Abstract
Background
Ophthalmia neonatorum is an acute conjunctivitis that occurs in newborns within the first month of life. The most serious infections are due to Chlamydia trachomatis and Neisseria gonorrhoeae, that may cause permanent damages. The use of ophthalmic prophylaxis varies widely around the world, according to the different health and socio-economic contexts. To date in Italy there is no a clear legislation regarding ophthalmia neonatorum prophylaxis at birth.
Methods
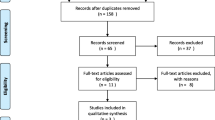
We invited all birth centers in Italy to carry out a retrospective survey relating the last three years. We collected data regarding demographics of neonates, drugs used for ophthalmic prophylaxis and results of the screening of pregnant women for Chlamydia trachomatis and Neisseria gonorrhoeae vaginal infections.
Results
Among 419 birth centers, 302 (72,1%) responded to the survey. Overall 1041384 neonates, 82,3% of those born in the three years considered, received ophthalmic prophylaxis. Only 4,585 (0,4%) of them received one of the drugs recommended by the WHO. The Centers that participated to the survey reported 12 episodes of Chlamydial conjunctivitis and no Gonococcal infection in the three years. Only 38% of the Centers performed vaginal swabs to pregnant women: 2,6% screened only for Neisseria, 9,6% only for Chlamydia and 25,8% for both germs.
Conclusions
The data obtained from the survey showed a low incidence of neonatal conjunctivitis due to either Neisseria gonorrhoeae or Chlamydia trachomatis in Italy. Due to the lack of legislation regulating the prophylaxis of ophthalmia neonatorum in newborns, the Italian Society of Neonatology, the Italian Society of Obstetrics and Gynecology and the Italian Society of Perinatal Medicine have recently issued new recommendations on this topic.
Similar content being viewed by others
Background
Ophthalmia neonatorum (ON) is an acute conjunctivitis that occurs in newborns within the first month of life [1,2,3]. Originally this term only referred to cases caused by Neisseria gonorrhoeae, but currently it includes any conjunctivitis in this age group. Neisseria gonorrhoeae and Chlamydia trachomatis cause the most serious infections, with possible severe complications such as corneal ulceration, corneal perforation or permanent blindness. Neisseria gonorrhoeae conjunctivitis now accounts for less than 1% of reported cases of ON in the United States, while Chlamydia trachomatis infections ranges from 2 to 40%. Other bacteria such as Staphylococcus, Streptococcus, Hemophilus and some Gram-negative bacteria account for 30% to 50% of cases [2]. The epidemiology of ON due to Neisseria gonorrhoeae dramatically decreased in Germany, from 10 to 0,3% [4], after Carl Siegmund Franz Credè (1819–1892) introduced, in the late nineteenth century, the prophylaxis with 2% silver nitrate solution instilled in the conjunctiva of newborns, to prevent the gonococcal conjunctivitis [5]. Before this procedure Neisseria gonorrhoeae was the primary cause of neonatal blindness (60–73%) in Germany [6]. Subsequently, the practice of topical prophylaxis with 2% silver nitrate spread rapidly around the world.
The worldwide incidence of gonococcal conjunctivitis currently varies from 2 to 23%. This variability depends on the specific socio-economic context and on the level of maternal and prenatal care [7]. In the United States, from 2013 to 2017, the estimated incidence of gonococcal conjunctivitis was 0,4 cases/100 000 live births per year [8, 9] while that of chlamydial conjunctivitis was 2,1/100 000 live births per year [9]. Unfortunately, the cases of neonatal conjunctivitis due to Neisseria gonorrhoeae or Chlamydia trachomatis in Italy are not reported by the national surveillance system of the Italian Institute of Health; therefore, there are no available data on the incidence of these infections in Italian newborns.
Both Neisseria gonorrhoeae and Chlamydia trachomatis infections are contracted during childbirth by the contact of newborn with the infected endocervical secretions. The neonate born to an infected mother has a 30% to 50% chance to develop conjunctivitis [10]. Untreated or inappropriately treated gonococcal conjunctivitis may result in corneal perforation and vision loss in less than 24 hours [11]. Untreated Chlamydial conjunctivitis can be associated with corneal and conjunctival scarring, hemorrhagic conjunctivitis, and rarely, loss of vision [12,13,14].
Due to the potential complications related to gonococcal and chlamydial conjunctivitis in newborns, the World Health Organization (WHO) guidelines [15] recommend topical ophthalmic prophylaxis for all newborns, immediately after birth, with one of the following treatments:
-
Tetracycline hydrochloride 1% eye ointment;
-
Erythromycin 0,5% eye ointment;
-
Povidone iodine 2,5% solution (water-based);
-
Silver nitrate 1% solution;
-
Chloramphenicol 1% eye ointment.
To date in Italy the area of ON and its prophylaxis shows several gaps of knowledge and inconsistencies in practice and management.
First, prophylaxis is not regulated by any national legislation, since the old law of 1940, which established its obligation, has been repealed and never updated.
Second, no nationwide, recent data regarding frequency of use and type of ophthalmic prophylaxis at birth in Italy are available.
Third, we lack epidemiological data on the actual incidence of ON in neonates in Italy.
In order to address these pending questions, we conducted a nationwide questionnaire survey, to collect data regarding the prophylaxis of ON, the type of antibiotics used and the frequency of the screening for Chlamydia trachomatis and Neisseria gonorrhoeae vaginal infections in pregnant women in Italy, as well as the actual incidence of ON in the nurseries.
Methods
Design and settings
In 2021 a questionnaire in electronic format was sent to all birth centers in Italy with the questions showed in the Table 1. The questionnaire sent out requests data on all infants born in each center between 1st of January 2018 and 31st of December 2020. Responding Centers were divided according to the Italian Ministry of Health’s instructions regarding the number of assisted births per year [16] in four different groups: centers assisting less than 500 births/year, between 500 to 999 births/year, between 1000 to 2499 births/year and more than 2500 births/year.
