Abstract
Background
Bloodstream infections are associated with high morbidity and mortality, both of which contribute substantially to healthcare costs. The effects of early administration of appropriate antimicrobials on the prognosis and timing of defervescence of bacteremic patients remain under debate.
Methods
In a 6-year retrospective, multicenter cohort, adults with community-onset bacteremia at the emergency departments (EDs) were analyzed. The period from ED arrival to appropriate antimicrobial administration and that from appropriate antimicrobial administration to defervescence was regarded as the time-to-appropriate antibiotic (TtAa) and time-to-defervescence (TtD), respectively. The primary study outcome was 30-day mortality after ED arrival. The effects of TtAa on 30-day mortality and delayed defervescence were examined after adjustment for independent predictors of mortality, which were recognized by a multivariate regression analysis.
Results
Of the total 3194 patients, a TtAa-related trend in the 30-day crude (γ = 0.919, P = 0.01) and sepsis-related (γ = 0.909, P = 0.01) mortality rate was evidenced. Each hour of TtAa delay was associated with an average increase in the 30-day crude mortality rate of 0.3% (adjusted odds ratio [AOR], 1.003; P < 0.001) in the entire cohort and 0.4% (AOR, 1.004; P < 0.001) in critically ill patients, respectively, after adjustment of independent predictors of 30-day crude mortality. Of 2469 febrile patients, a TtAa-related trend in the TtD (γ = 0.965, P = 0.002) was exhibited. Each hour of TtAa delay was associated with an average 0.7% increase (AOR, 1.007; P < 0.001) in delayed defervescence (TtD of ≥ 7 days) after adjustment of independent determinants of delayed defervescence. Notably, the adverse impact of the inappropriateness of empirical antimicrobial therapy (TtAa > 24 h) on the TtD was noted, regardless of bacteremia severity, bacteremia sources, or causative microorganisms.
Conclusions
The delay in the TtAa was associated with an increasing risk of delayed defervescence and 30-day mortality for adults with community-onset bacteremia, especially for critically ill patients. Thus, for severe bacteremia episodes, early administration of appropriate empirical antimicrobials should be recommended.
Similar content being viewed by others
Background
Empirical administration of appropriate antimicrobials to septic or infective individuals has remained challenging because of the increased antibiotic resistance in both hospitals and communities [1] as well as atypical presentations in the specific population, such as the elderly [2] and human immunodeficiency virus-infected adults [3]. Particularly in septic patients presenting with a critical illness, inappropriate empirical therapy is associated with increased mortality [4, 5]. Generally, bloodstream infections lead to high morbidity and mortality and substantially contribute to healthcare costs [6]. However, whether appropriate initial antimicrobial administration has beneficial effects on the outcome of patients with bloodstream infections remains debated [4, 7,8,9,10,11].
To shorten the hospital stay, the timing of defervescence in response to antimicrobial therapy must be addressed. Numerous studies on bacteremia [12] and pneumonia [13, 14] found a significant association between defervescence timing and administration of antimicrobial classes. However, for bloodstream infections, the beneficial effect of rapid administration of appropriate antimicrobial therapy on defervescence remains unclear. Accordingly, we hypothesized that timely appropriate antimicrobial therapy heralds a favorable outcome and speedy defervescence, and a large cohort of adults with community-onset bacteremia was studied.
Methods
Study design
This retrospective cohort study was conducted at the emergency departments (EDs) of two hospitals in southern Taiwan: a university-affiliated medical center with 1200 beds and another teaching hospital with 800 beds. The patient (aged ≥ 18 years) with community-onset bacteremia from January 2010 to December 2015 was included. The study was approved by the institutional review board of two study hospitals and reported by the format recommended by STROBE (Strengthening the Reporting of Observational Studies in Epidemiology).
