Abstract
Background
Neurological deterioration after intracerebral hemorrhage (ICH) is thought to be closely related to increased intracranial pressure (ICP), decreased cerebral blood flow (CBF), and brain metabolism. Transcranial Doppler (TCD) is increasingly used as an indirect measure of ICP, and quantitative EEG (QEEG) can reflect the coupling of CBF and metabolism. We aimed to combine TCD and QEEG to comprehensively assess brain function after ICH and provide prognostic diagnosis.
Methods
We prospectively enrolled patients with severe acute supratentorial (SAS)-ICH from June 2015 to December 2016. Mortality was assessed at 90-day follow-up. We collected demographic data, serological data, and clinical factors, and performed neurophysiological tests at study entry. Quantitative brain function monitoring was performed using a TCD-QEEG recording system at the patient’s bedside (NSD-8100; Delica, China). Univariate and multivariable analyses and receiver operating characteristic (ROC) curves were employed to assess the relationships between variables and outcome.
Results
Forty-seven patients (67.3 ± 12.6 years; 23 men) were studied. Mortality at 90 days was 55.3%. Statistical results showed there were no significant differences in brain symmetry index between survivors and nonsurvivors, nor between patients and controls (all p > 0.05). Only TCD indicators of the pulsatility index from unaffected hemispheres (UPI) (OR 2.373, CI 1.299–4.335, p = 0.005) and QEEG indicators of the delta/alpha ratio (DAR) (OR 5.306, CI 1.533–18.360, p = 0.008) were independent predictors for clinical outcome. The area under the ROC curve after the combination of UPI and DAR was 0.949, which showed better predictive accuracy compared to individual variables.
Conclusions
In patients with SAS-ICH, multimodal neuromonitoring with TCD combined with QEEG indicated that brain damage caused diffuse changes, and the predictive accuracy after combined use of TCD-QEEG was statistically superior in performance to any single variable, whether clinical or neurophysiological.
Similar content being viewed by others
Background
Spontaneous intracerebral hemorrhage (ICH), especially in patients with severe coma, has a high mortality and disability rate. The pathophysiology of ICH is incompletely understood; there is general agreement that the acute formation of a parenchymal hematoma produces tissue disruption and displacement [1]. Mortality in the early stage after ICH is attributable to increased intracranial pressure (ICP) and tissue shifts [2, 3]. Transcranial Doppler (TCD) is utilized as an indirect measure of ICP because higher ICP causes characteristic changes of decreased end-diastolic flow velocity (Vd) and increased pulsatility index (PI) in the Doppler waveform [4]. Several studies have confirmed that the PI of the unaffected hemisphere may be a predictor of death in acute ICH, suggesting that intracranial hypertension is the most likely cause of death in patients with ICH [5,6,7]. However, compared to patients with supratentorial cerebral infarction, patients with supratentorial cerebral hemorrhage are more prone to disturbance of consciousness; that is, changes in consciousness state after ICH, which are not always easily explained on the basis of increased ICP, mass effect, or herniation [8]. Relief of elevated ICP by ventricular drainage is commonly performed, and may improve the level of consciousness of patients with ICH with coma. Notwithstanding, coma often persists, implicating other causative pathology [9].
The secondary pathophysiological processes of ICH include progress in cerebral edema [10], activation of apoptotic processes [11], and the toxic effects of hematoma components [12, 13]; these factors can cause severe, persistent damage. Functional imaging with PET indicated that surrounding the hematoma was a region of reduced cerebral blood flow (CBF), cerebral metabolic rate for oxygen (CMRO2), and oxygen extraction fraction (OEF) [14]. Combined application of Xenon CT and PET in previous studies on CBF and CMRO2 has also shown that EEG changes can reflect the coupling of CBF and brain metabolism [15]. In comparison with primitive EEG, quantitative EEG (QEEG) has an advantage in quantification and interpretation. Delta power measures had the strongest negative correlation with CBF, and alpha power had a relatively strong positive correlation with CBF; increased power in slower frequency bands (delta and theta) and decreased power in faster frequency bands (alpha and beta) are seen with reductions in CMRO2 [15,16,17].
In this study, we sought to investigate whether it is possible to comprehensively evaluate brain function by administering TCD combined with QEEG in patients with severe acute supratentorial (SAS)-ICH, and to assess outcome at the 90-day follow-up; and to explore a new basis for pathophysiological changes in severe ICH.
