Abstract
Background
Several studies have identified graded oxygen saturation targets to prevent retinopathy of prematurity (ROP), a serious complication in preterm infants. We aimed to analyze the critical period of oxygen supplementation and/or invasive ventilation associated with severe ROP.
Methods
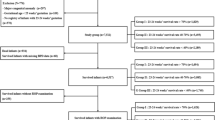
This retrospective case-control study included neonates with a gestational age (GA) < 29 weeks. Participants were divided into two groups: treated retinopathy and untreated/no retinopathy. Time-weighted average FiO2 (TWAFiO2) and weekly invasive ventilation were compared between groups by postnatal age (PNA) and postmenstrual age (PMA). The association of treated retinopathy with TWAFiO2 and invasive ventilation was analyzed.
Results
Data from 287 neonates were analyzed; 98 were treated for ROP and had lower GAs (25.5 vs. 27.4 weeks, p < 0.01) and lower birthweights (747.6 vs. 1014 g, p < 0.001) than those with untreated/no ROP. TWAFiO2 was higher from PMA 26–34 weeks, except for PMA 31 weeks in treated ROP, and higher in the first nine weeks of life in treated ROP. On multiple logistic regression, TWAFiO2 and invasive ventilation were associated with ROP treatment during the first seven weeks PNA. Invasive ventilation was associated with ROP treatment from PMA 26–31 weeks; no association was found for TWAFiO2 and PMA.
Conclusions
Amount of oxygen supplementation and/or invasive ventilation during the first 7 weeks of life or up to 31 weeks PMA was associated with development of severe ROP. This period might be candidate timing for strict oxygen supplementation strategies in preterm infants, while concerns of mortality with low oxygen supplementation should be further explored.
Similar content being viewed by others
Background
Retinopathy of prematurity (ROP) is a serious complication in preterm infants and can lead to blindness in severe cases. The incidence of ROP has been reported to be 60–70% in preterm infants with a birthweight of less than 1500 g or with extremely low gestational age (GA), with treatment required in one-fourth of cases [1,2,3]. The pathophysiology of the disease is abnormal growth of retinal blood vessels, which is associated with low GA and birthweight [4,5,6]. After preterm birth, excessive oxygenation via ventilatory support contributes to the development of ROP in the early stages by inhibiting retinal vascular development (phase I), followed by vasoproliferation induced by hypoxia in the avascular regions of the retina (phase II) [7, 8].
Low oxygen saturation targets have been associated with a reduction in the incidence of ROP, and several randomized controlled trials have been conducted to determine the optimal oxygen supplementation to prevent the development of ROP. The Surfactant, Positive Pressure, and Oxygenation Randomized Trial (SUPPORT) showed that the incidence of severe ROP was significantly lower in survivors with a lower oxygen saturation target of 85–89% [9], and a meta-analysis found reduced ROP treatment rates, but increased mortality at 36 weeks postmenstrual age (PMA) and at discharge [10]. Based on these results, the American Academy of Pediatrics (AAP) Committee on Fetuses and Newborns does not recommend a target oxygen saturation of less than 90% [11].
Several recent studies have investigated graded oxygen saturation targets based on PMA [10, 12, 13]. This strategy is based on the pathophysiology of ROP, as hyperoxia in phase I ROP and hypoxia in phase II ROP contribute to the development of ROP in preterm infants. However, studies investigating graded or biphasic oxygen-targeting strategies have been conducted based on the predetermined timing of oxygen saturation differences. So far, there is a lack of data on the duration of the critical period for development of severe ROP from hyperoxia in preterm infants based on the analysis of continuous data of respiratory support or oxygen supplementation. In this study, we aimed to analyze the critical period for oxygen supplementation and/or invasive ventilation with regard to the development of severe ROP in extremely preterm infants.
