Abstract
Background
Usefulness of noninvasive ventilation (NIV) in weaning patients with non-hypercapnic hypoxemic acute respiratory failure (hARF) is unclear. The study aims to assess in patients with non-hypercapnic hARF, the efficacy of NIV after early extubation, compared to standard weaning.
Methods
In this individual patient data meta-analysis, we searched EMBASE, Medline and Cochrane Central Register of Controlled Trials to identify potentially eligible randomized controlled trials published from database inception to October 2020. To be eligible, studies had to include patients treated with NIV after early extubation and compared to conventional weaning in adult non-hypercapnic hARF patients. Anonymized individual patient data from eligible studies were provided by study investigators. Using one-step and two-step meta-analysis models we tested the difference in total days spent on invasive ventilation.
Results
We screened 1605 records. Six studies were included in quantitative synthesis. Overall, 459 participants (mean [SD] age, 62 [15] years; 269 [59%] males) recovering from hARF were included in the analysis (233 in the intervention group and 226 controls). Participants receiving NIV had a shorter duration of invasive mechanical ventilation compared to control group (mean difference, − 3.43; 95% CI − 5.17 to − 1.69 days, p < 0.001), a shorter duration of total days spent on mechanical ventilation (mean difference, − 2.04; 95% CI − 3.82 to − 0.27 days, p = 0.024), a reduced risk of ventilatory associated pneumonia (odds ratio, 0.24; 95% CI 0.08 to 0.71, p = 0.014), a reduction of time spent in ICU (time ratio, 0.81; 95% CI 0.68 to 0.96, p = 0.015) and in-hospital (time ratio, 0.81; 95% CI 0.69 to 0.95, p = 0.010), with no difference in ICU mortality.
Conclusions
Although primary studies are limited, using an individual patient data metanalysis approach, NIV after early extubation appears useful in reducing total days spent on invasive mechanical ventilation.
Trial registration
The protocol was registered to PROSPERO database on 12/06/2019 and available at PROSPERO website inserting the study code i.e., CRD42019133837.
Similar content being viewed by others
Introduction
Though a life-saving intervention, invasive mechanical ventilation (i-MV) is prone to side-effects and complications [1, 2]. The process of weaning patient off i-MV should be started promptly to make the time spent on i-MV the shortest possible [3]. Weaning has been recently defined as the time between the first separation attempt and successful extubation that leads to either 7 days of continuous spontaneous breathing or intensive care unit (ICU) discharge, whichever comes first and irrespective of the use of noninvasive ventilation (NIV) in the post extubation period [4].
NIV applied immediately after extubation has been proposed as a measure to prevent post-extubation respiratory failure (i.e., prophylactic NIV in high-risk patients) or as an alternative to i-MV in patients not yet ready to be extubated (i.e., NIV to facilitate weaning) [5, 6].
In patients with acute-on-chronic respiratory failure, particularly those secondary to chronic obstructive pulmonary disease (COPD) exacerbations, compared to standard weaning with the endotracheal tube in place, early extubation followed by immediate NIV application reduces rates of weaning failure and ventilator associated pneumonia, duration of mechanical ventilation, ICU and hospital length of stay (LOS), and improves the rate of survival compared to standard weaning with the endotracheal tube in place [6, 7]. Recent guidelines provide a conditional recommendation in favor of this therapeutic approach in hypercapnic patients with acute-on-chronic respiratory failure. The guideline authors were unable to make recommendation in patients with non-hypercapnic hypoxemic acute respiratory failure (hARF), because of scarcity of available data [6]. After completion of these guidelines, however, two properly powered studies have been published, which included many more patients than previous investigations [8, 9].
Therefore, we designed this systematic review and individual patient data meta-analysis (IPD) to re-assess, in a population of patients recovering from an episode of non-hypercapnic hARF, whether NIV after early extubation would reduce the duration of i-MV (primary endpoint), overall time spent on mechanical ventilation (i-MV + NIV), rate of ventilator associated pneumonia (VAP), time from randomization to ICU and hospital discharges, and time from randomization to ICU death (secondary endpoints), when compared to conventional weaning with the endotracheal tube in place.
