Abstract
Introduction
Endotracheal intubation (ETI) is an infrequent but key component of prehospital and retrieval medicine. Common measures of quality of ETI are the first pass success rates (FPS) and ETI on the first attempt without occurrence of hypoxia or hypotension (DASH-1A). We present the results of a multi-faceted quality improvement program (QIP) on paramedic FPS and DASH-1A rates in a large regional critical care transport organization.
Methods
We conducted a retrospective database analysis, comparing FPS and DASH-1A rates before and after implementation of the QIP. We included all patients undergoing advanced airway management with a first strategy of ETI during the time period from January 2016 to December 2021.
Results
484 patients met the inclusion criteria during the study period. Overall, the first pass intubation success (FPS) rate was 72% (350/484). There was an increase in FPS from the pre-intervention period (60%, 86/144) to the post-intervention period (86%, 148/173), p < 0.001. DASH-1A success rates improved from 45% (55/122) during the pre-intervention period to 55% (84/153) but this difference did not meet pre-defined statistical significance (p = 0.1). On univariate analysis, factors associated with improved FPS rates were the use of video-laryngoscope (VL), neuromuscular blockage, and intubation inside a healthcare facility.
Conclusions
A multi-faceted advanced airway management QIP resulted in increased FPS intubation rates and a non-significant improvement in DASH-1A rates. A combination of modern equipment, targeted training, standardization and ongoing clinical governance is required to achieve and maintain safe intubation by paramedics in the prehospital and retrieval environment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Endotracheal intubation (ETI) is a high-risk procedure performed by physician and paramedics in the austere prehospital and retrieval environment [1,2,3,4]. While ETI is a key component of care for most prehospital critical care or retrieval services, research findings have been equivocal, with suggestions of benefit, no difference, or even harm [4,5,6,7]. A number of factors are likely responsible for this wide range of findings of patient outcomes following prehospital ETI. Careful patient selection is a key component to assure clinical benefit and should include the indication, resources available, likelihood of complications, and anticipated transport time and modality [2, 8]. Once the decision for prehospital ETI has been made the procedure needs to be undertaken to a high standard if it is to be beneficial [9]. The quality of ETI is difficult to measure [10], particularly if facilitated by sedative drugs (drug facilitated intubation—DFI) or through a combination of sedative drugs and a paralytic drug (rapid sequence intubation—RSI) [11]. Common variables reported as proxy-measures for the quality of ETI during prehospital DFI or RSI are the first pass success (FPS) rates, the number of intubations attempts required, overall failure rates of intubation (ie. ETI aborted after usually multiple attempts), and the incidence of new hypoxia or hypotension during DFI or RSI [4, 12,13,14]. A both process- and patient-focused quality metric suggested by the international Ground and Air Medical Quality in Transport organization (GAMUT) is DASH-1A: successful intubation on the first attempt, without the occurrence of hypoxia or hypotension [14]. Many prehospital critical care and retrieval services have published improved quality of prehospital ETI provided, as measured by these variables. Factors associated with improved quality in previous publications are the use of checklists and standard operating procedures, the introduction of video laryngoscopes (VLs), simulation training, and audit and review of cases [10, 15,16,17].
In the past, internal quality control measures demonstrated a wide variability of FPS rates for paramedics undertaking intubations within our large provincial Canadian critical care transport organization. This study describes the FPS and DASH-1A rates before and after implementation of a multi-faceted quality improvement program (QIP) focused on advanced airway management (AAM).
Methods
We designed a retrospective before and after cohort study to test the hypothesis that a multi-faceted AAM QIP improved the quality of paramedic intubation in our critical care transport organization, as measured by FPS and DASH-1A rates.
Setting
Ornge is the sole critical care transport provider for Ontario, Canada, covering an area of just over one million km2 and a population of close to 15 million. Most of the population live in the Southernmost areas of the province, and access to critical or tertiary care requires often long transfers for the remote population in Northern Ontario. The organization operates six rotor wing bases, four land vehicle bases, two fixed wing bases and one base with access to rotor and fixed wing assets. In addition, Ornge provides education and clinical oversight for the Toronto Paramedic Services (TPS) critical care transport program. All aspects of call taking and dispatch are handled at one central operations control centre. Within Ornge and TPS, three levels of paramedics are trained to provide AAM.
-
Advanced care paramedics (ACP-L) provide advanced life support (ALS) interventions including AAM and a limited number of intravenous (IV) medications such as Morphine.
-
Advanced care flight paramedics (ACP-F) provide AAM including RSI but have some restrictions regarding higher-risk drugs such as Propofol or Epinephrine
-
Critical care paramedics (CCP) provide a wide range of critical care interventions, including RSI, comparable to the level of care available in most emergency departments
Entry into the Ornge ACP-F or CCP programs requires provincial ACP-L certification. In Ontario, paramedics achieve ACP-L certification through successful completion of a two-year primary care paramedic (PCP) program followed by a one-year ACP-L college program. Upon acceptance to the Ornge ACP-F/CCP training program, paramedics complete a minimum of 18 months of theoretical modules, practical skill practice, simulation training, clinical rotations, and a certification exam. Airway management is an important aspect of this initial education and consists of a combination of theoretical, skill-based and simulation training, field-based evaluations, and certification exams.