Methods
This retrospective case-control study included neonates with a GA of < 29 weeks born between 2013 and 2021 who were admitted to the neonatal intensive care unit (NICU) of Seoul National University Children’s Hospital. Patients who died before discharge were excluded from the study. The participants were divided into two groups: (1) those with retinopathy with spontaneous regression (untreated ROP) or those without retinopathy, and (2) those who underwent surgery (treated ROP). ROP was diagnosed and staged according to the International Classification of Retinopathies of Prematurity [14]. Infants with a birthweight < 2,000 g or gestational age less than 32 weeks were initially screened for ROP at 4 weeks PNA or 31–32 weeks’ GA, whichever came first. The patients were treated for extraretinal fibrovascular proliferation above a certain stage 3, a positive finding, or aggressive ROP [14]. The study institution did not offer intravenous injections of bevacizumab, an anti-VEGF drug, during the study period. Data on GA, birthweight, sex, ROP stage, ROP treatment, length of invasive ventilation, length of hospitalization, and inspired oxygen concentrations were collected. The presence of other neonatal comorbid conditions including respiratory distress syndrome (RDS), bronchopulmonary dysplasia, persistent ductus arteriosus (PDA), sepsis, intraventricular hemorrhage, periventricular leukomalacia, necrotizing enterocolitis was also recorded. This study was approved by the Institutional Review Board of our institution (H-2210-131-1372). The requirement for informed consent was waived due to the retrospective study design.
Time-weighted average (TWAFiO2) was calculated as the area under the FiO2 versus the time plot on a weekly basis, and compared between groups according to PNA and PMA. TWAFiO2 during invasive oxygen supplementation, continuous nasal positive end-expiratory pressure, and high-flow nasal cannula (≥ 2 L/min) were included in the calculation. Each week, based on PNA and PMA, the categorical variable of invasive ventilation was determined if more than four days of oxygen supplementation via invasive ventilation was provided. The target SpO2 of the study population during oxygen supplementation was 90–95% regardless of PNA.
The chi-square test was used to compare categorical variables and the independent sample t-test was used to compare continuous variables. GA- and birthweight-adjusted p-values were calculated using adjusted proportion analysis or multiple linear regression analysis for demographic and clinical data. Multivariate logistic regression analysis was performed for ROP treatment on a weekly basis with respect to PMA and PNA, adjusted for GA, birthweight, and duration of invasive ventilation. Continuous variables are presented as mean ± standard deviation (SD). The results were considered statistically significant if the p-value was < 0.05.
Results
Of the 287 infants analyzed, 98 were treated for ROP. Infants in the treated ROP group had a lower gestational age (25.5 vs. 27.4 weeks, p < 0.001) and lower birthweight (747.6 vs. 1014 g, p < 0.001) than those in the untreated/no ROP group (Table 1). After adjusting for GA and birthweight, the prevalence of RDS and treated PDA was significantly higher in the treated ROP group, and infants in the treated ROP group had significantly longer durations of invasive ventilation (46.3 vs. 13.1 days, p < 0.001) and hospitalization.
In a weekly comparison based on PMA, TWAFiO2 was higher from PMA 26–34 weeks, except for PMA at 31 weeks, in the treated ROP group (Table 2). In the comparison based on PNA, TWAFiO2 was higher in the first nine weeks of life in the treated ROP group. In a subgroup analysis, the difference in TWAFiO2 was evident from PNA 2–7 weeks in infants born at 26–28 weeks GA, whereas differences were found at PMA 33 weeks (Supplementary Table 1, Additional file 1). In the subgroup of 23–25 weeks GA, differences were found at 26 weeks of PMA and at two, three, and five weeks of PNA.
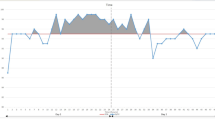
In multivariate logistic regression analysis adjusted for GA, birthweight, and weekly invasive ventilation, invasive ventilation was associated with treated ROP from 1 to 4 weeks PNA, and higher supplemental oxygen (as an increase in FiO2 by 0.1) was associated with treated ROP from 5 to 7 weeks PNA (Fig. 1a). Treated ROP was associated with invasive ventilation from 26 to 31 weeks PMA, whereas the level of supplemental oxygen was not associated with the treated ROP (Fig. 1b).
