Abstract
Background
Microaspiration of gastric and oropharyngeal secretions is the main causative mechanism of ventilator-associated pneumonia (VAP). Transesophageal echocardiography (TEE) is a routine investigation tool in intensive care unit and could enhance microaspiration. This study aimed at evaluating the impact of TEE on microaspiration and VAP in intubated critically ill adult patients.
Methods
It is a four-center prospective observational study. Microaspiration biomarkers (pepsin and salivary amylase) concentrations were quantitatively measured on tracheal aspirates drawn before and after TEE. The primary endpoint was the percentage of patients with TEE-associated microaspiration, defined as: (1) ≥ 50% increase in biomarker concentration between pre-TEE and post-TEE samples, and (2) a significant post-TEE biomarker concentration (> 200 μg/L for pepsin and/or > 1685 IU/L for salivary amylase). Secondary endpoints included the development of VAP within three days after TEE and the evolution of tracheal cuff pressure throughout TEE.
Results
We enrolled 100 patients (35 females), with a median age of 64 (53–72) years. Of the 74 patients analyzed for biomarkers, 17 (23%) got TEE-associated microaspiration. However, overall, pepsin and salivary amylase levels were not significantly different between before and after TEE, with wide interindividual variability. VAP occurred in 19 patients (19%) within 3 days following TEE. VAP patients had a larger tracheal tube size and endured more attempts of TEE probe introduction than their counterparts but showed similar aspiration biomarker concentrations. TEE induced an increase in tracheal cuff pressure, especially during insertion and removal of the probe.
Conclusions
We could not find any association between TEE-associated microaspiration and the development of VAP during the three days following TEE in intubated critically ill patients. However, our study cannot formally rule out a role for TEE because of the high rate of VAP observed after TEE and the limitations of our methods.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is the most common acquired infection in critically ill patients under mechanical ventilation [1], often associated with significant morbidity [2, 3]. VAP is mainly precipitated by microaspiration of contaminated gastric and oropharyngeal secretions [4]. Microaspiration is defined by leakage of oropharyngeal secretions accumulated upstream the tracheal cuff into the lower respiratory tract [5, 6]. The gold standard test for the diagnosis of microaspiration is using technetium 99 m [7]. However, applying this technique in intubated patients in the intensive care unit (ICU) is thwarted by the difficulty of transporting patients to the radiology department to avoid radioactivity in ICU [8]. Pepsin comes from pepsinogen and is secreted by the chief cells in the stomach, and amylase is a digestive enzyme, secreted by the salivary glands and the pancreas. Because they are not normally present in the respiratory tract, pepsin, and salivary amylase were proposed to diagnose microaspiration of gastric content and oropharyngeal secretions, respectively [9,10,11,12]. Their use in intubated critically ill patients is rapid, easy to perform in routine, cheap and only requires tracheal secretions.
Over the past decade, transesophageal echocardiography (TEE) has emerged as a common, minimally invasive, bedside examination in ICU [13], with a low complication rate in intubated patients [14, 15]. TEE-induced bacteremia is extremely rare; thus, TEE is not an indication for antibiotic prophylaxis [16]. Nevertheless, potential microaspiration associated with TEE has never been evaluated in intubated ICU patients. TEE could indirectly trigger microaspiration of oropharyngeal and gastric contents in mechanically ventilated patients via factors such as loss of integrity of the esophageal sphincter, gastroesophageal reflux, displacement of tracheal tube, and modification of tracheal cuff inflation.
The main objective of this study was to evaluate the role of TEE in triggering microaspiration of gastric contents and oropharyngeal secretions, and VAP in intubated critically ill patients.
Methods
Study design and participants
We performed a multicentric prospective observational study in four French medical ICUs of university hospitals between March 2017 and September 2018. Consecutive adult patients intubated and mechanically ventilated for more than 24 h prior to enrollment and who required TEE were included. Exclusion criteria were pregnancy, tracheostomy, and TEE contraindications. This study was conducted in compliance with the amended Declaration of Helsinki. The protocol was approved by the ethical committee CPP, Ile de-France III (EUDRACT number: 2016-A01488-43, approval number: S.C.3457). The protocol was considered as a component of standard care, and patient consent was waived. Written and oral information about the study was given to patients or families.