Data collection
During the study period, blood cultures sampled at the EDs were screened for bacterial growth by a computer database. Clinical information of adults with bacteremia was retrieved from medical charts (electronic and paper records). For the patients with multiple bacteremic episodes, only the first episode of each patient was included. Patients with community-onset bacteremia were eligible after the exclusion of those with hospital-onset bacteremia, contaminated blood cultures, bacteremia diagnosed prior to visiting the ED, incomplete clinical information of covariates listed in the predetermined case-record form, or uncertain fatality within 30 days after bacteremia onset. A predetermined record form was used to collect clinical variables, including age, vital signs at the EDs and during hospitalization, comorbidities and comorbidity severity (graded by the McCabe classification), image studies, the duration and type of antimicrobials and antipyretics administered, bacteremia sources, surgical record, the duration of hospital stay, bacteremia severity (evaluated by the Pitt bacteremia score), and patient outcomes. Furthermore, to study the time-to-defervescence (TtD), only febrile patients (with tympanic body temperature ≥ 38.3 °C) were included, and afebrile or hypothermic patients during the first 24 h after ED arrival, those with any dose of systemic steroid or antipyretics during antimicrobial therapy, those with inadequate source control, and those with uncertain date of defervescence were excluded. Two of the authors were randomly assigned to review electronic medical records and paper records. The primary study endpoint was the crude mortality within 30 days after ED arrival. The TtD, the duration of hospitalization, and the 30-day sepsis-related and crude mortality rate were regarded as the patient outcome.
Definitions
A patient aged ≥ 65 years was regarded as the elderly [15]. Community-onset bacteremia indicates that the place of onset of bacteremic episodes is the community, which includes long-term healthcare facility- and community-acquired bacteremia, as previously described [12, 16]. Polymicrobial bacteremia was defined as the isolation of more than one microbial species from a single bacteremic episode. Blood cultures with the growth of potentially contaminating pathogens were considered to be contaminated, based on the previous criteria [17].
As previously described [12, 16], antimicrobial therapy was considered appropriate when all of the following criteria were fulfilled: (i) the route and dosage of antimicrobial agents were administered as recommended in the Sanford Guide [18]; (ii) bacteremic pathogens were in vitro susceptible to the administrated antimicrobial agent based on the contemporary breakpoints of the Clinical and Laboratory Standards Institute (CLSI) [19]. The time-to-appropriate antibiotic (TtAa) was defined as the period between the bacteremia onset (i.e., ED triage) and administration of appropriate antimicrobials [16, 20].
Body temperature was measured within the first 24 h after ED arrival; if fever or hypothermia was observed more than once in one patient, the extreme temperature was recorded. Hypothermia was defined as temporal body temperature of ≤ 36.0 °C. Defervescence was defined as an afebrile state in which tympanic body temperature maintained at < 37.0 °C for at least 24 h [12, 21], and the TtD as the period between the initiation of appropriate antimicrobial administration and the onset of defervescence. The bacteremia severity was graded, according to a Pitt bacteremia score using a previously validated scoring system based on vital signs, use of intravenous vasopressors, mental status, receipt of mechanical ventilation, and cardiac arrest during the first 24 h after ED arrival [12, 16]. A high Pitt bacteremia score (≥ 4) was indicative of a critical illness, and a Pitt bacteremia score of < 4 was indicative of a non-critical illness. Comorbidities were defined as described previously [22], and malignancies included hematological malignancies and solid tumors. The prognosis of comorbid diseases was assessed by a previous established McCabe classification [23]. The removal of infected hardware, drainage of infected fluid collections, or resolution of obstruction in biliary or urinary tracts was referred as adequate source control for complicated bacteremia, as previously defined [24,25,26]. Crude mortality was used to define the death from all causes, and sepsis-related mortality was defined based on the circumstance of death, as determined by the review of the available recorded observation and septic parameters.
Microbiological methods
Blood cultures were incubated in a BACTEC 9240 instrument (Becton Dickinson Diagnostic Systems, Sparks, MD, USA) for 5 days at 35 °C. Bacterial species was identified by means of the Vitek 2 system (bioMe’rieux, Durham, NC), and antimicrobial susceptibility was determined by the disk diffusion method, based on contemporary CLSI standards [19]. To ensure the appropriateness of antimicrobial therapy for each bacteremia episode, aerobic isolates in the study period were prospectively stored. If empirical antibiotics were not included in the initial susceptibility panel, their susceptibility was measured after the inclusion in the study.
