Abstract
Background
Bronchiolitis is a major cause of hospitalization in infants, particularly in the first six months of life, with approximately 60–80% of admissions due to respiratory syncytial virus (RSV) infection. Currently, no prophylactic options are available for healthy infants. The present study aimed at describing the demographic, clinical, and epidemiological characteristics of infants hospitalized for bronchiolitis in the Apulia region of Italy in 2021.
Methods
From January to December 2021, data on children aged 0–12 months admitted for bronchiolitis in nine neonatal or pediatric units covering 61% of pediatric beds of hospitals in the Apulia region of Italy were analyzed. Demographic data, comorbidities, need for oxygen support, length of hospital stay, palivizumab administration, and outcomes were collected. For the purpose of the analysis, patients were divided into those aged 0–3 months and > 3 months. A multivariate logistic regression model was used to explore associations between the need for oxygen support and sex, age, comorbidities, history of prematurity, length of hospital stay, and palivizumab administration.
Results
This study included 349 children aged 0–12 months admitted for bronchiolitis, with a peak of hospitalization in November (7.4 cases/1,000 children). Of these patients, 70.5% were RSV positive, 80.2% were aged 0–3 months, and 73.1% required oxygen support. Moreover, 34.9% required observation in the sub-intensive care unit, and 12.9% in the intensive care unit. Of the infants who required intensive care, 96.9% were aged 0–3 months and 78.8% were born at term. Three patients required mechanical ventilation and one, who required Extra Corporeal Membrane Oxygenation, died. Children aged 0–3 months were more likely to show dyspnea, need oxygen support, and have a longer hospital stay.
Conclusions
The present study showed that almost all of the children who required intensive care support were aged ≤ 3 months and most were born at term. Therefore, this age group remains the highest risk group for severe bronchiolitis. Preventive measures such as single-dose monoclonal antibody immunoprophylaxis, and maternal and childhood vaccination against RSV, may reduce the high public health burden of bronchiolitis.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Bronchiolitis is a leading cause of hospital admission for infants and young children worldwide, accounting for 15–17% of all hospitalizations in children aged < 2 years [1, 2]. Children with bronchiolitis typically present with signs of respiratory distress and acute lower respiratory tract infections (ALRTIs) [1]. Respiratory syncytial virus (RSV) is responsible for 60–80% of bronchiolitis cases in infants and could lead to severe disease and death in children aged < 5 years, especially during the first 6 months of life [1, 3,4,5]. It has been estimated that almost all children have been infected with RSV by age 2 years [6, 7].
Globally, RSV infection is responsible for 3.1 million episodes of RSV-ALRTIs, resulting in about 3.2 million hospital admissions and 59,600 in-hospital deaths among children aged < 5 years, making RSV-ALRTIs the third leading cause of death in this age group [5, 8]. Hospitalization for RSV in young children has been reported to peak during the first 12 months of life, with 45% of hospital admissions and in-hospital deaths due to RSV-ALRTIs occurring in children aged < 6 months [5, 9].
In temperate regions, bronchiolitis shows a seasonal pattern, characterized by an increase in number in late October, a peak in January/February, and an ending in April [10]. In 2021, the COVID-19 pandemic affected the rate of infant hospitalization for acute bronchiolitis, with a drastic reduction in number of patients during in the usual seasonal peak period [11]. Unexpectedly, many countries experienced an interseasonal resurgence of RSV infections in late 2021 [12,13,14]. In Italy, RSV infection had almost disappeared during the 2020–2021 season [15,16,17].
Yearly, hospital pediatric wards must deal with large numbers of children, especially infants, with bronchiolitis. The hospitalization cost for acute bronchiolitis in Europe is about 2,000 euros per patient in pediatric wards and 8,000 euros per patient in pediatric intensive care units, with the costs of hospitalization being significantly higher for RSV bronchiolitis than for bronchiolitis caused by other etiologies [18, 19]. Moreover, the costs of hospitalization for bronchiolitis have been reported to be higher for children aged ≤ 3 months than for older children [19].
