70% of ICUs worldwide still implement RVPs with different visiting methods, times, frequencies, and numbers of visitors permitted [5, 8, 11]. The comparative effectiveness and safety of RVPs and UVPs remains uncertain. The aim of the current study was to compare the safety and effects associated with UVPs and RVPs in ICU patients with respect to outcomes related to mortality, infection, and delirium.
Methods
The current study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and Cochrane Collaboration recommendations [23, 24], and the prespecified protocol was registered on PROSPERO (registration number CRD42020148782).
Literature databases and search strategies
Two researchers (WG Y, YC W) searched the Cochrane Library, MEDLINE (PubMed), Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, China Biology Medicine disk (CBMdisc), China National Knowledge Infrastructure (CNKI), Wanfang, and VIP databases in accordance with the PRISMA standards, from database inception until 22 January 2022, with no restrictions. The references lists of all retrieved publications were also checked in an effort to detect additional published studies.
Search terms included “visit,” “visiting,” “visitation,” “visitor,” “visitors,” “critical care,” “intensive care,” “burn units,” “NICU,” “MICU,” “EICU,” “SICU,” “RICU,” “recovery room,” “respiratory care unit,” and “ICU.” A combination of exploded Medical Subject Heading/Emtree terms along with “or” and “and” was used, as per the database specifications. The search strategy was developed by the author team and an evidence-based medicine expert (the search strategy in Additional file 1).
Inclusion and exclusion criteria
Inclusion criteria
-
(1)
Randomized control trials (RCTs) or quasi-experimental studies (QEs) comparing the clinical effects of UVPs and RVPs.
-
(2)
Evaluated at least one of delirium, CRBSI, CAUTI, VAP, or mortality rate.
-
(3)
Used the Confusion Assessment Method for the ICU (CAM-ICU) scale to evaluate delirium [23].
Exclusion criteria
-
(1)
Review articles, case studies, or letters to editors
-
(2)
Pediatric studies
-
(3)
Duplicate references
-
(4)
Did not report relevant primary outcomes
-
(5)
Full text unavailable
Data extraction
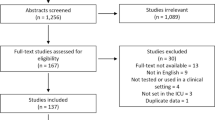
Two researchers independently screened the titles and abstracts to evaluate the potential relevance of studies. Disagreements were resolved by consensus or discussion with a third author. After screening (Fig. 1), full-text reviews were performed. Detailed study information, interventions, controls, and outcomes were retrieved using a standardized data extraction protocol.
Statistical analysis
Statistical analysis was conducted with Review Manager (RevMan) software (version 5.3, Cochrane Collaboration, Copenhagen, Denmark). For dichotomous variables (delirium, mortality, rate of ICU-acquired infection), odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the Mantel–Haenszel test. For continuous variables (length of ICU stay, anxiety, depression) the standardized mean difference (SMD) and 95% CI were calculated using the inverse-variance test. Chi-square test was applied to test heterogeneity (p < 0.05, I2 > 50%), and if it was found to exist, sensitivity analysis was applied to find out the cause. A random-effects model was used again if heterogeneity still could not be eliminated. Sensitivity analysis, subgroup analysis, or just descriptive analysis were applied when meeting significant clinical heterogeneity. A fixed-effects model was used for data with no significant heterogeneity (p ≥ 0.05, I2 ≤ 50%). The subgroup analysis will compare the study type included in all the included literature as sub-sites to see the source of heterogeneity. If ≥ 10 studies were present reporting bias was visually assessed via funnel plots. Pooled index significance was determined via the Z test. A two-sided p value of ≤ 0.05 was considered statistically significant.
Assessment of risk of bias
A critical appraisal of each study was independently conducted by two reviewers using the JBI Critical Appraisal Checklists for Randomized Controlled Trials and Quasi-Experimental Studies [25]. Differences in opinion were resolved via discussion between the two reviewers, occasionally with arbitration by a third reviewer (JHT). To investigate study heterogeneity and test the robustness of results, sensitivity analyses omitting one study at a time were conducted. Two researchers used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach for priority outcomes (GRADEpro version 3.6.1; GRADE Working Group 2004–2011) [26].