Participants and study procedures
The following data were collected on each birth centers: number of births between 1st of January 2018 and 31st of December 2020, performance of eye prophylaxis, drug administered, type of packaging, number of ON cases in the same three-year period, maternal data on screening for Chlamydia trachomatis and/or Neisseria gonorrhoeae performed during pregnancy. Chlamydial or gonococcal ON were defined to assure consistency among sites. ON is defined as conjunctivitis occurring within the first 4 weeks after birth. Gonococcal ON has an incubation period of 2–5 days, with ocular swab positive for Neisseria gonorrhoeae. Chlamydial ON has an incubation period of 5–12 days with ocular swab positive for Chlamydia trachomatis [17]. In addition, information was obtained on the geographic location of the birth centers.
Data sources
Information on how respondents are recruited to SurveyMonkey is available here: http://www.surveymonkey.com/mp/audience. A neonatologist from each department anonymously entered the answers to the questions. All data were anonymized. The answers to the questions were only available to persons appointed as data processors. Those who answered the questions could only view the answers from their own hospital. Although we were not able to perform external data validation at each site, procedures were implemented to minimize data entry errors.
Statistical analysis
Data are presented as descriptive analysis, means and proportions, and have been processed by Microsoft Excel version 16.68 for Mac.
Ethics statement
In Italy, approval by the ethics committee is not required in surveys that do not require specific data of each patient, completed by medical staff.
Funding source
This study did not receive any funding.
Results
Demographics
In 2021, all Italian birth Centers were approached and sent the questionnaire. Some 72% of them took the survey [302/419: 137/ 173 (79,2%) in Northern, 63/89 (70,8%) in Central and 102/157 (65%) in Southern Italy]. Among the centers assisting less than 500 births/year, 50/103 (48,5%) answered to the survey, among those assisting between 500 to 999 births/year 123/170 (72,3%) centers answered, among those assisting between 1000 to 2499 births/year 112/127 (88,2%) centers answered and those assisting more than 2500 births year 17/19 (89,5%). We did not observe any difference in terms of adherence to the survey between centers of North, Centre, and South of Italy nor between regions. Figure 1 and Table 2 show the distribution of the results clustered by Italian Regions.
Ophthalmic prophylaxis
During the study period all neonates born in the centers participating to the survey (which correspond to 82,3% of total births in Italy in the same period [18,19,20]) underwent ophthalmic antibiotic prophylaxis. Newborns who received one of the drugs recommended by the WHO (povidone iodine 2,5% solution) were 4585/1041384 (0,4%). Chloramphenicol and tetracycline were administered to 37095/1041384 (3,6%) and to 46193/1041384 (4,4%) of newborns, respectively, but as topical antibiotic solution, combined with other drugs and not as eye ointment, as recommended by the WHO. Topical tobramycin was administered in 474418/1041384 (45,6%) newborns and gentamycin in 202937/1041384 (19,5%).
The WHO recommendation invites to use a single-use antibiotic ointment. The medications used for prophylaxis of the Italian newborns included in the survey were in double antibiotic solution, in multi-use packaging and not prepared as single-use antibiotic ointment (Fig. 2). Therefore, 1036799/1041384 newborns (99,6%) received a suboptimal ophthalmic prophylaxis. Figure 3 shows the drugs used for the prophylaxis in our cohort of newborns.
Ophthalmia neonatorum
Overall, 12 cases of Chlamydia trachomatis conjunctivitis were reported (incidence rate 0,001%), all occurring in only six neonatal units (2%) out of 302 participating to the survey reported Neisseria gonorrhoeae infection was never reported.
Pregnancy data
One hundred and fifteen centers (39,5%) performed screening of sexually transmitted diseases via vaginal swabs: 8 (2,7%) centers for gonococcal infections, 29 (10%) for chlamydial infections and 78 (26,8%) for both germs (Fig. 4).
Discussion
In Italy there is no clear legislation regarding ophthalmia neonatorum prophylaxis at birth. The law regulating the administration of antibiotic prophylaxis to newborns at birth dates back to 1940 [21] and has been repealed in 1975 [22]. Despite this gap in legislation on this subject, the administration of conjunctival antibiotics to newborns in Italy is still routinely carried out in all birth centers.
In Italy, the National Surveillance System of the National Health Institute does not collect data on the incidence of chlamydial or gonococcal conjunctivitis in the neonatal period. The data from our national survey shed a light on the incidence of neonatal conjunctivitis and on the current prophylactic practices in Italy, at the same time underpinning an urgent need to update the Italian scientific societies’ recommendations regarding the administration of ophthalmic prophylaxis.
It is somewhat concerning that in Italy 99,6% of all newborns did not receive at birth the ophthalmic prophylaxis according to WHO recommendations, despite an extremely wide use of ophthalmic prophylaxis. Although this clear inconsistency, no cases of gonococcal and very few cases of chlamydial conjunctivitis in newborns have been reported period of the study. These low incidences of conjunctivitis recorded by our survey may be a limitation of our report. However, it must be considered that a high number of birth points participated in our survey, in most of which infants are followed up for routine checkups even after discharge. This allows the identification of conjunctivitis at least in the first 10 days of life. In addition, the severe conjunctivitis may require hospitalization, and in Italy all infants must be admitted to Neonatal Units. Surely, more complete data would have been obtained by involving all primary care pediatricians and all pediatric ophthalmology units; in contrast, we would have had a lower survey participation rate.