Supportive therapy rather than interventional therapy, has been recently recommended for patients with acute viral bronchiolitis [1]. Because no specific therapies are available, preventive measures represent the only chance to reduce the burden of such infections. Prophylaxis with the monoclonal antibody palivizumab may reduce the severity of RSV associated bronchiolitis and hospitalizations for RSV infection. To date, however, palivizumab has been recommended only for infants born at gestational age ≤ 35 weeks and aged < 6 months at the beginning of the RSV season, and for children aged < 2 years with major risk factors, requiring up to five monthly administrations throughout the RSV season [20, 21]. Currently, no prophylaxis options are available for healthy term and preterm infants. New preventive strategies, such as the single-dose monoclonal antibody nirsevimab, and maternal and childhood vaccines, are about to be developed [1].
The present study aimed at describing the clinical and epidemiological characteristics of infants aged 0–12 months hospitalized with a diagnosis of bronchiolitis in neonatal or pediatric units of the Apulia region (Southern Italy) during in the 2021 out-of-season epidemic.
Methods
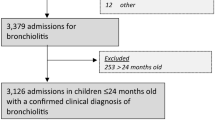
Data on children aged 0–12 months in the Apulia region of Italy, which contains about 4 million people, who were hospitalized for bronchiolitis from January to December 2021 were collected and analyzed. Nine neonatal or pediatric units covering 61% pediatric beds of hospitals in Apulia were involved in the study, with these units providing retrospectively collected data. Eligible patients were enrolled by searching discharge reports for the following diagnoses, coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM): 079.6 (RSV infection), 466.1 (acute bronchiolitis), 466.11 (acute bronchiolitis due to RSV), and 466.19 (acute bronchiolitis due to pathogens other than RSV). RSV infection was ascertained through the use of molecular tests (real-time PCR). Moreover, at admission, all children were tested for SARS-CoV-2 infection through an antigenic or molecular test (real-time PCR). Demographic data, comorbidities, need for oxygen support, length of hospital stay, palivizumab administration, and outcomes were collected by filling in a file with coded variables for each patient. Data were analyzed using STATA 14.0 software (StataCorpLLC, College Station, TX, USA). Patients were divided into those aged 0–3 months and > 3 months. Proportions were compared by chi-squared tests, whereas the average numbers of days from symptom onset to hospitalization and the average length of hospital stay in the two groups were compared by t-tests. A p-value ≤ 0.05 was considered statistically significant. A multivariate logistic regression model was used to explore associations between the need for oxygen support and sex, age, comorbidities, history of prematurity, length of hospital stay, and palivizumab administration.
All procedures performed in the study were in accordance with the ethical standards and the Declaration of Helsinki, as revised in 2013. Ethical approval was obtained from the Institutional Review Board at the Apulian Regional Observatory for Epidemiology (n. 614|04 of 4 January 2022). Informed consent was waived because all data were deidentified.
Results
Between 1 January and 31 December 2021, 349 children aged 0–12 months were hospitalized for bronchiolitis in nine neonatal or pediatric units in the Apulia region of Italy. Of these patients, 280 (80.2%) were aged 0–3 months. Etiologically, bronchiolitis was attributed to RSV infection in 246 (70.5%) patients. For the remaining 29.5% of cases, molecular testing for RSV detection was not performed and the diagnosis was based on clinical data. The demographic and clinical characteristics of all patients are summarized in Table 1.
Overall, 255 (73.1%) of the 349 patients required additional oxygen support; of these, 89/255 (34.9%) required observation in the neonatal sub-intensive care unit, and 33/255 (12.9%) in the neonatal intensive care unit. In particular, of the 33 patients in the neonatal intensive care unit, 19 (57.6%) required nasal continuous positive airway pressure (n-CPAP), three (9.0%) required nasal intermittent positive pressure ventilation (n-IPPV), and three (9.0%) required endotracheal intubation and mechanical ventilation. One patient aged one month with severe comorbidities required extracorporeal membrane oxygenation (ECMO). All the hospitalized children were tested for SARS-CoV-2 infection at admission. Only 4 children resulted positive for SARS-CoV-2 infection. All of them were aged 0–3 months and none required intensive care support. Overall, only 13 (3.7%) patients received at least one dose of palivizumab. The average time between the onset of symptoms and hospitalization was 3.7 days (range: 0–45 days), and the average length of hospital stay was 7.1 days (range: 1–76 days). The patient who required ECMO died. The incidence rates (per 1,000 resident children aged 0–12 months) of all bronchiolitis and bronchiolitis tested positive for RSV, by month of hospitalization, are shown in Fig. 1. Hospitalizations for bronchiolitis and RSV-caused bronchiolitis peaked in November 2021 (n = 207) with a incidence rate of 7.4 cases/1,000 children.
