Abstract
Background
When conventional high-volume, low-pressure cuffs of endotracheal tubes (ETTs) are inflated, channel formation due to folds in the cuff wall can occur. These channels facilitate microaspiration of subglottic secretions, which is the main pathogenic mechanism leading to intubation-related pneumonia. Ultrathin polyurethane (PU)-cuffed ETTs are developed to minimize channel formation in the cuff wall and therefore the risk of microaspiration and respiratory infections.
Methods
We systematically reviewed the available literature for laboratory and clinical studies comparing fluid leakage or microaspiration and/or rates of respiratory infections between ETTs with polyvinyl chloride (PVC) cuffs and ETTs with PU cuffs.
Results
The literature search revealed nine in vitro experiments, one in vivo (animal) experiment, and five clinical studies. Among the 9 in vitro studies, 10 types of PU-cuffed ETTs were compared with 17 types of PVC-cuffed tubes, accounting for 67 vs. 108 experiments with 36 PU-cuffed tubes and 42 PVC-cuffed tubes, respectively. Among the clinical studies, three randomized controlled trials (RCTs) were identified that involved 708 patients. In this review, we provide evidence that PU cuffs protect more efficiently than PVC cuffs against fluid leakage or microaspiration. All studies with leakage and/or microaspiration as the primary outcome demonstrated significantly less leakage (eight in vitro and two clinical studies) or at least a tendency toward more efficient sealing (one in vivo animal experiment). In particular, high-risk patients intubated for shorter periods may benefit from the more effective sealing capacity afforded by PU cuffs. For example, cardiac surgery patients experienced a lower risk of early postoperative pneumonia in one RCT. The evidence that PU-cuffed tubes prevent ventilator-associated pneumonia (VAP) is less robust, probably because microaspiration is postponed rather than eliminated. One RCT demonstrated no difference in VAP risk between patients intubated with either PU-cuffed or PVC-cuffed tubes, and one before-after trial demonstrated a favorable reduction in VAP rates following the introduction of PU-cuffed tubes.
Conclusions
Current evidence can support the use of PU-cuffed ETTs in high-risk surgical patients, while there is only very limited evidence that PU cuffs prevent pneumonia in patients ventilated for prolonged periods.
Similar content being viewed by others
Background
Intubation-related pneumonia, including ventilator-associated pneumonia (VAP) or early postoperative pneumonia, remains a feared complication in the acute healthcare setting. Despite a plethora of preventive measures and growing attention to care bundle initiatives for patients at risk, the average occurrence rate of VAP among intensive care unit (ICU) patients intubated for at least 2 days ranges from 10 % to 20 % [1–5]. This is particularly worrisome, given the substantial clinical and economic burden of this infectious complication [6]. With an excess length of ICU stay of 5–7 days, there exists an important cost-saving potential [3].
The main pathogenic mechanism of intubation-related pneumonia is bacterial translocation from the stomach and/or oropharynx to the lower respiratory tract. Within a few hours following endotracheal intubation, pathogenic microorganisms colonize the oropharyngeal mucosa, dental plaque, stomach, and sinuses. As such, microbiologically contaminated subglottic secretions accumulate above the cuff of the endotracheal tube (ETT). While the purpose of the cuff is to seal the extraluminal airway, its effectiveness is not flawless. When conventional high-volume, low-pressure (HVLP) cuffs are inflated, channel formation due to folds in the cuff wall can occur. These channels facilitate microaspiration of subglottic secretions, even when the cuff pressure (Pcuff) is adequate (20–30 cmH2O) [7].
Ultrathin polyurethane (PU) cuffs have been developed to minimize the channel size within the folds of an inflated cuff. While the cuff membrane thickness of conventional polyvinyl chloride (PVC) cuffs is about 50–70 μm, the cuff wall thickness of PU cuffs ranges from 7 to 10 μm [8]. Therefore, the intention of these PU-cuffed ETTs is that the relatively smaller cuff channels will minimize microaspiration of subglottic secretions and thus the risk for intubation-related pneumonia. The purpose of this study was to systematically review the evidence, including that from laboratory and clinical investigations, concerning the effectiveness of PU-cuffed ETTs to minimize fluid leakage (microaspiration) and intubation-related pneumonia compared with conventional PVC-cuffed ETTs.