Several European countries no longer administer universal ocular prophylaxis but recommend the screening and treatment of sexually transmitted diseases in pregnant women at high risk. The Canadian Pediatric Society does not recommend universal prophylaxis with erythromycin but promote epidemiological investigations to estimate the incidence of ON [23]. However, in countries where ophthalmic antibiotic prophylaxis is still performed, there is no agreement on which drugs to use. In the United States, only the 0,5% erythromycin ophthalmic ointment is available among the drugs recommended by the WHO. Other medications, such as tetracycline ophthalmic ointment and silver nitrate, are no longer available and gentamicin was reported as responsible for chemical conjunctivitis [24]. In Brazil, the use of povidone iodine 2,5%, erythromycin 0,5%, tetracycline 1%, or silver nitrate 1% is recommended as rescue [25], in Chile chloramphenicol 0,5% or erythromycin 0,5% are used [26], and in Spain ophthalmic prophylaxis with erythromycin 0,5% or tetracycline 1% ointment is performed only in newborns delivered by vaginal route [27]. Whichever the antibiotic chosen, it is mandatory to use preparations with a single active ingredient. Furthermore, it is necessary to administer the drug exclusively using a single-dose package, to prevent any spread of conjunctival infections and to allow proper storage of the drug.
To prevent ON, the Center for Disease Control and Prevention (CDC), recommends that all pregnant women with risk factors for sexually transmitted diseases and their partners should be screened for Neisseria gonorrhoeae at the first prenatal visit [28]. Pregnant women who remain at high risk for gonococcal and chlamydial infection should be tested again during the third trimester to prevent maternal postnatal complications and a gonococcal infection in the neonate [29].
Conclusion
In the light of the above mentioned evidence, and taking into account the scenario that our data have disclosed, the low incidence in Italy of neonatal conjunctivitis from Chlamydia trachomatis and Neisseria gonorrhoeae, and the current national shortage of drugs recommended by the CDC and the WHO, the Italian Society of Neonatology (SIN), the Italian Society of Gynecology and Obstetrics (SIGO) and the Italian Society of Perinatal Medicine (SIMP), have deemed necessary to issue a position statement [30], with the aim of providing shared indications for the best and appropriate preventive approach of neonatal conjunctivitis contracted during delivery, thus overcoming the absence of a specific regulation on the mandatory nature of ocular prophylaxis in the newborn.
The two objectives of the position statement are the following:
-
1.
To standardize the prophylactic procedures throughout Italy, at the same time assessing the actual need to perform ophthalmic prophylaxis to all birth cohorts based on the data coming from Italian birth centers
-
2.
To avoid administering useless antibiotics to infants, which may be in turn harmful when used without a precise indication.
For this initiative to be successful, it is essential to have a multidisciplinary approach, with the obstetrical, neonatological and nursing staff working together to have primary prevention activities to be started from the earliest stages of pregnancy.
The Intersociety document does not recommend anymore the administration of the ophthalmic antibiotic prophylaxis at birth to all newborns, but only to neonates born from unattended pregnancies (defined as less than three visits performed during pregnancy) or unscreened pregnant women at risk for sexually transmitted diseases. Neonates requiring ophthalmic prophylaxis should receive immediately after birth, either 0,5% erythromycin or 1% tetracycline or 1% chloramphenicol ophthalmic ointment.
Moreover, a vulvovaginal swab for Neisseria gonorrhoeae and Chlamydia trachomatis is recommended for all pregnant women at risk for sexually transmitted diseases at the first prenatal care visit. The document recommends against administering ophthalmic antibiotic prophylaxis at birth to neonates born from a mother with a vaginal swab positive for Chlamydia trachomatis regardless of treatment during pregnancy or with a vaginal swab positive for Neisseria gonorrhoeae, but adequately treated during pregnancy.
Finally, symptomatic neonates born to a mother positive for Chlamydia trachomatis, regardless of treatment during pregnancy, and asymptomatic/symptomatic neonates born to a mother positive for Neisseria gonorrhoeae not treated or inadequately treated during pregnancy should be treated with systemic antibiotic therapy.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ON:
-
Ophthalmia neonatorum
- WHO:
-
World health organization
- CDC:
-
Center for disease control and prevention
- SIN:
-
Italian society of neonatology
- SIGO:
-
Italian society of gynecology and obstetrics
- SIMP:
-
Italian society of perinatal medicine
References
Zar HJ. Neonatal chlamydial infections: prevention and treatment. Paediatr Drugs. 2005;7:103–10.
Pickering LK, Baker CJ, Kimberlin DW, Long SS. American academy of pediatrics. Prevention of neonatal ophthalmia. In: Red Book: 2012 report of the committee on infectious disease. 29th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012. p. 880–2.
Normann EK, Bakken O, Peltola J, et al. Treatment of acute neonatal bacterial conjunctivitis: a comparison of fucidic acid to chloramphenicol eye drops. Acta Ophthalmol Scand. 2002;80:183–7.
Woods CR. Gonococcal infections in neonates and young children. Semin Pediatr Infect Dis. 2005;16:258–70.
Credè CSF. Die Verhutung der augenentzundung bei Neugeborenen, der haufigsten und wichtigsten Urasche der Blindheit, 63 ppA Hirschwald, Berlin, 1984. Based on a translation by H. Thomas. Surv Ophthalmol. 1963;4:367–70.
Zuppa AA, D’Andrea V, Catenazzi P, Scorrano A, Romagnoli C. Ophthalmia neonatorum: what kind of prophylaxis? J Matern-Fetal Neonatal Med. 2011;24:769–73.
Boadi-Kusi SB, Kyei S, Holdbrook S, Abu EK, Ntow J, Ateko AM. A study of ophthalmia neonatorum in the Central Reion of Ghana: causative agents and antibiotic susceptibility patterns. Glob Pediatr Health. 2021;8:2333794X211019700.
