Abstract
Introduction
Serum lactate level may correlate with no-flow and low-flow status during cardiac arrest. Current guidelines have no recommended durations for cardiopulmonary resuscitation (CPR) before transition to the next strategy. We hypothesized that the lactate level measured during CPR could be associated with the survival probability and accordingly be useful in estimating the optimal duration for CPR.
Methods
We conducted a retrospective observational study in a single medical centre and included adult patients who had suffered an in-hospital cardiac arrest between 2006 and 2012. We used multivariable logistic regression analysis to study the association of lactate level measured during CPR and outcomes. We used generalized additive models to examine the nonlinear effects of continuous variables and conditional effect plots to visualize the estimated survival probability against CPR duration.
Results
Of the 340 patients included in our analysis, 50 patients (14.7 %) survived to hospital discharge. The mean lactate level was 9.6 mmol/L and mean CPR duration was 28.8 min. There was an inverse near-linear relationship between lactate level and probability of survival to hospital discharge. A serum lactate level <9 mmol/L was positively associated with patient survival to hospital discharge (odds ratio 2.00, 95 % confidence interval 1.01-4.06). The optimal CPR duration may not be a fixed value but depend on other conditions.
Conclusions
Serum lactate level measured during CPR could correlate with survival outcomes. A lactate level threshold of 9 mmol/L may be used as a reference value to identify patients with different survival probabilities and determine the optimal CPR durations.
Similar content being viewed by others
Introduction
More than 200,000 hospitalized adult patients experience in-hospital cardiac arrest (IHCA) annually in the USA with an estimated incidence of 1.6 per 1,000 hospital admissions [1]. The survival rate from IHCA has increased over the past decade [2], probably due to earlier recognition of cardiac arrest, higher quality of cardiopulmonary resuscitation (CPR), and improved post-resuscitation care [3, 4]. Despite this progress, mortality following IHCA remains high, with only about 18 % of patients surviving to hospital discharge [1].
The causes of high mortality could be due to the inability to establish rapid return of spontaneous circulation (ROSC) leading to subsequent multi-organ failure. Extracorporeal CPR (ECPR) has been advocated as a novel alternative for cardiac arrests that are considered refractory to initial conventional CPR [5, 6], especially for IHCA [7]. Nevertheless, the term, “refractory cardiac arrest,” is ill-defined. Most studies on ECPR have used CPR duration as an indicator of futile resuscitation, which varied from 10 to 15 minutes [7–9] and led to initiation of ECPR within 30 to 60 minutes of CPR.
However, using CPR duration alone may not be an accurate indicator for estimating survival probability and determination of futile CPR. Matos et al. [10] reported that even in the case of equivalent CPR durations, the survival probability still differed greatly between different patient groups. Although studies have suggested that the greater the time prior to initiation of ECPR, the poorer the outcome [7], few studies have been carried out on the optimal transition time to consider alternative resuscitation methods in patients with potentially prolonged CPR. Therefore, finding additional parameters besides CPR duration to assist clinicians in more accurately estimating the survival probability during CPR could help strike a balance between optimizing patient outcomes and avoiding the misuse of scarce critical care medical resources, such as ECPR.
Weil et al. [11] found that serum lactate level measured within 10 minutes of CPR could serve as a sensitive indicator of prognosis. A higher post-ROSC serum lactate level [12–16] or a slower clearance rate of serum lactate after ROSC [12, 17, 18] has also been shown to correlate with poor outcomes after cardiac arrest. We therefore hypothesized that the serum lactate level measured during CPR may be associated with the survival probability and accordingly be useful in estimating the optimal CPR duration before transition to the next strategy for IHCA.
Methods
Setting
We carried out a retrospective cohort study in a tertiary medical centre, National Taiwan University Hospital (NTUH). Before data collection, the Research Ethics Committee of the National Taiwan University Hospital approved this study (reference number: 201505161RIN) and waived the requirement for written informed consent. The NTUH has 2,600 beds, including 220 beds in intensive care units (ICUs). According to hospital policy, a code team is activated when cardiac arrest events occur in the general wards. Each code team member has been certified to provide advanced cardiac life support. For cardiac arrest events in the ICUs, resuscitation is performed by the staff of the ICU where the cardiac arrest events have occurred and by staff from neighbouring ICUs.