Association of time-weighted average FiO2 and invasive ventilation with treated ROP. (a) at each postnatal age and (b) at each postmenstrual age. Adjusted for gestational age, birthweight and invasive ventilation at each week (*p < 0.05). FiO2, Fraction of inspired oxygen; ROP, retinopathy of prematurity
Discussion
This study investigated the critical postnatal periods for the development of severe ROP influenced by oxygen supplementation or invasive ventilation in the setting of a target saturation of 90–95% using an institutional protocol. TWAFiO2 or invasive ventilation was associated with ROP treatment in the first 7 weeks PNA. In terms of PMA, invasive ventilation was associated with ROP from PMA 26–31 weeks, whereas no association between TWAFiO2 and treated ROP was found.
One of the notable findings elucidated in the present study pertains to the association between invasive ventilation and severe ROP even after adjusting for the level of oxygen given to the patients. While the existing literature has underscored the link between mechanical ventilation and ROP, prior investigations have not scrutinized the independent impact of invasive ventilation, distinct from the quantity of oxygen concentration delivered [15,16,17]. Although non-invasive ventilation can effectively support patient’s respiratory support, there are disadvantages of oxygenation supplementation compared with invasive ventilation in several aspects [18]. Patient-dependent factors, such as minute ventilation, amount of mouth breathing, leakage around the patient-device interface, and the relative duration of inspiration and expiration, can influence the fractional inspired oxygen concentration, thereby compromising the intended oxygen delivery efficacy [19, 20].
As the present study investigated the level of oxygen given to the patients with regard to the development of severe ROP, considering the mode of ventilation that affects effective oxygen delivery was crucial in this study. Our findings were also supported by the results of an ad hoc analysis, comparing the incidence of severe ROP between patients receiving invasive ventilation and non-invasive ventilation in the subgroup stratified by weekly TWAFiO2 (< 0.3 and ≥ 0.3). Across both subgroup delineations, there was a higher incidence of severe ROP in the group receiving invasive ventilation early in life (Supplementary Table 2, Additional file 1).
After the AAP stated that a lower target saturation strategy for the prevention of ROP could not account for the higher incidence of death in preterm infants, several studies have attempted to demonstrate the effect of a graded saturation target strategy in the prevention of ROP without increasing mortality in preterm infants [10, 12, 13]. The hypothesis that the target saturation varies with age is based on the pathophysiology of ROP, which comprises two phases. In phase I, early hyperoxia induces attenuation of retinal vascular growth and vaso-obliteration. This is followed by the hypoxia-induced phase II vasoproliferation in the avascular areas of the retina [7, 8]. However, these studies evaluated specific periods of oxygen restriction based on the PMA rather than on the PNA. A retrospective study in 2016 applied a graded SpO2 target based on PMA (83–89% until 326/7 weeks, 90–94% until 356/7 weeks, and > 94% at ≥ 36 weeks PMA) and showed decreased rates of severe ROP and laser surgery without increasing mortality [12]. Another study by Shukla et al. compared a graded SpO2 target (85–92% until 336/7 weeks PMA and 95% at ≥ 34 weeks PMA) with a constant target (91–95%) [13]. The results of the present study also showed that setting the period before and after PMA to 32–33 weeks might be rational, as severe ROP was associated with higher level of oxygen supplementation or invasive ventilation before 32 weeks PMA. Moreover, our study investigated the period of interest in terms of PNA. PNA-based evaluation could provide additional information, as preterm infants of various GAs were included in the study. As the oxygen concentration in the atmosphere is higher than that in the intrauterine environment, it can be assumed that virtually all preterm infants are exposed to oxygen stress from the moment they are born.