Results
Search outcomes
The search strategy identified 5768 relevant publications. After removing duplicate publications and screening the titles and abstracts, the remaining 3345 publications were rescreened. This process yielded 52 studies deemed appropriate for full review, of which 41 were subsequently excluded. Eleven studies [2, 11, 19, 27,28,29,30,31,32,33,34] were ultimately included in the current analysis (Fig. 1).
Demographics of included studies
Eleven studies with a combined total of 3741 participants enrolled between 2006 and 2021 were included in the current investigation; 1868 assigned to a UVP group and 1873 assigned to an RVP group. Patient characteristics are shown in Table 1.
Critical appraisal of included studies and GRADE assessment for priority outcomes
Five RCTs incorporated random allocation, without incomplete outcome data and without selective reporting or other biases [11, 19, 27, 28, 34]. Three RCTs incorporated blinding methods and allocation concealment [19, 27, 34]. One study was deemed to be of good overall quality [28], and three were deemed to be of fair overall quality [19, 27, 34]. The most frequent issue apart from blinding of participants and personnel was allocation concealment. Six QEs [2, 29,30,31,32,33] included a control group with similar participants and interventions, reliable measurements, appropriate statistical, clearly report “what is the cause and what is the effect” except follow-up that not applicable. Risks of bias assessment in RCTs are shown in Table 2, and risks of bias assessment in QEs are shown in Table 3. The numbers of RCTs reporting results for each priority outcome were low, and there was no indication of a small study effect that may have influenced the results. A GRADE assessment of the certainty of evidence is shown in Table 4.
Delirium
Nine studies including a total of 2975 patients investigated the effects of UVPs on the incidence of delirium, including four RCTs [11, 19, 27, 28] and five QEs [2, 29,30,31,32]. Subgroup analysis was performed using the type of study. According to the heterogeneity test results (p = 0.0005, I2 = 71%) the level of heterogeneity was high. Subgroup analysis was conducted according to research method, and a random effects model was used for the meta-analysis, and the overall meta-analysis showed that UVPs could reduce the incidence of delirium (OR = 0.40, 95% CI 0.25–0.63, p = 0.0001) (Fig. 2). The heterogeneity of each study was low.
ICU-acquired infection
Six studies including a total of 3246 patients investigated relationships between UVPs and infections acquired in ICU patients, three RCTs [11, 28, 34] and three QEs [2, 29, 33]. Study type subgroup analysis was performed. Overall meta-analysis was performed using a fixed-effects model because the heterogeneity of each study was low (p = 0.51, I2 = 0%). UVP had no influence on ICU-acquired infection of patients (OR = 0.92, 95% CI 0.72–1.18, p = 0.5) (Fig. 3). Six studies investigated the effects of UVPs on the incidence of VAP. Study type subgroup analysis was performed. Overall meta-analysis using a fixed-effects model showed that UVPs did not increase the incidence of VAP (I2 = 0%, p = 0.49, OR = 0.96, 95% CI 0.71–1.30, p = 0.80) (Fig. 4).
Five studies (three RCTs [11, 28, 34] and two QEs [2, 33]) including 3082 patients reported CRBSIs and CAUTIs in ICU patients. Heterogeneity test results of CRBSI (p = 0.66, I2 = 0%) and CAUTI (p = 0.55, I2 = 0%) were acceptable, and a fixed-effects model was used in the meta-analysis. UVPs did not increase the incidence of CRBSI (OR 1.15, 95% CI 0.72–1.84, p = 0.56) (Fig. 5) or CAUTI (OR 0.97, 95% CI 0.52–1.80, p = 0.92) (Fig. 6).
ICU mortality rate
Four studies (two RCTs [11, 34] and two QEs [2, 33]) investigated the effects of UVPs on the ICU mortality rate in 2727 patients, and UVPs did not significantly increase the ICU mortality rate (I2 = 49%, p = 0.12, fixed effect model; OR = 1.03, 95% CI 0.83–1.28, p = 0.75) (Fig. 7).