Participants
We included patients who had experienced an IHCA at the NTUH between 2006 and 2012. We used the following inclusion criteria: (1) age ≥18 years; (2) documented absence of pulse with performance of chest compression for ≥2 minutes; (3) without do-not-resuscitate order; and (4) serum lactate level measured during the initial 10 minutes of CPR. If multiple cardiac arrest events occurred in a single patient, we only recorded the first event of the same hospitalization. We excluded patients who had suffered a cardiac arrest related to major trauma.
Data collection and outcome measures
We recorded the following information for each patient: demographics, comorbidities, variables derived from the Utstein template [19], the first serum lactate level measured during CPR, and any critical intervention that was implemented. CPR duration was defined as the time from the first chest compression provided by the code team or ICU members to the termination of resuscitation efforts, either due to ROSC or declaration of death. The definitions of comorbidities are appended in Additional file 1: Table S1.
The primary outcome was survival to hospital discharge. Secondary outcomes included 10-minute ROSC, defined as ROSC within 10 minutes of CPR, and favourable neurological status at hospital discharge, defined as a score of 1 or 2 on the cerebral performance category (CPC) scale [20]. The CPC score was retrospectively determined by reviewing medical records for each patient.
Statistical analysis
We used R 2.15.3 software (R Foundation for Statistical Computing, Vienna, Austria) for data analysis. Categorical data were expressed as counts and proportions; continuous data were expressed as means and standard deviations. Categorical variables were compared by the Fisher’s exact test, and continuous variables were examined by the Wilcoxon rank-sum test. A two-tailed p value of ≤0.05 was considered statistically significant.
We selected the odds ratio as the outcome measure. We conducted a multivariable logistic regression analysis to examine the association between independent variables and outcomes. All available variables were considered in the regression model, regardless of whether they were significant by univariate analysis. The stepwise variable selection procedure (with iterations between the forward and backward steps) was applied to obtain the final regression model. Significance levels for entry and for stay were set at 0.15 to avoid exclusion of potential candidate variables. The final regression model was identified by excluding individual variables with a p value >0.05, until all regression coefficients were statistically significant. If the lactate level was excluded during the variable selection procedure, we would re-enter it into the final model to obtain the effect estimate.
We used generalized additive models (GAMs) [21] to examine the nonlinear effects of continuous variables and, if necessary, to identify the appropriate cutoff point(s) for dichotomizing a continuous variable during the variable selection procedure. We used conditional effect plots to visualize the predicted probability of survival to hospital discharge against CPR duration, while maintaining the other independent variables in the final model constant. Based on the conditional effect plot, we used CPR duration of 30 minutes and probability of survival of 18 % [1] as reference to calculate the corresponding probabilities of survival and CPR duration, respectively, for each group of patients.
We assessed the goodness-of-fit of the fitted regression model using c statistics (the estimated area under the receiver operating characteristic curve), adjusted generalized R 2, and the Hosmer-Lemeshow goodness-of-fit test.
Results
A total of 1,123 adult patients received chest compression ≥2 minutes in the period between 2006 and 2012. Of these, only 349 patients had concomitant measurements of serum lactate level during the initial 10 minutes of CPR. Nine patients were excluded due to trauma-related cardiac arrest. The remaining 340 patients were included for further analysis.
The characteristics of the patients included in this study, stratified by primary outcome, are outlined in Tables 1 and 2. The mean age of the patients was 65.9 years. A total of 151 cardiac arrest events (44 %) occurred in the ICUs and 171 cardiac arrest events (50 %) occurred in the general wards. Shockable rhythms represented 14 % of initial arrest rhythms. The mean lactate level was 9.6 mmol/L and the mean CPR duration was 28.8 minutes. Both lactate levels and CPR durations were significantly different between survivors and non-survivors. There were 242 patients (71 %) who achieved ROSC and 76 of these patients (22 %) achieved a 10-minute ROSC. Only 50 patients (15 %) survived to hospital discharge and 21 of these patients (6 %) displayed a favourable neurological status.
All variables listed in Tables 1 and 2 were included in the variable selection procedure for the primary outcome. The GAM plot revealed a near-linear association between logit (p), where p represented the probability for survival to hospital discharge, and lactate level (Additional file 2: Figure S1). If logit (p) was ≥0, the odds for survival would be ≥1. Therefore, 9 mmol/L of lactate was selected as the cutoff point to transform the lactate level into a binary variable. The characteristics and outcomes of patients in this study, stratified by lactate level, are reported in Additional file 3: Table S2, Additional file 4: Table S3, and in Table 3.
