Abstract
Background
Quality sleep is essential for physical and mental health. We aimed to analyze sleep disorders in children with acute leukemia and explore associated factors.
Methods
General data and sleep disorders in children with acute leukemia during chemotherapy were collected by general questionnaires, Children's Sleep Disorders Scale and the Parenting Stress Index-short form.
Results
In total, 173 valid questionnaires were collected. The total Sleep Disorder Scale score > 39 is considered a sleep disorder, while sleep disorders accounted for 45.66% (79/173). In the cohort, 167 children had acute lymphoblastic leukemia, with 40.12% (67/167) having sleep disorders, while six children had acute non-lymphoblastic leukemia, with 50.00% (3/6) having sleep disorders. Single- and multi-factor regression analyses of age, gender, number of children in the family, and time spent using electronic devices showed that factors influencing sleep disorders in these children were mainly parental scolding and adenoid hypertrophy. Children with sleep disorders had more parental stress than those without sleep disorders (P < 0.05).
Conclusions
The high incidence of sleep disorders in children with acute leukemia is related to airway conditions and parental behaviors. Sleep disorders in children can increase parenting stress. Factors potentially affecting sleep quality should be addressed as early as possible, while parental education should be strengthened to better facilitate the physical and psychological recovery of their children.
Similar content being viewed by others
Introduction
Quality sleep is essential for physical and mental health. Thus, sleep disorders may be associated with impaired cognitive performance [1], mood disorders [2], language and behavior problems like attention deficits [3, 4], lagging performance [5], and obesity [6]. Sleep is influenced by different factors such as genes, brain activity, the sleep environment, and airway conditions [7,8,9]. The incidence of sleep disorders in children of different ages is high. Difficulty going to bed and frequent waking during the night are reported in 20 to 30 percent of children under 3 years of age and 25 to 50 percent of preschoolers [10,11,12,13]. Up to 50% of children having sleep problems [14, 15] and sleep disorders have gained increased research traction. A study reported sleep disturbances in children with leukemia after receiving chemotherapy, but only for a short period of time [16]. There are few studies on long-term sleep and its influencing factors in children with leukemia during chemotherapy. So we hope to assess the long-time sleep situation of leukemia children by sleep disorder scale during the chemotherapy, and collect information like age, electronic products, for analysing of factors affecting the sleep quality in them. We believe our study will comprehensively improve the healthcare management of children with acute leukemia by exploring sleep disorders, identifying associated factors and its relationship with parental stress index. Parenting stress occurs in the process of parenting, and high parenting stress is not conducive to the physical and mental health of parents and children [17]. To understand the parenting status and influencing factors of children with leukemia, and to analyze the correlation between children's sleep disorders and parental parenting stress, so as to provide a basis for reducing parenting stress.
Materials and methods
Study information
From 2020 to 2022, the Childhood Sleep Disorders Scale questionnaire was administered to children (and guardians) undergoing chemotherapy in the Department of Hematology Oncology, Children's Hospital of Zhejiang University. General information including age, gender, parents' situation, work status of parents, family monthly income, number of children in the family, place of residence, whether playing cell phones and other electronic products before going to bed, average daily time spent in using electronics, whether scolding children, whether central nervous system involvement(leukemia with central nervous system infiltration), presence or absence of adenoid hypertrophy, was also collected. Inclusion criteria: 1) a confirmed diagnosis of acute lymphoblastic leukemia or acute non-lymphoblastic leukemia; 2) informed consent from guardians. Exclusion criteria: 1) an extremely critical and life-threatening condition; 2) children under the age of 6 months were excluded.