ICU length of stay
Seven studies (one RCT [11] and six QEs [2, 29,30,31,32,33]) including 2972 patients reported ICU length of stay (LoS). The level of heterogeneity was high (p < 0.00001, I2 = 97%), and the random effects model was used in the meta-analysis. Pooled analysis of the data indicated that UVPs could reduce the lengths ICU of stays (SMD = − 0.97, 95% CI − 1.61 to − 0.32, p = 0.003) (Fig. 8).
Anxiety and depression
Two studies used the Hamilton Anxiety Scale and the Hamilton Depression Scale to evaluate patient anxiety and depression [30, 34], and one study used the Self-Rating Anxiety Scale and the Self-Rating Depression Scale to evaluate patient anxiety and depression [31]. Due to large differences in mean anxiety and depression the SMD and the effect size were calculated, and the heterogeneity test results were p < 0.00001, I2 = 99% for anxiety and p = 0.0002, I2 = 93% for depression. A random effects model was used for the meta-analysis. Patient anxiety scores were better in the UVP group than in the control group, but not statistically significantly (SMD = − 2.39, 95% CI − 5.03 to 0.25, p = 0.08) (Fig. 9). There was a significant reduction in Hamilton Depression Scale scores associated with UVPs in the random effects model (SMD − 2.1, 95% CI − 3.22 to − 0.97, p = 0.0003, I2 93%) (Fig. 10).
Funnel plot
Funnel plots were drawn with the primary outcome of delirium, and the results showed risk bias. We further conducted sensitivity analyses to explore heterogeneity, which related with a big sample research [11] (Fig. 11). We planned to conduct heterogeneity assessment based on predefined factors (study type, sample size) and to assess small study effects using funnel plots and Egger’s test, where appropriate. However, the number of studies for each reported outcome was too low to allow a meaningful assessment.
Discussion
“Being close” is one of the most basic and important needs of family members of critically ill patients. UVPs provide an increased opportunity to be at the bedside with the patient, but they are not universally embraced by adult intensive care units worldwide [13]. The current meta-analysis suggests that compared with RVPs, UVPs are associated with a lower incidence of delirium and no increased risk of ICU mortality or ICU-acquired infection. This conclusion is consistent with the results of Nassar et al. [10] and also supports the concept of an “open” ICU in which family visits are unrestricted based on “humanistic care” and a “patient-centered” approach, in line with the latest guidelines, comments, expert consensus, and conference reports [2, 8].
It has been authoritatively stated that delirium is strongly associated with mortality [16,17,18], and mortality was almost the same in the RVP and UVP groups, which is associated with the following factors. Firstly, only four studies reported mortality but nine studies reported delirium. Secondly, the duration of visits, number of visitors during each visit, and visitation frequency varied across studies with respect to times of the day. Thirdly, because the heterogeneity of delirium-related studies was high (I2 = 71%, p = 0.0005) there was a significant difference in the incidence of delirium in RVP and UVP groups (OR = 0.40, 95% CI 0.25–0.63, p = 0.0001). This may be related to the large sample size of the study by Rosa et al. [11], and inclusion of QEs which affected the effect sizes.
More than half of critically ill patients experience anxiety and depression symptoms [35], and the incidence of delirium in response to sudden mental symptoms in this population ranges from 38.9 to 77.4% [36,37,38]. The incidence of delirium in ICU patients with restricted visitation was reported to be more than threefold that of patients with unrestricted visitation [39]. A UVP is a humanized service aimed at reducing separation anxiety caused by a closed ICU. It can provide comfort and a sense of security to critically ill patients [12, 34, 40]. Studies have found that UVPs can help patients establish contact with the outside world, giving them courage and confidence to fight against their condition [5, 12]. Secondly, visitors can provide mental and social support and relieve patients’ negative emotions during treatment, all of which protect against stress [10, 41]. Lastly, family involvement can reduce the need for analgesics and sedatives, reduce the incidence of ICU syndrome, and shorten ICU stays [19, 42, 43]. Collectively, our findings suggest that UVPs should be implemented in ICUs so that family members can participate in the psychological, social, and emotional support of critically ill patients in a timely manner to promote their reorientation, cognitive health, and rehabilitation.