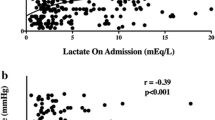
The final regression model is shown in Table 4. Shockable rhythm/lactate level <9 mmol/L was positively associated with survival to hospital discharge, and hepatic insufficiency/CPR duration was inversely associated with survival to hospital discharge. The association between CPR duration and estimated survival probability for different patient groups is illustrated in Fig. 1. With reference to Fig. 1, we calculated the survival probability when CPR was performed for 30 minutes for each patient group. We also calculated the CPR duration when survival probability dropped to 18 % or when survival probability was half the initial probability (Table 5).
For secondary outcomes, a lactate level <9 mmol/L was positively associated with a 10-minute ROSC but not significantly associated with neurological outcome (Additional file 5: Table S4).
Discussion
In this retrospective observational study, results have indicated that the serum lactate level measured during CPR correlated with the outcome of survival to hospital discharge for IHCA. A serum lactate level <9 mmol/L within 10 minutes of CPR initiation was positively associated with survival. Moreover, together with other variables, the serum lactate level could be useful in estimating optimal CPR durations before transition to next strategy for different patient groups, which could help clinicians create further resuscitation strategies in addition to the initial conventional CPR.
Excess production of lactate has been reported to be largely due to tissue hypoxia or hypoperfusion with associated anaerobic metabolism [22]. For the past few decades, it has been noted that the blood lactate level might correlate with the duration of no-flow and low-flow status during CPR [23, 24], both of which are known to impact outcomes after cardiac arrest [25]. This biomarker is therefore a promising candidate for a prognostic predictor of CPR. Weil et al. [11] suggested that the lactate level measured within 10 minutes of CPR could be associated with survival outcomes despite the fact that other important confounders were not considered during their analysis. In subsequent investigations, lower serum lactate measurements or early and effective serum lactate clearance was also shown to correlate with decreased mortality in cardiac arrest patients [12–18]. These studies [12–18] all used post-ROSC lactate level for analysis.
In line with previous studies [11–18], we revealed that the serum lactate level measured during CPR was significantly associated with survival outcomes after adjusting for the confounding effects of multiple factors. There was a near-linear inverse association between the lactate level and the probability of survival. Furthermore, a lactate level <9 mmol/L was significantly associated with higher survival probabilities. This cutoff point was higher than those reported in previous studies [15, 16]. Seeger et al. [15] reported that a lactate level >6.94 mmol/L was associated with poor neurological outcomes; Kaji et al. [16] reported that a lactate level <5 mmol/L correlated with a favourable neurological outcome. The difference in threshold values could be explained by the different time points of lactate measurement and outcome selection. Compared to measurements after ROSC [15, 16], in which blood flow had already recovered to ameliorate systemic hypoxia and hypoperfusion, it seems reasonable that lactate levels would be higher when measured during ongoing CPR.
However, the causes of elevated serum lactate do merit further explanation. Firstly, the serum lactate level could indeed be a surrogate marker for duration of no-flow and low-flow status after cardiac arrest [23, 24]. Nevertheless, Müllner et al. also suggested that the lactate level may be just a weak measure of the duration of cardiac arrest [26]. For IHCA patients, various conditions, such as severe septic shock, could also produce similarly high lactate levels even without cardiac arrest. The use of adrenaline had also been shown to increase the serum lactate level [27]. Secondly, the serum lactate level reflected the difference between lactate production and elimination; thus, an increased lactate level may also indicate mechanisms other than cellular hypoxia or hypoperfusion. For example, impaired liver function could lead to reduced lactate elimination and an elevated lactate level, even when the hemodynamic status was not compromised [28, 29]. Despite these considerations, by adjusting the effects of multiple confounders, including hepatic insufficiency, we believe that the serum lactate level measured during CPR, with its complex physiologic and pathologic implications, could still serve as a useful prognostic factor for outcomes.
There are currently no recommendations for optimal CPR duration before transition to the next strategy [3, 4]. In clinical practice, patients usually received a predetermined duration of CPR, often 30 minutes, even if the patients had not exhibited any response to the repeated resuscitation efforts. However, for adult IHCA patients, Goldberger et al. showed that patients would have a higher probability of survival if they were resuscitated at hospitals that tended to implement longer CPR durations [30]. Furthermore, Matos et al. [10] demonstrated that outcomes after paediatric IHCA could differ significantly between different patient groups, indicating that surgical cardiac patients had the highest probability of a good outcome and trauma patients had the lowest probability, and that CPR >20 minutes may not be futile in certain patient groups. Conversely, Kim et al. [31] recommended that ECPR should be considered for adult patients with out-of-hospital cardiac arrest (OHCA) when CPR was ≥21 minutes. In addition, in an adult OHCA study, Reynolds et al. [32] revealed that the probability of favourable outcomes declined rapidly with each minute of CPR and most surviving patients (89.7 %) with favourable neurological outcomes would achieve ROSC within 16.1 minutes of CPR. Therefore, Reynolds et al. [32] suggested that novel therapeutics, such as ECPR, should be considered early after CPR rather than after the complete failure of resuscitation. This could also hold true for IHCA patients especially for whom applications of ECPR were more available and mature [7].