Methods
Patients
In this prospective study, we consecutively enrolled patients with ICH with coma who were admitted to the Department of Neurology, First Hospital of Jilin University, China, between June 2015 and December 2016. The patients were included in our study if they met the following criteria: admission time ≤ 72 h after onset; presence of supratentorial hemorrhage; and Glasgow Coma Scale (GCS) score ≤ 8 points on admission, as assessed by an experienced neurologist. Exclusion criteria were the following: ICH secondary to aneurysm, vascular malformation, tumor, and cerebral infarction; deficient temporal acoustic bone window; scheduled surgical treatments, including ventricular drainage, clot removal, and craniotomies; middle cerebral artery or other intracranial and extracranial major vascular stenosis/occlusion; previous ischemic or hemorrhagic cerebrovascular disease; pathological changes that affect intracranial EEG activity, such as intracranial infection, ischemia anoxic encephalopathy, cerebral trauma, and others; presence of marked environmental turbulence, such as low temperature (core body temperature < 32 °C), hypoglycemia (<50 mg/dl), hyponatremia (<116 mg/dl), and others; and central nervous system depressant use, including sedative, narcotic, antidepressants, antipsychotics, antiepileptic drugs, and others. Fifteen age and sex-matched healthy controls (64.3 ± 13.5 years old, eight men) were recruited. Written informed consent was obtained from each patient’s immediate family members before the beginning of the study. The study was approved by the Ethics Committee of the First Hospital of Jilin University, China, and conformed to the tenets of the Declaration of Helsinki.
Clinical data
All patients received routine monitoring of vital signs and intensive nursing care in the Neurological Intensive Care Unit. We recorded and analyzed the following variables: demographics (age and sex); stroke risk factors (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, previous acute coronary event, smoking, excessive drinking); admission GCS score; time from ICH onset until the time monitoring commenced; whether blood pressure and glucose management were in accordance with current ICH management guidelines [18]; other admission laboratory tests (serum potassium, calcium, and sodium, white blood cell count, platelet count, activated partial thromboplastin time (APTT), International Normalized Ratio (INR)); neuroimaging variables (for regular hematoma, ICH volume was measured using length × width × depth/2; for irregular hematoma, length × width × depth/3 was adopted [19]—head CT with hematoma location and volume on admission was evaluated by a neuroradiologist blinded to the clinical and brain function data); and clinical outcome assessed using the 5-point Glasgow Outcome Scale score 90 days after ictus.
TCD-QEEG measurements
Patients were in the supine position during quantitative brain function monitoring. TCD was performed using 2-MHz pulsed-wave Doppler probes fixed to each temporal window with a helmet. The depth of acquiring optimal middle cerebral artery signals was 50–60 mm from both sides. Simultaneous EEG was obtained with standard 16-channel electroencephalography with silver chloride scalp electrodes placed in accordance with the 10–20 system; electrode impedance was maintained below 10 KΩ. The healthy control group remained with their eyes closed and awake during the process. Data were recorded for over 30 min until a stable recording was established; the recorded data were stored for further analysis.
Data analysis
Blinded analysis was performed for each patient. All clearly readable TCD waveforms were used in the calculations. The following variables were analyzed: systolic flow velocity (Vs), diastolic flow velocity (Vd), mean velocity (Vm), and PI from the affected and unaffected hemispheres. Vm was calculated using the following equation:
and PI was calculated using the following equation:
Offline QEEG analysis was performed using MATLAB (MathWorks, Natick, MA, USA). After data filtering (high pass 0.3 Hz, low pass 30 Hz) and all segments of artifact-free EEG were analyzed, spectral power was calculated using Fast Fourier transform (FFT) for each electrode over the 1–30 Hz range. The relative power of the delta (1–3 Hz, RDP), theta (4–7 Hz, RTP), alpha (8–13 Hz, RAP), and beta (14–30 Hz, RBP) frequency bands over all channels were used to calculate the global delta/alpha ratio (DAR) and the (delta + theta)/(alpha + beta) ratio (DTABR). The brain symmetry index (BSI) was calculated according to the following formula:
with the power of the signal obtained from a particular hemispheric bipolar channel pair i (with i = 1, 2, …, N) at frequency j (or Fourier coefficient, with index j = 1, 2, …, M), N being the number of channel pairs, M being the number of Fourier coefficients, Rij(t) and Lij(t) for the right and left hemisphere, respectively [20].