Procedures and definitions
All included patients were subjected to endotracheal suction just before TEE and within the two hours after. For quantitative analyses, endotracheal aspirates were drawn without the addition of saline beforehand. The collected endotracheal aspirates were stored at − 20 °C in each center and sent to a central laboratory (Lille University Hospital) at the end of the study. All measurements of pepsin and amylase were performed by biologists who were blinded to the chronological status of TEE samples (before vs. after TEE). Pepsin was quantitatively measured by ELISA technique, and salivary amylase activity was calculated as the difference between total and pancreatic amylase activities [12, 17]. The tracheal cuff pressure was manually checked before and after TEE. For some patients included in the Henri Mondor center, Creteil, the tracheal cuff pressure was continuously and mechanically assessed from five minutes before TEE until five minutes after. For those patients, the tracheal cuff pressure signal was recorded using differential pressure transducer TSD160D (Biopac Systems, Goleta, CA, USA) connected to analog/numeric data acquisition system (MP150, Biopac systems, Goleta, CA, USA) and stored on a computer to be analyzed with AcqKnowledge software version 5.0 (Biopac systems, Goleta, CA, USA).
Microaspiration of gastric contents and oropharyngeal secretions is usually confirmed upon detecting significant pepsin (> 200 μg/L) [17] and salivary amylase (> 1685 IU/L) [12] concentrations in the tracheal secretions, respectively. TEE-associated microaspiration of gastric contents (or oropharyngeal secretions) was defined by the association of: (1) pepsin (or salivary amylase) concentration which is ≥ 50% higher in the post-TEE sample than in the pre-TEE sample and (2) a significant post-TEE concentration of pepsin of > 200 μg/L (or salivary amylase of > 1685 IU/L).
VAP diagnosis relied on clinical, radiological, and microbiological criteria. Namely, new and persistent infiltrate on chest X-rays (CXR) was associated with two of the following criteria: (1) turbid tracheal aspirates; (2) temperature > 38 °C or < 36 °C; and (3) peripheral leukocyte count > 10 G/L or < 1.5 G/L). All VAP diagnoses were documented by a positive microbiological sample of tracheal aspirate (≥ 105 CFU/mL), protected telescopic catheter liquid (≥ 103 CFU/mL), or bronchoalveolar lavage (≥ 104 CFU/mL). Tracheobronchial colonization was confirmed by a positive (≥ 105 CFU/ml) tracheal aspirate without CXR signs of VAP [18]. The participating ICUs management fulfilled the VAP-prevention guidelines [18, 19].
Data collection
All data were prospectively collected starting with the inclusion data: age, gender, body mass index, simplified acute physiology score II (SAPS II) at ICU admission [20], comorbidities, history of acute respiratory distress syndrome, shock, and VAP prior to TEE, date and cause of intubation, tracheal tube characteristics (type, diameter, position), Sequential Organ Failure Assessment (SOFA) score, Richmond Agitation and Sedation Scale (RASS), duration of mechanical ventilation prior to TEE, time between last oral decontamination and TEE, ventilator parameters, tracheal cuff pressure before and after TEE, gastric tube and enteral feeding management, evaluation of residual gastric volume, concomitant treatments, probe type and introduction (duration, number of attempts, method, patient position), TEE characteristics (date, duration, indication, use of transgastric view), and complications. The following data were collected during ICU stay: length of stay, mechanical ventilation duration, VAP, and mortality.
Outcomes
The primary endpoint of this study was the percentage of patients with TEE-associated microaspiration of gastric contents and/or oropharyngeal secretions. The secondary outcomes were the percentage of patients who developed VAP within three days after TEE and the evolution of tracheal cuff pressure throughout TEE procedure.
Statistical analysis
Statistical analysis was performed using JMP software (version 9; SAS Institute Inc, Cary, NC) and GraphPad Prism 5 software (GraphPad Software Inc., La Jolla, CA, USA). The number of patients required to assess the incidence rate of microaspiration during TEE was estimated at 75, considering a theoretical prevalence of 75% (previous studies reported the presence of microaspiration at baseline in at least 50% of intubated patients) [12, 21, 22], a precision of ± 10%, a confidence interval of 95%, and a type I error rate of 5%. We anticipated a 25% failure rate for sample processing and analysis and decided to include a total of 100 patients.