Using CPR duration alone to define futile resuscitation may risk delaying timely implementation of ECPR and missing opportunities to improve patient outcomes. However, the classification method of patient groups used by Matos et al. [10] was somewhat difficult to be generalized and applied in clinical practice. In our current study, in addition to serum lactate level and CPR duration, we also noted that shockable rhythm and hepatic insufficiency were also significantly associated with survival outcomes, both of which have also been reported in previous studies [33, 34]. Based on these variables, we were able to divide patients into groups with different survival probabilities (Fig. 1). In this way, clinicians may be more prepared for determining the optimal CPR duration for each patient group before transition to the next strategy, either a more advanced strategy, such as ECPR, or termination of CPR.
For example, if we choose the average IHCA survival rate 18 % as a reference [1, 2], we would note that the maximally allowed CPR duration was 32.3 minutes for patient group 1 before the survival probability dropped below 18 %; however, for patient groups 7 and 8, the survival probability would be far below 18 % even from the start of CPR (Table 5). From another perspective, if we choose the commonly used CPR duration of 30 minutes, we could note that even if the CPR intervals were the same, there would be a 10-fold difference in the probability of survival between patient groups 1 (23 %) and 8 (2 %) (Table 5). Therefore, it is clear that if clinicians depended solely on CPR duration to define futile resuscitation, it may be premature to give up for some patients and delayed to activate alternative resuscitation measures for other patients. However, because of the limited number of patients in our analysis, the estimations for CPR duration and survival probability can only serve for the purpose of explanation rather than precise estimations.
A lactate level <9 mmol/L was also significantly associated with a 10-minute ROSC. This CPR interval has been used as one of prerequisites prior to activation of ECPR [7] and termination of IHCA CPR [35, 36]. We suggest that for IHCA patients with a lactate level higher than 9 mmol/L and without exclusion criteria for ECPR, the ECPR team should probably be alerted earlier in order to be able to initiate the ECPR sooner to improve outcomes, as these patients were shown to have less chance of achieving rapid ROSC. Conversely, the clinical decision to terminate IHCA was based solely on witness status, initial arrest rhythm and CPR duration [35, 36]. Using serum lactate level as an additional variable could probably increase the accuracy of this decision and avoid lengthening the dying process of critical patients.
Post-ROSC serum lactate level or the clearance rate of serum lactate has been associated with neurological outcomes [12, 14, 16, 17]. An elevated lactate level may represent a more severe status of tissue hypoperfusion and ischaemia-reperfusion injury, which might aggravate the cerebral dysfunction in post-cardiac arrest syndrome [37]. As there were only 21 patients (6.2 %) in our cohort who regained a favourable neurological outcome, the statistical power may be insufficient to detect the difference between patients with and without a favourable neurological outcome. Nonetheless, the trend of the point estimate of lactate level (odds ratio 1.86) supports our hypothesis. Future studies with more patients would be expected to clarify this issue.
In summary, we found that the serum lactate level measured during CPR was associated with survival outcomes. Along with other variables, the lactate level could help separate patients into several groups with different levels of survival probability. With a predetermined survival probability, clinicians may be able to determine the optimal CPR duration for each group. However, in our current study, we were not aiming to obtain and recommend a fixed CPR duration for each patient group as this was dependent on individual patients. We also did not intend to analyse which strategies should be undertaken following implementation of this optimal CPR duration. What we did emphasize, however, was that the CPR duration alone should not be used for decision-making in CPR. The optimal resuscitation strategy should be personalised and be adjusted to the specific context, taking into account the autonomy of patients, wishes of family members, or the availability of ECPR and other resources of critical care.