Statistical analysis
All statistical analyses were performed with SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) and MedCalc version 11.4.4 (MedCalc Software, Mariakerke, Belgium). In the univariate analysis, data were reported as mean and SD for normally distributed variables and as median and interquartile range (IQR) for nonnormally distributed variables. Categorical variables were presented as percentages. Student’s t tests and median two-sample tests were used for normally distributed variables. Nonparametric Wilcoxon (Kruskal–Wallis) analysis of variance was used for nonnormally distributed variables. The comparison of categorical variables was performed with the chi-squared test. From these analyses, we could select the variables with some prognostic significance (p ≤ 0.001). Then, we performed a backward stepwise logistic regression analysis with death at 90 days as the dependent variable. If a TCD or QEEG measure was statistically associated with survival, we calculated its separated and united sensitivity, specificity, and area under the curve with the aid of receiver operator characteristic (ROC) curves. ROC curves were compared by applying DeLong’s test. Calculated two-tailed p < 0.05 was considered statistically significant.
Results
Basic data
During a 1.5-year period, 76 consecutive patients were diagnosed with severe, acute, spontaneous supratentorial ICH. The following patients were excluded: admission beyond 72 h from onset of symptoms (n = 4), surgical procedure (n = 2), macrovascular stenosis (n = 7), previous cerebrovascular disease (n = 5), deficient temporal window (n = 6), signal artifacts (n = 3), and loss to follow-up (n = 2). Finally, we enrolled 47 patients, of which 26 (55.3%) died during the 90-day follow-up period. The median age was 67.3 ± 12.6 years, and 23 (48.9%) of the patients were male. The first TCD-QEEG was performed a mean of 31.0 (19.0–59.0) h after the onset of symptoms. No statistically significant differences between survivors and nonsurvivors were noted for clinical baseline data, including age, sex, risk factors, blood pressure, serum glucose, serum potassium, calcium, and sodium, white blood cell count, platelet count, APTT, INR, and hematoma location. Only larger hematoma volume (p < 0.0001) and higher Glasgow Coma Scale score (p = 0.001) were associated with mortality (Table 1).
Evaluation of brain function with TCD-QEEG
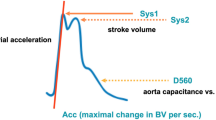
Figure 1 shows the CT and TCD-QEEG findings of representative patients.
Examples of representative patients. a Nonsurvivor patient. QEEG shows the slower delta frequency band significantly increased and the faster alpha frequency band significantly decreased. Moreover, DAR, but not BSI, also increased. TCD shows the PI of bilateral hemispheres significantly increased. b Survivor patient. QEEG and TCD show similar changes, but not as significant, to those seen in (a). BSI did not increase either. c Healthy control patient. QEEG and TCD normal. DAR delta/alpha ratio, DTABR (delta + theta)/(alpha + beta) ratio, BSI brain symmetry index, VS systolic flow velocity, VM mean flow velocity, VD diastolic flow velocity, PI pulsatility index, TCD transcranial Doppler, QEEG quantitative electroencephalography
Regarding TCD relevant indicators, Vd of unaffected hemispheres was lower in nonsurvivors (UVd p = 0.018) and the PI of both hemispheres was higher in nonsurvivors than survivors in patients with SAS-ICH (API p < 0.0001, UPI p < 0.0001) (Table 2 and Fig. 2b, c). Vm in the affected hemisphere and Vd and PI in both hemispheres showed significant differences (all p < 0.0001) between patients with ICH and healthy controls (Table 2 and Fig. 2a–c).
