Abstract
Introduction
Knowledge of the genetic mechanisms driving hereditary breast and ovarian cancer (HBOC) has recently expanded due to advances in gene sequencing technologies. Genetic testing for HBOC risk now involves multi-gene panel testing, which includes well characterized high-penetrance genes (e.g. BRCA1 and BRCA2), as well as moderate- and low-penetrance genes. Certain moderate and low penetrance genes are associated with limited data to inform cancer risk estimates and clinical management recommendations, which create new sources of genetic and clinical uncertainty for patients.
Purpose
The aim of this review is to evaluate the psychological and health behaviour outcomes associated with multi-gene panel testing for HBOC risk. The search was developed in collaboration with an Information Specialist (Princess Margaret Cancer Centre) and conducted in the following databases: MEDLINE, EMBASE, EMCare, PsycINFO, Epub Ahead of Publication.
Results
Similar to the BRCA1/2 literature, individuals with a pathogenic variant (PV) reported higher levels of testing-related concerns and cancer-specific distress, as well as higher uptake of prophylactic surgery in both affected and unaffected individuals compared to those with variant of uncertain significance (VUS) or negative result. A single study demonstrated that individuals with a PV in a moderate penetrance gene reported higher rates of cancer worry, genetic testing concerns and cancer-related distress when compared to women with high penetrance PV. Analysis of cancer screening and prevention outcomes based upon gene penetrance were limited to two studies, with conflicting findings.
Conclusion
The findings in this review emphasize the need for studies examining psychological and health behavior outcomes associated with panel testing to include between group differences based upon both variant pathogenicity and gene penetrance. Future studies evaluating the impact of gene penetrance on patient-reported and clinical outcomes will require large samples to be powered for these analyses given that a limited number of tested individuals are found to have a PV.
Similar content being viewed by others
Introduction
Knowledge of the genetic mechanisms driving hereditary breast and ovarian cancer (HBOC) has recently expanded due to advances in gene sequencing technologies. BRCA1 and BRCA2 (BRCA1/2) account for only 20–30% of HBOC cases [1, 2], leading to the identification of other genes implicated in this hereditary syndrome. As a result, cancer genetic testing has shifted away from sequentially screening high-risk individuals for a limited number of well-characterized genes towards adopting multi-gene panel testing [3].
Currently, the clinical utility and validity of panel testing remains limited due to the minimal and often variable data informing age-specific risk estimates associated with several moderate-penetrance (MP) gene mutations [3,4,5,6,7]. There are few guidelines regarding the medical management of individuals harboring mutations in MP genes [3, 5, 8]. Panel testing also increases the likelihood of identifying variants of uncertain clinical significance (VUS), as well as variants where the clinical implications extend beyond the indication for testing. Multi-gene panel testing introduces new sources of clinical uncertainty, which may create challenging cancer screening and prevention decisions for patients and practitioners [3, 5, 9].
Initial studies examining patient outcomes with panel testing for hereditary cancer risk focused on exploring patient understanding and preferences [3]. These studies suggest that although patients are highly motivated to pursue testing, gaps in patient understanding exist and preferences surrounding return of results are variable [10,11,12]. These findings have raised concerns about the specific informational and support-based needs of individuals undergoing panel testing and identified challenges to traditional genetic counselling approaches [3, 13, 14].
Research examining the psychological impact and health behaviors of patients undergoing germline BRCA1/2 testing described a cognitive process that follows result disclosure, where tested individuals must interpret their own cancer genetic risk in the context of their personal and/or familial cancer history [15]. The literature suggests that the type of genetic test result influences an individual’s risk perception [16,17,18]. Uncertain genetic risk associated with uninformative test results can negatively influence one’s cancer risk perceptions, psychological functioning, and uptake of cancer screening and prevention options [15, 19]. Extrapolating from the BRCA1/2 literature highlights how the new sources of complexity and uncertainty associated with multi-gene panel testing may impact how patients respond to panel-based testing and underscores the need for research to be focused in this area. The aim of this review is to evaluate the psychological and health behaviour outcomes associated with multi-gene panel testing for HBOC risk.
Methods
Search strategy
The search strategy was developed in consultation with an Information Specialist at the University Health Network Library (Toronto, ON), who has expertise in conducting literature reviews, with a specialization in oncology. The following research questions guided this review: (i) How does multi-gene panel testing for HBOC risk impact the level of psychological distress of tested individuals? (ii) How does multi-gene panel testing for HBOC risk inform the cancer screening and prevention decisions of tested individuals? and (iii) Does the type of test result influence one’s psychological distress and/or uptake of cancer screening and prevention options? The search was conducted in November 2019 in the following databases: MEDLINE, EMBASE, EMCare, PsycINFO, Epub Ahead of Publication. An updated search was performed in March 2021. The following are examples of Medical Subject Headings (and associated keywords) used in this search: Neoplastic Syndromes, Hereditary/ (hereditary breast and ovarian cancer); Genetic Testing/ (multigene panel testing); Genetic Counseling/ (genetic screening OR genetic risk); Early Detection of Cancer/ ((prophylactic OR preventative) AND (mastectomy OR oophorectomy)); and Stress, Psychological/ (distress OR anxiety). Limitations were set in each database to ensure studies were published in the English language between January 2010 and March 2021 to align with the integration of panel testing into clinical care.