Materials and methods
Search strategy and selection criteria
This systematic review with meta-analysis was conducted in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis of Individual Participant Data.
We considered eligible for inclusion all randomized controlled trials (RCTs) comparing early extubation + NIV with standard weaning with the endotracheal tube in place in adult patients with non-hypercapnic (as defined by PaCO2 ≤ 50 mmHg and pH ≥ 7.35) hARF and receiving i-MV for more than 48 h. Patients were excluded in the case of (1) ARF secondary to neurological/ neuromuscular disorders, status asthmaticus, chronic obstructive pulmonary disease (COPD), cardiogenic pulmonary edema; (2) body mass index ≥ 30 kg/m2; (3) tracheostomy; (4) obstructive sleep apnoea.
Two authors (FM/AP), independently, searched EMBASE, Pubmed/Medline and Cochrane Central Register of Controlled Trials (CENTRAL) bibliographic databases, without language restriction. Our search encompassed a period from database inception to the 1st October 2020. We supplemented this search by searching review articles and reference lists of trial publications. Collaborators were asked if they knew of any additional RCTs.
Search term combinations are detailed in the Additional file 1.
On search completion and after removal of duplicates, two authors (FM/AP), with the help of a third author (RV) in case of discrepancies, independently assessed for relevance all titles identified by the search strategy. Following title screening, the same independent review procedure was adopted for screening of abstracts and, finally, full texts.
Data analysis
Data were extracted onto a piloted proforma by two authors (RV/FBA) independently. Extracted data included characteristics of the studies, populations, intervention and comparator, and outcomes. Data were checked for sequence generation, data consistency and completeness and baseline imbalance. IPD were obtained from the authors through a process detailed in the Additional file 2.
RCTs included in quantitative synthesis were evaluated using the Cochrane Risk of Bias assessment tool [10]. The following variables were assessed: sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; completeness of outcome data; evidence of selective outcome reporting; and other potential threats to validity. We assessed selectivity of reporting either by comparing study protocols against study reports or by specifically asking study authors whether all prespecified outcomes were reported. Two investigators (FM and AP) independently assessed study quality. Details of the assessment are reported in the Additional files 3 and 4.
Our primary endpoint was to determine whether, in adults receiving i-MV due to non-hypercapnic hARF (population), early extubation followed by immediate NIV application (intervention) compared to standard weaning (comparator), reduces the time spent on i-MV, i.e., days spent on i-MV from randomization to ICU discharge (outcome). Secondary endpoints are summarized in the Additional file 4.
Statistical analysis
We conducted a meta-analysis with one-step and two-step approach, incorporating all available IPD. Only complete case data were included for all trials in the main analyses. Continuous variables were presented in descriptive analyses as mean ± standard deviation (SD), while categorical and binary variables were presented as frequencies (n) and percentages (%), as indicated. Data were analyzed on an intention-to-treat basis. Mixed-effects linear regression models were used to model total days of ventilation and the other continuous outcome variables. Time-to-event outcomes were analyzed through parametric survival models, including random effects considering the cluster effect deriving from different studies. Heterogeneity was assessed within 2-stage models using the I2 statistic. We also performed a leave-one-out sensitivity analysis, alternatively removing one study at a time, to measure how each study affected the overall estimate and to identify studies that potentially drove the results.
All tests were two-sides and performed at the 5% level of statistical significance. Statistical analyses were done using STATA software version 15 (StataCorp).
The protocol was registered to PROSPERO database on 12/06/2019 and available at PROSPERO website inserting the study code i.e., CRD42019133837.
Results
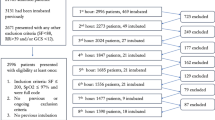
Our search identified 1605 records (486 citations in PubMed/Medline, 591 in EMBASE and 528 in the Cochrane Controlled Register of Trials). Following removal of duplicates (n = 460), 1076 records were excluded for title and 56 in abstract form. Thirteen full text articles were assessed for eligibility. Seven studies were excluded in full text: 2 for PICO reasons i.e., 1 for intervention and 1 for population and 5 as IPD were not available [11,12,13,14,15,16,17]. Six studies were included in the quantitative synthesis [8, 9, 18,19,20,21]. Excluded studies and reasons for exclusion are reported in the Additional file 5. The selection process is summarized in the PRISMA-IPD flow diagram (Fig. 1).