We used the Chinese version of Children's Sleep Disorders Scale (CSDS) made by Bruni et al. [18] and the Parenting Stress Index-short form (PSI-SF) compiled by Abidin [19, 20]. The PSI-SF consists of three 12-item subscales, with a total of 36 items, including three dimensions: Parenting distress, parent–child interaction disorder, and difficult child. Each item is rated on a 5-point Likert-type scale with 1 indicating (strongly disagree) and 5 indicating (strongly agree). higher scores were associated with greater stress. The CSDS has high reliability and validity in the context of Chinese culture. The scale consisted of 26 questions divided into six categories: i) difficulty falling asleep and maintaining sleep, ii) sleep breathing disorder, iii) arousal disorder, iv) sleep–wake transition disorder, v) excessive sleepiness, and vi) excessive night sweating. The scale was also divided into five categories: a) none, b) occasionally (< 1–2 times/month), c) sometimes (1–2 times/month), d) often (3 or 5 times/month), and e) always (daily), with scores of 1, 2, 3, 4, and 5, respectively. Higher total scores indicated more severe sleep disorders. A total score > 39 was considered a sleep disorder.
Children’s body mass index (BMI) was calculated by weight (kg)/height squared (m2). Children in different age groups were classified as obese, overweight, or lean, with reference to corresponding sex and BMI indices and BMI percentile values for Chinese boys/girls [21]. Children with a BMI in the 85th–95th percentile in the same sex and age group were considered overweight, a BMI > 95th percentile indicated obesity, and a BMI < 3th percentile were considered lean. In this study, children’s BMIs were divided into normal group and abnormal group, with the latter category including obesity, overweight, and lean.
The scale is commonly used to investigate sleep issues in children > 5 years old; Due to several studies suggested the scale was applicable to preschool children and infants [22,23,24], children < 18 years old were included in this study. Notably, the study mentioned above [22,23,24] made some adjustments to the scale items and was in diffrent coutries, so we suggest futher research on the application of CSDS in children under 6 years of age in China to increase the validity of the results of this study.
Statistical analysis
Statistical analyses was performed using SPSS 23.0 software(IBM Corp, Armonk, NY, USA). Chi-square test was used for count data, and t test or analysis of variance was used for measurement data. The factors included age, gender, single-parent family, number of children in the family, parents’ working situation, place of residence, parents' education, monthly household income, playing cell phones and other electronic products before going to bed, average daily time spent in using electronics, scolding children, central nervous system involvement(leukemia with central nervous system infiltration), adenoid hypertrophy. When analysing the influencing factors of sleep disorders, single-factor analysis results showing a significance of P < 0.1 were included in multi-factor analysis. Then, multi-factor logistic regression analysis was used for statistical analysis.In multifactor analysis, we considered a P value < 0.05 as statistically significant. In the analysis of the influencing factors related to PSI, multiple linear regression analysis was used, with P value < 0.05 as statistically significant.
Results
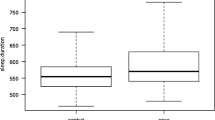
In total, 173 valid questionnaires were collected from children with acute leukemia, with 96 boys and 77 girls. The age range was 8 months–18 years (12 children were 0–2 years, 47 were 3–4 years, 39 were 5–6 years, and 75 were 7–18 years). The mean age and SD was 6.86 ± 3.67. The BMI ranged from 13.10 to 37.12, with a median of 16.80. The total Sleep Disorders Scale score range for all children was 26–84 (Fig. 1), with a median of 38 and interquartile range of 34–46, and 79 cases (45.66%) have sleep disorders. Detailed scores are shown in Table 1.
Among 173 children, 167 had acute lymphoblastic leukemia, with 40.12% (67/167) having sleep disorders, while six had acute non-lymphoblastic leukemia, with 50.00% (3/6) having sleep disorders. After grouping according to different gender, age and other factors, the situation of sleep disorders in different groups are shown in Table 2. Eleven children had central nervous system leukemia, including seven cases of sleep disorders. The CNS was not involved in 162 children, including 72 cases of sleep disorders. We observed 139 children where electronic devices were used before bedtime, of which 46.04% had sleep disorders (64/139). In 34 children, electronic devices were not used before bedtime, of which 44.12% had sleep disorders (15/34). The sleep disorder rate was 41.07% (23/56) in children who used electronic products for < 3 h/day, 50.00% (33/66) in children who used electronic products for 3–6 h/day, and 45.10% (23/51) in children who used electronic products for > 6 h/day. The rate of sleep disturbance in children in families where parents said they never hit/scolded their children was 35.82% (24/67), and in families where children were scolded, the rate was 51.89% (55/106).