Intervention
The QIP was implemented across the organization in 2018 and 2019. It was led by clinically active paramedics with support from transport medicine physicians, respiratory therapists, and educational specialists. It included the purchase and distribution of new equipment, standardization of equipment and procedures, and provider training in these areas. Table 1 provides a comparison of advanced airway management in the organization before and after implementation of the airway management QIP.
Inclusion/exclusion criteria
We included all patients receiving AAM and where the initial AAM strategy was orotracheal intubation. We excluded cases where the initial AAM strategy was nasotracheal intubation or the placement of a supraglottic airway. We included pediatric patients and those in cardiac arrest.
Data collection
Data was collected from the organization’s electronic records database containing all patient records. Patient demographics, intubation successes or failures, vital signs were extracted automatically. If data was missing, a manual chart review of the respective records was undertaken to complete data fields, where possible.
Definitions
During the study period, an intubation attempt was defined as the insertion of a laryngoscope beyond the patient’s teeth or gums for the purpose of achieving tracheal intubation. Successful intubation required confirmation of end tidal carbon dioxide (EtCO2) for multiple breaths and/or confirmation of ETT placement on chest x-ray. For DASH-1A rates, we excluded patients being intubated during cardiac arrest. For all other patients, DASH-1A success was defined as intubation on the first attempt, systolic blood pressure (SBP) ≥ 90 mmHg and SpO2 ≥ 90% for 10 min following intubation. Of note, we included patients whose highest SBP or SpO2 prior to intubation were lower than the cut-off of 90 mmHg or 90%, respectively. For pediatric patients, the cut-off for SBP was adjusted to the lower margin of the 95% percentile bracket of the normal distribution for the patient’s age.
Statistical analysis
Data were anonymized and statistical analysis performed using Stata Version 14 (StataCorp). We divided the study period into a pre-, peri-, and post-intervention period, covering the years 2016–2017, 2018–2019, and 2020–2021, respectively. We used the Chi-square and Kruskal–Wallis tests to examine for statistical significance of differences between the pre- and post-intervention periods for categorical and non-normal continuous data, respectively. P-values of < 0.05 were considered to have reached statistical significance.
Ethics approval
The study was reviewed and approved by the Ornge Research and Scholarly Activities Committee and research ethics approval was granted by the University of Toronto (REB: 30628).
Results
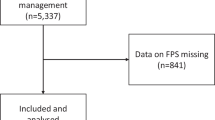
We identified 484 patient records of AAM with a first strategy of orotracheal intubation during the time period from January 2016 to December 2021. A total of 168 paramedics were involved in these cases as either intubator or airway assistant, with a median of eight cases per paramedic over the six-year study period (interquartile range [IQR] 4–12). Table 2 provides an overview of demographics and distributions of these cases.
Overall, the first pass intubation success (FPS) rate was 72% (350/484). There was a significant increase in FPS from the pre-intervention period (60%, 86/144) to the post-intervention period (86%, 148/173), p < 0.001. 69 (14%) of patients were intubated during cardiac arrest, with a FPS rate of 62% (43/69). These 69 patients were excluded from DASH-1A success rate analyses. Of the remaining 415 patients, 205 (49%) were intubated on first attempt and without the occurrence of hypoxia or hypotension. Of the 210 patients without DASH-1A success, 61 patients (29%) had pre-existing hypotension or hypoxia below the SBP of 90 mmHg and SpO2 of 90% cut-off, respectively, prior to intubation. DASH-1A success rates improved from 45% (55/122) during the pre-intervention period to 55% (84/153) but this difference did not meet pre-defined statistical significance (p = 0.1). Figure 1 outlines the development of FPS and DASH-1A rates over the study period.
The use of VL for first intubation attempts increased from 0% (0/144) in the pre-intervention period to 88% (153/173) in the post-intervention period (p < 0.001). Table 3 provides an overview of factors which were hypothesised to be potentially associated with FPS and DASH-1A rates, based on previous literature.
Discussion
This retrospective database analysis demonstrated that a multi-faceted advanced airway management quality improvement program resulted in a significant improvement in first pass success rates of endotracheal intubation in the setting of paramedic-delivered critical care transport. DASH-1A rates improved to a lesser degree, and this change was not statistically significant. In an exploratory analysis, the use of paralytics as well as intubation in a healthcare facility (as opposed to intubation during scene calls) were associated with higher FPS and DASH-1A rates. The use of VL was associated with higher FPS rates but not higher DASH-1A rates.