Critical patients are frail and prone to cross-infection, and one of the most frequent objections to UVPs in ICUs is the risk of an increased rate of acquired infections. Although there is no evidence of an increased incidence of infections in open ICUs, several surveys have expressed caregivers’ concerns that visitors could bring infections into the units through a form of ‘‘pollination’’ [33]. Therefore, visitors are required to practice good hand hygiene and wear disposable isolation clothes and/or personal protective equipment when appropriate [2, 33]. Hand hygiene is an economical, simple, unique, and effective measure for controlling nosocomial infection [3, 7, 44]. A World Health Organization review found that baseline compliance with hand hygiene among healthcare workers was on average only 38.7% (range 5–89%) [44]. Multicomponent interventions are effective in improving hand hygiene compliance, and improved hand hygiene compliance can reduce the rate of hospital-acquired infections and catheter-associated urinary tract infections [4, 45]. However, due to busy schedules, improper hand washing, insufficient equipment, and other reasons, hand hygiene implementation by medical staff still needs improvement [3]. Similarly, when we asked family members why they did not wash their hands in accordance with hospital procedures one replied that “the total visit time is 20 min, hand hygiene takes too much time, and our other family members also want to visit.” With RVPs, family members want to provide more emotional support to patients in a short period and therefore ignore hand hygiene. In contrast, UVPs provide time, so family members may be more likely to perform the hand washing protocol. This may be why UVPs do not increase the incidence of ICU-acquired infections.
More liberal visiting policies seem to be safe for patients with regard to the risks of ICU mortality and LoS. There was no increase in the LoS in the combined analysis of data from the four studies that reported on this outcome [2, 29,30,31,32,33]. Although no difference was observed in ICU mortality, in the largest included study, units with lower standardized mortality ratios were also those with more liberal visiting policies [13].
Visiting hours vary among countries, due to national, cultural, and religious differences. This confounding factor could not be addressed in the meta-analysis. Compared with developing countries, ICU visitation policies in developed countries are more flexible and allow relatively long visits [2, 5, 10, 46,47,48]. The median number of visiting hours was > 4/d in ICUs in Brazil, USA, and Italy [11, 12, 49], and visiting hours ranged from 1.5 to 24.0 h/d in the Netherlands [14], compared to just 1–2 h/d in Iran [19]. The results of this meta-analysis should be interpreted with caution. Firstly, despite a comprehensive database search, only a five RCTs were eligible for inclusion. Our study demonstrated that there is high heterogeneity in visitation policies among ICUs in different countries. But, it is unable to address potential effect modifiers at country level. Secondly, the concept of UVP varies between studies and countries, which may related to different periods of cultural and organizational aspects. Thirdly, our study was only possible for some patient-related outcomes, and most of the results showed high heterogeneity. Consequently, we need to implement UVP with critical thinking.
Conclusion
The current meta-analysis compared the efficacy and safety of UVPs and RVPs for adult ICU patients, and the conclusions were based on moderate-certainty evidence. The results indicate that UVPs can reduce the incidence of delirium in ICU patients, shorten the lengths of ICU stays, and reduce anxiety and depression scores, without increasing rates of ICU-acquired infection. Based on this, we suggest that ICUs should implement UVPs.
Availability of data and materials
Data can be requested from the Ethics Committee of the First Hospital of Lanzhou University, Lanzhou, Gansu, China (email ldyylwh@126.com) by researchers who meet the criteria for access to confidential data.
References
Venkataraman R, Divatia JV, Ramakrishnan N, Chawla R, Amin P, Gopal P, et al. Multicenter observational study to evaluate epidemiology and resistance patterns of common intensive care unit-infections. Indian J Crit Care Med. 2018;22(1):20–6. https://doi.org/10.4103/ijccm.IJCCM_394_17.
Rosa RG, Tonietto TF, da Silva DB, Gutierres FA, Ascoli AM, Madeira LC, et al. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45(10):1660–7. https://doi.org/10.1097/CCM.0000000000002588.