Statistical analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences for Windows (Version 23.0; Chicago, IL, USA). Clinical parameters were compared by the Fisher exact test or Pearson chi-square test for categorical variables and the independent t or Mann–Whitney U test for continuous variables. Trends in the TtAa and patient outcomes were analyzed by the equivalent linear-by-linear association test (i.e., Pearson’s correlation). To study the independent impact of TtAa delay on 30-day mortality or delayed defervescence, the variables with a P value of < 0.05 in the univariate analysis were included in a stepwise and backward multivariable logistic regression model. A P value of less than 0.05 was considered significant.
Results
Demographics and clinical characteristics of the entire cohort
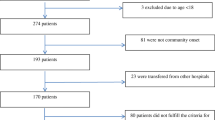
Of 6102 adults with bacterial growth in blood cultures, 3194 eligible patients with community-onset bacteremia were included, according to the inclusion and exclusion criteria (Fig. 1). Of 3194 patients, their mean age was 67.6 years and 1625 (50.9%) were male (Table 1). Overall, 2922 patients (91.5%) had hospitalization through the EDs, 105 (3.3%) died during the ED stay, and 167 (5.2%) discharged from the EDs and followed up in the outpatient clinics. Fever at the ED stay was noted in 2469 (77.3%) patients. The median (interquartile range, IQR) of the ED stay, intravenous antimicrobial administration, and hospitalization was 15.6 (5.9–26.7) h, 9 (5–16) days, and 11 (6–18) days, respectively. The proportion of critically ill patients at ED arrival was 20.2% (646 patients). The 30-day crude mortality rate in critically and non-critically ill patients was 46.7% (302) and 14.8% (472), respectively.
In the entire cohort (Table 1), the five leading sources of bacteremia were urinary tract infections (1034 patients, 32.4%), pneumonia (473, 14.8%), intra-abdominal infections (383, 12.0%), skin and soft-tissue infections (307, 9.6%), and biliary tract infections (272, 8.5%). The five major comorbidities included hypertension (1563 patients, 48.9%), diabetes mellitus (1187, 37.2%), malignancies (951, 29.8%), neurological diseases (735, 23.0%), and chronic kidney diseases (587, 18.4%). Patients with complicated bacteremia requiring source control accounted for 20.4% (653 patients), and those without adequate source control was merely 2.4% (78).
Bacteremic isolates and susceptibilities
Because of 306 (9.6%) episodes of polymicrobial bacteremia, a total of 3583 causative microorganisms from 3194 patients were collected. Gram-positive aerobes majorly included Staphylococcus aureus (418 isolates, 11.7%), Streptococcus species (396, 11.1%), and Enterococcus species (117, 3.3%). The five leading Gram-negative aerobes were Escherichia coli (1332 isolates, 37.2%), Klebsiella species (497, 13.9%), Pseudomonas species (129, 3.6%), Enterobacter species (96, 2.6%), and Proteus species (88, 2.5%).
Cefazolin, cefuroxime, cefotaxime, ceftazidime, cefepime, ertapenem, ampicillin/sulbactam, piperacillin/tazobactam, or levofloxacin was active against 8.6–76.0%, 16.6–88.6%, 87.1–95.6%, 85.1–96.6%, 95.4–100%, 96.8–100%, 17.6–89.9%, 91.2–100%, or 83.3–100%, respectively, of Gram-negative species. Imipenem was active against all Gram-negative aerobes. Methicillin-susceptible S. aureus and ampicillin-susceptible enterococci accounted for 37.8% (158 isolates) of staphylococci and 87.2% (102) of enterococci, respectively. Of 396 streptococci, 93.7% (371 isolates) were susceptible to penicillin.