Normality of variables was evaluated by Shapiro–Wilk test. Continuous variables were expressed as mean (± standard deviation) or median (first quartile–third quartile) according to their Gaussian or non-Gaussian distribution, respectively. We compared patients who developed VAP within the three days following TEE with their counterparts using Student t test for Gaussian continuous variables, Mann–Whitney test for non-Gaussian continuous variables, and Chi-square or Fisher exact tests for categorical variables, as appropriate. We compared concentrations of pepsin and salivary amylase before and after TEE using paired Wilcoxon test. We evaluated the change in tracheal cuff pressure throughout TEE procedure using one-way ANOVA and Dunnett multiple comparison test. For all tests, a two-tailed P < 0.05 was considered statistically significant.
Results
The study population
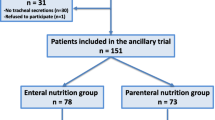
A total of 310 patients who underwent TEE were screened during the study period in the participating centers, of whom 242 met the eligibility criteria; however, only 100 patients (35 females) were retained in this study (Fig. 1), with a median age of 64 (53–72) years. The majority of eligible patients were excluded for logistical reasons (absence of the investigator when TEE was performed, at night and on weekends) or because of lack of sufficient tracheal secretions. During TEE examination, most patients were already sedated (93%) and sedation was increased in many of them (62%), but only few (n = 12, 12%) received additional neuromuscular blocking agent.
Altogether, 19/100 patients (19%) were diagnosed with VAP within three days after TEE. Patients’ characteristics at baseline and throughout TEE procedure with comparison between those who developed VAP and those who did not are shown in Tables 1 and 2, respectively. VAP patients had a larger tracheal tube size, endured more attempts of TEE probe introduction, and were more often on anticoagulants than no-VAP patients. TEE complications were scarce and similar in both groups. Among the 19 VAP episodes, three had no bacteriological documentation and six were polymicrobial. The causative microorganisms identified were Pseudomonas aeruginosa (seven cases), Klebsiella pneumoniae (six cases), Staphylococcus aureus (three cases), Enterobacter cloacae (three cases), Stenotrophomonas maltophilia (three cases), Escherichia coli (two cases) and Proteus mirabilis (one case).
Microaspiration
It was possible to assess pepsin and salivary amylase concentrations (sufficient amount of tracheal suction) in 82 patients before TEE, 83 patients after TEE, and 74 patients for both time points (Fig. 1). We detected 17/74 patients with TEE-associated microaspiration (prevalence of 23%, 95% confidence interval 15–34%), and this prevalence did not differ between the four participating centers. The concentrations of pepsin and salivary amylase were not different between VAP and no-VAP patients (Table 3). Moreover, median pepsin and salivary amylase levels were not significantly different before and after TEE (Figs. 2 and 3). No association was found between the occurrence of VAP within three days of TEE and TEE-associated microaspiration (Table 3). A sensitivity analysis assessing patients who developed VAP within 5 days following TEE (22/100, 22%) found similar results (Additional file 1: Table S1).
Continuous monitoring of tracheal cuff pressure
Continuous monitoring of tracheal cuff pressure throughout TEE process was performed in 20 patients, of whom six had TEE-associated microaspiration and three had VAP. Overall, as compared with baseline (2 min before TEE start), TEE induced an important increase in tracheal cuff pressure, especially during insertion and removal of the TEE probe (Fig. 4).
Discussion
To the best of our knowledge, this is the first study conducted to evaluate the impact of performing TEE on the occurrence of microaspiration and VAP in intubated critically ill patients. Although a substantial number of patients could be characterized as having TEE-associated microaspirations (23%), according to an ad hoc definition, the changes in pepsin and salivary amylase levels throughout TEE process showed huge interindividual variability. We detected no association between TEE-associated microaspiration and the development of VAP during the three days following TEE. However, because of the high rate of VAP observed after TEE and the limitations of our methods, our findings cannot formally rule out a role for TEE in the occurrence of VAP. TEE generated a transient variation of tracheal cuff pressure, especially upon inserting and removing the TEE probe.
Microaspiration is a well-known causative factor of VAP [23]. Pepsin and salivary amylase are reliable markers of microaspiration and are tightly linked to the development of VAP [21, 24, 25]. These markers have been used as surrogates in studies evaluating the efficacy of various devices in preventing VAP, as tracheal tubes [26], subglottic secretion drainage systems [27], and mechanical devices controlling tracheal cuff pressure [17]. In such studies, microaspiration assessment relied on several tracheal aspirates drawn over a wide timeframe (1 or 2 days), and its definition considered the percentage of tracheal aspirates with higher levels of pepsin (> 200 μg/L) and/or salivary amylase (> 1685 IU/L). For us, it was not possible to evaluate TEE-associated microaspiration using the same approach given the limited number of tracheal aspirates available in our protocol (only two/patient). Of more, we relied on commonly reported thresholds for salivary amylase and pepsin [8, 12, 26].