In recent years, there has been an increasing focus in preclinical and clinical research on target therapies aimed at decoupling oxygenation and vascularization [21, 22]. Given the variability in VEGF levels between phase I and phase II of ROP pathogenesis, it is valuable to identify specific target periods where therapeutic interventions can maximize their efficacy in decoupling the effects of oxygen on vascular development. Hence, the results of the current study may provide insights into determining the optimal timing of these therapeutic agents in future applications.
The first limitation of the present study is that different oxygen saturations were not compared. Instead, we sought to evaluate the effect of the actual amount of oxygen supplementation and invasive ventilation on severe ROP. The analysis of these factors is a different approach from previous studies that set different oxygen saturation targets [10, 12, 13]. However, SpO2 can be affected by other systemic conditions such as pulmonary hypertension, blood pressure, or lung disease. In fact, the treated ROP group in this study tended to have lower mean SpO2 values, even though they were supplemented with higher oxygen levels (Supplementary Table 3, Additional file 1). Moreover, because oxygen can be delivered both invasively and noninvasively, and the level of oxygen can be determined accordingly, the association of invasive ventilation at a specific PNA or PMA with the development of severe ROP was also considered. Considering the graded oxygen saturation target strategy, the first seven weeks of life or up to PMA 31 weeks could be a candidate period for a lower saturation target. As infants who died before discharge were excluded from the study population, the concerns regarding mortality in the lower saturation target group, as seen in previous studies such as the SUPPORT trial, could not be addressed in this study. The primary objective of the present study was to investigate the vulnerable period in the development of severe ROP in preterm infants.
Another limitation of this study is that we did not calculate the actual amount of oxygen delivered during non-invasive ventilation. However, the aim of this study was not to determine the exact amount of oxygenation that increases the risk of severe ROP but rather to investigate the period of significance affected by oxygen supplementation and invasive ventilation. Therefore, we adjusted for invasive ventilation in each period.
Conclusion
Differences in required oxygen supplementation and/or invasive ventilation between the untreated and treated ROP groups were present in our population sample. The first 7 weeks of life or up to PMA 31 weeks may be a candidate period for a lower saturation target when considering graded or biphasic oxygen saturation target strategies for reducing ROP. Further prospective studies are required to determine the critical period for oxygen restriction policies for neonates born before 29 weeks GA.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AAP:
-
American Academy of Pediatrics
- BPD:
-
Bronchopulmonary dysplasia
- GA:
-
Gestational age
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- PDA:
-
Patent ductus arteriosus
- PMA:
-
Postmenstrual age
- PNA:
-
Postnatal age
- PVL:
-
Periventricular leukomalacia
- RDS:
-
Respiratory distress syndrome
- ROP:
-
Retinopathy of prematurity
- SGA:
-
Small for gestational age
- SUPPORT:
-
Surfactant, Positive Pressure, and Oxygenation Randomized Trial
- TWAFiO2 :
-
Time-weighted average FiO2
References
Stoll BJ, Hansen NI, Bell EF, shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Hong EH, Shin YU, Bae GH, Choi YJ, Ahn SJ, Sobrin L, et al. Nationwide incidence and treatment pattern of retinopathy of prematurity in South Korea using the 2007–2018 national health insurance claims data. Sci Rep. 2021;11:1451.
Hwang JH, Lee EH, Kim EAR. Retinopathy of prematurity among very-low-birth-weight infants in Korea: Inidence, treatment, and risk factors. J Korean Med Sci. 2015;30(Suppl 1):S88–94.
Hartnett ME, Penn JS. Mechanisms and management of retinopathy of prematurity. N Engl J Med. 2012;367:2515–26.
Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips CL, Schaffer DB, et al. Incidence and early course of retinopathy of prematurity. Ophthalmology. 1991;98:1628–40.
Arima M, Fujii Y, Sonoda KH. Translational research in retinopathy of prematurity: from bedside to bench and back again. J Clin Med. 2021;10:331.
Penn JS, Tolman BL, Lowery LA. Variable oxygen exposure causes preretinal neovascularization in the newborn rat. Investig Ophthalmol Vis Sci. 1993;34:576–85.