Methods
Search strategy
The PubMed, EMBASE, and Web of Science databases were each systematically searched using the following key terms: “endotracheal” OR “tracheal,” “poly-urethane” OR “polyurethane,” AND “cuff.” Additionally, the snowball method was used to detect potentially eligible studies. The literature searches were performed on 7 December 2015 without time or language restriction. No predefined review protocol was registered.
Study selection
Eligible studies included nonclinically (i.e., laboratory) or clinically controlled studies in which fluid leakage (either laboratory or clinical studies) or intubation-related pneumonia (clinical studies) was compared between PU- and PVC-cuffed ETTs. Search results were screened by title and abstract. Selected papers underwent a full-text assessment, and eligibility issues were resolved between authors. Reference inclusion and exclusion criteria for this review are described in Table 1.
Data extraction and quality assessment
Extracted data included study setting, design, and sample size; implemented interventions; definitions; presence or volume of fluid leakage; and rates of respiratory infections. The methodological quality (i.e., risk of bias) of included randomized controlled trials (RCTs) was assessed using the Jadad quality scale, which assigns a score ranging from 0 to 5 points, with a score ≥3 indicating a high-quality study [9]. Evaluation criteria in the Jadad scale assessment include randomization, blinding, and accounting for all study subjects. For non-RCTs, the risk of bias was assessed using the Downs and Black tool [10]. This score is based on 27 questions related to reporting of the data, internal and external validity, and factors potentially confounding internal validity. Summaries of the methodological evaluations of included RCTs and non-RCTs are shown in Additional file 1.
According to the objective of this review, for studies evaluating multiple types of ETTs, only comparisons of PU-cuffed ETTs with conventional PVC-cuffed tubes were selected (see also Table 1 for inclusion and exclusion criteria). If necessary, statistical analyses were performed on reported data in the original articles (Fisher’s exact test for comparison of leakage and/or pneumonia rates). Where necessary, the authors of the original studies were contacted to provide additional information.
Results and discussion
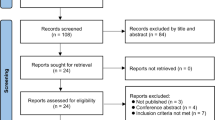
The search strategy yielded 205 records. Following title, abstract, and full-text assessments, 14 publications were included for final evaluation (Fig. 1). The studies included nine different in vitro experiments (Table 2), one in vivo experiment (Table 2), and five clinical studies (Table 3).
In vitro studies
Among the 9 in vitro studies, 10 types of PU-cuffed ETTs were compared with 17 types of PVC-cuffed tubes, accounting for 67 vs. 108 experiments with 36 PU-cuffed tubes and 42 PVC-cuffed tubes, respectively (Table 2). The results of these studies were generally in favor of PU-cuffed tubes, primarily because they demonstrated no or, compared with PVC-cuffed tubes, less fluid leakage. Several aspects of the experimental setup should be considered, including shape and elasticity of the trachea model, positioning of the tube, room temperature, gel lubrication of the cuff, Pcuff, viscosity of the fluid, ventilatory simulation and positive end-expiratory pressure (PEEP), additional cuff characteristics, and duration of the leakage observation. These aspects are summarized in Table 2.
Gel lubrication of ETT cuffs reduces the risk of microaspiration by plugging channels formed in the cuff wall. In one study, the sealing capacity of cuffs was tested with and without gel lubrication. Improved sealing was observed in all tested tubes except one PVC-cuffed tube [8]. On the one hand, an argument in favor of not using lubricated cuffs is that in such experiments the sole potential of cuff material to avoid leakage was evaluated. On the other hand, gel lubrication is standard in daily practice, albeit to smoothen the intubation maneuver in the first place.
The viscosity of the test fluid is another issue in which in vitro experiments might deviate from the clinical situation. All but one of the included in vitro studies used (dyed) water to evaluate the sealing ability of the cuffs. Li Bassi et al., however, used an oropharyngeal secretion simulant [11]. In this investigation, PU-cuffed tubes sealed more efficiently than PVC-cuffed tubes.