Prognostic impact of TtAa in the entire cohort
For 3194 patients, the association of clinical variables, in terms of patient demography, bacteremia severity, bacteremia sources, comorbidity severity, and major comorbidities, with 30-day crude mortality was examined in the univariate analysis. The following variables were positively associated with 30-day mortality: the elderly, male, nursing-home residents, inadequate source control, fatal comorbidities (McCabe classification), a critical illness (a Pitt bacteremia score ≥ 4) at ED arrival, bacteremic pneumonia, and comorbidities with malignancies, neurological disorders, or liver cirrhosis (Table 2). In contrast, bacteremia due to urinary tract infections, biliary tract infections, or liver abscess was negatively associated with 30-day mortality. However, nursing-home residents, a critical illness at ED arrival, inadequate source control, bacteremic pneumonia, bacteremia due to urinary or biliary tract infections, fatal comorbidities (McCabe classification), and underlying malignancies or liver cirrhosis were independent prognostic factors in the multivariate regression analysis (Table 2).
In the entire cohort, the median (IQR) of TtAa was 2 (1–8) h. A positive TtAa-related trend in 30-day crude (γ = 0.919, P = 0.01) and sepsis-related (γ = 0.909, P = 0.01) mortality rate was evidenced in Fig. 2. Notably, the TtAa (measured by hours) remained to be a crucial determinant (adjusted odds ratio [AOR], 1.003; P < 0.001) of crude 30-day mortality, after adjustment of nine independent variables (Table 2).
Prognostic impact of TtAa in critically ill patients
Of 646 patients with a critical illness at ED arrival, the association of clinical variables and 30-day crude mortality was initially examined in a univariate analysis. The following variables were associated with 30-day mortality: fatal comorbidities (McCabe classification), bacteremic pneumonia, primary bacteremia, bacteremia due to urinary or biliary tract infections, and pre-existing malignancies, neurological disorders, or liver cirrhosis (Table 3). In the multivariate regression analysis, there were only three independent variables: fatal comorbidities (McCabe classification), and bacteremia due to urinary or biliary tract infections (Table 4). More importantly, the TtAa (measured by hours) remained to be a crucial predictor (AOR, 1.004; P < 0.001) of 30-day mortality, after adjustment of three independent variables.
Association of time-to-appropriate antibiotics and delayed defervescence in overall febrile patients
Among 2469 febrile patients, the median (IQR) of the TtD, the duration of intravenous antimicrobial administration, and the hospital stay was 4.5 (3.0–9.0), 9.0 (6.5–16.0), and 11.0 (7.0–19.0) days, respectively. Because the mean of the TtD was 6.7 days, a TtD of ≥ 7 days was regarded as delayed defervescence. In univariate analyses, nursing-home residents, a critical illness at ED arrival, polymicrobial bacteremia, bacteremic pneumonia, fatal comorbidities (McCabe classification), and comorbid malignancies were positively associated with delayed defervescence (Table 5). However, bacteremia due to urinary or biliary tract infections were negatively associated with delayed defervescence. In the multivariate regression model, four positive independent predictors (i.e., a critical illness at ED arrival, fatal comorbidities, bacteremic pneumonia, and comorbid malignancies) and two negative independent predictors (i.e., bacteremia due to urinary or biliary tract infections) of delayed defervescence were found (Table 5).
For febrile patients, there was a linear-by-linear association of the TtAa and the TtD (γ = 0.965, P = 0.002) (Fig. 3a). Furthermore, a TtAa-related trend in the duration of intravenous antimicrobial administration (γ = 0.964, P = 0.002) and hospital stay (γ = 0.957, P = 0.003) was evidenced in Fig. 3b. Of importance, the TtAa (measured by hours) was an independent determinant (AOR, 1.002; P = 0.001) of delayed defervescence, after adjustment of six independent predictors (Table 5).