Guirguis-Blake JM, Evans CV, Rushkin M. ocular prophylaxis for gonococcal ophthalmia neonatorum: updated evidence report and systematic review for the US preventive services task force. JAMA. 2019;321:404–46.
Kreisel K, Weston E, Braxton J, Llata E, Torrone E. keeping an eye on chlamydia and gonorrhea conjunctivitis in infants in the United States, 2010–2015. Sex Transm Dis. 2017;44:356–8.
Laga M, Naamara W, Brunham RC. Single-dose therapy of gonococcal ophthalmia neonatorum with ceftriaxone. N Engl J Med. 1986;315:1382–5.
Donham BP, Gibler WB. Images in emergency medicine Gonococcal conjunctivitis. Ann Emerg Med. 2008;52:11–6.
Chang K, Cheng VYW, Kwong NS. Neonatal haemorrhagic conjunctivitis: a specific sign of chlamydial infection. Hong Kong Med J. 2006;12:27–32.
Darville T. Chlamydia trachomatis infections in neonates and young children. Semin Pediatr Infect Dis. 2005;16:235–44.
Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–21.
WHO. Guidelines for the Treatment of Neisseria gonorrhoeae. Geneva: World Health Organization. (WHO Guidelines Approved by the Guidelines Review Committee); 2016. Available from: http://www.ncbi.nlm.nih.gov/books/NBK379221/. Accessed on 22 Oct 2022.
Tavole Certificato di assistenza al parto (CeDAP). Anno 2020. Available from: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3149_0_alleg.xlsx. Accessed on 22 Sept 2022.
Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH. Neonatal ophthalmia. In: Red Book (2021): report of the committee on infectious diseases. 32nd ed. Itasca, IL: American Academy of Pediatrics; 2021. p. 1023–6.
Natalità e fecondità della popolazione residente. Anno 2018. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjM_dfx99_5AhWFOHoKHYXTBoIQFnoECAQQAw&url=https%3A%2F%2Fwww.istat.it%2Fit%2Ffiles%2F2019%2F11%2FReport_natalit%25C3%25A0_anno2018_def.pdf&usg=AOvVaw0X2xf9nApNwDSot5irEfhy. Accessed on 22 Sept 2022.
Natalità e fecondità della popolazione residente. Anno 2019. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj6mvrZ99_5AhVAQ_EDHVrjDh4QFnoECAYQAQ&url=https%3A%2F%2Fwww.istat.it%2Fit%2Ffiles%2F2020%2F12%2FREPORT-NATALITA-2019.pdf&usg=AOvVaw1VDsXtwF57vH2hp314VAWo. Accessed on 22 Sept 2022.
Natalità e fecondità della popolazione residente. ANN0 2020. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiwko2z99_5AhXaVfEDHcogDDUQFnoECAUQAw&url=https%3A%2F%2Fwww.istat.it%2Fit%2Ffiles%2F2021%2F12%2FREPORT-NATALITA-2020.pdf&usg=AOvVaw0bjFmTIt8JAmqXswZ3_SEf. Accessed on 22 Sept 2022.
Gazzetta Ufficiale del Regno d’Italia, n. 249, 23-X-1940, XVIII, Decreto ministeriale 11 Ottobre 1940-XVIII. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwibsbCVx-H5AhWD8LsIHcMSDM8QFnoECAoQAQ&url=http%3A%2F%2Fwww.gazzettaufficiale.it%2Feli%2Fgu%2F1940%2F10%2F23%2F249%2Fsg%2Fpdf&usg=AOvVaw1BC9fIsy4o-SNbAZdq6h58. Accessed on 13 Sept 2022.
Gazzetta Ufficiale della Repubblica Italiana, n. 147, 6 -VI – 1975, Decreto del Presidente della Repubblica 7 Marzo 1975, n. 163. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj22qCvyOH5AhVuhf0HHXjmB2cQFnoECA0QAQ&url=http%3A%2F%2Fwww.gazzettaufficiale.it%2Feli%2Fgu%2F1976%2F03%2F22%2F75%2Fsg%2Fpdf&usg=AOvVaw0jHHJNNz7frHHiSIrOwKJ. Accessed on 13 Sept 2022.
Moore DL, MacDonald NE. Canadian paediatric society, infectious diseases and immunization committee preventing ophthalmia neonatorum. Paediatr Child Health. 2015;20:93–6.
US Preventive Services Task Force, Curry SJ, Krist AH, et al. Ocular prophylaxis for gonococcal ophthalmia neonatorum: US preventive services task force reaffirmation recommendation statement. JAMA. 2019;321:394–8.
Departamento Científico de Neonatologia – Sociedade Brasileira de Pediatria. profilaxia da conjuntivite neonatal: novas diretrizes da sociedade brasileira de pediatria. 2020. Available from: https://www.sbp.com.br/imprensa/detalhe/nid/profilaxia-da-oftalmia-neonatal-por-transmissao-vertical. Accessed on 23 Oct 2022.
Consultivo de Infecciones Neonatales, Sociedad Chilena de Infectología. Rationale of ocular prophylaxis of neonatal ophtalmia in the newborn infant. Rev Chil Infectol. 2017;34:257–8.
Ministerio de sanidad, servicios sociales e igualdad Spain. Guía de práctica clínica de atención en el embarazo y puerperio. Available from: http://portal.guiasalud.es/completa-pdf/. Accessed on 23 Oct 2022.
LeFevre ML, U.S. Preventive Services Task Force. Screening for Chlamydia and gonorrhea: U.S. Preventive services task force recommendation statement. Ann Intern Med. 2014;161:902–10.
Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1–184.