Literature review and data extraction
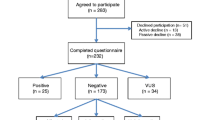
A total of 5469 unique articles were identified through this search (Fig. 1). The titles and abstracts of these articles were manually screened by two independent reviewers (LC, BG, and ET), excluding studies that included any of the following criteria: (i) evaluating alternate forms of genetic testing and/or non-HBOC syndromes; (ii) evaluating clinical interventions and/or models of care; (iii) examining the familial implications of hereditary cancer genetic testing; (iv) pediatric and/or adolescent malignancies; (v) in-vitro and biomarker-focused studies; (vi) review articles or meta-analyses; (vii) clinical case reports, expert opinion articles, and/or clinical guidelines; and (viii) studies examining cancer screening modalities and surgical strategies in high-risk cohorts. A subset of 99 articles were then selected for full text review referencing the same exclusion criteria, from which a final set of 16 articles were selected for complete review and data extraction. The following data points were extracted: (i) study publication details; (ii) study design; (iii) sample description (including sample size); (iv) methods description (including survey tools and timing of assessments); (v) psychological outcomes and/or cancer screening and prevention outcomes (Tables 1 and 2 – condensed versions).
Quality assessment
The Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields developed by Kmet and colleagues (2004) was used to assess the quality of articles [36]. This assessment involved an evaluation of the key aspects of the research design, analysis, and reported results for each of the final articles. Quality assessments were completed by two reviewers for each of the final 16 articles. Discordant quality assessments were resolved by a third reviewer conducting a quality assessment.
Results
Sixteen research studies met the eligibility criteria, including 5 prospective, 2 cross-sectional, and 9 retrospective cohort studies (Tables 1 and 2). Methodological differences between studies limited the findings of this review to a descriptive analysis. Specifically, inconsistent reporting of key participant and clinical details (familial and clinical variables, and genetic testing details) and variability in study methods and the clinical populations. All articles met quality review assessment thresholds by two independent reviewers [36]. The median quality assessment for the final 16 articles was 0.90 (range = 0.70–1.0).
Sample sizes ranged between 49 and 2000, with a total of 7781 participants enrolled across the 16 studies. Participants were predominantly female (93%) and Caucasian (61%). The mean age of participants ranged between 47.7 to 55.3 years. Amongst the 8 studies that reported education levels of study participants [20, 22,23,24,25,26,27, 32], the majority of study participants (63%) were college or university educated. Eight studies exclusively evaluated panel testing [21, 23, 24, 26, 29, 34], the remaining studies included participants who underwent either targeted (e.g. BRCA1/2) or panel testing. Five studies included individuals diagnosed with breast cancer [26,27,28, 30, 32] and eleven studies included affected and unaffected individuals [20,21,22,23,24,25, 29, 31, 33,34,35]. The majority of studies included in this review were conducted in the United States (n = 14).
Psychological outcomes (Table 1)
Four prospective studies evaluated changes in psychological outcomes following multi-gene panel testing [20, 21, 24, 25], and two studies described psychological outcomes of affected and unaffected individuals from clinical cancer genetics programs at a single time point post-disclosure [22, 23]. Psychological outcomes included: anxiety and depression (State Trait Anxiety Inventory [STAI] [20, 24] and Hospital and Depression Scale [HADS] [20, 24]), cancer worry (Cancer Worry Scale [CWS]), cancer-related distress (Impact of Event Scale [IES] [21, 22, 24]), and genetic testing specific concerns (Multidimensional Impact of Cancer Risk Assessment [MICRA] [21,22,23,24] and Psychosocial Aspects of Hereditary Cancer [PHAC] [25]). Prospective studies included pre- and post-test evaluation [20, 25] and longitudinal follow-up (1-week to 12-months post-disclosure) [21, 24]. Study participants were recruited from cancer genetics programs, only three study explicitly stated that participants met NCCN guidelines for HBOC testing [21, 28, 33].
Anxiety and depression
Two studies measured changes in anxiety and depression levels over time among all tested individuals in the study sample and between subgroups based upon test result (pathogenic variant (PV), VUS or negative result) [20, 24]. No significant changes in state and general anxiety or general depression were observed post-disclosure compared to baseline levels [20]. In their follow-up study, Bradbury and colleagues [24] observed a significant increase in depression levels amongst all study participants at 12-months post-disclosure. Although the change in depression levels was statistically significant (p < 0.01) at 12-months it did not reach clinical significance (HADS score of < 8/21). No between group differences based upon variant pathogenicity were observed in anxiety and depression levels across 12-month follow-up [24].