Impact of time-to-appropriate antibiotics on defervescence in febrile patient subgroups
Of 2469 febrile patients, the mean TtD of 422 critically ill patients at ED arrival was longer than that of 2047 non-critically ill patients (10.2 vs. 6.0 days, P < 0.001). Of five leading bacteremic sources, the highest median (IRQ) of the TtD was observed in 296 patients with pneumonia, 10.0 (5.5–14.0) days, followed by 6.0 (3.5–10.0) days in 218 with skin and soft-tissue infections, 5.0 (2.5–9.0) days in 305 with intra-abdominal infections, 4.5 (2.5–7.0) days in 893 with urinary tract infections, and 4.0 (2.0–6.5) days in 223 with biliary tract infections. Of four major causative pathogens, the highest median (IQR) of the TtD was present in 280 patients with S. aureus bacteremia, 7.0 (4.5–14.0) days, followed by 5.5 (3.5–10.0) days in 378 with Klebsiella bacteremia, 5.0 (2.5–9.0) days in 275 with streptococcal bacteremia, and 4.0 (2.0–7.0) days in 1095 with E. coli bacteremia. Regardless of the initial presence of the critical or non-critical illness, bacteremic sources, or causative pathogens, inappropriate empirical antimicrobial therapy (TtAa > 24 h) was significantly related to a longer TtD (Fig. 4).
Discussion
Bacteremia is associated with substantial morbidity and mortality and thus is typically considered a severe presentation of systemic infections [6]. However, in contrast to the effects of appropriate empirical antibiotic therapy on severe sepsis or septic shock, the potential benefits of appropriate empirical therapy in bacteremia has achieved little consensus. Some studies reported minimal effect [10, 11], whereas some noted a significant reduction of case fatality rates [4, 7,8,9]. This controversy may be related to the variations in bacteremia severity, comorbidities, immune status, and distribution of causative microorganisms in the study patients [27]. Similar to two studies of bloodstream infections [7, 8], our results support that appropriate initial antimicrobial therapy could reduce short-term mortality in the setting of community-onset bacteremia.
It has been recognized that antimicrobial delays decreased short-term survival in patients with severe sepsis and septic shock [28, 29]. Likewise, the risk of mortality steadily increased; if appropriate, antimicrobial administration was delayed in our patients with community-onset bacteremia. Our cohort demonstrated that each hour of TtAa delay was associated with an increase in 30-day mortality rate of 0.4% in critically ill patients and 0.3% in all enrolled patients. Consequently, for severe bacteremic episodes, the appropriateness of empirical administration should be emphasized. Therefore, in addition to identifying those critically ill cases of bloodstream infections among febrile visitors at the EDs, timely empirical administration of broad-spectrum antimicrobial agents, epidemiological surveillance, and rapid detection of etiological pathogens and antimicrobial susceptibility is crucial for timely administration of appropriate antimicrobials.
The time gap between the initiation of antimicrobial administration and defervescence has been assessed as an outcome parameter in response to antimicrobial therapy in previous investigations of bloodstream infections [12, 30, 31]. Focusing on this outcome vastly linked to the hospital stay, our cohort highlighted the temporal association between the defervescence timing and the appropriateness of empirical antimicrobial therapy was evident in not only non-critically ill cases, but also critically ill ones at initial presentations. Such a therapeutic benefit of timely appropriate therapy also can be noted in the subgroup patients with variable bacteremic sources or causative pathogens. In other words, the association of delayed defervescence and inappropriate empirical antimicrobials was clearly and reasonably demonstrated herein.
Similar to several ED-based investigations of bloodstream infections [32, 33], the bacteremia source of urinary or biliary infections was a protective factor against mortality in our cohort, whereas bacteremia due to pneumonia was a crucial determinant of fatality. From our suspect, major reasons for the differences in the prognoses between these bacteremia sources may have been the different proportions for three most powerful prognostic factors recognized here, in terms of bacteremia severity at initial presentations, comorbidity severity, and adequate source control. For instance, compared with patients with bacteremia due to urosepsis, patients with bacteremic pneumonia had a significantly higher tendency to have a critical illness at ED arrival (228/473, 48.2% vs. 133/1034, 12.9%; P < 0.001), severe underlying diseases (i.e., fatal comorbidities) (159/473, 33.6% vs. 173/1034, 16.7%; P < 0.001), and inadequate source control (11/473, 2.3% vs. 8/1034, 0.8%; P = 0.01).