The continuous monitoring of tracheal cuff pressure throughout TEE procedure showed significant elevation of cuff pressure, especially during insertion and removal of the TEE probe. Persistent underinflation (< 20 cmH2O) of the tracheal cuff was shown as an independent risk factor for microaspiration and VAP [28], whereas cuff leakage was inversely correlated with cuff pressure [29]. Hypothesizing that acute variations of tracheal cuff pressure during TEE might be associated with microaspiration and VAP warrants further research.
The relatively high rate of VAP found in this study can be reasonably attributed to the severe cases we included. Of note, 38% of patients presented with acute respiratory distress syndrome. However, we cannot formally exclude a role of microaspiration in this high rate. The fact that patients who caught VAP had their tracheal tubes larger than those used in patients who did not may suggest more leaks occurring in the former group. Moreover, patients who caught VAP were more often on anticoagulant, a therapy that has potential anti-inflammatory effects beyond anticoagulation, and which may be beneficial in acute respiratory distress syndrome [30]. For instance, nebulized heparin was proposed for lung injury but with contradictory results [31] and was not effective in preventing VAP [32].
We did not identify any dreaded clinical complication associated with TEE neither did TEE significantly impact salivary amylase and pepsin concentrations. However, the substantial levels of pepsin and amylase observed in some patients and the fact that VAP patients had endured more attempts of TEE probe introduction might represent a good incentive to install some VAP prevention measures before and/or during TEE. Such measures may involve deep oropharyngeal suctioning [33], subglottic suctioning [34], semi-recumbent positioning [35], continuous control of tracheal cuff pressure [17], or using higher PEEP levels [29].
This multicenter study was conducted in four tertiary university ICUs where TEE is routinely used in intubated critically ill patients. The major strengths of the study are the comprehensive search for risk factors for microaspiration, its prospective design, the combined use of salivary amylase and pepsin for microaspiration documentation, and the continuous assessment of tracheal cuff pressure to scrutinize VAP pathophysiology. Our study has several limitations. First, the cohort included a relatively small number of patients with no control arm. Second, pepsin and salivary amylase and tracheal cuff pressure continuous monitoring were not assessed in all patients. Third, the definition of TEE-associated microaspiration may be questionable, as previously discussed. It used a single assessment of biomarkers and an arbitrary cutoff. We did not correct for baseline concentration of biomarkers in the digestive tract, but these biomarkers are not normally found in the respiratory tract and previous studies did not use such corrections. Fourth, the use of three days as a cutoff point to define VAP after TEE is also questionable, but results were similar upon using a five-day cutoff point. Fifth, we focused on direct microaspiration during TEE and did not assess other mechanisms that may cause pneumonia, as dysphagia or swallowing dysfunction [36]. Eventually, we did not assess the change in tracheal bacterial colonization. The amount of bacterial inoculum could be used as a closer surrogate for VAP [37]. Sixth, VAP would have been more relevant as a primary endpoint from a clinical point of view. However, if TEE has a potential impact on VAP, it is likely to be small given the multiple factors influencing VAP occurrence. We therefore used microaspiration as the primary endpoint because microaspiration is considered as the main mechanism of VAP. Lastly, the limitations of the methods used to identify TEE-associated microaspiration and the high rate of VAP observed after TEE cannot allow ruling out a role for TEE.
Conclusion
In this multicenter prospective observational study, we detected no association between TEE-associated microaspiration and the development of VAP during the three days following TEE. However, because of the high level of VAP observed after TEE and the limitations of the methods used, our findings cannot allow formally ruling out a role for TEE in the occurrence of VAP.
Availability of data and materials
All data generated and analyzed during the study are included in the published article and can be shared upon request. All authors helped to revise the draft of the manuscript. All authors read and approved the final manuscript.