Cancer worry
A single study used the CWS to evaluate cancer worry longitudinally [21]. No significant changes in cancer worry were noted over 12-month follow-up and there were no between group differences observed based upon genetic test results (positive, negative, VUS). Levels of cancer worry were higher at all post-disclosure time points in the moderate penetrance variant subgroup compared to high penetrance subgroup, however, was only significant at 1-week post-disclosure (p = 0.043) [21].
Cancer related distress
Three studies used the IES tool to measure changes in cancer-related distress levels over time [20, 21, 24]. Pre- and post-disclosure comparison did not reveal significant changes in cancer-related distress [20]. No differences in cancer-related distress were observed longitudinally (3 time points) between groups classified by test result (positive, VUS, and negative), but the moderate penetrance variant subgroup was shown to have higher mean IES scores compared to the high penetrance subgroup at 12 months post-disclosure (30.67 vs 10.71, p = 0.031) [21]. Bradbury and colleagues [24] focused on within group change over 12-month follow-up and observed no changes in cancer-related distress levels in the PV and negative test result subgroups. However, VUS carriers reported significantly elevated cancer-related distress levels at 6-months post-disclosure compared to baseline (p = 0.04).
One cross-sectional study found that PVs were associated with higher mean scores on the IES tool when measured 13 months post-disclosure compared to VUS and negative result subgroups [22]. Lumish and colleagues [22] considered the interaction between personal cancer history and genetic test result in their analysis. Unaffected carriers with a PV reported statistically elevated levels of distress compared to affected individuals with a PV, as well as when compared to unaffected and affected individuals with a VUS or negative result (p < 0.05).
Genetic testing specific concerns
Two studies [20, 21] used the MICRA tool to measure changes in genetic testing specific concerns over time among all tested individuals in the study sample and between subgroups based upon both the test result (pathogenic, VUS or negative result) and gene penetrance. Pre- and post-disclosure evaluation did not reveal significant changes in testing concerns [20]. Between group differences in testing-specific distress (MICRA subscale) was observed longitudinally when subgroups were classified by type of test result and gene penetrance [21]. Higher levels of distress were associated with a PV compared to VUS and negative test result subgroups (p < 0.01) at all time points (1-week; 3- and 12-month post-disclosure). Moderate penetrance PV were also observed to be associated with higher reported levels of distress compared to those with a high penetrance PV at the 12-month time point (17.67 vs 6.59, p = 0.026).
Two studies evaluated between group differences on the MICRA tool based upon variant pathogenicity at a single follow-up time point [22, 23]. Idos and colleagues [23] found that a PV was associated with higher reported levels of testing concerns compared to negative and VUS subgroups. The VUS subgroup was observed to have higher levels of testing-related uncertainty (MICRA subscale) compared to the negative result subgroup (p = 0.017). Similarly, Lumish et al. [22] observed higher genetic testing specific distress (MICRA distress subscale) in the unaffected carrier subgroup compared to affected carriers, as well as when compared to affected and unaffected individuals with VUS or a negative test result (p < 0.05).
One study prospectively evaluated changes in PAHC scores over time (pre- and 2 months post-disclosure) among all tested individuals and between group differences based upon gene panel result (pathogenic BRCA1/2 variant; non-BRCA1/2 pathogenic variant; VUS; and negative result) [25]. Overall, concerns related to ‘hereditary risk’ (p < 0.001), ‘personal cancer risk’ (p < 0.05), and ‘children-related considerations’ (p < 0.001) decreased over time in the study sample. Between group differences based upon the genetic test result were observed pre- and 2-months post-disclosure in concerns related to ‘hereditary risk’ and ‘familial and social issues’.
Behavioral Outcomes (Table 2)
Five studies examined uptake of prophylactic surgery in patients diagnosed with breast cancer [26,27,28, 30, 32], and five studies evaluated the medical recommendations and patient-reported uptake of prophylactic surgery of patients reviewed in clinical genetics programs (affected and unaffected individuals) [23, 29, 31, 33, 35]. Three studies evaluated cancer screening uptake after result disclosure in patients of a cancer genetics clinic, including both affected and unaffected individuals [22, 24, 34].
Prophylactic surgery: breast cancer patient cohorts
Across studies, rates of contralateral prophylactic mastectomy (CPM) in women with breast cancer was higher in individuals with a PV compared to VUS and negative test result subgroups [26,27,28, 32]. Kurian et al. [27] found that uptake of CPM is more likely in individuals with a PV compared to a negative result (OR, 7.7; 95% CI, 3.9 to 15.3). In their 2018 study, Kurian and colleagues [32] expanded their analysis to include a subgroup of individuals with PV in genes other than BRCA1/2. Similar to their findings in 2017, a BRCA1/2 PV was more strongly associated with both patient consideration of a CPM (p < 0.001), as well as a surgeon’s management recommendation for a CPM (p < = 0.001) when compared to the remaining three categories (PV in a non-BRCA gene, VUS, and negative result). This contrasts findings from Elsayegh and colleagues [26] who reported that carriers of a PV (BRCA1/2 and non-BRCA1/2) were more likely than VUS carriers to undergo a CPM (p < 0.0001), with no statistical difference found between BRCA1/2 and non-BRCA1/2 PVs. Observed rates of CPM in the VUS and negative subgroup ranged between 21.4%-30.2% and 20.1%-35.3%, respectively [28, 30, 32].