Univariate analyses were performed on gender, age, single parent, single-child family, parental work status, place of residence, BMI, electronic devices used before bedtime, average daily time spent using electronic devices,scolding children, involving the central nervous system, and the presence of adenoid hypertrophy. Univariate analyses showed that child in a single-child family, be beaten/scolded, with adenoidal hypertrophy, were possibly factors related to sleep disturbance in children with acute leukemia (P < 0.1, Table 2). Further multifactorial logistic regression analysis suggested that scolding (P = 0.033) and adenoid hypertrophy (P = 0.032) were risk factors for sleep disturbance in these children (Fig. 2).
Logistic regression analysis results of factors influencing sleep disorders in children. ORa(odds ratio a): OR values of the independent variables single child and scolding are referenced to the left y-coordinate. ORb(odds ratio b): OR of the independent variable adenoid hypertrophy is referenced to the y-coordinate on the right
The total score of the parenting stress scale was 92.27 for the children with sleep disorder and 82.22 for the children without sleep disorder. In order to understand the influencing factors of parental stress index in children with leukemia, univariate analyses (Table 3) and multiple linear regression analysis were performed on child gender, single parent, the number of child, parental work status, parents' education, number of children, family monthly income, Sleep disorders in children. Through univariate analyses, we found an inverse relationship between parenting stress index and parental education level (P < 0.05). In households where both parents were employed and the household monthly income was higher, the parental stress index was lower (P < 0.05). Compared to families with children having sleep disorders, parents whose children had sleep disorders had a higher stress index (P < 0.05). However, multiple linear regression analysis showed that(F = 5.691, p < 0.001), family monthly income (β = -0.233, P < 0.007)significantly negatively predicted parental stress index, and children's sleep disorder (β = 0.232, p = 0.001)significantly positively predicted parental stress index. These variables explained 16.00% of the variation in parental stress index. Factors such as child gender, single parent, the number of child, parental work status, parents' education, number of children, could not predict the parental stress index. So family monthly income and child with sleep disorders, were both risk factors for PSI.
Discussion
Sleep disorders that occur in infants often persist into later development [25, 26]. Sleep disorders can impact cognition, mood, social well-being, immunity, and cardiovascular systems [27,28,29], while high quality sleep enhances immune defenses [30] and allows children with leukemia to sleep well and improve their immunity. Many studies on acute leukemia in children have focused on disease pathogenesis and prognosis, but less on sleep in children with leukemia. Environments where children with acute leukemia undergo chemotherapy are quite different to ordinary environments, therefore factors affecting sleep disorders in these children may be quite different to ordinary children.
From our data, sleep disturbance risk factors in children with acute leukemia during chemotherapy involved parental scolding and adenoid hypertrophy, while age, gender, BMI, single parent families, number of children in the home, and time spent using electronic devices were not risk factors. Previous studies considered single parent and only child families as influencing factors impacting children's sleep [31, 32], but we observed no relationship between these factors, probably because children with leukemia have more time with family and less emotional problems due to parental absence, which laterally suggests relatives help improve children's sleep. We observed no statistically significant differences in total sleep disorder scores of children with leukemia living in urban/suburban areas, which may be related to increased urbanization in China, while no significant differences between urban and suburban environments were observed in Hangzhou, Zhejiang Province, China. A previous study of sleep disorders in children with brain tumors concluded these children were more likely to develop sleep disorders when compared with healthy children [33]. We identified no differences in sleep disorder scores between children with and without CNS leukemia, but the number of cases with definitive CNS leukemia was low, thus these results may be biased. Thus, the impact of CNS leukemia on sleep quality in these children requires further study. Previous studies examined the role of both delayed sleep onset and school demands which reduced sleep levels in adolescents [34]. In China, schoolwork stress significantly increases in children starting at age 7 years, but there was no significant difference in the incidence of sleep disturbance between children aged less than 7 years and those older than 7 years. In this study, presumably due to the fact that children with leukemia during chemotherapy are essentially off school and do not have the need to get up early for school compared to the general population. This suggests the importance of reducing academic pressure and ensuring adequate sleep in school-aged children.