Abbreviations
- VAP:
-
Ventilator-associated pneumonia
- ICU:
-
Intensive care unit
- TEE:
-
Transesophageal echocardiography
- CXR:
-
Chest X-rays
- SAPS II:
-
Simplified acute physiology score II
- SOFA:
-
Sequential organ failure assessment
- RASS:
-
Richmond agitation and sedation scale
References
Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903.
Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C. The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. The Canadian Critical Trials Group. Am J Respir Crit Care Med. 1999;159:1249–56.
Melsen WG, Rovers MM, Groenwold RHH, Bergmans DCJJ, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13:665–71.
Cook D, De Jonghe B, Brochard L, Brun-Buisson C. Influence of airway management on ventilator-associated pneumonia: evidence from randomized trials. JAMA. 1998;279:781–7.
Levine SA, Niederman MS. The impact of tracheal intubation on host defenses and risks for nosocomial pneumonia. Clin Chest Med. 1991;12:523–43.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–71.
Heyland DK, Drover JW, MacDonald S, Novak F, Lam M. Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized controlled trial. Crit Care Med. 2001;29:1495–501.
Nseir S, Zerimech F, Jaillette E, Artru F, Balduyck M. Microaspiration in intubated critically ill patients: diagnosis and prevention. Infect Disord Drug Targets. 2011;11:413–23.
Metheny NA, Dahms TE, Chang YH, Stewart BJ, Frank PA, Clouse RE. Detection of pepsin in tracheal secretions after forced small-volume aspirations of gastric juice. JPEN J Parenter Enter Nutr. 2004;28:79–84.
Nseir S, Zerimech F, De Jonckheere J, Alves I, Balduyck M, Durocher A. Impact of polyurethane on variations in tracheal cuff pressure in critically ill patients: a prospective observational study. Intensive Care Med. 2010;36:1156–63.
Filloux B, Bedel A, Nseir S, Mathiaux J, Amadeo B, Clouzeau B, et al. Tracheal amylase dosage as a marker for microaspiration: a pilot study. Minerva Anestesiol. 2013;79:1003–10.
Dewavrin F, Zerimech F, Boyer A, Maboudou P, Balduyck M, Duhamel A, et al. Accuracy of alpha amylase in diagnosing microaspiration in intubated critically-ill patients. PLoS ONE. 2014;9:e90851.
Vieillard-Baron A, Millington SJ, Sanfilippo F, Chew M, Diaz-Gomez J, McLean A, et al. A decade of progress in critical care echocardiography: a narrative review. Intensive Care Med. 2019;45:770–88.
Garcia YA, Quintero L, Singh K, Lakticova V, Iakovou A, Koenig SJ, et al. Feasibility, safety, and utility of advanced critical care transesophageal echocardiography performed by pulmonary/critical care fellows in a medical ICU. Chest. 2017;152:736–41.
Hüttemann E, Schelenz C, Kara F, Chatzinikolaou K, Reinhart K. The use and safety of transoesophageal echocardiography in the general ICU—a minireview. Acta Anaesthesiol Scand. 2004;48:827–36.
Mentec H, Vignon P, Terre S, Cholley B, Roupie E, Legrand P, et al. Frequency of bacteremia associated with transesophageal echocardiography in intensive care unit patients: a prospective study of 139 patients. Crit Care Med. 1995;23:1194–9.
Nseir S, Zerimech F, Fournier C, Lubret R, Ramon P, Durocher A, et al. Continuous control of tracheal cuff pressure and microaspiration of gastric contents in critically ill patients. Am J Respir Crit Care Med. 2011;184:1041–7.
American Thoracic S, Infectious Diseases Society of A. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416.
Klompas M, Branson R, Eichenwald EC, Greene LR, Howell MD, Lee G, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35:915–36.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Metheny NA, Clouse RE, Chang YH, Stewart BJ, Oliver DA, Kollef MH. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med. 2006;34:1007–15.
Metheny NA, Davis-Jackson J, Stewart BJ. Effectiveness of an aspiration risk-reduction protocol. Nurs Res. 2010;59:18–25.
Palmer LB. Ventilator-associated infection. Curr Opin Pulm Med. 2009;15:230–5.
Weiss CH, Moazed F, DiBardino D, Swaroop M, Wunderink RG. Bronchoalveolar lavage amylase is associated with risk factors for aspiration and predicts bacterial pneumonia. Crit Care Med. 2013;41:765–73.