Prophylactic surgery: clinical genetics patient cohorts (unaffected and affected)
Overall, higher rates of prophylactic mastectomy and oophorectomy were associated with a PV compared to those with a VUS or negative test result [23, 31]. This association was found to be statistically significant at 13 months (p < 0.001) and 27.1 months (p = 0.03) post-disclosure in two studies [23, 31]. Chang and colleagues [31] found prophylactic oophorectomy rates were higher with PV in high penetrance genes (10.7%) compared to moderate penetrance (1.7%) and low risk (2.6%) genes (p = 0.05). This association was not observed in rates of prophylactic mastectomy. Two studies reported rates of prophylactic surgery in a cohort of individuals with non-BRCA PV [34, 35], supporting patient adherence to medical recommendations following result disclosure.
Two additional studies evaluated changes in clinical management plans following multi-gene panel testing. Frost and colleagues [33] observed a change to the clinical management plan in 23.3% of patients who underwent genetic testing. This included prophylactic surgery in 37.1% of patients and chemoprevention in 0.1% of patients. Conversely, Bunnell et al. [29] identified an actionable variant in only 8.8% (n = 12) of their sample, and the recommendations for clinical management (screening and/or prophylactic surgery) changed for 10 of those individuals. Of interest, 8 of the 12 individuals had non-BRCA PVs which informed medical recommendations.
Cancer screening
Three studies evaluated patient reported uptake and/or intention regarding cancer screening and prevention options in a cohort of affected and unaffected individuals referred to a cancer genetics clinic [22, 24, 34]. Lumish and colleagues [22] observed that a higher proportion of unaffected individuals with a pathogenic variant (92.9% vs 9.1%) or VUS (35% vs. 21.4%) reported that their test result impacted their cancer screening activities compared to affected individuals with a PV or VUS. Caution is warranted given the small number of individuals in each group. Bradbury and colleagues [24] similarly evaluated patient intention toward cancer screening and prevention but looked at within group changes over a 12-month follow-up (baseline, 1 week, 6- and 12-months post-disclosure). Individuals with a VUS and negative panel test result reported a significantly reduced intention to undergo breast cancer screening at 12 months. This trend over time was not observed in individuals with a PV. Finally, Vysotskaia et al. [34] evaluated changes in medical recommendations following a genetic test result, as well as patient adherence to those recommendations. Recommendations for screening MRI increased (42% to 82% post-disclosure) in individuals with a PV in PALB2, ATM, CHEK2, and/or NBN, which was associated with high rates of compliance (97%) [34].
Discussion
The findings in this review emphasize the need for studies examining psychological and health behavior outcomes associated with panel testing to include between group differences based upon both variant pathogenicity and gene penetrance. Analyzing findings with both classification approaches will be critical in understanding how the clinical uncertainty associated with specific types of results impact psychological, screening and prevention outcomes in this population. Similar to the BRCA1/2 literature, individuals with a PV reported higher levels of testing-related concerns and cancer-specific distress, as well as higher uptake of prophylactic surgery in both affected and unaffected individuals compared to those with VUS or negative result. Interestingly, individuals with MP PVs had higher rates of cancer worry, genetic testing concerns and cancer related distress when compared to women with high penetrance PV [21, 23]. Analysis of health behavior outcomes based upon gene penetrance was limited, with conflicting findings [26, 31, 32], and thus further research is needed.
Future studies designed to evaluate between group differences based upon gene penetrance will require large sample sizes to power such analyses given that the observed frequency of PVs is low. Depending on the clinical population and panel test used, PVs are observed in only 7–12% of tested individuals, which limits the ability to look at differences based upon penetrance due to the small numbers in each subgroup [23, 24, 37, 38]. In this review, the number of individuals carrying a MP PV was variable across study samples, ranging from 4 ATM carriers (11% of pathogenic variants) [21] to 12 MP (ATM, CDH1, CHEK2, PALB2, NBN, NF1, and STK11) carriers (17% of pathogenic variants) [23]. In addition, classification of MP variants was not consistent across studies. For example, PALB2 was classified as both a MP and high penetrance variant in different studies [21, 31]. Thus, caution is warranted when interpreting these findings given the small number of individuals in each subgroup and the lack of uniform classification of variants.