Pierce EA, Avery RL, Foley ED, Smith LE. Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc Natl Acad Sci U S A. 1995;92:905–9.
SUPPORT study group of the Eunice Kennedy Shiriver NICHD Neonatal research network. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69.
Chen ML, Guo L, Smith LE, Dammann CE, Dammann O. High or low oxygen saturation and severe retinopathy of prematurity: a meta-anaylsis. Pediatrics. 2010;125:e1483–92.
Cummings JJ, Polin RA, Committee on fetus and newborn, Watterberg KL, Poindexter B, Benitz WE et al. Oxygen targeting in extremely low birth weight infants. Pediatrics. 2016;138:e20161576.
Cayabyab R, Arora V, Wertheimer F, Durand M, Ramanathan R. Graded oxygen saturation targets and retinopathy of prematurity in extremely preterm infants. Pediatr Res. 2016;80:401–6.
Shukla A, Sonnie C, Worley S, Sharma A, Howard D, Moore J, et al. Comparison of biphasic vs static oxygen saturation targets among infants with retinopathy of prematurity. JAMA Ophthalmol. 2019;137:417–23.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Chan RVP, Berrocal A, et al. International classification of retinopathy of prematurity. Ophthalmology. 2021;128:e51–68.
Bortea CL, Stoica F, Boia M, laco ER, Dinu M, lacob R, et al. Risk factors associated with retinopathy of prematurity in very and extremely preterm infants. Med. 2021;57:420.
de las Rivas Ramírez N, Luque Aranda G, Rius Díaz F. Pérez Frías FJ, Sánchez Tamayo T. Risk factors associated with retinopathy of Prematurity development and progression. Sci Rep. 2022;12:21977.
Chang JW. Risk factor analysis for the development and progression of retinopathy of prematurity. PLoS ONE. 2019;14:e0219934.
Benaron DA, Benitz WE. Maximizing the stability of oxygen delivered via nasal cannula. Arch Pediatr Adolesc Med. 1994;148:294–300.
Vain NE, Prudent LM, Stevens DP, Weeter MM, Maisels MJ. Regulation of oxygen concentration delivered to infants via nasal cannulas. Am J Dis Child. 1989;143:1458–60.
Walsh M, Engle W, Laptook A, Kazzi SNJ, Buchter S, Rasmussen M, et al. Oxygen delivery thorugh nasal cannulae to preterm infants: can practice be improved? Pediatrics. 2005;116(4):857–61.
Filippi L, Cammalleri M, Amato R, Ciantelli M, Pini A, Bagnoli P, et al. Decoupling oxygen tension from retinal vascularization as a new perspective for management of retinopathy of prematurity. New opportunities from β-adrenoceptors. Front Pharmacol. 2022;13:835771.
David L, Hallberg B, Hansen-Pupp I, Dani C, Ramenghi LA, Marlow N, et al. rhIGF-1/rhIGFBP-3 in preterm infants: a phase 2 randomized controlled trial. J Pediatr. 2019;206:56–65.
Acknowledgements
Not applicable.
Funding
This research was supported and funded by SNUH Lee Kun-hee Child Cancer & Rare Disease Project, Republic of Korea (grant number: 23 C-014-0000). The funders of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to publish.
Author information
Authors and Affiliations
Contributions
HJC, SHS, EKK and HSK contributed to the study’s conception and design. Data collection and analysis were performed by HJC, BSS and SHS. The first draft of the manuscript was written by HJC and SHS. All co-authors commented and reviewed the revised manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Seoul National University Hospital (approval number: H-2210-131-1372) and was performed in line with the principles of the Declaration of Helsinki (7th revision, 2013).
The requirement for informed consent was waived due to the retrospective study design.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choi, H.J., Shin, B.S., Shin, S.H. et al. Critical period of oxygen supplementation and invasive ventilation: implications for severe retinopathy of prematurity. Ital J Pediatr 50, 58 (2024). https://doi.org/10.1186/s13052-024-01629-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-024-01629-6