Of the 33 babies who needed intensive care support, 32 (96.9%) were aged 0–3 months and 26 (78.8%) were born at term. Table 2 compared the demographic and clinical characteristics of patients aged 0–3 months and > 3 months.
Children aged > 3 months were significantly more likely to present with comorbidities and fever (p < 0.001 each), whereas children aged 0–3 months were significantly more likely to present with dyspnea (p = 0.01) and need for oxygen support (p < 0.001). Moreover, the number of days from symptom onset to hospitalization was significantly lower (p < 0.001) and the length of hospital stay significantly higher (p < 0.001) in children aged 0–3 months than in those aged > 3 months. Multivariate logistic regression revealed that age (OR: 0.79, 95% CI: 0.71–0.88), comorbidities (OR: 4.5, 95% CI: 1.43–14.22), and length of hospital stay (OR: 1.2, 95% CI: 1.11–1.32) were significantly related to the need for oxygen support.
Discussion
Viral bronchiolitis is a common cause of hospitalization in young children. Despite RSV being recognized as the main cause of bronchiolitis presentations in infants, the community burden of RSV infections still remains underestimated worldwide. Severe bronchiolitis mainly affects children aged < 6 months [3,4,5]. However, the COVID-19 pandemic altered the epidemiology and seasonality of many respiratory viruses, causing out-of-seasonal outbreaks worldwide [22].
The present study analyzed children aged 0–12 months in the Apulia region of southern Italy who were hospitalized for bronchiolitis in 2021. Most of these children were aged ≤ 3 months, with no differences between boys and girls. Four children aged 0–3 months showed a coinfection with SARS-CoV-2 but none of them required intensive care support, suggesting that the severe clinical picture of children who required intensive care support was not associated with COVID-19. A single center study in the Apulia region found that younger children were more likely to present with dyspnea and require oxygen support, whereas older children were more likely to present with fever and comorbidities [17]. Despite the low prevalence of risk factors, more than 70% of these children required oxygen support. In particular, only 13% of these children were born prematurely, rates lower than in recent studies from Italy (24.5%) and the USA (33%) [23, 24]. Only 12% of the children in the present study had comorbidities, similar to the percentage in a Norwegian study but lower than that reported in children from the USA [24, 25].
It has been demonstrated that most children hospitalized with RSV infection were previously healthy, with only 3% of RSV-infected children in primary care having comorbidities and only 5% born prematurely [26, 27]. These findings indicate that targeting preventive strategies exclusively at high-risk children would have a limited effect on the total disease burden of RSV infection. It has been estimated that 93% of infants hospitalized were ineligible for prophylaxis with palivizumab [28]. The low prevalence of risk factors in this population, making them ineligible for prophylaxis, suggests that an all-infant immunization strategy should be considered after a cost-effectiveness analysis.
Acute seasonal bronchiolitis is an important public health issue, with severe RSV disease having significant economic costs for healthcare systems. RSV was found to reduce health‑related quality of life (HRQoL) almost 40% during the first week after onset of symptoms in patients aged < 2 years, when the illness is most severe [29]. The disease also has an impact on parents/caregivers, as they experience worry, anxiety and distress [29]. A recent Italian study estimated that the mean cost of hospitalization for bronchiolitis in a pediatric ward was more than 5,000 euros, with the cost being higher for hospitalization in pediatric intensive care units (PICU) [19]. Nearly 35% of the children in the present study who required oxygen support needed to stay in neonatal sub-intensive care units, as they needed high flow oxygen administration. Moreover about 13% of patients requiring oxygen administration needed intensive care support (n-CPAP, n-IPPV, endotracheal intubation), with almost 80% being full-term newborns. A previous European study estimated that the average cost of PICU hospitalization for bronchiolitis in children aged < 12 months was four times higher than the cost for hospitalization in a pediatric ward and more than 20 times higher than children managed in the Emergency Department [30]. More than 80% of the children described in the present study were aged 0–3 months. This age range has been reported to be a risk factor for severe bronchiolitis, with hospital admission for bronchiolitis in this age group associated with higher costs [19, 31]. Because almost all the children in the present study requiring hospitalization in the PICU were aged 0–3 months, preventive strategies aimed at protecting this age group, such as maternal vaccination and monoclonal antibody immunoprophylaxis for newborns, could potentially reduce the economic impact of bronchiolitis [19].