Duszynska W, Rosenthal VD, Szczesny A, Zajaczkowska K, Fulek M, Tomaszewski J. Device associated-health care associated infections monitoring, prevention and cost assessment at intensive care unit of University Hospital in Poland (2015–2017). BMC Infect Dis. 2020;20(1):761. https://doi.org/10.1186/s12879-020-05482-w.
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906. https://doi.org/10.1007/s00134-020-05980-0.
Cappellini E, Bambi S, Lucchini A, Milanesio E. Open intensive care units: a global challenge for patients, relatives, and critical care teams. Dimens Crit Care Nurs. 2014;33(4):181–93. https://doi.org/10.1097/DCC.0000000000000052.
Khaleghparast S, Joolaee S, Maleki M, Peyrovi H, Ghanbari B, Bahrani N. New visiting policy: a step toward nursing ethics. Nurs Ethics. 2019;26(1):293–306. https://doi.org/10.1177/0969733017703701.
Adams S, Herrera A 3rd, Miller L, Soto R. Visitation in the intensive care unit: impact on infection prevention and control. Crit Care Nurs Q. 2011;34(1):3–10. https://doi.org/10.1097/CNQ.0b013e31820480ef.
Shinohara F, Unoki T, Horikawa M. Relationship between no-visitation policy and the development of delirium in patients admitted to the intensive care unit. PLoS ONE. 2022;17(3):e0265082. https://doi.org/10.1371/journal.pone.0265082.
Kynoch K, Chang A, Coyer F, McArdle A. The effectiveness of interventions to meet family needs of critically ill patients in an adult intensive care unit: a systematic review update. JBI Database Syst Rev Implement Rep. 2016;14(3):181–234. https://doi.org/10.11124/jbisrir-2016-2477.
Nassar Junior AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: a systematic review and meta-analysis. Crit Care Med. 2018;46(7):1175–80. https://doi.org/10.1097/ccm.0000000000003155.
Rosa RG, Falavigna M, da Silva DB, Sganzerla D, Santos MMS, Kochhann R, et al. Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU visits randomized clinical trial. JAMA. 2019;322(3):216–28. https://doi.org/10.1001/jama.2019.8766.
Fumis RR, Ranzani OT, Faria PP, Schettino G. Anxiety, depression, and satisfaction in close relatives of patients in an open visiting policy intensive care unit in Brazil. J Crit Care. 2015;30(2):440.e1-6. https://doi.org/10.1016/j.jcrc.2014.11.022.
Ning J, Cope V. Open visiting in adult intensive care units—a structured literature review. Intensive Crit Care Nurs. 2020;56:102763. https://doi.org/10.1016/j.iccn.2019.102763.
Tabah A, Ramanan M, Bailey RL, Chavan S, Baker S, Huckson S, et al. Family visitation policies, facilities, and support in Australia and New Zealand intensive care units: a multicentre, registry-linked survey. Aust Crit Care. 2021;35:S1036-7314(21)00103-X. https://doi.org/10.1016/j.aucc.2021.06.009.
Krewulak KD, Stelfox HT, Leigh JP, Ely EW, Fiest KM. Incidence and prevalence of delirium subtypes in an adult ICU: a systematic review and meta-analysis. Crit Care Med. 2018;46(12):2029–35. https://doi.org/10.1097/ccm.0000000000003402.
Krewulak KD, Stelfox HT, Ely EW, Fiest KM. Risk factors and outcomes among delirium subtypes in adult ICUs: a systematic review. J Crit Care. 2020;56:257–64. https://doi.org/10.1016/j.jcrc.2020.01.017.
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753–62. https://doi.org/10.1001/jama.291.14.1753.
Lindroth H, Mohanty S, Ortiz D, Gao S, Perkins AJ, Khan SH, et al. Dynamic delirium severity trajectories and their association with 2-year healthcare utilization and mortality outcomes. Crit Care Explor. 2021;3(9):e0524. https://doi.org/10.1097/cce.0000000000000524.
Fike GC, Smith-Stoner M, Blue DI, Abuatiq AA. Current trends and practices of intensive care unit visitations. J Dr Nurs Pract. 2018;11(2):169–74. https://doi.org/10.1891/2380-9418.11.2.169.