TCD and QEEG parameters in patients with ICH compared to healthy controls. TCD parameters: a affected hemisphere systolic flow velocity (AVS), mean flow velocity (AVM), and diastolic flow velocity (AVD); b unaffected hemisphere systolic flow velocity (UVS), mean flow velocity (UVM), and diastolic flow velocity (UVD); and c pulsatility index (PI). QEEG parameters: d relative band power of delta, theta, alpha, and beta; e delta/alpha ratio (DAR) and (delta + theta)/(alpha + beta) ratio (DTABR); and f brain symmetry index (BSI). #p < 0.05 for nonsurvivors vs survivors; *p < 0.05 for nonsurvivors vs healthy controls; +p < 0.05 for survivors vs healthy controls
Regarding QEEG relevant indicators, higher relative delta power (RDP p < 0.0001), lower relative alpha power (RAP p < 0.0001), higher delta/alpha ratio (DAR p < 0.0001), and higher (delta + theta)/(alpha + beta) ratio (DTABR p = 0.002) were associated with mortality in patients with SAS-ICH. All indicators except BSI showed significant differences (all p < 0.0001) between patients with ICH and healthy controls (Table 2 and Fig. 2d, e). There were no significant differences in BSI between survivors and nonsurvivors or between patients and controls (all p > 0.05) (Table 2 and Fig. 2f).
Multivariate analysis
All p ≤ 0.001 variables in the univariate analysis were entered into a logistic regression model with mortality at 90 days as the dependent variable. The result showed that only DAR (OR 5.306, CI 1.533–18.360, p = 0.008) and UPI (adjusted OR 2.373, CI 1.299–4.335, p = 0.005) were identified as independent predictors for mortality at 90 days after SAS-ICH. The results of the logistic regression analysis remained unchanged when we excluded the GCS score and hematoma volume to verify model stability.
Comparison of ROC curves
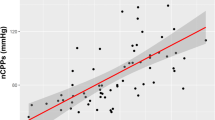
To determine whether the combination of TCD and QEEG variations in the model improved outcome prediction, we compared the ROC curves of five models: the first model was obtained by the GCS score, the second model contained the hematoma volume, the third model was obtained by the independent predictors of TCD with UPI, the fourth model was obtained by the independent predictors of QEEG with DAR, and the final model included both UPI and DAR. All models could predict mortality in patients with ICH at 90 days. The final model attained a high prognostic power, as the area under the ROC curve was 0.949 when UPI and DAR were combined. The contribution of the final model was significant, while each variable alone did not seem to be significant (Fig. 3).
Comparison of ROC curves to predict outcome in this cohort between five models: Glasgow Coma Scale (GCS), AUROC 0.776 (0.630–0.884); hematoma volume, AUROC 0.816 (0.676–0.914); unaffected side pulsatility index (UPI), AUROC 0.822 (0.683–0.918); delta/alpha ratio (DAR), AUROC 0.860 (0.728–0.944); transcranial Doppler (TCD) + quantitative electroencephalography (QEEG), AUROC 0.949 (0.842–0.992). p < 0.05 for TCD (UPI) + QEEG (DAR) comparison with GCS, hematoma volume, UPI (independent predictor of TCD), and DAR (independent predictor of QEEG). AUROC area under the receiver operating curve
Discussion
To our knowledge, this is the first study that focused on combined application of TCD-QEEG to assess the brain function of patients with SAS-ICH, and its prospective design could provide 90-day prognostic information. The results mainly suggested that TCD parameters of response to ICP and QEEG parameters of response to CBF and brain metabolism were significantly changed; UPI in TCD and DAR in QEEG were two independent predictors for 90-day mortality. Moreover, the area under the ROC curve after the combination of UPI and DAR was 0.949, which was superior to any single variable.
In previous studies, a variety of scales based on clinical data have often been used to assess ICH mortality and prognosis; variables that enter the scale usually include age, NIHSS score, GCS score, blood glucose, location of ICH, hematoma volume, intraventricular hemorrhage, and others [21,22,23]. After analyzing these clinical variables, we found that only GCS score and hematoma volume were associated with mortality. However, after entering these factors into the multiple regression model, they were not independent predictors. The reason may be that we enrolled patients with coma with GCS score ≤ 8, where GCS score and hematoma volume no longer have significant advantage in predicting prognosis in severe ICH.
TCD can assess intracranial compliance and, to some extent, reflect the level of ICP when it increases. The reason for the increase in ICP may be through a rise in intracranial volume, or secondarily through acute obstructive hydrocephalus [24]. The progressive increase in ICP and the decrease in cerebral perfusion pressure (CPP) significantly affect the Doppler waveform; typical changes include decreased Vd and increased PI. Mayer et al.’s [5] study showed that alterations in PI more reliably reflected intracranial lesion volume, and TCD could assess the asymmetry of intracranial hemodynamics. Martí-Fàbregas et al. [6] suggested that TCD is effective for assessing intracranial hypertension, and elevated UPI can predict 30-day outcome in patients with ICH. Kiphuth et al. [7] found that early PI monitoring by TCD correlated with ICP, and may be used to predict the outcome after 6 months. Our study on TCD drew a similar conclusion; decreased UVd and increased bilateral PI were significantly correlated with 90-day mortality, and API and UPI were the more significant predictors. Multivariate regression analysis showed that UPI was an independent prognostic factor.