Currently, the only approved prophylactic measure is the administration of palivizumab. Palivizumab, however, is expensive, provides short-lived protection, and re-quires up to five monthly doses [32, 33]. The approval of the new long-acting mono-clonal antibody nirsevimab is the next expected advance in RSV prevention. In term and preterm infants, nirsevimab showed an overall efficacy of 75% in preventing ALRTIs requiring medical attention [28]. Moreover, when compared with placebo, nirsevimab showed greater ability to prevent hospitalization and provided a longer duration of protection [34]. Use of this preventive strategy in all infants during their first RSV season has been estimated to reduce direct medical costs 49%, although the costs of nirsevimab could represent a barrier to its implementation [28, 35]. A recent evaluation of the cost-effectiveness of nirsevimab programs in England and Wales revealed that, at a price per dose of £63, a large-scale seasonal program would be a cost-effective strategy for all infants at birth [33]. Moreover, by reducing the numbers of patients infected with RSV, this strategy would reduce the numbers of patients prescribed antibiotics, reducing both costs and the negative effects of antimicrobial resistance on other pathogens [33]. Despite evidence suggesting that antibiotics do not benefit patients with viral bronchiolitis, due to the low rate of bacterial superinfections, the use of antibiotics is still widespread [1, 24, 36].
The study had several limitations. First, data on the etiology of bronchiolitis were available for only 70% of the included patients, with the remaining 30% not undergoing molecular tests for RSV. The recent proposal of the World Health Organization to add RSV testing to existing influenza surveillance systems could lead to the implementation of molecular testing, at least in hospital settings [37, 38]. Second, data on possible coinfection with viruses other than SARS-CoV-2 were not available. The presence of coinfections could have affected length of hospital stay or the need for oxygen support in some patients with severe bronchiolitis.
Conclusions
The clinical and economic burden of viral bronchiolitis is still underestimated. Currently, RSV disease affects millions of children every year and is associated with high costs, even for patients with mild disease. The present study confirmed that children aged ≤ 3 months remain the highest risk group for severe bronchiolitis and admission to intensive care units. Preventive measures such as single-dose monoclonal antibody immunoprophylaxis, and maternal and childhood vaccination against RSV may reduce the high public health burden of bronchiolitis.
Availability of data and materials
Data are available on request from the corresponding author.
Abbreviations
- RSV:
-
respiratory syncytial virus
- ALRTIs:
-
acute lower respiratory tract infections
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- n-CPAP:
-
nasal continuous positive airway pressure
- n-IPPV:
-
nasal intermittent positive pressure ventilation
- ECMO:
-
extracorporeal membrane oxygenation
- HRQoL:
-
health‑related quality of life
- PICU:
-
pediatric intensive care units
References
Dalziel SR, Haskell L, O’Brien S, Borland ML, Plint AC, Babl FE, Oakley E, Bronchiolitis. Lancet. 2022 Jul 30;400(10349):392–406. doi: https://doi.org/10.1016/S0140-6736(22)01016-9. Epub 2022 Jul 1. PMID: 35785792.
Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics. 2013 Jul;132(1):28–36. https://doi.org/10.1542/peds.2012-3877. Epub 2013 Jun 3. PMID: 23733801; PMCID: PMC3691534.
Fretzayas A, Moustaki M. Etiology and clinical features of viral bronchiolitis in infancy. World J Pediatr. 2017 Aug;13(4):293–9. https://doi.org/10.1007/s12519-017-0031-8. Epub 2017 May 4. PMID: 28470580; PMCID: PMC7090852.
Bont L, Checchia PA, Fauroux B, Figueras-Aloy J, Manzoni P, Paes B, Simões EA, Carbonell-Estrany X. Defining the epidemiology and burden of severe respiratory syncytial virus infection among Infants and Children in Western Countries. Infect Dis Ther. 2016 Sep;5(3):271–98. Epub 2016 Aug 1. PMID: 27480325; PMCID: PMC5019979.
Shi T, McAllister DA, O’Brien KL, Simoes EAF, Madhi SA, Gessner BD, Polack FP et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017 Sep 2;390(10098):946–958. doi: https://doi.org/10.1016/S0140-6736(17)30938-8. Epub 2017 Jul 7. PMID: 28689664; PMCID: PMC5592248.