Samanta S, Poddar B, Azim A, Singh RK, Gurjar M, Baronia AK. Significance of mini bronchoalveolar lavage fluid amylase level in ventilator-associated pneumonia: a prospective observational study. Crit Care Med. 2018;46:71–8.
Jaillette E, Girault C, Brunin G, Zerimech F, Behal H, Chiche A, et al. Impact of tapered-cuff tracheal tube on microaspiration of gastric contents in intubated critically ill patients: a multicenter cluster-randomized cross-over controlled trial. Intensive Care Med. 2017;43:1562–71.
Millot G, Boddaert P, Parmentier-Decrucq E, Palud A, Balduyck M, Maboudou P, et al. Impact of subglottic secretion drainage on microaspiration in critically ill patients: a prospective observational study. Ann Transl Med. 2018;6:416.
Rello J, Sonora R, Jubert P, Artigas A, Rue M, Valles J. Pneumonia in intubated patients: role of respiratory airway care. Am J Respir Crit Care Med. 1996;154:111–5.
Pitts R, Fisher D, Sulemanji D, Kratohvil J, Jiang Y, Kacmarek R. Variables affecting leakage past endotracheal tube cuffs: a bench study. Intensive Care Med. 2010;36:2066–73.
Camprubí-Rimblas M, Tantinyà N, Bringué J, Guillamat-Prats R, Artigas A. Anticoagulant therapy in acute respiratory distress syndrome. Ann Transl Med. 2018;6:36.
Juschten J, Tuinman PR, Juffermans NP, Dixon B, Levi M, Schultz MJ. Nebulized anticoagulants in lung injury in critically ill patients-an updated systematic review of preclinical and clinical studies. Ann Transl Med. 2017;5:444.
Bandeshe H, Boots R, Dulhunty J, Dunlop R, Holley A, Jarrett P, et al. Is inhaled prophylactic heparin useful for prevention and Management of Pneumonia in ventilated ICU patients? The IPHIVAP investigators of the Australian and New Zealand Intensive Care Society Clinical Trials Group. J Crit Care. 2016;34:95–102.
Sole ML, Talbert S, Yan X, Penoyer D, Mehta D, Bennett M, et al. Impact of deep oropharyngeal suctioning on microaspiration, ventilator events, and clinical outcomes: a randomized clinical trial. J Adv Nurs. 2019;75:3045–57.
Mao Z, Gao L, Wang G, Liu C, Zhao Y, Gu W, et al. Subglottic secretion suction for preventing ventilator-associated pneumonia: an updated meta-analysis and trial sequential analysis. Crit Care Lond Engl. 2016;20:353.
Wang L, Li X, Yang Z, Tang X, Yuan Q, Deng L, et al. Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation. Cochrane Database Syst Rev. 2016;1:CD009946.
Hogue CW, Lappas GD, Creswell LL, Ferguson TB, Sample M, Pugh D, et al. Swallowing dysfunction after cardiac operations: Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110:517–22.
Toews GB, Gross GN, Pierce AK. The relationship of inoculum size to lung bacterial clearance and phagocytic cell response in mice. Am Rev Respir Dis. 1979;120:559–66.
Acknowledgements
We are very indebted to Thiziri Sadaoui, Amelie Cerf, Claire Delcourte, and Celine Delatage-Metreau for their good hands in data acquisition and to Christian Brun-Buisson for his help in manuscript reviewing.
Funding
The present study has been conducted without any financial support.
Author information
Authors and Affiliations
Contributions
FB and AMD designed the study, performed statistical analyses and wrote the manuscript. FB, AR, VL, and FB collected the data and performed echocardiography. FZ, MB, PM analyzed the endotracheal aspirates. FZ, KR, NdP, GC, and SN helped design the study and contributed to the conception and quality assessment of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The protocol was approved by the ethical committee CPP, Ile de-France III (EUDRACT number: 2016-A01488-43, approval number: S.C.3457). The protocol was considered as a component of standard care, and patient consent was waived. Written and oral information about the study was given to patients or families.
Consent for publication
All authors have agreed to the publication of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1
. Microaspiration indicators and outcomes stratified by VAP incidence within 5 days after TEE.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bagate, F., Rouzé, A., Zerimech, F. et al. Transesophageal echocardiography-associated tracheal microaspiration and ventilator-associated pneumonia in intubated critically ill patients: a multicenter prospective observational study. Crit Care 24, 679 (2020). https://doi.org/10.1186/s13054-020-03380-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-020-03380-w