QEEG is capable of quantitatively reflecting changes in intracranial neuronal activity, CBF, and metabolism. Powers used PET-measured CBF and CMRO2 in patients with ICH, and found that both perihematomal CBF and CMRO2 were significantly reduced compared to the contralateral side [25]. QEEG changes after ICH have not been reported; many QEEG studies of ischemic stroke have confirmed that QEEG correlates well with CBF and brain metabolism (CMRO2) in early subacute ischemic stroke. Finnigan et al. [26] assessed patients with acute supratentorial infarction, and suggested that DAR and RAP were positively correlated with the 30-day NIHSS score. Cuspineda et al. [27] reported (sub)acute ischemic stroke RDP to be the most significant and RAP the next best predictor of the 3-month outcome. Finnigan et al. [28] found that DAR showed maximal accuracy for discriminating between patients with acute ischemic stroke and controls. Our study also showed that the slower frequency band delta power increased and the faster frequency band alpha power decreased with the aggravation of brain injury. RDP, RAP, DAR, and DTABR were all significantly correlated with 90-day mortality; DAR and DTABR were the most significant among them. Multivariate regression analysis showed that DAR was an independent prognostic factor.
Many questions remain regarding the pathophysiological changes in ICH. Severely impaired consciousness is more common with acute supratentorial ICH than with supratentorial infarction ischemic stroke [8]. Alterations in consciousness following ICH are not always easily explained by increased ICP or herniation. We also found that in some patients with severe supratentorial ICH, clinical indications, state of consciousness, and QEEG indicate that the patient is in a state of exhaustion, but the TCD waveform is normal, and PI is not high in the last few hours of monitoring. Additionally, we found that there was no difference in BSI between severe ICH and healthy controls in QEEG. The BSI is an indicator of bilateral hemisphere damage symmetry, while in ischemic stroke the BSI or pairwise-derived BSI significantly increased, and the degree of increase was significantly related to prognosis [29, 30]. It may, therefore, be assumed that brain damage in hemorrhagic stroke is diffuse, unlike in ischemic stroke. Neuroimaging has provided objective evidence of damage to the contralateral hemisphere in unilateral ICH. Zazulia et al. [31] reported swelling of the bilateral hemispheres during the first week following acute supratentorial ICH.
Our study aimed at evaluating the brain function of severe supratentorial ICH using TCD combined with QEEG, and obtained good results, which can be utilized in future research in numerous ways. First, we hope to expand the sample size and obtain the boundary value, which could better guide clinical applications. Second, we could compare brain function of TCD-QEEG with functional imaging, and intensively study the mechanism of ICH. Third, a series of studies have confirmed that there are many similarities between acute ICH and TBI in pathogenesis and clinical manifestations. If TCD and QEEG monitoring of these two groups of patients are performed simultaneously, perhaps we can provide a new basis for the disease pathogenesis. Finally, with the undergoing intensive studies on the pathophysiological mechanisms that follow ICH, new treatment methods are bound to appear. TCD combined with QEEG can dynamically, rapidly, and in a timely manner respond to the changes in brain function before and after treatment.
This study has some limitations. First, this was a single-center study in a university hospital setting, and the sample was relatively small. Thus, prospective validation in different settings and with larger samples is needed. Second, we only monitored the patients in the acute phase, and did not perform dynamic monitoring, which is helpful in comprehensively understanding the changes of brain function with disease progression. Well-designed multicenter TCD combined with QEEG dynamic monitoring studies with a larger sample are urgently needed in the future to provide more information for understanding brain functional changes after ICH.
Conclusions
This study demonstrated that in patients with SAS-ICH, brain damage caused diffuse changes, evident with multimodality neuromonitoring of TCD combined with QEEG; UPI and DAR were independent predictors of 90-day clinical outcome. Diagnostic power after combined use of TCD-QEEG is statistically superior in performance to any single variable, whether clinical or neurophysiological.