Bohmwald K, Espinoza JA, Pulgar RA, Jara EL, Kalergis AM. Functional Impairment of Mononuclear Phagocyte System by the Human Respiratory Syncytial Virus.Front Immunol. 2017 Nov27;8:1643. doi: https://doi.org/10.3389/fimmu.2017.01643. PMID: 29230219; PMCID: PMC5712212.
Efstathiou C, Abidi SH, Harker J, Stevenson NJ. Revisiting respiratory syncytial virus’s interaction with host immunity, towards novel therapeutics. Cell Mol Life Sci. 2020 Dec;77(24):5045–58. https://doi.org/10.1007/s00018-020-03557-0. Epub 2020 Jun 16. PMID: 32556372; PMCID: PMC7298439.
Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, O’Brien KL, Roca A, Wright PF, Bruce N, Chandran A, Theodoratou E, Sutanto A, Sedyaningsih ER, Ngama M, Munywoki PK, Kartasasmita C, Simões EA, Rudan I, Weber MW, Campbell H. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young chil-dren: a systematic review and meta-analysis. Lancet. 2010 May 1;375(9725):1545-55. doi: https://doi.org/10.1016/S0140-6736(10)60206-1. PMID: 20399493; PMCID: PMC2864404.
Kuhdari P, Brosio F, Malaventura C, Stefanati A, Orsi A, Icardi G, Gabutti G. Human respiratory syncytial virus and hospitalization in young children in Italy. Ital J Pediatr. 2018 May 4;44(1):50. doi: https://doi.org/10.1186/s13052-018-0492-y. PMID: 29728106; PMCID: PMC5935991.
Obando-Pacheco P, Justicia-Grande AJ, Rivero-Calle I, Rodríguez-Tenreiro C, Sly P, Ramilo O, Mejías A, Baraldi E, Pa-padopoulos NG, Nair H, Nunes MC, Kragten-Tabatabaie L, Heikkinen T, Greenough A, Stein RT, Manzoni P, Bont L, Martinón-Torres F. Respiratory Syncytial Virus Seasonality: A Global Overview. J Infect Dis. 2018 Apr 11;217(9):1356–1364. doi: https://doi.org/10.1093/infdis/jiy056. PMID: 29390105.
Berdah L, Romain AS, Rivière S, Schnuriger A, Perrier M, Carbajal R, Lorrot M, Guedj R, Corvol H. Retrospective ob-servational study of the influence of the COVID-19 outbreak on infants’ hospitalisation for acute bronchiolitis. BMJ Open. 2022 Oct 31;12(10):e059626. doi: https://doi.org/10.1136/bmjopen-2021-059626. PMID: 36316083; PMCID: PMC9627576.
Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of Social Distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during Early 2020. Pediatr Infect Dis J. 2020;39:e423–7.
Guedj R, Lorrot M, Lecarpentier T, Leger PL, Corvol H, Carbajal R. Infant bronchiolitis dramatically reduced during the second french COVID-19 outbreak. Acta Paediatr. 2021;110:1297–9.
Rambaud J, Dauger S, Morin L, Bergounioux J, Leger PL, Carbajal R, Renolleau S, Guedj R. Bronchiolitis ad-missions to intensive care during COVID. Pediatrics. 2021;147:e2021050103.
Vittucci AC, Piccioni L, Coltella L, Ciarlitto C, Antilici L, Bozzola E, Midulla F, Palma P, Perno CF, Villani A. The disappearance of respiratory viruses in children during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:9550.
Curatola A, Lazzareschi I, Bersani G, Covino M, Gatto A, Chiaretti A. Impact of COVID-19 outbreak in acute bronchiolitis: lesson from a tertiary italian Emergency Department. Pediatr Pulmonol. 2021;56:2484–8.
Loconsole D, Centrone F, Rizzo C, Caselli D, Orlandi A, Cardinale F, Serio C, Giordano P, Lassandro G, Milella L, Fi-carella MT, Baldassarre ME, Laforgia N, Chironna M. Out-of-Season Epidemic of Respiratory Syncytial Virus during the COVID-19 Pandemic: The High Burden of Child Hospitalization in an Academic Hospital in Southern Italy in 2021. Children (Basel). 2022 Jun 8;9(6):848. doi: https://doi.org/10.3390/children9060848. PMID: 35740785; PMCID: PMC9221938.
Heikkilä P, Forma L, Korppi M. Hospitalisation costs for infant bronchiolitis are up to 20 times higher if intensive care is needed. Acta Paediatr. 2015 Mar;104(3):269–73. https://doi.org/10.1111/apa.12881. Epub 2015 Jan 30. PMID: 25431309.