The rate of sleep disturbance was significantly higher in children with leukemia with adenoidal hypertrophy and agreed with previous studies showing that adenoid hypertrophy caused airway hypoventilation and sleep architecture disorders [35]. Studies also reported an increased risk of sleep apnea in obese and underweight children [36, 37]. However, we observed no significant differences in sleep disorders between children with normal and abnormal BMIs, but an insufficient sample size may be partly responsible for this. Additionally, the correlation between BMI and sleep quality may not be significant if BMI abnormalities did not significantly affect airway ventilation conditions during sleep.
Previous studies reported that the longer the exposure time to artificial light and electronic screens, the shorter the sleep time, thus the effects of electronic screens (cell phones and computers) on sleep may be related to psychological and physiological arousal and inhibited melatonin levels [38,39,40]. However, we observed no effects of electronic product and bedtime use on sleep disorders in children with acute leukemia. We speculate the effects of electronics on sleep may be two-fold. Moderate electronic device use can relax the body and mind, but excessive use at inappropriate times, and an unwillingness to disconnect when the body and mind are in a drowsy state can excite the brain which is not conducive to brain "rest". For children with stable acute leukemia, and for whom chemotherapy is going well, these children are away from school, without schoolwork and accompanied by parents or relatives at home, so their psychological stress is less when compared with healthy children. Their daily use of electronic products is mainly to play simple games, watch short videos or cartoons. Their day and night sleep rhythm is relatively fixed and can basically leave electronic products on time before bedtime under parental supervision. So electronic products have less impact on sleep disorders in children with acute leukemia. We hypothesize that disrupted sleep rhythms exert a larger impact on sleep than staying up late.
Sleep and emotions interact with each other; brain structures and neurochemicals involved in emotion regulation are also involved in sleep [41, 42]. Also, emotional disorders are often accompanied by sleep disturbances [43, 44], while sleep deprivation increases negative emotions but decreases positive emotions [45], and the stronger the negative stimulus, the more sleep is required [46]. Parental scolding can cause sleep disturbance in children with acute leukemia due to negative stimulation caused by parental behaviors.
The current study found that the higher the family income, the lower the parenting stress index, which was also confirmed by Atout M et al. [47]. They also found an association between parental stress and education level, which was not found in this study and may require support from a larger sample size. The biggest innovation of this study is the combination of sleep disorders and parenting stress index in children with leukemia. The decline of children's sleep quality can affect their daytime activities and emotional state, thereby increasing parenting stress. Increased parenting stress also enhances parents' negative emotions, adversely affects parents' physical and mental health, and is not conducive to their care of children. Other studies have found that parenting stress is related to the duration of the disease [48], and the decline of sleep quality in children with leukemia is also related to drug use [49] and fatigue [16]. This study did not count the data of drug use and course of disease in children with leukemia, which is a limitation of this study.
Conclusions
Adenoid hypertrophy and parental scolding were important factors in sleep disorder development in children with acute leukemia. In the future, we must ensure improved child airway conditions (e.g., prompt treatment of adenoid hypertrophy by hormones or surgery), maintain harmonious parent–child relationships, avoid scolding, and promptly channel children’s negative emotions. In doing so, the sleep quality of children with leukemia can be improved, with their immunity strengthened, parenting stress reduced, and initial steps toward physical and mental health recovery taken.