In addition to the timing of appropriate antimicrobial administration, the role of adequate source control for complicated bloodstream infections was examined herein. Consistent with published studies on severe sepsis [25] and complicated bacteremia [26], we found that inadequate source control was an independent determinant of short-term mortality. Although an association between adequate source control and the TtD was not evident in the literature, it is reasonable to assume individuals with inadequate source control have delayed defervescence. In our cohort, patients with inadequate source control for complicated bacteremia accounted only for the minority (2.4%), but the median TtD was longer in those with inadequate source control than in those who received adequate source control, irrespective of the appropriateness of empirical antimicrobial administration (appropriate, 11 vs. 4 h, P < 0.001; inappropriate, 84 vs. 74 h, P < 0.001). Therefore, to accurately assess the effect of the TtAa on the TtD, patients with inadequate source control was reasonably excluded from our analyses.
This study possesses several limitations. First, its retrospective and observational nature is the main limitation. However, the study cohort was large, and the record discrepancy was minimized by discussion between the chart reviewers during the capture of clinical information. Valuable information on the interaction between the TtAa and TtD has therefore been provided. Second, antimicrobial therapy is a cornerstone of clinical management for patients with bloodstream infections. Similar to the positive attitude on the appropriateness of empirical antimicrobial administration on patient outcomes [4, 7,8,9,10,11], our study had no detailed information of early goal-directed therapy and the sepsis bundle as covariates. Superior to these established reports, the impact of inadequate source control for complicated bacteremia was firstly highlighted herein. Third, in the analysis of the effect of antimicrobial therapy on patient survival, we excluded those with uncertain outcome. Although the chance that the excluded cases of unknown outcome were too severe to return the healthcare system is substantial, only 148 (4.4%) of 3342 adults with community-onset bacteremia were excluded and trivial selection bias is thus expected. Fourth, to prevent interference from several covariates linked to the TtD, patients with initial afebrile presentation or hypothermia, those with steroid therapy for severe sepsis or adrenal insufficiency, and those without adequate source control were excluded. Therefore, caution should be exercised in interpreting the effects of TtAa delay on the TtD. Finally, because the study hospitals were localized in southern Taiwan, a lack of an independent validation is one of the study limitations, and our results may not be extended to other population with variable infection sources, proportions of antimicrobial-resistant microorganisms, or bacteremia severity. However, several clinical predictors of short-term mortality identified in our cohort, including specific bacteremia sources (such as bacteremic pneumonia) and comorbidities (such as liver cirrhosis and malignancies), are consistent with earlier reports involving ED bacteremia [32, 33]. More importantly, the study findings from our large bacteremia cohort highlight that adults with community-onset bacteremia requires early administration of appropriate antimicrobials to achieve favorable outcomes and therapeutic efficacies, as noted before [16, 28, 29]. Additionally, the beneficial influence of rapid administration of appropriate antimicrobials on defervescence was the novelty for patients with bloodstream infections.
Conclusions
Regardless of bacteremia severity, early administration of appropriate antimicrobials is a crucial determinant of short-term outcomes in patients with community-onset bacteremia. Additionally, rapid administration of appropriate antimicrobials facilitated defervescence. Therefore, to achieve a favorable outcome and rapid defervescence, epidemiological surveillance, rapid pathogen identification, and the incorporation of broad-spectrum antimicrobial as empirical therapy into an antibiotic stewardship program should be considered, particularly in critically ill patients.
Availability of data and materials
Available from the corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- CLSI:
-
Clinical and Laboratory Standards Institute
- ED:
-
Emergency department
- ICUs:
-
Intensive care units
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- TtAa:
-
Time-to-appropriate antibiotic
- TtD:
-
Time-to-defervescence
References
Arias CA, Murray BE. Antibiotic-resistant bugs in the 21st century--a clinical super-challenge. N Engl J Med. 2009;360:439–43.