Profilassi della Ophthalmia neonatorum. Raccomandazioni sulla procedura della profilassi della Ophthalmia neonatorum in Italia: documento congiunto SIN-SIGO-SIMP. Available from: https://www.sin-neonatologia.it/wp-content/uploads/2022/11/Profilassi-della-Ophthalmia-neonatorum.pdf. Accessed on 21 Nov 2022.
Acknowledgements
List of the neonatal units responding to the survey: Vincenzo Zanardo, Policlinico di Abano Terme (Abano Terme); Giuseppina De Luca, Casa di cura Villa dei Fiori (Acerra); Pinella Di Stefano, PO S. Maria e S. Venera (Acireale); Giovanni Latorre, Ospedale Generale Regionale “F. Miulli” (Acquaviva delle Fonti); Simone Rugolotto, Santa Maria degli Angeli (Adria); Francesco Ciccullo, Istituto Clinico Mediterraneo (Agropoli); Federico Schena, Azienda Ospedaliera Santi Antonio e Biagio e Cesare Arrigo (Alessandria); Maria Giovanna Mirizzi, Ospedale della Nurgia Fabio Pirenei (Altamura); Cesare Antonio Ghitti, Ospedale Pesenti Fenaroli (Alzano Lombardo); Paolo Serravale, Ospedale Beuregard (Aosta); Giovanni Testa, Casa di Cura Città di Aprilia (Aprilia); Flavio Civitelli, Ospedale San Donato (Arezzo) e Ospedali Riuniti Valdichiana Sudest (Montepulciano); Patrizia Tedesco, PO Sant’Ottone Frangipane (Ariano Irpino); Maragliano Giovanna, Ospedale dei Castelli (Ariccia); Ermanno Ruffini, Area Vasta 5 ASUR Marche (Ascoli Piceno, San Benedetto del Tronto); Mariachiara Strozzi, Presidio Ospedaliero Cardinal Massai (Asti); Angelo Izzo, casa di Cura Malzoni-Villa Platani (Avellino); Sabino Moschella, AORN San Giuseppe Moscati (Avellino); Nicola Laforgia, AOUC Policlinico di Bari (Bari); Gabriele D’Amato, Ospedale Di Venere (Bari); Giulio Paganetti, Mater Dei Hospital (Bari); Ferdinando Chiorazzo, Ospedale Monsignor Dimiccioli (Barletta); Laura Ghiro, Ospedale San Bassiano (Bassano del Grappa); Domenico Cortazzo, Ospedale Santa Maria della Speranza (Battipaglia); Raffaele Rabauno, Ospedale Sacro Cuore del Gesù-Fatebenefratelli (Benevento); Francesco Cocca, Azienda Ospedaliera San Pio (Benevento); Maurizio Giozani, ASST Papa Giovanni XXIII (Bergamo); Graziella Portale, Ospedale Maria SS. Addolorata (Biancavilla); Paolo Manzoni, Ospedale degli Infermi (Biella); Fabrizio Sandri, Ospedale Maggiore (Bologna); Luigi Tommaso Corvaglia, Policlinico Sant’ Orsola (Bologna); Alex Staffler, Ospedale di Bolzano (Bolzano); Oscar Nis Haitink, Presidio Ospedaliero di Borgomanero (Borgomanero); Gianluca Cosi, Ospedale di Borgosesia (Borgosesia) e Ospedale S. Andrea (Vercelli); Francesca Maria Risso, Spedali Civili (Brescia); Ibrahim Hazi, Istituto Sant’Anna (Brescia); Paolo Ernesto Villani, Fondazione Poliambulanza (Brescia); Markus Markat, Ospedale di Bressanone (Bressanone); Placido Pennisi, Ospedale Castiglione Prestianni (Bronte); Waldurga Cassar, Ospedale di Brunico (Brunico); Simonetta Cherubini, AO Busto Arsizio (busto Arsizio); Elisabetta Piu, SS Trinità (Cagliari); Luciana Pibiri, AO Brotzu (Cagliari); Vassilios Fanos, AOU Cagliari (Cagliari); Rosario Caci, ASP Caltanissetta (Caltanissetta); Luigi Gagliardi, Ospedale Versilia (Camaiore); Vincenzo Santillo, Ospedale Cardarelli (Campobasso) e Ospedale San Timoteo (Termoli); Luca Vecchiato, Ospedale di Camposampiero (Camposanpiero); Rocco Boncori, PO Canicattì (Canicattì); Luca Ghiacchetti, CdC Villa Fiorita (Capua); Patrizia Calzi, PO Carate Brianza (Carate Brianza); Marco Aicardi, Ospedale Santo Spirito (Casale Monferrato); Italo Bernardo, AO Sant’Anna e San Sebastiano (Caserta); Marilena Raponi, PO Santa Scolastica (Cassino); Lucio Giordano, Pineta Grande Hospital (Castel Volturno); Roberto Cinelli, Ospedale San Leonardo (Castellamare di Stabia); Iolanda Chinellato, Ospedale San Pio (Castellaneta); Maria Rosaria La Bianca, Ospedale Vittorio Emanuele II (Castelvetrano); Riccardo Scudo, Ospedale civile Ferrari (Castrovillari); Pietro D’ Amico, Ospedale Cannizaro (Catania); Vincenzo Di Benedetto, PO Gaspare Rodolico (Catania); Raffaele Falsaperla, PO San Marco (Catania); Giacomo Tornabene, CdC Falcidia (Catania); Gabriella Tina, Azienda Arnas Garigaldi-Nesima (Catania); Maria Lucente, AO Pugliese-Ciaccio (Catanzaro); Massimo Soffiari, PO Cavalese (Cavalese) e Ospedale Valli del noce (Cles) e Ospedale Santa Chiara (Trento); Samuele Giuseppe Gragnani, PO Cecina (Cecina); Vincenzo Miceli, Fondazione Istituto G. Giglio (Cefalù); Stella