Despite the low expected frequency of PVs with panel testing, initial work by Kurian and colleagues [38] in a BRCA1/2 negative cohort, found that of the 15 PVs identified, 14 were actionable and informed medical management. This aligns with the observed changes in clinical management of individuals found to have a PV in this review [29, 33]. In both studies [29, 33] challenges were reported when formulating management plans for MP PVs and newly identified genes (e.g. BARD1 and NBN) due to a lack of available medical management guidelines [29, 33]. This supports the need for individualized genetic counselling, as clinical expertise is required to provide recommendations in the absence of guidelines, by drawing on relevant literature in the context of the patient’s personal and familial history. Given limited genetic counseling resources and an increasing proportion of panel-based testing offered by non-genetics healthcare providers, post-test counseling with a certified genetic counselor may provide the optimal setting for this discussion [39].
Results from this review indicate that while more individuals with a PV undergo preventative surgery following panel testing compared to those with a VUS or negative result, a VUS result may inform cancer screening and prevention decisions. Kurian and colleagues [32] found rates of prophylactic surgery to be approximately 30% in affected patients with VUS and negative test results. These authors argued that the similar rates of prophylactic surgery observed between VUS and negative cohorts was suggestive that those with a VUS were not overestimating their cancer risk. These findings may support this claim, but it is worth considering that 30.2% of participants with a VUS opted to have prophylactic surgery, when it was recommended by the surgeon in 14.1% of cases [32]. Across studies in this review, VUS results were found to inform cancer screening and prevention decisions in approximately one-third of unaffected patients [22, 28, 30, 32]. As such, further work is needed to explore patient interpretation of cancer risk after receiving a VUS result and the perceived utility of these variants. Currently, there is limited data regarding other factors that may contribute to a patient’s risk management decision, such as current disease attributes, family history of cancer, as well as cancer and genetic testing related distress. Understanding patient decision-making surrounding cancer screening and prevention is further complicated by the inconsistent reporting of gene variants. Lumish and colleagues [22] noted that 62.5% of VUS were in a high penetrance gene, which may have contributed to the perceived utility of these variants. Consistent reporting of the gene where the VUS was identified may illuminate differences in health behavior outcomes and also reinforce the need for patient follow-up for variant reclassification updates.
Finally, screening for heightened levels of distress requires measuring these outcomes with tools that include clinical thresholds, such that clinically significant distress can be identified and appropriately managed. The BRCA1/2 literature suggests that the majority of patients do not experience persistent psychological distress but estimates that 20–25% of tested individuals report long-term negative affective outcomes [15, 19]. Thus, as we evaluate psychological outcomes in the context of panel testing, it is important to question whether these observed differences in psychological outcomes actually translate into clinically meaningful differences. Lumish and colleagues [22] found the mean IES score of the unaffected carrier subgroup was significantly higher than all remaining subgroups 13 months post-disclosure (p = 0.01), yet the level of distress was considered ‘mild’ (< 25) on the IES tool, and not clinically significant. This can be contrasted with the findings from Esteban et al. [21], where the MP subgroup reported a mean score on the IES-R tool at a level where symptoms of distress may be present, suggesting clinical significance. Thus, it is important that when between group differences are evaluated for statistical differences, that they are also evaluated for clinical significance. Identifying subgroups at increased risk of experiencing clinically meaningful distress may assist in providing tailored genetic counselling and identifying supportive resources for those individuals that are at higher risk of experiencing negative psychological outcomes.
Limitations
This literature review has several limitations. First, due to variable reporting of participant details and methodological differences, this review was limited to a descriptive analysis. Although, the authors followed a rigorous and systematic approach when conducting this literature search and synthesis of findings, this review was not pre-registered for PROSPERO. Second, this review was limited to publications in the English language, with most of the articles published by research teams in the USA (n = 14), which potential limits scope and relevance of the findings. In addition, across the studies in this review, the majority of participants were Caucasian women, who were highly educated, which may limit the generalizability of the findings. Finally, the conclusions drawn in this review are based upon the classification of variant pathogenicity and gene penetrance published in the included articles, which reflects the knowledge and guidelines at the time of each publication.
Conclusions
The findings in this review highlight the importance of considering both variant pathogenicity and gene penetrance when exploring the impact of panel testing on psychological and health behavior outcomes. With the growing trend towards multi-gene panel testing, healthcare providers should be cognizant of individuals who are at risk for increased cancer worry and distress, as well as those who may overestimate their cancer risk and undergo inappropriate risk reduction surgery. Further research is needed to explore the factors that contribute to heightened levels of cancer worry and distress, the different personal demographics and clinical variables that inform cancer screening and prevention decisions, and the impact of supportive resources and counselling.
Availability of data and materials
Not applicable.
References
Kuusisto KM, Bebel A, Vihinen M, Schleutker J, Sallinen SL. Screening for BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 mutations in high-risk Finnish BRCA1/2-founder mutation-negative breast and/or ovarian cancer individuals. Breast Canc Res : BCR. 2011;13(1):R20. https://doi.org/10.1186/bcr2832.
Maxwell KN, Nathanson KL. Common breast cancer risk variants in the post-COGS era: a comprehensive review. Breast Canc Res : BCR. 2013;15(6):212. https://doi.org/10.1186/bcr3591.