Mistraletti G, Giannini A, Gristina G, Malacarne P, Mazzon D, Cerutti E, et al. Why and how to open intensive care units to family visits during the pandemic. Crit Care. 2021;25(1):191. https://doi.org/10.1186/s13054-021-03608-3.
Eghbali-Babadi M, Shokrollahi N, Mehrabi T. Effect of family–patient communication on the incidence of delirium in hospitalized patients in cardiovascular surgery ICU. Iran J Nurs Midwifery Res. 2017;22(4):327–31. https://doi.org/10.4103/1735-9066.212985.
Estrup S, Kjer CKW, Vilhelmsen F, Poulsen LM, Gøgenur I, Mathiesen O. Cognitive function 3 and 12 months after ICU discharge—a prospective cohort study. Crit Care Med. 2018;46(12):e1121–7. https://doi.org/10.1097/ccm.0000000000003391.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142. https://doi.org/10.1002/14651858.ed000142.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. https://doi.org/10.1136/bmj.j4008.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. https://doi.org/10.1016/j.jclinepi.2010.04.026.
Yu X, Wang H, Yao X. Comparison of the efficacy of two visiting systems in relieving ICU syndrome in awake patients with tracheal intubation. Lingnan Modern Clin Surg. 2017;17(2):247–9. https://doi.org/10.3969/j.issn.1009⁃976X.2017.02.029.
Pan L, Ye X, Tang Q, Zheng R, Tong H. Effect of scheduled visits on delirium in ICU patients. China Modern Dorctor. 2018;56(21):97–101.
Jiao X, Liu R, Li W, Ji H, Zhang Y, Huo J. Efect of family-centered visitation on delirium in ICU patients with cancer. J Nurs Sci. 2021;36(06):1–4. https://doi.org/10.3870/J.ISSN.1001-4152.2021.06.001.
Zhou X, Hu Y. The impact of family visiting duration on the recovery of critical ill patients. Chin Prev Med. 2020;21(09):1011–3. https://doi.org/10.16506/j.1009-6639.2020.09.013.
Pan Z. Study on the application of family participation nursing mode in the nursing of conscious patients in ICU. Shijiazhuang: Hebei Medical University; 2020.
Chen L, Wei X, Yin Q. The impact of different family visiting duration on ICU patients. J Nurs Train. 2018;33(10):915–7. https://doi.org/10.16821/j.cnki.hsjx.2018.10.016.
Malacarne P, Corini M, Petri D. Health care-associated infections and visiting policy in an intensive care unit. Am J Infect Control. 2011;39(10):898–900. https://doi.org/10.1016/j.ajic.2011.02.018.
Fumagalli S, Boncinelli L, Lo Nostro A, Valoti P, Baldereschi G, Di Bari M, et al. Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit: results from a pilot, randomized trial. Circulation. 2006;113(7):946–52. https://doi.org/10.1161/CIRCULATIONAHA.105.572537.
Shdaifat SA, Al QM. Anxiety and depression among patients admitted to intensive care. Nurs Crit Care. 2022;27(1):106–12. https://doi.org/10.1111/nicc.12536.
Li Y, Yali C, Chunyan H, Liping Y, Caiyun Z, Jinhui T, et al. Effect of early activity on delirium in ICU patients: a meta⁃analysis. Chin Nurs Res. 2019;33(15):2600–5. https://doi.org/10.12102/j.issn.1009-6493.2019.15.011.
Trogrlić ZT, van der Jagt M, Bakker J, Balas MC, Ely EW, van der Voort PH, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care. 2015;19(1):157. https://doi.org/10.1186/s13054-015-0886-9.
Liu Z, Meng S, Yang S. Influence of early mobilization on delirium and respiratory dynamics in mechanically ventilated patients with acute excerbation of COPD: a prospective study. Chin J Respir Crit Care Med. 2016;15(04):324–8. https://doi.org/10.7507/1671-6205.2016077.
Van Rompaey B, Elseviers MM, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, Bossaert L. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care. 2009;13(3):R77. https://doi.org/10.1186/cc7892.