Study limitations
First, this was an observational study, which could only establish an association rather than a causal relationship between independent and dependent variables. Second, the quality of CPR could not be retrospectively determined. Currently, there were no studies indicating that the serum lactate level measured during CPR could reflect the quality of CPR. The association between serum lactate level and quality of CPR should be further examined in a prospective method. Third, we could not be sure whether the serum lactate was from arterial or venous samples. Ralston et al. [23] reported that there was no significant difference in lactate levels between arterial and venous samples during animal CPR. Therefore, this issue may not bias our results to a significant extent. Fourth, the proportion of patients receiving therapeutic hypothermia was low in our cohort. The influence of therapeutic hypothermia on the association between lactate levels and CPR outcomes might be left for future researchers to investigate. Fifth, we used survival to hospital discharge as the primary outcome because the number in the studied cohort was small. Nonetheless, neurologically intact survival might be a more important and meaningful long-term outcome and should be explored as the primary outcome in future research with larger patient populations. Finally, we used IHCA patients for analysis, and so the results might not be applicaple to OHCA patients. In addition, the current analysis was a retrospective study in a single centre with a highly selective cohort, so the probability for selection bias might be high. The lactate levels measured during the initial 10 minutes of CPR were only available in 30 % (340/1123) of the total IHCA patients. Most of the lactate values were reported simultaneously with measurements of blood gases or potassium by point-of-care machines. As resuscitation guidelines [3, 4] do not suggest the measurement of lactate level during CPR, only a prospective study could avoid this kind of selection bias.
Conclusions
The serum lactate level measured during CPR may correlate with survival outcomes. A 9-mmol/L lactate level could probably be used as a reference value to identify patients with different survival probabilities and to determine the optimal duration of CPR.
Key messages
-
The serum lactate level measured during CPR may correlate with survival outcomes
-
A 9-mmol/L lactate level could probably be used as a reference value to identify patients with different survival probabilities and to determine the optimal CPR durations
Abbreviations
- CPC:
-
cerebral performance category
- CPR:
-
cardiopulmonary resuscitation
- ECPR:
-
extracorporeal cardiopulmonary resuscitation
- GAM:
-
generalized additive model
- ICU:
-
intensive care unit
- IHCA:
-
in-hospital cardiac arrest
- NTUH:
-
National Taiwan University Hospital
- OHCA:
-
out-of-hospital cardiac arrest
- ROSC:
-
rapid return of spontaneous circulation
References
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322.
Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–20.
Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640–56.
Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219–76.
Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S676–84.
Cave DM, Gazmuri RJ, Otto CW, Nadkarni VM, Cheng A, Brooks SC, et al. Part 7: CPR techniques and devices: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S720–8.
Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372:554–61.
Fagnoul D, Combes A, De Backer D. Extracorporeal cardiopulmonary resuscitation. Curr Opin Crit Care. 2014;20:259–65.
Conseil français de réanimation cardiopulmonaire; Société française d'anesthésie et de réanimation; Société française de cardiologie; Société française de chirurgie thoracique et cardiovasculaire; Société française de médecine d'urgence; Société française de pédiatrie, et al. Guidelines for indications for the use of extracorporeal life support in refractory cardiac arrest. French Ministry of Health. Ann Fr Anesth Reanim. 2009;28:182–90.
Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127:442–51.
Weil MH, Ruiz CE, Michaels S, Rackow EC. Acid–base determinants of survival after cardiopulmonary resuscitation. Crit Care Med. 1985;13:888–92.
Donnino MW, Andersen LW, Giberson T, Gaieski DF, Abella BS, Peberdy MA, et al. Initial lactate and lactate change in post-cardiac arrest: a multicenter validation study. Crit Care Med. 2014;42:1804–11.
Starodub R, Abella BS, Grossestreuer AV, Shofer FS, Perman SM, Leary M, et al. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation. 2013;84:1078–82.
Kliegel A, Losert H, Sterz F, Holzer M, Zeiner A, Havel C, et al. Serial lactate determinations for prediction of outcome after cardiac arrest. Medicine (Baltimore). 2004;83:274–9.
Seeger FH, Toenne M, Lehmann R, Ehrlich JR. Simplistic approach to prognosis after cardiopulmonary resuscitation-value of pH and lactate. J Crit Care. 2013;28:317. e13-20.
Kaji AH, Hanif AM, Bosson N, Ostermayer D, Niemann JT. Predictors of neurologic outcome in patients resuscitated from out-of-hospital cardiac arrest using classification and regression tree analysis. Am J Cardiol. 2014;114:1024–8.
Lee TR, Kang MJ, Cha WC, Shin TG, Sim MS, Jo IJ, et al. Better lactate clearance associated with good neurologic outcome in survivors who treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Crit Care. 2013;17:R260.