PEEP plays an important role in the risk of microaspiration because the upward pressure that it exerts on an ETT cuff enables better sealing capacities and thus reduces microaspiration and pneumonia [12]. Dave et al. [13] tested cuffed ETTs under various levels of positive pressure ventilation, with either 5 or 10 cmH2O PEEP, simulation of an endotracheal suction maneuver using a closed suction catheter with variable suction pressure (either −20000 or −30000 Pa), and variable duration of suctioning (5–20 seconds). Significantly less fluid leakage was observed among PU-cuffed tubes than in PVC-cuffed tubes, regardless of PEEP or suctioning settings. Lucangelo et al. demonstrated that PVC-cuffed ETTs leaked whether exposed to PEEP or not, while PU-cuffed ETTs did not leak under either circumstance [14]. Zanella et al. evaluated fluid leakage according to various PEEP levels (0, 5, 10, and 15 cmH2O) [15]. The PU-cuffed tubes demonstrated minor leakage in the absence of PEEP, while PVC-cuffed tubes leaked at all PEEP levels except 15 cmH2O. Lau et al. demonstrated that PU cuffs sealed better than PVC cuffs when PEEP levels were varied, and the ventilator was disconnected [8].
The target Pcuff for HVLP cuffs is 20–30 cmH2O, and all studies used a Pcuff within this range. In clinical practice, however, and in the absence of an automated Pcuff controller, the Pcuff is extremely variable due to some technical conditions (positive pressure ventilation, N2O ventilation, sedation, and neuromuscular blocking agents) [16–18], environmental circumstances (high altitudes, such as during helicopter transport) [19], and patient-related factors (e.g., core temperature, changes in patient positioning) [20–22]. For that reason, with some in vitro experiments, researchers additionally evaluated fluid leakage in case of low (<20 cmH2O) and high (>30 cmH2O) Pcuff [8, 11, 13, 23]. Overall, a higher Pcuff results in better sealing efficacy. Li Bassi et al. controlled for various cuff characteristics by means of multivariate analysis [11]. A greater cuff outer diameter was protective against fluid leakage in multivariate analysis, together with Pcuff and cuff length. Of note, cuff material had no significant impact in multivariate analysis, but it displayed a clear advantage in favor of PU cuffs in univariate analyses.
A caution pertaining to the amount of time allotted to observe leakage past the cuffs is warranted when interpreting the results of the in vitro experiments. The observation periods varied from 20 minutes [23], to 1 h [8, 14, 24, 25], and to 24 h [15, 26, 27]. Although these studies included observation periods that were sufficient to demonstrate significant differences between PU- and PVC-cuffed ETTs, it is critical to recognize that aspiration may occur in patients who are ventilated longer than 24 h. Indeed, exposure time is pivotal in device-associated infections such as VAP [28, 29].
In vivo study
Li Bassi et al. conducted an investigation that included 29 pigs in which 7 different ETTs were tested [26]. Fluid leakage, as indicated by methylene blue or fluorescence microsphere detection, was compared between PU- and PVC-cuffed ETTs residing in five and four pigs, respectively. Leakage of methylene blue was not observed past either cuff type, but the percentage of microspheres per gram of tracheal secretion was lower in animals with PU cuffs than in those with PVC cuffs. The lack of statistically significant differences in leakage between the cuffs may be attributable to the limited number of pigs (i.e., power) that were compared.
Clinical studies
Table 3 summarizes the clinical studies that compare PU- and PVC-cuffed ETTs. Three RCTs were identified that involved 708 patients, comprising 363 patients with PU-cuffed tubes and 345 with PVC-cuffed tubes [14, 30, 31]. The Jadad score indicated two high-quality trials [14, 30] and one trial with higher risk of bias [31] (Additional file 1). Lucangelo et al. measured microaspiration (leakage) of blue dye over 12 h, as evidenced by bronchoscopic evaluation [14]. One hour after PEEP removal, leakage became evident in all patients intubated with PVC-cuffed ETTs, but leakage was not observed in the PU group. However, at the end of the observation period, 17 of 20 patients in the PU group experienced microaspiration. This study demonstrates that, after PEEP is removed, microaspiration is relatively delayed with use of PU-cuffed tubes compared with its onset when ETTs with PVC cuffs are used. The clinical relevance of this observation is particularly pertinent to patients undergoing short-term intubation (e.g., surgical patients).