Berman P, Hogan DB, Fox RA. The atypical presentation of infection in old age. Age Ageing. 1987;16:201–7.
Lee CC, Chu FY, Ko WC, Chi CH. Different clinical presentation of community-onset bacteremia among human immunodeficiency virus-infected and human immunodeficiency virus-uninfected adults in the ED. Am J Emerg Med. 2014;32:1241–7.
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–55.
Kollef MH, Sherman G, Ward S, Fraser VJ. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115:462–74.
Bates DW, Pruess KE, Lee TH. How bad are bacteremia and sepsis? Outcomes in a cohort with suspected bacteremia. Arch Intern Med. 1995;155:593–8.
Lee CC, Lee CH, Chuang MC, Hong MY, Hsu HC, Ko WC. Impact of inappropriate empirical antibiotic therapy on outcome of bacteremic adults visiting the ED. Am J Emerg Med. 2012;30:1447–56.
Chen HC, Lin WL, Lin CC, Hsieh WH, Hsieh CH, Wu MH, et al. Outcome of inadequate empirical antibiotic therapy in emergency department patients with community-onset bloodstream infections. J Antimicrob Chemother. 2013;68:947–53.
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med. 1998;244:379–86.
Lin MY, Weinstein RA, Hota B. Delay of active antimicrobial therapy and mortality among patients with bacteremia: impact of severe neutropenia. Antimicrob Agents Chemother. 2008;52:3188–94.
Corona A, Bertolini G, Lipman J, Wilson AP, Singer M. Antibiotic use and impact on outcome from bacteraemic critical illness: the BActeraemia Study in Intensive Care (BASIC). J Antimicrob Chemother. 2010;65:1276–85.
Lee CC, Wang JL, Lee CH, Hsieh CC, Hung YP, Hong MY, et al. Clinical benefit of appropriate empirical fluoroquinolone therapy for adults with community-onset bacteremia in comparison with third-generation-cephalosporin therapy. Antimicrob Agents Chemother. 2017;61:e012174–16.
Welte T, Petermann W, Schurmann D, Bauer TT, Reimnitz P, Group MS. Treatment with sequential intravenous or oral moxifloxacin was associated with faster clinical improvement than was standard therapy for hospitalized patients with community-acquired pneumonia who received initial parenteral therapy. Clin Infect Dis. 2005;41:1697–705.
Bergallo C, Jasovich A, Teglia O, Oliva ME, Lentnek A, de Wouters L, et al. Safety and efficacy of intravenous tigecycline in treatment of community-acquired pneumonia: results from a double-blind randomized phase 3 comparison study with levofloxacin. Diagn Microbiol Infect Dis. 2009;63:52–61.
Lee CC, Wang JL, Lee CH, Hung YP, Hong MY, Chang CM, et al. Age-related trends in adults with community-onset bacteremia. Antimicrob Agents Chemother. 2017;61:e01050–17.
Lee CC, Lee CH, Hong MY, Tang HJ, Ko WC. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit Care. 2017;21:119.
Lee CC, Lin WJ, Shih HI, Wu CJ, Chen PL, Lee HC, et al. Clinical significance of potential contaminants in blood cultures among patients in a medical center. J Microbiol Immunol Infect. 2007;40:438–44.
Gilbert DN, Moellering RC Jr, Chambers HF, Saag MS. Selected pharmacologic faetures of antimicrobial agents. The Sanford Guide to Antimicrobial Therapy; 2009. p. 78–82.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; approved standard. Twenty-nineth informational supplement. CLSI document M100-S29. Wayne: CLSI; 2019.
Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–53.
Chang UI, Kim HW, Wie SH. Propensity-matched analysis to compare the therapeutic efficacies of cefuroxime versus cefotaxime as initial antimicrobial therapy for community-onset complicated nonobstructive acute pyelonephritis due to Enterobacteriaceae infection in women. Antimicrob Agents Chemother. 2015;59:2488–95.