Bozzola E, Ciarlitto C, Guolo S, Brusco C, Cerone G, Antilici L, Schettini L, Piscitelli AL, Chiara Vittucci A, Cutrera R, Raponi M, Villani A. Respiratory Syncytial Virus Bronchiolitis in Infancy: The Acute Hospitalization Cost.Front Pediatr. 2021 Jan18;8:594898. doi: https://doi.org/10.3389/fped.2020.594898. PMID: 33537260; PMCID: PMC7848214.
Agenzia Italiana del Farmaco. Determina 2 Novembre 2017. Available online: https://www.gazzettaufficiale.it/eli/id/2017/11/09/17A07585/sg.2017 (accessed on 15 February 2022).
Bollani L, Baraldi E, Chirico G, Dotta A, Lanari M, Del Vecchio A, Manzoni P, Boldrini A, Paolillo P, Di Fabio S et al. Revised recommendations concerning palivizumab prophylaxis for respiratory syncytial virus (RSV). Ital. J. Pe-diatr. 2015, 41,97.
Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJE, Grenfell BT. The impact of COVID-19 nonpharmaceu-tical interventions on the future dynamics of endemic infections. Proc. Natl. Acad. Sci. USA 2020, 117, 30547–30553.
Barbati F, Moriondo M, Pisano L, Calistri E, Lodi L, Ricci S, Giovannini M, Canessa C, Indolfi G, Azzari C. Epidemiology of Respiratory Syncytial Virus-Related Hospitalization Over a 5-Year Period in Italy: Evaluation of Seasonality and Age Distribution Before Vaccine Introduction. Vaccines (Basel). 2020 Jan 4;8(1):15. doi: https://doi.org/10.3390/vaccines8010015. PMID: 31947976; PMCID: PMC7157234.
Ramilo O, Mejias A. Measuring the Burden of RSV in children to precisely assess the impact of preventive strategies. Pediatrics. 2020 Jul;146(1):e20201727. https://doi.org/10.1542/peds.2020-1727. Epub 2020 Jun 16. PMID: 32546584.
Havdal LB, Bøås H, Bekkevold T, Kran AB, Rojahn AE, Størdal K, Debes S, Døllner H, Nordbø SA, Barstad B, Haarr E, Fernández LV, Nakstad B, Inchley C, Flem E. The burden of respiratory syncytial virus in children under 5 years of age in Norway. J Infect. 2022 Feb;84(2):205–15. Epub 2021 Dec 11. PMID: 34906596.
Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, Auinger P, Griffin MR, Poehling KA, Erdman D, Grijalva CG, Zhu Y, Szilagyi P. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009 Feb;5(6):588–98. https://doi.org/10.1056/NEJMoa0804877. PMID: 19196675; PMCID: PMC4829966.
van Summeren JJGT, Rizzo C, Hooiveld M, Korevaar JC, Hendriksen JMT, Dückers MLA, Loconsole D, Chironna M, Bangert M, Demont C, Meijer A, Caini S, Pandolfi E, Paget J. Evaluation of a standardised protocol to measure the dis-ease burden of respiratory syncytial virus infection in young children in primary care. BMC Infect Dis. 2021 Jul 26;21(1):705. doi: https://doi.org/10.1186/s12879-021-06397-w. PMID: 34311699; PMCID: PMC8311415.
Kieffer A, Beuvelet M, Sardesai A, Musci R, Milev S, Roiz J, Lee JKH. Expected Impact of Universal Immunization With Nirsevimab Against RSV-Related Outcomes and Costs Among All US Infants in Their First RSV Season: A Static Model.J Infect Dis. 2022 Aug15;226(Suppl 2):S282-S292. doi: https://doi.org/10.1093/infdis/jiac216. PMID: 35968866; PMCID: PMC9377043.
Díez-Gandía E, Gómez-Álvarez C, López-Lacort M, Muñoz-Quiles C, Úbeda-Sansano I, Díez-Domingo J, Orrico-Sánchez A. ; Study collaborators. The impact of childhood RSV infection on children’s and parents’ quality of life: a prospective multicenter study in Spain. BMC Infect Dis. 2021 Sep 6;21(1):924. doi: https://doi.org/10.1186/s12879-021-06629-z. PMID: 34488668; PMCID: PMC8422742.