In the remaining two RCTs, the rate of early postoperative pneumonia and VAP were the respective outcomes of interest. Philippart et al. evaluated the risk of VAP among patients intubated with either PU-cuffed or PVC-cuffed ETTs [31]. The study included four different arms: a cylindrical PU group, a conical PU group, a cylindrical PVC group, and a conical PVC group. No differences in VAP rates were observed among the groups. Despite its multicenter and randomized design, however, that study had limitations. First, the study was not blinded. Second, randomization was not organized on an individual basis. Instead, the investigators predetermined clusters of nine or ten consecutive patients stratified by study centers, with each cluster being assigned to one of the study groups. It was anticipated that inclusion in a single cluster would cover a period of 4–6 weeks for which an appropriate number of ETTs were made available. This approach does not completely rule out bias generated by natural fluctuations in local epidemiology of nosocomial infection (e.g., outbreaks). Third, throughout the study period, Pcuff was controlled by a manual manometer every 6 h. As already mentioned, Pcuff is easily affected by several conditions and can as such be considered an uncontrolled factor potentially affecting the study results.
Two nonrandomized clinical studies with low risk of bias according to the Downs and Black tool [10] were identified (Additional file 1). Nseir et al. prospectively measured pepsin levels in tracheal aspirates to assess microaspiration in 48 patients. Despite the relative small study size, significantly less microaspiration was observed among patients intubated with PU-cuffed tubes. Of note, the observation period was limited to 24 h, thereby suggesting a potential advantage for short-term intubated patients, whereas the clinical benefit for patients with prolonged ventilation remained uncertain. This hypothesis is supported by data reported by Poelaert et al. [30]. In their high-risk cardiac surgical patients, the rate of early postoperative pneumonia was significantly lower among patients intubated with PU-cuffed tubes (23 % vs. 42 %; p = 0.026). In that study, the average periods of intubation and mechanical ventilation were 25 h and 19 h for patients in the PVC cuff and PU cuff groups, respectively (p = 0.22). In a post hoc analysis, Poelaert et al. determined that use of PU-cuffed ETTs in high-risk cardiac surgery patients is protective against early postoperative pneumonia in patients who are intubated for up to 16.6 h [29].
In another non-RCT, Miller et al. evaluated VAP rates in five ICUs during two periods of 1 year (baseline and intervention). In the baseline and intervention periods, respectively, PVC- and PU-cuffed ETTs were used. Thereafter, ICUs used PVC-cuffed ETTs and VAP rates were monitored for a 3-month period. The authors showed a favorable reduction in VAP rates following the introduction of the PU-cuffed ETT; however, nonrandomized studies are prone to bias, such as natural trends in local epidemiology of microbial ecology and nosocomial infection [32]. In addition, a Hawthorne effect cannot be excluded. The Hawthorne effect might have led to improved adherence in universal precautions in infection prevention (e.g., hand hygiene) or in more specific measures to avoid VAP (e.g., oral care), albeit that no changes in infection prevention policy were advocated during the study period.
The potential positive effect of a medical device to prevent microaspiration might be completely eliminated by the failure to control for adequate Pcuff. No cuff seals efficiently in the absence of a sufficiently inflated cuff. At least three RCTs demonstrated that automated Pcuff controllers are effective in keeping Pcuff levels within the target range [33–35]. Therefore, it seems that automated Pcuff control is indispensable, regardless of the cuff material. In addition, the value of automated Pcuff controllers to avoid VAP was demonstrated in a recent meta-analysis [36].
While PU cuffs do not totally succeed in avoiding microaspiration, their advantage might strengthen other features of ETTs to avoid leakage. Lorente et al. reported the results of an RCT in which PU-cuffed tubes with subglottic secretion drainage (SSD) were compared with PVC-cuffed tubes without SSD [37]. The trial demonstrated significantly reduced rates of early and late VAP in the group of patients intubated with the PU-cuffed tube (+SSD).