Donnino MW, Miller J, Goyal N, Loomba M, Sankey SS, Dolcourt B, et al. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation. 2007;75:229–34.
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–97.
Becker LB, Aufderheide TP, Geocadin RG, Callaway CW, Lazar RM, Donnino MW, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation. 2011;124:2158–77.
Hastie TJ, Tibshirani RJ. Generalized Additive Models. 1st ed. London and New York: Chapman & Hall; 1990.
Bernardin G, Pradier C, Tiger F, Deloffre P, Mattei M. Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensive Care Med. 1996;22:17–25.
Ralston SH, Voorhees WD, Showen L, Schmitz P, Kougias C, Tacker WA. Venous and arterial blood gases during and after cardiopulmonary resuscitation in dogs. Am J Emerg Med. 1985;3:132–6.
Carden DL, Martin GB, Nowak RM, Foreback CC, Tomlanovich MC. Lactic acidosis during closed-chest CPR in dogs. Ann Emerg Med. 1987;16:1317–20.
Adrie C, Cariou A, Mourvillier B, Laurent I, Dabbane H, Hantala F, et al. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J. 2006;27:2840–5.
Müllner M, Sterz F, Domanovits H, Behringer W, Binder M, Laggner AN. The association between blood lactate concentration on admission, duration of cardiac arrest, and functional neurological recovery in patients resuscitated from ventricular fibrillation. Intensive Care Med. 1997;23:1138–43.
Grip J, Jakobsson T, Hebert C, Klaude M, Sandström G, Wernerman J, et al. Lactate kinetics and mitochondrial respiration in skeletal muscle of healthy humans under influence of adrenaline. Clin Sci (Lond). 2015;129:375–84.
Jeppesen JB, Mortensen C, Bendtsen F, Møller S. Lactate metabolism in chronic liver disease. Scand J Clin Lab Invest. 2013;73:293–9.
De Jonghe B, Cheval C, Misset B, Timsit JF, Garrouste M, Montuclard L, et al. Relationship between blood lactate and early hepatic dysfunction in acute circulatory failure. J Crit Care. 1999;14:7–11.
Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–81.
Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. 2014;18:535.
Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128:2488–94.
Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, et al. A validated prediction tool for initial survivors of in-hospital cardiac arrest. Arch Intern Med. 2012;172:947–53.
Ebell MH, Jang W, Shen Y, Geocadin RG, Get With the Guidelines–Resuscitation Investigators. Development and validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med. 2013;173:1872–8.
van Walraven C, Forster AJ, Stiell IG. Derivation of a clinical decision rule for the discontinuation of in-hospital cardiac arrest resuscitations. Arch Intern Med. 1999;159:129–34.
van Walraven C, Forster AJ, Parish DC, Dane FC, Chandra KM, Durham MD, et al. Validation of a clinical decision aid to discontinue in-hospital cardiac arrest resuscitations. JAMA. 2001;285:1602–6.
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation. 2008;79:350–79.
Acknowledgements
We thank Centre of Quality Management of National Taiwan University Hospital for providing the list of patients sustaining in-hospital cardiac arrest. This study was funded by the academic research grant NTUHYL.104.S010 from the National Taiwan University Hospital Yunlin Branch, which was not involved in the study design, in the collection, analysis or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare no conflicts of interest or sources of funding for this study.
Authors’ contributions
CHW, CHH, WTC and WJC conceived the study and designed the study protocol. MST and PHY participated in the acquisition of data. CHW, YWW and KYH conducted the analysis and interpretation of data. CHW drafted the manuscript in conjunction with the other authors. WJC was responsible for the critical revision. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and approved the final version of the manuscript.
Authors’ information
The corresponding author had full access to all data and final responsibility to submit the results for publication.
Additional files
Additional file 1: Table S1.
Definitions of comorbidities used in the multivariable models. (DOCX 21 kb)
Additional file 2: Figure S1.
Generalized additive model plot for non-parametric modelling of the effect of serum lactate level on the logit of probability for survival to hospital discharge. (TIFF 23 kb)
Additional file 3: Table S2.
Baseline characteristics of study patients stratified by lactate level. (DOCX 17 kb)
Additional file 4: Table S3.
Features of cardiac arrest events stratified by lactate level. (DOCX 18 kb)
Additional file 5: Table S4.
Multiple logistic regression model with secondary outcomes as the dependent variable. (DOCX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, CH., Huang, CH., Chang, WT. et al. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit Care 19, 344 (2015). https://doi.org/10.1186/s13054-015-1058-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-015-1058-7