Hamilton, Jada G, and Mark E Robson. “Psychosocial Effects of Multigene Panel Testing in the Context of Cancer Genomics.” The Hastings Center report vol. 49 Suppl 1,Suppl 1 (2019): S44-S52. https://doi.org/10.1002/hast.1016
Easton DF, Lesueur F, Decker B, Michailidou K, Li J, Allen J, Luccarini C, Pooley KA, Shah M, Bolla MK, Wang Q, Dennis J, Ahmad J, Thompson ER, Damiola F, Pertesi M, Voegele C, Mebirouk N, Robinot N, Durand G, Chenevix-Trench G. No evidence that protein truncating variants in BRIP1 are associated with breast cancer risk: implications for gene panel testing. J Med Genet. 2016;53(5):298–309. https://doi.org/10.1136/jmedgenet-2015-103529.
Tung N, Domchek SM, Stadler Z, Nathanson KL, Couch F, Garber JE, Offit K, Robson ME. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol. 2016;13(9):581–8. https://doi.org/10.1038/nrclinonc.2016.90.
Breast Cancer Association Consortium, Dorling L, Carvalho S, Allen J, González-Neira A, Luccarini C, Wahlström C, Pooley KA, Parsons MT, Fortuno C, Wang Q, Bolla MK, Dennis J, Keeman R, Alonso MR, Álvarez N, Herraez B, Fernandez V, Núñez-Torres R, Osorio A, Easton DF. Breast cancer risk genes - association analysis in more than 113,000 women. N Engl J Med. 2021;384(5):428–39. https://doi.org/10.1056/NEJMoa1913948.
Hu C, Hart SN, Gnanaolivu R, Huang H, Lee KY, Na J, Gao C, Lilyquist J, Yadav S, Boddicker NJ, Samara R, Klebba J, Ambrosone CB, Anton-Culver H, Auer P, Bandera EV, Bernstein L, Bertrand KA, Burnside ES, Carter BD, Couch FJ. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384(5):440–51. https://doi.org/10.1056/NEJMoa2005936.
Daly MB, Pal T, Berry MP, Buys SS, Dickson P, Domchek SM, Elkhanany A, Friedman S, Goggins M, Hutton ML, Karlan BY, Khan S, Klein C, Kohlmann W, Kurian AW, Laronga C, Litton JK, Mak JS, Menendez CS, Merajver SD, Yurgelun MB. NCCN clinical practice guidelines in oncology (NCCN Guidelines) genetic/familial high-risk assessment: beast, ovarian, and pancreatic. NCCN, Version 2.2021. 2020.
Pilarski R. How have multigene panels changed the clinical practice of genetic counseling and testing. J Natl Compr Canc Netw. 2021;19(1):103–8. https://doi.org/10.6004/jnccn.2020.7674.
Bennette CS, Trinidad SB, Fullerton SM, Patrick D, Amendola L, Burke W, Hisama FM, Jarvik GP, Regier DA, Veenstra DL. Return of incidental findings in genomic medicine: measuring what patients value–development of an instrument to measure preferences for information from next-generation testing (IMPRINT). Genet Med. 2013;15(11):873–81. https://doi.org/10.1038/gim.2013.63.
Blanchette PS, Spreafico A, Miller FA, Chan K, Bytautas J, Kang S, Bedard PL, Eisen A, Potanina L, Holland J, Kamel-Reid S, McPherson JD, Razak AR, Siu LL. Genomic testing in cancer: patient knowledge, attitudes, and expectations. Cancer. 2014;120(19):3066–73. https://doi.org/10.1002/cncr.28807.
Gray SW, Hicks-Courant K, Lathan CS, Garraway L, Park ER, Weeks JC. Attitudes of patients with cancer about personalized medicine and somatic genetic testing. Journal of oncology practice. 2012;8(6):329–35. https://doi.org/10.1200/JOP.2012.000626.
Bradbury AR, Patrick-Miller L, Long J, Powers J, Stopfer J, Forman A, Rybak C, Mattie K, Brandt A, Chambers R, Chung WK, Churpek J, Daly MB, Digiovanni L, Farengo-Clark D, Fetzer D, Ganschow P, Grana G, Gulden C, Hall M, Domchek SM. Development of a tiered and binned genetic counseling model for informed consent in the era of multiplex testing for cancer susceptibility. Genet Med. 2015;17(6):485–92. https://doi.org/10.1038/gim.2014.134.
Domchek SM, Bradbury A, Garber JE, Offit K, Robson ME. Multiplex genetic testing for cancer susceptibility: out on the high wire without a net? J Clin Oncol. 2013;31(10):1267–70. https://doi.org/10.1200/JCO.2012.46.9403.
Vadaparampil ST, Miree CA, Wilson C, Jacobsen PB. Psychosocial and behavioral impact of genetic counseling and testing. Breast Dis. 2006;27:97–108. https://doi.org/10.3233/bd-2007-27106.