Limitations and future directions for research
This review has limitations. First, none of the clinical studies addressed safety issues. While there are no particular concerns linked with the use of PU-cuffed tubes, considering long-term safety data may be a point of interest in future studies. Second, the fact that tube characteristics other than cuff material may play a role in sealing efficacy is a limitation of this review. We could take into account neither differences in cuff length nor discreet differences in shape. Regarding the latter, we excluded comparisons of PU vs. PVC cuffs when cuff shapes were tapered and/or conical vs. cylindrical and/or globular in shape, as there are in vitro and clinical data demonstrating improved sealing capacity with taper-shaped cuffs [24, 38]. Finally, among the included studies, there appeared to be substantial differences in study designs, experimental setups, and endpoints. As such, it appeared very difficult to make a pooled estimate of the collected scientific evidence.
More clinical studies on the topic are welcome. RCTs with optimal control for confounding factors should be performed to further assess the value of PU-cuffed ETTs in the prevention of VAP. Special emphasis should be placed on identifying patients who might benefit the most from PU-cuffed ETTs to reduce VAP risk. Concerning early postoperative pneumonia, it may be worthwhile to focus on oncology patients, such as those with esophageal cancer undergoing esophagectomy, as these patients have a particularly high risk for developing postoperative pneumonia [39].
Conclusions
The in vitro, in vivo, and clinical studies reviewed here provide evidence that, compared with PVC-cuffed tubes, PU-cuffed tubes protect more efficiently against microaspiration, or at least postpone substantial leakage of secretions. Indeed, all studies reviewed here that had leakage and/or microaspiration as the primary outcome demonstrated significant results [8, 11, 13–15, 23–25, 27, 40] or at least a tendency toward more efficient sealing [26] in association with PU cuffs. It should be mentioned that only two (single-center) clinical studies assessed microaspiration, including only one RCT. In particular, high-risk patients intubated for shorter periods seemed to benefit from the more effective sealing capacity of PU cuffs, as such patients experienced a lower risk of early postoperative pneumonia [30]. The evidence that PU-cuffed ETTs prevent VAP is less robust, because microaspiration is probably postponed rather than totally eliminated with use of PU cuffs. As such, current evidence can support the use of PU-cuffed ETTs in high-risk surgical patients, while there is currently only very limited evidence that PU cuffs prevent pneumonia in patients ventilated for prolonged periods.
Abbreviations
CDC, Centers for Disease Control and Prevention; cP, centipoise; CPAP, continuous positive airway pressure; ETT, endotracheal tube; GCS, Glasgow Coma Scale; HVLP, high volume, low pressure; ICU, intensive care unit; ID, internal diameter; OD, outer diameter; PaO2/FiO2, ratio of arterial oxygen partial pressure to fractional inspired oxygen; Pcuff, cuff pressure; PEEP, positive end-expiratory pressure; PEP, positive expiratory pressure; PIP, peak inspiratory pressure; PSV, pressure support ventilation; PU, polyurethane; PVC, polyvinyl chloride; RCT, randomized controlled trial; SSD, subglottic secretion drainage; VAP, ventilator-associated pneumonia; VC, volume-controlled; VT, tidal volume
References
Lorente L, Blot S, Rello J. New issues and controversies in the prevention of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2010;182:870–6.
Muscedere JG, Martin CM, Heyland DK. The impact of ventilator-associated pneumonia on the Canadian health care system. J Crit Care. 2008;23:5–10.
Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005;33:2184–93.
Koulenti D, Lisboa T, Brun-Buisson C, Krueger W, Macor A, Solé-Violán J, et al. Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit Care Med. 2009;37:2360–8.
Lambert ML, Palomar M, Agodi A, Hiesmayr M, Lepape A, Ingenbleek A, et al. Prevention of ventilator-associated pneumonia in intensive care units: an international online survey. Antimicrob Resist Infect Control. 2013;2:9.
Blot S, Koulenti D, Dimopoulos G, Martin C, Komnos A, Krueger WA, et al. Prevalence, risk factors, and mortality for ventilator-associated pneumonia in middle-aged, old, and very old critically ill patients. Crit Care Med. 2014;42:601–9.