Availability of data and materials
The data supporting the results of these studies are available upon reasonable request to the respective authors. The data involving patients are not publicly available due to privacy or ethical restrictions.
References
Short MA, Blunden S, Rigney G, Matricciani L, Coussens S, Reynolds CM, Galland B. Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep Health. 2018;4(3):292–300. https://doi.org/10.1016/j.sleh.2018.02.004.
Wong MM, Brower KJ, Craun EA. Insomnia symptoms and suicidality in the national comorbidity survey—adolescent supplement. J Psychiatr Res. 2016;81:1–8. https://doi.org/10.1016/j.jpsychires.2016.06.004.
McGregor KK, Alper RM. Sleep Disorders as a Risk to Language Learning and Use. EBP Briefs. 2015;10(1):1–21.
Kooij JJS, Bijlenga D. The circadian rhythm in adult attention-deficit/hyperactivity disorder: current state of affairs. Expert Rev Neurother. 2013;13:1107–16. https://doi.org/10.1586/14737175.2013.836301.
Beebe DW, Ris MD, Kramer ME, Long E, Amin R. The association between sleep disordered breathing, academic grades, and cognitive and behavioral functioning among overweight subjects during middle to late childhood. Sleep. 2010;33(11):1447–56. https://doi.org/10.1093/sleep/33.11.1447.
Li L, Zhang S, Huang YB, Chen KX. Sleep duration and obesity in children: A systematic review and meta-analysis of prospective cohort studies. J Paediatr Child Health. 2017;53(4):378–85. https://doi.org/10.1111/jpc.13434.
Bathory E, Tomopoulos S. Sleep Regulation, Physiology and Development, Sleep Duration and Patterns, and Sleep Hygiene in Infants, Toddlers, and Preschool-Age Children. Curr Probl Pediatr Adolesc Health Care. 2017;47(2):29–42. https://doi.org/10.1016/j.cppeds.2016.12.001.
Ophoff D, Slaats MA, Boudewyns A, et al. Sleep disorders during childhood: a practical review. Eur J Pediatr. 2018;177(5):641–8. https://doi.org/10.1007/s00431-018-3116-z.
Huang SY, Qin L, Liu HR, Li DD. Sleep and language development in children and adolescents. Chin J Behav Med Brain Sci, 2021,30(05). https://doi.org/10.3760/cma.j.cn371468-20200930-01758 (in Chinese)
Trosman I, Ivanenko A. Classification and Epidemiology of Sleep Disorders in Children and Adolescents. Child Adolesc Psychiatr Clin N Am. 2021;30(1):47–64. https://doi.org/10.1016/j.chc.2020.08.002.
Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18(1):60–73. https://doi.org/10.1111/j.1365-2869.2008.00699.x.
Owens J. Classification and epidemiology of childhood sleep disorders. Sleep Med Clin. 2007;2(3):353–61. https://doi.org/10.1016/j.pop.2008.06.003.
Gaylor EE, Burnham MM, Goodlin-Jones BL, Anders TF. A longitudinal follow-up study of young children’s sleep patterns using a developmental classification system. Behav Sleep Med. 2005;3(1):44–61. https://doi.org/10.1207/s15402010bsm0301_6.
Pagel JF, Forister N, Kwiatkowki C. Adolescent sleep disturbance and school performance: the confounding variable of socioeconomics. J Clin Sleep Med. 2007;3(1):19–23.
Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368–77.
Gedaly-Duff V, Lee KA, Nail L, Nicholson HS, Johnson KP. Pain, Sleep Disturbance, and Fatigue in Children With Leukemia and Their Parents: a pilot study. Oncol Nurs Forum. 2006;33(3):641–6. https://doi.org/10.1188/06.ONF.641-646.
Hildingsson I, Haines H, Johansson M, Rubertsson C, Fenwick J. Childbirth fear in Swedish fathers is associated with parental stress as well as poor physical and mental health. Midwifery. 2014;30(2):248–54. https://doi.org/10.1016/j.midw.2013.12.012.
Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, Giannotti F. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–61 https://doi.org/10.1111/j.1365-2869.1996.00251.x
Abidin RR. The Parenting Stress Index-Short Form. Charlottesville, VA: Pediatric Psychology Press; 1990.
Abidin RR. Parenting Stress Index/Short Form—manual. Odessa, FL: Psychologica l Assessment Resources, 1995.
Hui LI , Chengye JI, Xinnan Zong, Yaqin Zhang. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years. Chin J Pediatr, 2009,47(07). https://doi.org/10.3760/cma.j.issn.0578-1310.2009.07.004. (in Chinese).
Romeo DM, Bruni O, Brogna C, et al. Application of the sleep disturbance scale for children (SDSC) in preschool age. Eur J Paediatr Neurol. 2013;17(4):374–82. https://doi.org/10.1016/j.ejpn.2012.12.009.
Romeo DM, Cordaro G, Macchione E, et al. Application of the Sleep Disturbance Scale for Children (SDSC) in infants and toddlers (6–36 months). Sleep Med. 2021;81:62–8. https://doi.org/10.1016/j.sleep.2021.02.001.
Lecuelle F, Gustin MP, Leslie W, et al. French validation of the sleep disturbance scale for children (SDSC) in young children (aged 6 months to 4 years). Sleep Med. 2020;67:56–65. https://doi.org/10.1016/j.sleep.2019.09.014.
Pesonen AK, Martikainen S, Heinonen K, et al. Continuity and change in poor sleep from childhood to early adolescence. Sleep. 2014;37:289–97. https://doi.org/10.5665/sleep.3400.
Sheridan A, Murray L, Cooper PJ, et al. A longitudinal study of child sleep in high and low risk families: relationship to early maternal settling strategies and child psychological functioning. Sleep Med. 2013;14:266–73. https://doi.org/10.1016/j.sleep.2012.11.006.
Short MA, Chee MWL. Adolescent sleep restriction effects on cognition and mood. Prog Brain Res. 2019;246:55–71. https://doi.org/10.1016/bs.pbr.2019.02.008.
Carney CE, Edinger JD, Meyer B, Lindman L, Istre T. Daily activities and sleep quality in college students. Chronobiol Int. 2006;23(3):623–37. https://doi.org/10.1080/07420520600650695.
Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;3(66):143–72. https://doi.org/10.1146/annurev-psych-010213-115205.
Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19(11):702–15. https://doi.org/10.1038/s41577-019-0190-z.
Troxel WM, Lee L, Hall M, Matthews KA. Single-parent family structure and sleep problems in black and white adolescents. Sleep Med. 2014;15(2):255–61. https://doi.org/10.1016/j.sleep.2013.10.012.
Bacaro V, Chiabudini M, Buonanno C, et al. Sleep Characteristics in Italian Children During Home Confinement Due to Covid-19 Outbreak. Clin Neuropsychiatry. 2021;18(1):13–27. https://doi.org/10.36131/cnfioritieditore20210102.
Pilotto C, Passone E, Coassin E, et al. Sleep disorders in children with brain tumors: a pilot study based on a sleep disorder questionnaire. Childs Nerv Syst. 2018;34(8):1535–40. https://doi.org/10.1007/s00381-018-3809-7.
Williams JA, Zimmerman FJ, Bell JF. Norms and trends of sleep time among US children and adolescents. JAMA Pediatr. 2013;167(1):55–60. https://doi.org/10.1001/jamapediatrics.2013.423.
Zhang XW, Zhou F, Li Y, Huang ZT, Wang ZL. Sleep architecture in children with adenoidal hypertrophy. J Paediatr Child Health. 2006;42(10):625–9. https://doi.org/10.1111/j.1440-1754.2006.00939.x.