Marcello, Ospedale M Bufalini (Cesena); Michele Spandrio, Azienda Socio Sanitaria della Franciacorta (Chiari); Gian Maria Terragni, Ospedale Maggiore (Chieri), Fabio Stefano Timeus, Ospedale di Chivasso (Chivasso); Adalberto Brach del Prever, Presidio Ospedaliero di Ciriè (Ciriè); Rosanna Golin, Ospedale di Cittadella (Cittadella); Enrica Fabrizi, Ospedale di Civitanova Marche (Civitanova Marche); Francesco Di Turi, PO San Paolo (Civitavecchia); Daniele Merazzi, Ospedale Valduce (Como); Gian Paolo Chiaffoni, Ospedale di Conegliano (Conegliano); Giovanni Pompeo Ciccarone, Ospedale Umberto I (Corato); Francesco Milillo, Ospedale Guido Compagna (Corigliano Calabro); Gianfranco Scarpelli, AO di Cosenza (Cosenza); Salvatore Savasta, Ospedale Maggiore (Crema); Antonio Belcastro, Ospedale Civile San Giovanni di Dio (Crotone); Andrea Sannia, AO S. Croce e Carle (Cuneo); Donatella Cattarelli, Ospedale di Desenzano del Garda (Desenzano del Garda) e Ospedale Gavardo “La Memoria” (Gavardo); Tiziana Varisco, PO di Desio (Desio); Andrea Guala, Ospedale San Biagio (Domodossola) e Ospedale Castelli (Verbania); Sabrina Morreale, PO Umberto I (Enna); Fabio Focarile, Ospedale “Sacra Famiglia” Fatebenefratelli (Erba); Simona La Placa, Ospedale Sant Antonio Abate (Erice); Dario Magnini, PO Esine-Edolo (Esine); Stefano Marzini, PO “Santa Maria del Prato” (Feltre); Luisa Pieragostini, Ospedale Augusto Murri (Fermo); Agostina Solinas, Arcispedale Sant’Anna (Ferrara); Pier Luigi Bacchini, Ospedale di Fidenza (Fidenza); Carlo Dani, AOU Careggi (Firenze); Marco Pezzati, Ospedale San Giovanni di Dio (Firenze); Gianfranco Maffei, AOU Ospedali Riuniti (Foggia); Beatrice Messini, Nuovo Ospedale San Giovanni Battista (Foligno); Biagio De Mitri, Ospedale Dario Camberlingo (Francavilla Fontana); Giuseppe De Luca, Ospedale Civile San Giovanni di Dio (Frattamaggiore); Achille Campoli, Ospedale Fabrizio Spaziani (Frosinone); Raffaele Montinaro, Ospedale Santa Caterina Novella (Galatina); Marco Antonio Nedbal, Ospedale S. Antonio Abate (Gallarate); Salvatore Barberi, PO Gabernate Milanese (Gabernate Milanese) e ASST Rho (Rho); Cesare Arioni, Ospedale Policlinico San Martino (Genova); Massimo Mazzella, EO Ospedali Galliera (Genova); Stefano Macciò, Ospedale Villa Scassi (Genova); Paolo Adamoli, Ospedale Generale di zona Moriggia Pelascini (Gravedona ed Uniti); Susanna Falorni, Ospedale Misericordia (Grosseto); Ciro Clemente, PO CTO (Iglesias); Laura Serra, Ospedale Santa Maria delle Scalette (Imola); Giuseppina Bontempo, Ospedale Civile Ferdinando Veneziale (Isernia); Affif Barbara, Ospedale id Ivrea (Ivrea); Sandra Di Fabio, Ospedale San Salvatore (L’Aquila); Maria Franca Corona, Ospedale Sant’ Andrea (La Spezia); Nicola Di Lascio, Ospedale di Lagonegro (Lagonegro); Rossella Galliano, Ospedale Giovanni Paolo II (Lamezia Terme); Fabio Pace, Ospedale Civile Floraspe Renzetti (Lanciano); Fabio Narducci, Ospedale Nostra Signora della Mercede (Lanusei); Riccardo Lubrano, Ospedale Santa Maria Goretti (Latina); Giuseppe Presta, Ospedale Vito Fazzi (Lecce); Roberto Bellù, PO Alessandro Manzoni (Lecco) e PO di Merate (Merate); Federico Zaglia, Ospedale Nuovo di Legnano (Legnano); Giuseppe Gramaglia, PO di Licata (Licata); Roberto Danieli, Spedali Riunito (Livorno); Musolino Antonio, Ospedale di Locri (Locri); Roberta Giacchero, Ospedale Maggiore di Lodi (Lodi); Angelina Vaccaro, Ospedale San Luca (Lucca); Paolo Francesco Perri, Ospedale di Macerata—Generale Provinciale (Macerata); Bellini Marta, Ospedale di Magenta (Magenta); Giovanna Sassi, Ospedale di Manebrio (Manebrio); Valeria Angela Fasolato, Ospedale Carlo Poma (Mantova); Franco Mastro, PO “Valle d’Itria” (Martina Franca); Graziano Memmini, Ospedale Apuane (Massa Carrara); Giovanna Liguoro, CdC Nostra Signora di Lourdes (Massa di Somma); Fabio Rocco, PO “Madonna delle Grazie” (Matera); Antonino Moceri, Ospedale Abate Ajello (Mazara del Vallo); Giovanni Traina, Ospedale “Santa Maria delle Stelle” (Melzo); Gaia Weissman, Ospedale di Merano (Merano); Eloisa Gitto, AOU Gaetano Martino (Messina); Angelo D’Anieri, PO Papardo (Messina); Graziano Barera, IRCCS Ospedale San Raffaele (Milano); Gianluca Lista, Ospedale dei bambini “Vittore Buzzi” (Milano); Fabrizio Ciralli, Ospedale Humanitas San Pio X (Milano); Luca Bernardo, Ospedale Fatebenefratelli e Oftalmico (Milano); Fabio Mosca, Fondazione