Patients meeting all formal inclusion criteria were available for two RCTs [9, 21], while for the remaining 4 studies only selected patients fulfilling inclusion criteria were included (Table 1) [8, 18,19,20].
We conducted the quality assessment only for studies contributing to IPD meta-analysis. All the studies were rated as being at low risk of bias for randomization process, allocation concealment and incomplete outcome data (attrition bias). The inability to blind caregivers to treatment allocation meant that all the studies were at high risk of performance bias. The risk of detection bias was overall low; in 3 studies the strategies to blind outcome assessors from group allocation were described [8, 9, 21], in 2 studies we received description after contacting the authors [18, 20] and for one study the risk remained unclear [19]. One study was not registered in advance [19]. In 2 studies the predefined outcomes were not properly reported [18, 20], encompassing the risk of reporting bias (Additional file 3).
Patient characteristics, stratified by randomization group, are summarized in Table 2. We overall included 459 participants, 233 and 226 in the intervention and control group, respectively, mean (SD) age 62 (15) years, 269 (59%) males. The principal causes for instituting i-MV were post-operative ARF and acute respiratory distress syndrome (ARDS). Surgical and medical patients were 203 (44%) and 256 (56%), respectively. Mean risk of predicted in-hospital mortality based on APACHE [22] or SAPSII [23] scores, varied from 12 to 35% for surgical and medical patients.
Criteria for readiness to wean and spontaneous breathing trial before randomization are summarized in the Additional file 6. Ventilator settings and arterial blood gas values at randomization and prior to spontaneous breathing trial (SBT) are also displayed in Table 2. Mean positive end-expiratory pressure (PEEP) and pressure support levels were 7 and 11 cmH2O, respectively, in both groups. Noteworthy, PaO2/FiO2 was slightly though significantly different between intervention 242 (58) mmHg and control group 258 (77) mmHg, (p = 0.014).
The primary outcome of the study, i.e., length of i-MV, was available for all 459 patients. The two-stage IPD meta-analysis (Fig. 2a) showed a shorter time of i-MV in the treatment group, compared to the control group (mean difference: − 4.16 days; 95% CI − 7.09 to − 1.22; p = 0.006). The sensitivity analysis based on the leave-one-out method did not substantially modify the results, which remained statistically significant after exclusion of each study, with point estimates ranging between − 2.70 and − 5.06 days.
Results of 2-stage IPD-MA. a Mean i-MV time (p value = 0.006); b mean total ventilation time (p value = 0.13); c occurrence of VAP (p value = 0.03); d time to ICU discharge (p value = 0.09); e time to ICU death (p value = 0.222), f time to hospital discharge (p value = 0.009). CI confidence interval, ICU intensive care unit, i-MV invasive mechanical ventilation, IPD-MA individual patient data meta-analysis, VAP ventilator associated pneumonia
The one-stage IPD analysis confirmed the previous results. After adjusting for demographic (age, gender) and severity-related variables (severity scores at ICU admission and PaO2/FiO2 at randomization), the duration of i-MV remained significantly different between treatment and control group (mean difference: − 3.43 days; 95% CI − 5.17 to − 1.69; p < 0.001). Results of random and fixed-effects models did not substantially differ (Table 3).
Results of two-stage IPD meta-analysis for each secondary outcome are reported in Fig. 2 (panels b–f). The overall duration of mechanical ventilation was similar between intervention group and controls (mean difference: − 0.88 days; 95% CI − 2.01 to 0.25; p = 0.130). Time to ICU discharge (time ratio: 0.79; 95% CI 0.60 to 1.04; p = 0.09) and mortality (time ratio of 0.63; 95% CI 0.30 to 1.32; p = 0.222) were also not significantly different between groups, while the time to hospital discharge (time ratio: 0.82; 95% CI 0.71 to 0.95; p = 0.009) and the risk for VAP, (odds ratio: 0.29; 95% CI 0.09 to 0.90; p = 0.03) were reduced in the intervention group, as opposed to controls.