Abbreviations
- APTT:
-
Activated partial thromboplastin time
- BSI:
-
Brain symmetry index
- CBF:
-
Cerebral blood flow
- DAR:
-
Delta/alpha ratio
- DTABR:
-
(Delta + theta)/(alpha + beta)ratio
- GCS:
-
Glasgow Coma Scale
- ICH:
-
Intracerebral hemorrhage
- ICP:
-
Intracranial pressure
- INR:
-
International Normalized Ratio
- PI:
-
Pulsatility index
- QEEG:
-
Quantitative electroencephalography
- RAP:
-
Relative alpha power
- RBP:
-
Relative beta power
- RDP:
-
Relative delta power
- RTP:
-
Relative theta power
- TCD:
-
Transcranial Doppler
- Vd:
-
Diastolic flow velocity
- Vm:
-
Mean flow velocity
- Vs:
-
Systolic flow velocity
References
NINDS ICH Workshop Participants. Priorities for clinical research in intracerebral hemorrhage: report from a National Institute of Neurological Disorders and Stroke workshop. Stroke. 2005;36:e23–41.
Franke CL, van Swieten JC, Algra A, van Gijn J. Prognostic factors in patients with intracerebral haematoma. J Neurol Neurosurg Psychiatry. 1992;55:653–7.
Counsell C, Boonyakarnkul S, Dennis M, Sandercock P, Bamford J, Burn J, et al. Primary intracerebral haemorrhage in the Oxfordshire Community Stroke Project. Cerebrovasc Dis. 1995;5:26–34.
Hassler W, Steinmetz H, Gawlowski J. Transcranial Doppler ultrasonography in raised intracranial pressure and in intracranial circulatory arrest. J Neurosurg. 1988;68:745–51.
Mayer SA, Thomas CE, Diamond BE. Asymmetry of intracranial hemodynamics as an indicator of mass effect in acute intracerebral hemorrhage. A transcranial Doppler study. Stroke. 1996;27:1788–92.
Martí-Fàbregas J, Belvis R, Guardia E, Cocho D, Munoz J, Marruecos L, et al. Prognostic value of Pulsatility Index in acute intracerebral hemorrhage. Neurology. 2003;61:1051–6.
Kiphuth IC, Huttner HB, Dörfler A, Schwab S, Köhrmann M. Doppler pulsatility index in spontaneous intracerebral hemorrhage. Eur Neurol. 2013;70:133–8.
Poungvarin N, Viriyavejakul A, Komontri C. Siriraj stroke score and validation study to distinguish supratentorial intracerebral haemorrhage from infarction. BMJ. 1991;302:1565–67.
Adams RE, Diringer MN. Response to external ventricular drainage in spontaneous intracerebral hemorrhage with hydrocephalus. Neurology. 1998;50:519–23.
Gebel JM, Jauch EC, Brott TG, Khoury J, Sauerbeck L, Salisbury S, et al. Natural history of perihematomal edema in patients with hyperacute spontaneous intracerebral hemorrhage. Stroke. 2002;33:2631–5.
Qureshi AI, Ling GS, Khan J, Suri MF, Miskolczi L, Guterman LR, et al. Quantitative analysis of injured, necrotic, and apoptotic cells in a new experimental model of intracerebral hemorrhage. Crit Care Med. 2001;29:152–7.
Aronowski J, Zhao X. Molecular pathophysiology of cerebral hemorrhage: secondary brain injury. Stroke. 2011;42:1781–6.
Lee ST, Chu K, Sinn DI, Jung KH, Kim EH, Kim SJ, et al. Erythropoietin reduces perihematomal inflammation and cell death with enos and stat3 activations in experimental intracerebral hemorrhage. J Neurochem. 2006;96:1728–39.
Zazulia AR, Diringer MN, Videen TO, Adams RE, Yundt K, Aiyagari V, et al. Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab. 2001;21:804–10.
Nagata K, Tagawa K, Hiroi S, Shishido F, Uemura K. Electroencephalographic correlates of blood flow and oxygen metabolism provided by positron emission tomography in patients with cerebral infarction. Electroencephalogr Clin Neurophysiol. 1989;72:16–30.
Laman DM, Wieneke GH, van Duijn H, Veldhuizen RJ, van Huffelen AC. QEEG changes during carotid clamping in carotid endarterectomy: spectral edge frequency parameters and relative band power parameters. J Clin Neurophysiol. 2005;22:244–52.