Blot SI, Poelaert J, Kollef M. How to avoid microaspiration? A key element for the prevention of ventilator-associated pneumonia in intubated ICU patients. BMC Infect Dis. 2014;14:119.
Dullenkopf A, Gerber A, Weiss M. Fluid leakage past tracheal tube cuffs: evaluation of the new Microcuff endotracheal tube. Intensive Care Med. 2003;29:1849–53.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84.
Li Bassi G, Ranzani OT, Martí JD, Giunta V, Luque N, Isetta V, et al. An in vitro study to assess determinant features associated with fluid sealing in the design of endotracheal tube cuffs and exerted tracheal pressures. Crit Care Med. 2013;41:518–26.
Manzano F, Fernández-Mondejar E, Colmenero M, Poyatos ME, Rivera R, Machado J, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med. 2008;36:2225–31.
Dave MH, Frotzler A, Weiss M. Closed tracheal suction and fluid aspiration past the tracheal tube. Impact of tube cuff and airway pressure. Minerva Anestesiol. 2011;77:166–71.
Lucangelo U, Zin WA, Antonaglia V, Petrucci L, Viviani M, Buscema G, et al. Effect of positive expiratory pressure and type of tracheal cuff on the incidence of aspiration in mechanically ventilated patients in an intensive care unit. Crit Care Med. 2008;36:409–13.
Zanella A, Scaravilli V, Isgrò S, Milan M, Cressoni M, Patroniti N, et al. Fluid leakage across tracheal tube cuff, effect of different cuff material, shape, and positive expiratory pressure: a bench-top study. Intensive Care Med. 2011;37:343–7.
Guyton D, Banner MJ, Kirby RR. High-volume, low-pressure cuffs: are they always low pressure? Chest. 1991;100:1076–81.
Mehta S, Myat HM. The cross-sectional shape and circumference of the human trachea. Ann R Coll Surg Engl. 1984;66:356–8.
Tu HN, Saidi N, Lieutaud T, Bensaid S, Menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg. 1999;89:187–90.
Bassi M, Zuercher M, Erne JJ, Ummenhofer W. Endotracheal tube intracuff pressure during helicopter transport. Ann Emerg Med. 2010;56:89–93.
Lizy C, Swinnen W, Labeau S, Poelaert J, Vogelaers D, Vandewoude K, et al. Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. Am J Crit Care. 2014;23:e1–8.
Inada T, Kawachi S, Kuroda M. Tracheal tube cuff pressure during cardiac surgery using cardiopulmonary bypass. Br J Anaesth. 1995;74:283–6.
Sole ML, Penoyer DA, Su X, Jimenez E, Kalita SJ, Poalillo E, et al. Assessment of endotracheal cuff pressure by continuous monitoring: a pilot study. Am J Crit Care. 2009;18:133–43.
Lau ACW, Lam SM, Yan WW. Benchtop study of leakages across the Portex, TaperGuard, and Microcuff endotracheal tubes under simulated clinical conditions. Hong Kong Med J. 2014;20:7–15.
Dave MH, Frotzler A, Spielmann N, Madjdpour C, Weiss M. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth. 2010;105:538–43.
Ouanes I, Lyazidi A, Danin PE, Rana N, Di Bari A, Abroug F, et al. Mechanical influences on fluid leakage past the tracheal tube cuff in a benchtop model. Intensive Care Med. 2011;37:695–700.
Li Bassi G, Luque N, Martí JD, Aguilera Xiol E, Di Pasquale M, Giunta V, et al. Endotracheal tubes for critically ill patients: an in vivo analysis of associated tracheal injury, mucociliary clearance, and sealing efficacy. Chest. 2015;147:1327–35.
Kolobow T, Cressoni M, Epp M, Corti I, Cadringher P, Zanella A. Comparison of a novel Lycra endotracheal tube cuff to standard polyvinyl chloride cuff and polyurethane cuff for fluid leak prevention. Respir Care. 2011;56:1095–9.
Myny D, Depuydt P, Colardyn F, Blot S. Ventilator-associated pneumonia in a tertiary care ICU: analysis of risk factors for acquisition and mortality. Acta Clin Belg. 2005;60:114–21.