Fumagalli S, Calvani S, Gironi E, Roberts A, Gabbai D, Fracchia S, et al. An unrestricted visitation policy reduces patients’ and relatives’ stress levels in intensive care units. Eur Heart J. 2013;34:P5126.
Mitchell ML, Aitken LM. Flexible visiting positively impacted on patients, families and staff in an Australian Intensive Care Unit: a before-after mixed method study. Aust Crit Care. 2017;30(2):91–7. https://doi.org/10.1016/j.aucc.2016.01.001.
Fergé JL, Banydeen R, Le Terrier C, Fize H, Miguel M, Kentish-Barnes N, et al. Mental health of adolescent relatives of intensive care patients: benefits of an open visitation policy. Am J Crit Care. 2021;30(1):72–6. https://doi.org/10.4037/ajcc2021799.
Yao L, Li Y, Yin R, Yang L, Ding N, Li B, et al. Incidence and influencing factors of post-intensive care cognitive impairment. Intensive Crit Care Nurs. 2021;67:103106. https://doi.org/10.1016/j.iccn.2021.103106.
Luangasanatip N, Hongsuwan M, Limmathurotsakul D, Lubell Y, Lee AS, Harbarth S, et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ. 2015;351:h3728. https://doi.org/10.1136/bmj.h3728.
Al KA. Impact of a multicomponent hand hygiene intervention strategy in reducing infection rates at a university hospital in Saudi Arabia. Interv Med Appl Sci. 2017;9(3):137–43. https://doi.org/10.1556/1646.9.2017.24.
Riley BH, White J, Graham S, Alexandrov A. Traditional/restrictive versus patient-centered intensive care unit visitation: perceptions of patients’ family members, physicians, and nurses. Am J Crit Care. 2014;23(4):316–24. https://doi.org/10.4037/ajcc2014980.
Ramos FJ, Fumis RR, de Azevedo LC, Schettino G. Intensive care unit visitation policies in Brazil: a multicenter survey. Rev Bras Ter Intensiva. 2014;26(4):339–46. https://doi.org/10.5935/0103-507x.20140052.
Han Z, Liu X, He Y, Tian Z. The research development on patient and family-centered care visitation model in ICU. Chin J Nurs. 2019;54(2):235–40. https://doi.org/10.3761/j.issn.0254-1769.2019.02.013.
Vranceanu AM, Bannon S, Mace R, Lester E, Meyers E, Gates M, et al. Feasibility and efficacy of a resiliency intervention for the prevention of chronic emotional distress among survivor-caregiver dyads admitted to the neuroscience intensive care unit: a randomized clinical trial. JAMA Netw Open. 2020;3(10):e2020807. https://doi.org/10.1001/jamanetworkopen.2020.20807.
Acknowledgments
The authors thank the librarian of Lanzhou University who provided data resources, and Charlesworth Author Services for help revising the language in the manuscript.
Funding
This study was funded by the Health Commission of Gan Su Province (Project Number GSWSHL2020-11), China and the First Affiliated Hospital of Lanzhou University (Project Number ldyyyn2019-61), China. The funding source had no involvement in data collection or analyses, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
YCW, ZGZ, and BL contributed to the conception and design of this meta-analysis. WGY, YCW, and JHT performed the two-stage literature screening, extracted the data, and conducted the risk of bias assessment. FLM and BL statistically analyzed the data. FLM, BL, and LF interpreted and synthesized the data. YCW functioned as a senior reviewer, supervised the analysis, and advised on the interpretation of results. YCW and ZGZ wrote the draft manuscript. LF, WGY, GQW, and BL critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was reviewed by the Ethics Committee of the First Hospital of Lanzhou University (LDYYLL2020-198).
Consent for publication
The manuscript has been approved by all authors for publication.
Competing interests
The authors have declared that no competing interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, Y., Wang, G., Zhang, Z. et al. Efficacy and safety of unrestricted visiting policy for critically ill patients: a meta-analysis. Crit Care 26, 267 (2022). https://doi.org/10.1186/s13054-022-04129-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04129-3