Analyses of secondary outcomes based on one-stage approach are reported in Table 3. After adjusting for demographic (age, gender) and severity-related variables (ratio between partial pressure of oxygen and inspired oxygen fraction at randomization and severity scores at ICU admission), all the results became significantly different, except for time to ICU mortality.
As further analysis, reintubation occurrence resulted similar in the two groups as reported in the Additional file 7.
Discussion
The present IPD meta-analysis shows that, in selected patients recovering from an episode of hypoxemic ARF, early extubation followed by immediate NIV application reduces the duration of i-MV, as opposed to conventional weaning and extubation. Furthermore, compared to standard weaning, early extubation + NIV decreases overall duration of mechanical ventilation, risk of VAP, and time to ICU and hospital discharge.
The study did not identify a significant difference in ICU mortality between the two groups. One possible explanation is that ICU deaths are a relatively rare events (40 cases), leading to an underpowered analysis.
To the best of our knowledge, this is the first IPD meta-analysis of trials investigating the role of NIV in the weaning process of patients recovering from an episode of non-hypercapnic hARF. Previous systematic reviews and meta-analyses addressing the potential of NIV to facilitate weaning [7, 24], considered data on both COPD patients and mixed populations, in the present IPD meta-analysis we analyzed data from 459 patients with non-hypercapnic hARF only, allowing the study to focus on this specific population. By excluding not only hypercapnic patients with COPD or other chronic respiratory disorders, such as neuromuscular disease and obesity-hypoventilation, and those with cardiogenic pulmonary edema, we removed the group of patients who usually show a fast response to NIV.
A recent guideline considers the potential usefulness of NIV in the process of facilitating weaning from i-MV [6]. No recommendation was made for patients with non-hypercapnic hARF due to the paucity of available data. After these guidelines were completed, however, two properly powered studies were published. Both included many more patients than all previous investigations. The first assessed 364 mixed patients, mainly those with non-hypercapnic hARF [8] from 41 ICUs of the UK National Health Service, while the second, 130 non-hypercapnic hypoxemic patients from 9 ICUs, 6 in the Chinese Republic and 3 in Italy [9]. Notably, the results on the time to liberation from i-MV and from any ventilation were largely similar in both cases, showing a shorter duration of i-MV and a similar duration of overall mechanical ventilation, i.e., invasive plus noninvasive. We choose to consider i-MV, rather than the overall duration of mechanical ventilation, as primary endpoint since it has been repeatedly shown to be associated with greater requirement of sedatives, rate of VAP and mortality [7, 25].
Before drawing conclusions, some strengths and limitations of our study require discussion. The major strength is the study design; an IPD meta-analysis is considered to achieve the highest level of evidence and offers several advantages over aggregate patient data meta-analysis [26]. Furthermore, the present work considers only RCTs. If on the one hand our choice excludes observational studies of potential interest, on the other hand it incorporates the studies providing the highest level of evidence. Finally, the amount of missing data was small, and only present for outcomes considered secondary endpoints, in a range from 0 to 3%.
Our meta-analysis has several additional potential limitations. First, we could not include patients from 5 of the identified studies (one of which was available only in abstract form [11]) as in 2 cases we could not reach the authors, while in the other 3 cases datasets were not available [11, 1314, 16, 17]. Second, the study protocols of the included studies were not identical, as NIV after early extubation was applied before readiness for SBT in two studies [9, 21], after failing one SBT [8, 18, 20] in three RCTs, or after failing SBT for three consecutive days [19] in one study. Nevertheless, the sensitivity analysis based on the leave-one-out method indicates no effect on the primary endpoint. Third, despite the overall risk of bias being assessed as low, blinding the caregivers to treatment allocation was not possible in all the original studies. This is partly mitigated by our choice of objective outcomes, where the risk of detection bias is low. We share this limitation with previous meta-analyses on the use of NIV to facilitate weaning [7, 24]; however, the reporting bias affects IPD meta-analysis to a lesser extent than traditional meta-analysis. Fourth, most of the included studies are of limited size. As a result, baseline imbalances between treatment groups, such as PaO2/FiO2 values that was different in the intervention and control group could have occurred by chance. However, the results are not substantially affected when adjusting for possible confounders.