Kang KT, Lee PL, Weng WC, Hsu WC. Body weight status and obstructive sleep apnea in children. Int J Obes (Lond). 2012;36(7):920–4. https://doi.org/10.1038/ijo.2012.5.
Muzumdar H, Rao M. Pulmonary dysfunction and sleep apnea in morbid obesity. Pediatr Endocrinol Rev. 2006;3(Suppl 4):579–83 PMID: 17237747.
Moreira GA, Hallinan MP. Sleepiness in Children: An Update. Sleep Med Clin. 2017;12(3):407–13. https://doi.org/10.1016/j.jsmc.2017.03.013.
Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–8. https://doi.org/10.1016/j.smrv.2014.07.007.
Owens JA, Weiss MR. Insufficient sleep in adolescents: causes and consequences. Minerva Pediatr. 2017;69(4):326–36. https://doi.org/10.23736/S0026-4946.17.04914-3.
Palmer CA, Alfano CA. Sleep and emotion regulation: An organizing, integrative review. Sleep Med Rev. 2017;31:6–16. https://doi.org/10.1016/j.smrv.2015.12.006.
Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. 2014;10:679–708. https://doi.org/10.1146/annurev-clinpsy-032813-153716.
Harvey AG. Sleep and circadian functioning: critical mechanisms in the mood disorders? Annu Rev Clin Psychol. 2011;7:297–319. https://doi.org/10.1146/annurev-clinpsy-032210-104550.
Brown WJ, Wilkerson AK, Boyd SJ, et al. A review of sleep disturbance in children and adolescents with anxiety. J Sleep Res. 2018 Jun;27(3):e12635 https://doi.org/10.1111/jsr.12635.
Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10(6):831–41. https://doi.org/10.1037/a0020138.
Werner GG, Schabus M, Blechert J, Kolodyazhniy V, Wilhelm FH. Pre- to postsleep change in psychophysiological reactivity to emotional films: late night REM sleep is associated with attenuated emotional processing. Psychophysiology. 2015;52(6):813–25. https://doi.org/10.1111/psyp.12404.
Atout M, Almomani EM, Alhusban RY, Al-Tarawneh FS, Mohammad S. Stress levels and coping strategies among Jordanian parents caring for newly diagnosed children with leukemia: A cross sectional descriptive correlational study. J Psychosoc Oncol. 2022;40(5):632–51. https://doi.org/10.1080/07347332.2021.1995802.
Sherief LM, Kamal NM, Abdalrahman HM, Youssef DM, Alhady MAA, Ali AS, Elbasset MAA, Hashim HM. Psychological Impact of Chemotherapy for Childhood Acute Lymphoblastic Leukemia on Patients and Their Parents. Medicine (Baltimore). 2015 Dec;94(51):e2280 https://doi.org/10.1097/MD.0000000000002280.
Hinds PS, Hockenberry MJ, Gattuso JS, Srivastava DK, Tong X, Jones H, West N, McCarthy KS, Sadeh A, Ash M, Fernandez C, Pui CH. Dexamethasone alters sleep and fatigue in pediatric patients with acute lymphoblastic leukemia. Cancer. 2007;110(10):2321–30. https://doi.org/10.1002/cncr.23039.
Acknowledgements
We would like to acknowledge all the parents and children who participated in the study. We sincerely appreciate the assistance of all those not listed as authors. The views expressed in this publication are those of the authors only.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
Data collection were performed and the first draft of the manuscript was prepared mainly by XL. Data analysis and manuscript revising was done by DXK. WGS participated in questionnaire design and literature search. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all parents of children included in the study. The questionnaire and methodology for this study was approved by the Human Research Ethics committee of Children’s Hospital Affiliated to Zhejiang University (Ethics approval number: 2022-IRB-106). all methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xi, L., Wu, G. & Du, X. Analyzing sleep status in children with acute leukemia. Ital J Pediatr 49, 7 (2023). https://doi.org/10.1186/s13052-023-01409-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01409-8