Schellevis FG, van der Velden J, van de Lisdonk E, van Eijk JT, van Weel C. Comorbidity of chronic diseases in general practice. J Clin Epidemiol. 1993;46:469–73.
McCabe WR. Gram-negative bacteremia. Adv Intern Med. 1974;19:135–58.
Chotiprasitsakul D, Han JH, Cosgrove SE, Harris AD, Lautenbach E, Conley AT, et al. Comparing the outcomes of adults with Enterobacteriaceae bacteremia receiving short-course versus prolonged-course antibiotic therapy in a multicenter, propensity score-matched cohort. Clin Infect Dis. 2018;66:172–7.
Martinez ML, Ferrer R, Torrents E, Guillamat-Prats R, Goma G, Suarez D, et al. Impact of source control in patients with severe sepsis and septic shock. Crit Care Med. 2017;45:11–9.
Tellor B, Skrupky LP, Symons W, High E, Micek ST, Mazuski JE. Inadequate source control and inappropriate antibiotics are key determinants of mortality in patients with intra-abdominal sepsis and associated bacteremia. Surg Infect. 2015;16:785–93.
Kumar A. An alternate pathophysiologic paradigm of sepsis and septic shock: implications for optimizing antimicrobial therapy. Virulence. 2014;5:80–97.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96.
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42:1749–55.
Kim SH, Park WB, Lee CS, Kang CI, Bang JW, Kim HB, et al. Outcome of inappropriate empirical antibiotic therapy in patients with Staphylococcus aureus bacteraemia: analytical strategy using propensity scores. Clin Microbiol Infect. 2006;12:13–21.
Lee CH, Hsieh CC, Hong MY, Hung YP, Ko WC, Lee CC. Comparing the therapeutic efficacies of third-generation cephalosporins and broader-spectrum beta-lactams as appropriate empirical therapy in adults with community-onset monomicrobial Enterobacteriaceae bacteraemia: a propensity score matched analysis. Int J Antimicrob Agents. 2017;49:617–23.
Lin JN, Tsai YS, Lai CH, Chen YH, Tsai SS, Lin HL, et al. Risk factors for mortality of bacteremic patients in the emergency department. Acad Emerg Med. 2009;16:749–55.
Yeh CF, Chen KF, Ye JJ, Huang CT. Derivation of a clinical prediction rule for bloodstream infection mortality of patients visiting the emergency department based on predisposition, infection, response, and organ dysfunction concept. J Microbiol Immunol Infect. 2014;47:469–77.
Acknowledgements
We would like to thank Dr. Po-Lin Chen and the Core Research Laboratory of National Cheng Kung University Medical College for providing experimental space and facilities.
Funding
This study was partially supported by the research grants from the Ministry of Science and Technology (NSC102-2314-B-006-079), Ministry of Health and Welfare (MOHW106-TDU-B-211-113003), Sin-Lau Hospital (SLH-M106-01, SLH-M107-02, and SLH-M108-01), and National Cheng Kung University Hospital (NCKUH-10305018 and NCKUH--10406029), Tainan, Taiwan.
Author information
Authors and Affiliations
Contributions
CL, WK, and HT conceived the study idea and designed the study. CL, CY, HL, and MH supervised the data collection and chart reviews. CL, HL, WK, and HT provided methodological and statistical advice on study design and data analysis. CL, WK, and HT provided expertise in infectious disease, helped to draft this manuscript, and revised it carefully from a professional point of view. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of National Cheng Kung University Hospital (ER-100-182, 5th ed. revision) and Sin-Lau Hospital (SLH 9919-108-006), and the requirement of obtaining informed consent was waived.
Consent for publication
All authors have provided consent for publication of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, CC., Lee, CH., Yang, CY. et al. Beneficial effects of early empirical administration of appropriate antimicrobials on survival and defervescence in adults with community-onset bacteremia. Crit Care 23, 363 (2019). https://doi.org/10.1186/s13054-019-2632-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-019-2632-1