Conclusions
Patients recovering from an episode of hARF may benefit from a weaning strategy based on early extubation followed by immediate NIV application. Compared to conventional weaning, replacing the endotracheal tube with a noninvasive interface reduces the duration of i-MV. Overall time spent on mechanical ventilation, length of ICU and hospital stay, and risk of VAP may also be reduced by this weaning strategy. Future studies are warranted to evaluate whether this approach is also associated with reduced mortality.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Change history
03 August 2021
A Correction to this paper has been published: https://doi.org/10.1186/s13054-021-03692-5
Abbreviations
- APACHE II:
-
Acute Physiology and Chronic Health Disease Classification System II
- ARDS:
-
Acute Respiratory Distress Syndrome
- ARF:
-
Acute Respiratory Failure
- BMI:
-
Body Mass Index
- COPD:
-
Chronic Obstructive Pulmonary Disease
- GIT:
-
Gastrointestinal
- hARF:
-
Hypoxemic Acute Respiratory Failure
- ICU:
-
Intensive Care Unit
- i-MV:
-
Invasive Mechanical Ventilation
- IPD-MA:
-
Individual Patient Data Meta-Analysis
- i.v.:
-
Intravenous
- LOS:
-
Length Of Stay
- MOF:
-
Multiple Organ Failure
- n:
-
Number
- N.A.:
-
Not Applicable
- NIV:
-
Non-Invasive Ventilation
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PE:
-
Pulmonary Embolism
- UK:
-
United Kingdom
- RCT:
-
Randomized Controlled Trials
- SAPS II:
-
Simplified Acute Physiology Score II
- SD:
-
Standard Deviation
- VAP:
-
Ventilator Associated Pneumonia
- VAT:
-
Ventilator Associated Tracheobronchitis
- vs.:
-
Versus
References
Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Penuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188:220–30.
Tobin MJ. Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med. 2020;201:1319–20.
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29:1033–56.
Beduneau G, Pham T, Schortgen F, Piquilloud L, Zogheib E, Jonas M, et al. Epidemiology of weaning outcome according to a new definition. The WIND study. Am J Respir Crit Care Med. 2017;195:772–83.
Nava S, Navalesi P, Conti G. Time of non-invasive ventilation. Intensive Care Med. 2006;32:361–70.
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426.
Burns KE, Meade MO, Premji A, Adhikari NK. Noninvasive ventilation as a weaning strategy for mechanical ventilation in adults with respiratory failure: a Cochrane systematic review. CMAJ. 2014;186:E112–22.
Perkins GD, Mistry D, Gates S, Gao F, Snelson C, Hart N, et al. Effect of protocolized weaning with early extubation to noninvasive ventilation vs invasive weaning on time to liberation from mechanical ventilation among patients with respiratory failure: the breathe randomized clinical trial. JAMA. 2018;320:1881–8.
Vaschetto R, Longhini F, Persona P, Ori C, Stefani G, Liu S, et al. Early extubation followed by immediate noninvasive ventilation vs. standard extubation in hypoxemic patients: a randomized clinical trial. Intensive Care Med. 2019;45:62–71.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Charra B, Hachimi A, Benslama A, Motaouakkil S. Contribution of noninvasive ventilation in the precocious extubation in the medical ICU. Crit Care. 2009;13(Suppl 1):12.
Girault C, Daudenthun I, Chevron V, Tamion F, Leroy J, Bonmarchand G. Noninvasive ventilation as a systematic extubation and weaning technique in acute-on-chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999;160:86–92.
Guo F, Xu S, Liu G, Wang X. An investigation of the efficacy of invasive-noninvasive sequential mechanical ventilation in senile patients with severe community-acquired pneumonia. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2015;27:595–600.
Laiq N, Khan RA, Malik A. Non-Invasive Positive Pressure Ventilation facilitates early extubation in post operative cardiac patients. Postgrad Med Inst. 2013;27:361–5.
Laiq N, Khan S, Islam N, Khan MN. Effectiveness of continuous positive pressure ventilation in reducing the length of stay in post cardiac bypass surgery patients. J Med Sci. 2017;25:257–61.
Tawfeek MM, Elnabtity AMA. Noninvasive proportional assist ventilation may be useful in weaning patients who failed spontaneous breathing trial. Egyptian Journal of Anaesthesia. 2012;28:89–94.