Graves KD, Vegella P, Poggi EA, Peshkin BN, Tong A, Isaacs C, Finch C, Kelly S, Taylor KL, Luta G, Schwartz MD. Long-term psychosocial outcomes of BRCA1/BRCA2 testing: differences across affected status and risk-reducing surgery choice. Cancer Epidemiol Biomarkers Prev. 2012;21(3):445–55. https://doi.org/10.1158/1055-9965.EPI-11-0991.
van Dijk S, Timmermans DR, Meijers-Heijboer H, Tibben A, van Asperen CJ, Otten W. Clinical characteristics affect the impact of an uninformative DNA test result: the course of worry and distress experienced by women who apply for genetic testing for breast cancer. J Clin Oncol. 2006;24(22):3672–7. https://doi.org/10.1200/JCO.2005.03.7259.
Vos, J., Gómez-García, E., Oosterwijk, J. C., Menko, F. H., Stoel, R. D., van Asperen, C. J., Jansen, A. M., Stiggelbout, A. M., & Tibben, A. Opening the psychological black box in genetic counseling. The psychological impact of DNA testing is predicted by the counselees' perception, the medical impact by the pathogenic or uninformative BRCA1/2-result. Psycho-oncology. 2012;21(1):29–42. https://doi.org/10.1002/pon.1864
Eijzenga W, Hahn DE, Aaronson NK, Kluijt I, Bleiker EM. Specific psychosocial issues of individuals undergoing genetic counseling for cancer - a literature review. J Genet Couns. 2014;23(2):133–46. https://doi.org/10.1007/s10897-013-9649-4.
Bradbury AR, Patrick-Miller LJ, Egleston BL, DiGiovanni L, Brower J, Harris D, Stevens EM, Maxwell KN, Kulkarni A, Chavez T, Brandt A, Long JM, Powers J, Stopfer JE, Nathanson KL, Domchek SM. Patient feedback and early outcome data with a novel tiered-binned model for multiplex breast cancer susceptibility testing. Genet Med. 2016;18(1):25–33. https://doi.org/10.1038/gim.2015.19.
Esteban I, Vilaró M, Adrover E, Angulo A, Carrasco E, Gadea N, Sánchez A, Ocaña T, Llort G, Jover R, Cubiella J, Servitja S, Herráiz M, Cid L, Martínez S, Oruezábal-Moreno MJ, Garau I, Khorrami S, Herreros-de-Tejada A, Morales R, Balmaña J. Psychological impact of multigene cancer panel testing in patients with a clinical suspicion of hereditary cancer across Spain. Psychooncology. 2018;27(6):1530–7. https://doi.org/10.1002/pon.4686.
Lumish HS, Steinfeld H, Koval C, Russo D, Levinson E, Wynn J, Duong J, Chung WK. Impact of panel gene testing for hereditary breast and ovarian cancer on patients. J Genet Couns. 2017;26(5):1116–29. https://doi.org/10.1007/s10897-017-0090-y.
Idos GE, Kurian AW, Ricker C, Sturgeon D, Culver JO, Kingham KE, Koff R, Chun NM, Rowe-Teeter C, Lebensohn AP, Levonian P, Lowstuter K, Partynski K, Hong C, Mills MA, Petrovchich I, Ma CS, Hartman A, Allen B, Wenstrup RJ, Gruber SB. Multicenter prospective cohort study of the diagnostic yield and patient experience of multiplex gene panel testing for hereditary cancer risk. JCO Precis Oncol. 2019. https://doi.org/10.1002/cncr.32572.
Bradbury AR, Egleston BL, Patrick-Miller LJ, Rustgi N, Brandt A, Brower J, DiGiovanni L, Fetzer D, Berkelbach C, Long JM, Powers J, Stopfer JE, Domchek SM. Longitudinal outcomes with cancer multigene panel testing in previously tested BRCA1/2 negative patients. Clin Genet. 2020;97(4):601–9. https://doi.org/10.1111/cge.13716.
Brédart A, Kop JL, Dick J, Cano A, De Pauw A, Anota A, Brunet J, Devilee P, Stoppa-Lyonnet D, Schmutzler R, Dolbeault S. Psychosocial problems in women attending French, German and Spanish genetics clinics before and after targeted or multigene testing results: an observational prospective study. BMJ Open. 2019;9(9):e029926. https://doi.org/10.1136/bmjopen-2019-029926.
Elsayegh N, Webster RD, Gutierrez Barrera AM, Lin H, Kuerer HM, Litton JK, Bedrosian I, Arun BK. Contralateral prophylactic mastectomy rate and predictive factors among patients with breast cancer who underwent multigene panel testing for hereditary cancer. Cancer Med. 2018;7(6):2718–26. https://doi.org/10.1002/cam4.1519.
Kurian AW, Li Y, Hamilton AS, Ward KC, Hawley ST, Morrow M, McLeod MC, Jagsi R, Katz SJ. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232–9. https://doi.org/10.1200/JCO.2016.71.6480.