IRCCS Ca’ Grande (Milano); Claudio Migliori, Ospedale San Giuseppe (Milano); Stefano Martinelli, Ospedale Niguarda (Milano); Alberto Fabio Podestà, Ospedale San Carlo Borromeo (Milano); Giuseppe Banderali, Ospedale Santi Paolo e Carlo (Milano); Franco Cusumano, Ospedale Fogliani (Milazzo); Massimiliano De Bortoli, Ospedale di Mirano (Mirano); Bruno Mordini, AOU Policlinico di Modena (Modena); Ferdinando Zocco, PO Maggiore (Modica); Antonella Travierso, Ospedale Moncalieri (Moncalieri); Patrizia Fusco, Ospedale Regina Montis Regalis (Mondovì); Danica Dragovic, Ospedale San Polo (Monfalcone); Ignazio Lofù, Ospedale San Giacomo (Monopoli); Virginia Carlini, Ospedali Riuniti Padova Sud (Monselice); Debora Corazzin, Ospedale San Valentino (Montebelluna); Luca Tafi, Ospedale La Gruccia (Montevarchi); Maria Luisa Ventura, Ospedale San Gerardo (Monza); Fabrizio Stoecklin, CdC Ospedale Internazionale (Napoli); Francesco Raimondi, AOU Federico II (Napoli); Donato Zappulli, Ospedale Fetebenefratelli (Napoli); Cinzia Maria Montemarano, PO San Giovanni Bosco (Napoli); Marcello Napolitano, Ospedale Evangelico Villa Betania (Napoli); Maria Gabriella De Luca, AO Antonio Cardarelli (Napoli); Antonio Deganello, IRCCS Sacro Cuore Don Calabria (Negrar di Valpolicella); Giuseppa Di Costa, Ospedale Carlo Basilotta (Nicosia); Ignazio Franzese, PO Umberto I (Nocera Inferiore); Vincenzo Riccardi, PO Santa Maria della Pietà (Nola); Ivana Rabbone, AOU Maggiore della Carità (Novara); Flaminia Torelli, Ospedale San Giacomo (Novi Ligure); Angela Taraschi, Ospedale di Oderzo (Oderzo); Augusto Masia, Ospedale Giovanni Paolo II (Olbia); Enrica Paderi, Ospedale San Martino (Oristano); Elena Neri, Ospedale Santa Maria della Stella (Orvieto); Beatrice Dalla Barba, Dipartimento della Salute della Donna e del Bambino (Padova); Emilia Occhipinti, CdC Triolo Zancla (Palermo); Giorgio Sulliotti, AO Ospedali Riuniti Villa Sofia—Cervello (Palermo); Marcello Vitaliti, PO Civico Di Cristina Benfratelli (Palermo); Mario Giuffrè, Policlinico Giaccone (Palermo); Giovanni Muscolino, CdC Villa Serena (Palermo); Vincenzo Duca, PO “G.F. Ingrassia” (Palermo); Giampiero Pinna, Ospedale Buccheri La Ferla – Fatebenefratelli (Palermo); Maria Rosa Cinquegrani, CdC Candela (Palermo); Serafina Perrone, Ospedale dei Bambini “Pietro Barilla” (Parma); Caterina Cacace, Ospedale Barone Romeo (Patti); Lina Bollani, IRCCS Policlinico San Matteo (Pavia); Chryssoula Tzialla, Polo Ospedaliero dell’Oltrepo’ ASST di Pavia (Pavia); Stefania Troiani, Ospedale Santa Maria della Misericordia (Perugia); Monica Santoni, AO Ospedali Riuniti Marche Nord (Pesaro e Fano); Susanna Di Valerio, PO Pescara (Pescara); Alexandre Bidan, Ospedale P. Pederzoli (Peschiera del Garda); Rino Agostiniani, Ospedale SS. Cosma e Damiano (Pescia) e Ospedale San Jacopo (Pistoia); Giacomo Biasucci, Ospedale Guglielmo da Saliceto (Piacenza); Cesare Antonio Ghitti, Ospedale M.O.A. Locatolli (Piario); Marco Nangeroni, Ospedale Agnelli (Pinerolo); Antonio Boldrini, AOU di Pisa (Pisa); Domenico Minasi, Ospedale Santa Maria degli Ungheresi (Polistena); Camillo Lovati, Policlinico San Pietro (Ponte San Pietro); Roberto Dell’ Amico, Ospedale di Pordenone (Pordenone); Stefano Facchin, CdC Policlinico San Giorgio (Pordenone); Teresa Di Fraia, Ospedale Santa Maria delle Grazie (Pozzuoli); Pierluigi Vassari, Ospedale Santo Stefano (Prato); Vincenzo Salvo, Ospedale Giovanni Paolo II (Ragusa); Federico Marchetti, Ospedale Santa Maria delle Croci (Ravenna) e Ospedale degli Infermi (Faenza) e Ospedale Umberto I (Faenza); Isabella Mondello, Ospedali Riuniti Bianchi (Reggio Calabria); Giancarlo Gargano, Arcispedale Santa Maria Nuova (Reggio Emilia); Mauro De Martinis, Ospedale San Camillo de’ Lellis (Rieti); Gina Ancora, Ospedale degli Infermi (Rimini); Franco Garofalo, Ospedale di Rivoli (Rivoli); Maria Giovanna Colella, Ospedale Santo Spirito e Ospedale San Filippo Neri (Roma); Luca Maggio, AO San Camillo—Forlanini (Roma); Cristina Haass, Ospedale Villa San Pietro – Fatebenefratelli (Roma); Camilla Gizzi, Ospedale Sandro Pertini e Ospedale Sant Eugenio (Roma); Piermichele Paolillo, Policlinico Casilino (Roma); Francesco Crescenzi, CdC Santa Famiglia (Roma); Ambrogio Di Paolo, AO San Giovanni—Addolorata (Roma); Gustavo Caoci, CdC Mater Dei (Roma); Giovanni Vento, Policlinico Universitario