Wang X, Xu S, Liu G, Caikai S. Study of timing of invasive and noninvasive sequential ventilation in patients with acute respiratory distress syndrome. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:330–4.
Carron M, Rossi S, Carollo C, Ori C. Comparison of invasive and noninvasive positive pressure ventilation delivered by means of a helmet for weaning of patients from mechanical ventilation. J Crit Care. 2014;29:580–5.
Ferrer M, Esquinas A, Arancibia F, Bauer TT, Gonzalez G, Carrillo A, et al. Noninvasive ventilation during persistent weaning failure: a randomized controlled trial. Am J Respir Crit Care Med. 2003;168:70–6.
Trevisan CE, Vieira SR. Noninvasive mechanical ventilation may be useful in treating patients who fail weaning from invasive mechanical ventilation: a randomized clinical trial. Crit Care. 2008;12:R51.
Vaschetto R, Turucz E, Dellapiazza F, Guido S, Colombo D, Cammarota G, et al. Noninvasive ventilation after early extubation in patients recovering from hypoxemic acute respiratory failure: a single-centre feasibility study. Intensive Care Med. 2012;38:1599–606.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345–55.
Yeung J, Couper K, Ryan EG, Gates S, Hart N, Perkins GD. Non-invasive ventilation as a strategy for weaning from invasive mechanical ventilation: a systematic review and Bayesian meta-analysis. Intensive Care Med. 2018;44:2192–204.
Nava S, Ambrosino N, Clini E, Prato M, Orlando G, Vitacca M, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease. A randomized, controlled trial. Ann Intern Med. 1998;128:721–8.
Lyman GH, Kuderer NM. The strengths and limitations of meta-analyses based on aggregate data. BMC Med Res Methodol. 2005;5:14.
Acknowledgements
Not applicable.
Funding
The IPD meta-analysis was not funded. The Breathe trial was funded by the National Institute for Health Research NIHR Health Technology Assessment Programme (project HTA 10/134).
Author information
Authors and Affiliations
Contributions
We declare that all authors: RV, AP, GDP, DM, GC, FL, MF, RPA, MC, FM, HQ, FDC, FBA and PN gave substantial contributions to (1) conception or design of the work, or the acquisition, analysis, or interpretation of data for the work; (2) drafting of the work or revising it critically for important intellectual content; (3) final approval of the version to be published; and (4) agreement to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
PN reports, outside the submitted work, non-financial support from Draeger and Intersurgical SpA, personal fees from, Resmed, Philips, Novartis, MSD, Getinge and, Draeger. In addition, PN has a patent 102020000008305 pending to Università di Padova, and a patent 102016000114357 with royalties paid from Intersurgical S.p.A. GDP is supported as a NIHR Senior Investigator and by NIHR Applied Research Collaboration (ARC) West Midlands. FL contributed to the development of a new device (European Patent number EP3320941). RV, AP, DM, GC, MF, RPA, MC, FM, HQ, FDC, FBA declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Following publication of the original article, the authors identified an error in Table 1. The correct Table has been updated in the original article.
Supplementary Information
Additional file 1.
Search strategies
Additional file 2
. Letters sent to the authors
Additional file 3
. Risk of bias assessment within studies included in quantitative synthesis
Additional file 4
. Extended methods: secondary outcomes, search strategy, data collection process, and risk of bias (quality) assessment
Additional file 5
. 1076 studies were excluded considering the title, while 58 after reading the abstract or full text. The table summarize the reason for exclusion of the 58 papers
Additional file 6
. Criteria for readiness to wean and spontaneous breathing trails performed before randomization
Additional file 7
. Results of two-stage IPD-MA. Occurrence of reintubation (p value=0.83)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vaschetto, R., Pecere, A., Perkins, G.D. et al. Effects of early extubation followed by noninvasive ventilation versus standard extubation on the duration of invasive mechanical ventilation in hypoxemic non-hypercapnic patients: a systematic review and individual patient data meta-analysis of randomized controlled trials. Crit Care 25, 189 (2021). https://doi.org/10.1186/s13054-021-03595-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-021-03595-5