Poelaert J, Haentjens P, Blot S. Association among duration of mechanical ventilation, cuff material of endotracheal tube, and postoperative nosocomial pneumonia in cardiac surgical patients: a prospective study. J Thorac Cardiovasc Surg. 2014;148:1622–7.
Poelaert J, Depuydt P, De Wolf A, Van de Velde S, Herck I, Blot S. Polyurethane cuffed endotracheal tubes to prevent early postoperative pneumonia after cardiac surgery: a pilot study. J Thorac Cardiovasc Surg. 2008;135:771–6.
Philippart F, Gaudry S, Quinquis L, Lau N, Ouanes I, Touati S, et al. Randomized intubation with polyurethane or conical cuffs to prevent pneumonia in ventilated patients. Am J Respir Crit Care Med. 2015;191:637–45.
Miller MA, Arndt JL, Konkle MA, Chenoweth CE, Iwashyna TJ, Flaherty KR, et al. A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia. J Crit Care. 2011;26:280–6.
Valencia M, Ferrer M, Farre R, Navajas D, Badia JR, Nicolas JM, et al. Automatic control of tracheal tube cuff pressure in ventilated patients in semirecumbent position: a randomized trial. Crit Care Med. 2007;35:1543–9.
Nseir S, Zerimech F, Fournier C, Lubret R, Ramon P, Durocher A, et al. Continuous control of tracheal cuff pressure and microaspiration of gastric contents in critically ill patients. Am J Respir Crit Care Med. 2011;184:1041–7.
Lorente L, Lecuona M, Jiménez A, Lorenzo L, Roca I, Cabrera J, et al. Continuous endotracheal tube cuff pressure control system protects against ventilator-associated pneumonia. Crit Care. 2014;18:R77.
Nseir S, Lorente L, Ferrer M, Rouzé A, Gonzalez O, Bassi GL, et al. Continuous control of tracheal cuff pressure for VAP prevention: a collaborative meta-analysis of individual participant data. Ann Intensive Care. 2015;5:43.
Lorente L, Lecuona M, Jiménez A, Mora ML, Sierra A. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia. Am J Respir Crit Care Med. 2007;176:1079–83.
D’Haese J, De Keukeleire T, Remory I, Van Rompaey K, Umbrain V, Poelaert J. Assessment of intraoperative microaspiration: does a modified cuff shape improve sealing? Acta Anaesthesiol Scand. 2013;57:873–80.
Akutsu Y, Matsubara H, Shuto K, Shiratori T, Uesato M, Miyazawa Y, et al. Pre-operative dental brushing can reduce the risk of postoperative pneumonia in esophageal cancer patients. Surgery. 2010;147:497–502.
Nseir S, Zerimech F, De Jonckheere J, Alves I, Balduyck M, Durocher A. Impact of polyurethane on variations in tracheal cuff pressure in critically ill patients: a prospective observational study. Intensive Care Med. 2010;36:1156–63.
Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903.
Authors’ contributions
SIB contributed to study conception and design, the literature search, interpretation of the available literature data, and manuscript preparation. JR contributed to interpretation of the available literature and critical revision of the manuscript. DK contributed to the literature search, interpretation of the literature data, and manuscript preparation. All authors read and approved the final manuscript.
Competing interests
SIB holds a research mandate at Ghent University. This study was supported by an unrestricted grant from Halyard Health, Inc. (Alpharetta, GA, USA). The funding source had no involvement in the design of the review and did not have any role during its execution, analyses, interpretation of data, or the decision to submit the results for publication. The other authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Online Supplementary Material 1. Risk of bias assessment of randomized clinical trials using the Jadad quality scale. Online Supplementary Material 2. Risk of bias assessment of non-randomized clinical studies (Downs and Black tool [10]). (DOCX 82 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Blot, S.I., Rello, J. & Koulenti, D. The value of polyurethane-cuffed endotracheal tubes to reduce microaspiration and intubation-related pneumonia: a systematic review of laboratory and clinical studies. Crit Care 20, 203 (2016). https://doi.org/10.1186/s13054-016-1380-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-016-1380-8