Agostino Gemelli (Roma); Anna Maria Zingoni, Ospedale Giovan Battista Grassi (Roma); Gianluca Terrin, AOU Policlinico Umberto I (Roma); Cristina Ossicini, Ospedale Madre Giuseppina Vannini (Roma); Maurizio Gente, CdC Quisisana (Roma); Lorenzo Ferrante, Fabia Mater (Roma), Luigi Orfeo, Ospedale Fatebenefratelli Isola Tiberina—Gemelli Isola (Roma); Concetta Maria Alecci, Ospedale Cristo Re (Roma); Ugo Pradal, Ospedale Santa Maria Carmine (Rovereto); Simone Rugolotto, Ospedale Santa Maria della Misericordia (Rovigo); Raffaele Albano, AOU San Giovanni di Dio e Ruggi D’ Aragona (Salerno); Maria Paola Miani, Ospedale di Sant’ Antonio (San Daniele del Friuli) e Ospedale di Tolmezzo (Tolmezzo); Mario Barbarini, Ospedale Sant’Anna (San Fermo della Battaglia); Angelo Maria Iovino, CdC la Madonnina (San Gennaro Vesuviano); Alberto Gatta, Ospedale Casa Sollievo Della Sofferenza (San Giovanni Rotondo); Valentina Moretti, Ospedale Santa Maria dei Battuti (San Vito al Tagliamento); Roberta Pesavento, Ospedale Alto Vicentino (Santorso); Nelson Napolitano, PO dell’ Immacolata (Sapri); Gianluigi Palamone, PO “Villa Malta” (Sarno); Gianpaolo Mirri, Ospedale di Saronno (Saronno); Giorgio Olzai, AOU Sassari (Sassari); Claudio Rota, Ospedale di Sassuolo (Sassuolo); Raffaele Basta, Ospedale SS Annunziata (Savigliano); Alberto Gaiero, Ospedale San Paolo (Savona); Carmelo Perrone, Ospedale “Verris Delli Ponti” (Scorrano); Cristina Bellan, Ospedale Bolognini (Seriate); Aristide Cotta Ramusino, Ospedale Città di Sesto San Giovanni (Sesto San Giovanni); Massimo Tirantello, PO Umberto I (Siracusa); Lorella Rossi, Ospedale Civile (Sondrio) e PO Sondalo (Sondalo); Luigi Di Ruzza, Ospedale SS Trinità (Sora); Carlo Fugini, Ospedale Civile di Broni (Stradella); Massimo Cinque, PO Sulmona (Sulmona); Simone Reali, Ospedale San Vincenzo (Taormina); Lucrezia Decosmo, Ospedale SS Annunziata (Taranto); Franco Di Lollo, Ospedale Sant’Omero (Teramo); Maddalena Allegra, Ospedale San Cimino (Termini Imerese); Maria Elena Pacella, Ospedale di Tivoli (Tivoli); Patrizia Savant Levet, Ospedale Maria Vittoria (Torino); Manlio Mandrino, Ospedale Martini (Torino), Emila Parodi, AO Ordine Mauriziano (Torino); Maria Francesca Campagnoli e Caterina Carbonara, AOU Città della Salute e della Scienza (Torino); Anna Bussolini, Ospedale di Tradate (Tradate); Paolo Menghini, Ospedale Treviglio – Caravaggio (Treviglio); Paola Lago, Ospedale di Treviso (Treviso); Enrico Rosati, Ospedale Cardinale Giovanni Panico (Tricase); Laura Travan, IRCCS Materno Infantile Burlo Garofolo (Trieste); Carla Pittini, Ospedale Santa Maria della Misericordia (Udine); Emanuela Lanfranchi, PO Unico “Santa Maria della Misericordia” (Urbino); Massimo Agosti, Ospedale Filippo Del Ponte (Varese); Massimo Bellettato, Ospedale San Lorenzo (Valdagno); Patrizio Pulicati, Ospedale Velletri (Velletri); Luca Livio Ecclesio, Ospedale dell’Angelo (Venezia); Alessandro Vigo, Ospedale Michele e Pietro Ferrero (Verduno); Salvatore Bragò, PO Jazzolino (Vibo Valentia); Stefania Vedovato, Ospedale San Bortolo (Vicenza); Lidia Decembrino, Ospedale Civile di Vigevano (Vigevano); Marco Sala, Ospedale di Vimercate (Vimercate); Paola Bruni, Ospedale di Vizzolo Pradibassi (Vizzolo Pradibassi).
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
CA, VM, CT and SA conceptualized and designed the study. VM e SL collected the data. VM and CT analyzed the data. VM, CA, FP, PM and CT wrote the first draft of the manuscript. CT as the corresponding author had full access to all the data of the study. VM, CT, SA, DM, SM, GA, LM, GC, LG, MG, FM, IC, VT, HV, NC, LO and CA critically discussed various aspects of the new position statement. All authors have read and approved the final version of the manuscript. All authors had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics committee approval was not required for the type of study. All department heads who responded to the survey gave consent for their responses to be used. All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mondì, V., Tzialla, C., Aversa, S. et al. Antibiotic prophylaxis for ophthalmia neonatorum in Italy: results from a national survey and the Italian intersociety new position statements. Ital J Pediatr 49, 117 (2023). https://doi.org/10.1186/s13052-023-01507-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01507-7