Ledbetter J, Brannman L, Wade SW, Gonzales T, Kong AM. Healthcare resource utilization and costs in the 12 months following hospitalization for respiratory syncytial virus or unspecified bronchiolitis among infants. J Med Econ. 2020 Feb;23(2):139–147. doi: 10.1080/13696998.2019.1658592. Epub 2019 Sep 4. PMID: 31432723.
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, Johnson DW, Light MJ, Maraqa NF, Mendonca EA, Phelan KJ, Zorc JJ, Stanko-Lopp D, Brown MA, Nathanson I, Rosenblum E, Sayles S 3rd, Hernan-dez-Cancio S, American Academy of Pediatrics. ;. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014 Nov;134(5):e1474-502. doi: https://doi.org/10.1542/peds.2014-2742. Erratum in: Pediatrics. 2015 Oct;136(4):782. PMID: 25349312.
IMpact-RSV. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998 Sep;102(3):531–7. PMID: 9724660.
Hodgson D, Koltai M, Krauer F, Flasche S, Jit M, Atkins KE. Optimal Respiratory Syncytial Virus intervention pro-grammes using Nirsevimab in England and Wales. Vaccine. 2022 Nov 22;40(49):7151–7157. doi: https://doi.org/10.1016/j.vaccine.2022.10.041. Epub 2022 Oct 31. PMID: 36328884.
Hammitt LL, Dagan R, Yuan Y, Baca Cots M, Bosheva M, Madhi SA, Muller WJ, Zar HJ, Brooks D, Grenham A, Wählby Hamrén U, Mankad VS, Ren P, Takas T, Abram ME, Leach A, Griffin MP, Villafana T, MELODY Study Group. ;. Nirse-vimab for Prevention of RSV in Healthy Late-Preterm and Term Infants. N Engl J Med. 2022 Mar 3;386(9):837–846. doi: https://doi.org/10.1056/NEJMoa2110275. PMID: 35235726.
Scotta MC, Stein RT. Current strategies and perspectives for active and passive immunization against Respiratory Syncytial Virus in childhood. J Pediatr (Rio J). 2022 Nov 16:S0021-7557(22)00122-X. doi: https://doi.org/10.1016/j.jped.2022.10.004. Epub ahead of print. PMID: 36402228.
American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Volume 134. Pediatrics: American Academy of Pediatrics Committee on Infectious Diseases; 2014. pp. 415–20.
World Health Organization. Global Influenza Programme - Respiratory Syncytial Virus Surveillance. Available online: https://www.who.int/teams/global-influenza-programme/global-respiratory-syncytial-virus-surveillance (accessed on 10 November 2022).
Broor S, Campbell H, Hirve S, Hague S, Jackson S, Moen A, Nair H, Palekar R, Rajatonirina S, Smith PG, Venter M, Wairagkar N, Zambon M, Ziegler T, Zhang W. Leveraging the global influenza surveillance and response system for global respiratory syncytial virus surveillance-opportunities and challenges. Influenza Other Respir Viruses. 2020 Nov;14(6):622–9. https://doi.org/10.1111/irv.12672. Epub 2019 Aug 24. PMID: 31444997; PMCID: PMC7578328.
Acknowledgements
The authors would like to thank Dr. Ruggiero Carbone, Dr. Barbara Carlucci, Dr. Rosa Cafagna, Dr. Matteo Rinaldi, Dr. Domenico Martinelli, Dr. Antonio Ciro Mondelli, and Dr. Giulia Tomasicchio to kindly help us with investigation of cases.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: MEB, DL and MC; methodology: DL and FC; validation: MC; formal analysis: FC; investigation: DC, BM, LQ, AA, GDA, GM, GL, AR, and MDN; data curation: DL and FC; writing-original draft preparation: MEB and DL; writing-review and editing: MEB, MC, and NL; supervision, MC and NL. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committees, and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from the Institutional Review Board at the Apulian Regional Observatory for Epidemiology (n. 614|04 of 4 January 2022), which waived the requirement for informed consent because all data were deidentified.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests and no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baldassarre, M.E., Loconsole, D., Centrone, F. et al. Hospitalization for bronchiolitis in children aged ≤ 1year, Southern Italy, year 2021: need for new preventive strategies?. Ital J Pediatr 49, 66 (2023). https://doi.org/10.1186/s13052-023-01455-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01455-2