Pederson HJ, Gopalakrishnan D, Noss R, Yanda C, Eng C, Grobmyer SR. Impact of multigene panel testing on surgical decision making in breast cancer patients. J Am Coll Surg. 2018;226(4):560–5. https://doi.org/10.1016/j.jamcollsurg.2017.12.037.
Bunnell AE, Garby CA, Pearson EJ, Walker SA, Panos LE, Blum JL. The clinical utility of next generation sequencing results in a community-based hereditary cancer risk program. J Genet Couns. 2017;26(1):105–12. https://doi.org/10.1007/s10897-016-9985-2.
Murphy AE, Hussain L, Ho C, Dunki-Jacobs E, Lee D, Tameron A, Huelsman K, Rice C, Wexelman BA. Preoperative panel testing for hereditary cancer syndromes does not significantly impact time to surgery for newly diagnosed breast cancer patients compared with BRCA1/2 testing. Ann Surg Oncol. 2017;24(10):3055–9. https://doi.org/10.1245/s10434-017-5957-5.
Chang J, Seng S, Yoo J, Equivel P, Lum SS. Clinical management of patients at risk for hereditary breast cancer with variants of uncertain significance in the era of multigene panel testing. Ann Surg Oncol. 2019;26(10):3389–96. https://doi.org/10.1245/s10434-019-07595-230Frostetal.,2018.
Kurian AW, Ward KC, Hamilton AS, Deapen DM, Abrahamse P, Bondarenko I, Li Y, Hawley ST, Morrow M, Jagsi R, Katz SJ. Uptake, results, and outcomes of germline multiple-gene sequencing after diagnosis of breast cancer. JAMA Oncol. 2018;4(8):1066–72. https://doi.org/10.1001/jamaoncol.2018.0644.
Frost AS, Toaff M, Biagi T, Stark E, McHenry A, Kaltman R. Effects of cancer genetic panel testing on at-risk individuals. Obstet Gynecol. 2018;131(6):1103–10. https://doi.org/10.1097/AOG.0000000000002531.
Vysotskaia V, Kaseniit KE, Bucheit L, Ready K, Price K, Johansen Taber K. Clinical utility of hereditary cancer panel testing: Impact of PALB2, ATM, CHEK2, NBN, BRIP1, RAD51C, and RAD51D results on patient management and adherence to provider recommendations. Cancer. 2020;126(3):549–58. https://doi.org/10.1002/cncr.32572.
Caskey R, Singletary B, Ayre K, Parker C, Krontiras H, Lancaster RB. Expectations of surveillance for non-BRCA gene mutation carriers at increased risk for breast cancer. J Surg Res. 2020;256:267–71. https://doi.org/10.1016/j.jss.2020.06.029.
Kmet LM, Lee R C, Cook LS. 2004. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. [S.I] Alberta Heritage Foundation for Medical Research. https://books.scholarsportal.info/en/read?id=/ebooks/ebooks1/gibson_chrc/2010-08-06/1/10082980.
Frey MK, Kim SH, Bassett RY, Martineau J, Dalton E, Chern JY, Blank SV. Rescreening for genetic mutations using multi-gene panel testing in patients who previously underwent non-informative genetic screening. Gynecol Oncol. 2015;139(2):211–5. https://doi.org/10.1016/j.ygyno.2015.08.006.
Kurian AW, Hare EE, Mills MA, Kingham KE, McPherson L, Whittemore AS, McGuire V, Ladabaum U, Kobayashi Y, Lincoln SE, Cargill M, Ford JM. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32(19):2001–9. https://doi.org/10.1200/JCO.2013.53.6607.
Hoskovec JM, Bennett RL, Carey ME, DaVanzo JE, Dougherty M, Hahn SE, LeRoy BS, O’Neal S, Richardson JG, Wicklund CA. Projecting the supply and demand for certified genetic counselors: a workforce study. J Genet Couns. 2018;27(1):16–20. https://doi.org/10.1007/s10897-017-0158-8.
Acknowledgements
We acknowledge the conceptual and editorial support provided by Dr. Raymond H Kim MD/PhD, FRCPC and Dr. Philippe Bedard MD FRCPC (c), who are members of the supervisory committee of the first author (L.C). We also acknowledge the support of Rouhi Fazelzad, Information Specialist at Princess Margaret Cancer Centre who supported the development and execution of the search strategy.
Funding
No funding was received to support this literature review.
Author information
Authors and Affiliations
Contributions
All authors provided substantial contribution to this manuscript. Conceptualization and methodology: L.C., E.T., B.G., and K.M; article screening L.C., E.T, and B.G.; data extraction L.C.; initial manuscript development L.C., and manuscript review and editing L.C., E.T., B.G., and K.M. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Carlsson, L., Thain, E., Gillies, B. et al. Psychological and health behaviour outcomes following multi-gene panel testing for hereditary breast and ovarian cancer risk: a mini-review of the literature. Hered Cancer Clin Pract 20, 25 (2022). https://doi.org/10.1186/s13053-022-00229-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13053-022-00229-x