Tolonen U, Sulg IA. Comparison of quantitative EEG parameters from four different analysis techniques in evaluation of relationships between EEG and CBF in brain infarction. Electroencephalogr Clin Neurophysiol. 1981;51:177–85.
Morgenstern LB, Hemphill 3rd JC, Anderson C, Becker K, Broderick JP, Connolly Jr ES, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for health-care professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41:2108–29.
Huttner HB, Steiner T, Hartmann M, Köhrmann M, Juettler E, Mueller S, et al. Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke. 2006;37:404–8.
Van Putten MJ, Tavy DL. Continuous quantitative EEG monitoring in hemispheric stroke patients using the brain symmetry index. Stroke. 2004;35:2489–92.
Parry-Jones AR, Abid KA, Di Napoli M, et al. Accuracy and clinical usefulness of intracerebral hemorrhage grading scores: a direct comparison in a UK population. Stroke. 2013;44:1840–5.
Ruiz-Sandoval JL, Chiquete E, Romero-Vargas S, Padilla-Martínez JJ, González-Cornejo S. Grading scale for prediction of outcome in primary intracerebral hemorrhages. Stroke. 2007;38:1641–44.
Ji R, Shen H, Pan Y, Wang P, Liu G, Wang Y, et al. A novel risk score to predict 1-year functional outcome after intracerebral hemorrhage and comparison with existing scores. Crit Care. 2013;17:R275.
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373:1632–44.
Powers WJ. Intracerebral hemorrhage and head trauma: common effects and common mechanisms of injury. Stroke. 2010;41:S107–10.
Finnigan SP, Walsh M, Rose SE, Chalk JB. Quantitative EEG indices of sub-acute ischaemic stroke correlate with clinical outcomes. Clin Neurophysiol. 2007;118:2525–32.
Cuspineda E, Machado C, Galán L, Aubert E, Alvarez MA, Llopis F, et al. QEEG prognostic value in acute stroke. Clin EEG Neurosci. 2007;38:155–60.
Finnigan S, Wong A, Read S. Defining abnormal slow EEG activity in acute ischaemic stroke: delta/alpha ratio as an optimal QEEG index. Clin Neurophysiol. 2016;127:1452–9.
Van Putten MJAM, Peters JM, Mulder SM, de Haas JAM, Bruijninckx CMA, Tavy DLJ. A brain symmetry index (BSI) for online EEG monitoring in carotid endarterectomy. Clin Neurophysiol. 2004;115:1189–94.
Sheorajpanday RV, Nagels G, Weeren AJ, van Putten MJ, De Deyn PP. Reproducibility and clinical relevance of quantitative EEG parameters in cerebral ischemia: a basic approach. Clin Neurophysiol. 2009;120:845–55.
Zazulia AR, Videen TO, Diringer MN, Powers WJ. Poor correlation between perihematomal MRI hyperintensity and brain swelling after intracerebral hemorrhage. Neurocrit Care. 2011;15:436–41.
Acknowledgements
The authors thank Qiang Zhang and Ying Wang for providing technical assistance in TCD-QEEG monitoring.
Funding
There are no funding sources to declare.
Availability of data and materials
The datasets collected and/or analyzed during this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
YC contributed to study conception and design, data collection, analysis and interpretation, and drafting of the manuscript. YqX and JcF contributed to study conception and design, analysis and interpretation of the data, and revision of the final manuscript. WhX contributed to study conception and design, analysis and interpretation of the data, and revision of the manuscript. LjW contributed to data collection and revision of the manuscript. XmY contributed to study conception and design, data collection, and analysis and interpretation. JC and FD contributed to study conception and design and revision of the manuscript. All authors gave final approval of the version to be published.
Corresponding authors
Ethics declarations
The study was approved by the Ethics Committee of the First Hospital of Jilin University, and written informed consent was provided by each patient’s next of kin/participant.
Consent for publication
Written informed consent was obtained from each patient’s next of kin/participant for publication of their individual details and accompanying images in this manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, Y., Xu, W., Wang, L. et al. Transcranial Doppler combined with quantitative EEG brain function monitoring and outcome prediction in patients with severe acute intracerebral hemorrhage. Crit Care 22, 36 (2018). https://doi.org/10.1186/s13054-018-1951-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-018-1951-y