We believe that the increase in FPS rate from 60 to 86% (for the pre- and post-intervention period, respectively) proves the effectiveness of our organization’s AAM QIP. While the post-intervention results are encouraging, they are also comparable to previously published FPS rates from other prehospital or retrieval services [10, 18,19,20]. Our explorative analysis suggests that the organizational direction from DFI towards RSI and the introduction of VL might have contributed to increasing FPS rates. Paralysis with neuromuscular blockers has been shown to increase FPS rates during intubations in intensive care units and emergency departments, when compared to DFI [21, 22]. To our knowledge, there is no research which directly compares intubation FPS rates with and without paralysis in the prehospital and retrieval setting. A randomized controlled trial comparing intubation with Midazolam and Etomidate, without paralytics in both groups, demonstrated a low overall intubation success rate of only 76% [23]. This contrasts with multiple large case series of prehospital RSIs, where overall intubation success rates trend towards 100% [12, 18, 20]. Prehospital RSI is the recommended strategy for prehospital intubations (other than in cardiac arrest or peri-arrest situations) by the Association of Anaesthetists of Great Britain and Ireland [2].
The best available evidence for the use of VL, and specifically the C-MAC video-laryngoscope used in our organization, is a randomized controlled trial from a German physician-staffed helicopter emergency medical service (HEMS) [24]. FPS rates in this service were 95% and 79% with VL and DL, respectively (p = 0.007). A final factor associated with FPS in our organization was the location in which AAM occurred. FPS rates were significantly lower when intubations were undertaken during scene calls. The majority of these cases were trauma patients and intubation usually occurred in the back of a land ambulance. The lower FPS rate is likely a reflection of the underlying severity and acuity of these cases, limited space around the patient, and the challenges of intubation of trauma patients, when compared to patients with medical critical illness inside a healthcare facility [1, 18].
For our second primary outcome, DASH-1A success rates, our data showed a non-statistically significant increase from 45 to 55% (pre- and post-intervention, respectively). While the use of paralytics and the type of call were associated with higher FPS and DASH-1a rates, the increased FPS rates seen with the use of VL did not translate into higher DASH-1A rates. It is worth noting that most of the interventions of the QIP, particularly the use of a bougie and VL, were aimed at overcoming anatomical challenges of intubation. While this process has led to higher FPS rates over time, it did not directly address some of the physiological challenges of AAM, in particular avoidance of hypoxia and hypotension [25]. This highlights the importance of clinical governance with ongoing monitoring and training for prehospital AAM programs [9, 17]. In our organization, the 2022 annual training program will include simulation specifically focused on physiologically difficult intubations, particularly pre-intubation resuscitation of the severely hypoxic, hypotensive, or acidotic patient [25].
An important challenge that our organization faces in assuring safety and excellence in AAM is the relatively infrequent occurrence of AAM. On average, our paramedics are only involved in little more than one case of AAM per year, with some paramedics only being involved in AAM approximately once every 5 years. While the exact number of intubations or AAM cases required to maintain competence after initial training continues to be debated, many high-performing HEMS provide in excess of 100 prehospital RSIs per base per year [12, 18, 26]. In contrast, almost half of intubations in our dataset were undertaken by paramedics working at bases with less than 10 intubations per year. As part of the AAM QIP, paramedics are now required to participate in a minimum of four to six simulated AAM scenarios per year. To further maximise learning from these infrequent cases, structured debriefs of all DFIs and RSIs as well as regular clinical governance meetings with presentation of AAM cases were introduced to our organization mid-2021.
Limitations
This before and after study cannot clearly prove cause and effect of the AAM QIP and improved intubation FPS rates. However, the effect size is considerable and in keeping with previous literature. An important limitation is that the multiple aspects of the QIP were introduced in parallel, and due to the relative infrequence of intubations in our service, there is a likely delay between intervention and effect. As such, we were unable to clearly attribute changes in FPS or DASH-1A rate to individual interventions. Importantly, some of the changes made during the QIP, such as standardized equipment, the use of a pre-intubation checklist, or the use of a bougie, was not documented in individual patient charts. We were therefore unable to assess the effectiveness of these interventions individually. Finally, data completion and accuracy are well-documented challenges in retrospective database analyses. We undertook manual reviews of charts were required to minimise this issue, and the data entry and data retrieval process was the same for the pre- and post-intervention period.
Conclusions
A multi-faceted AAM QIP resulted in statistically significant increase in intubation FPS rates and a non-significant improvement in DASH-1A rates. A combination of modern equipment, targeted training, standardization, and ongoing clinical governance is required to achieve and maintain safe intubation by paramedics in the prehospital and retrieval environment.
Availability of data and materials
Research ethics approval only included the use of data for this specific research project. As such, we are unable to share our data with other researchers.
References
Powell EK, Hinckley WR, Stolz U, Golden AJ, Ventura A, McMullan JT. Predictors of definitive airway sans hypoxia/hypotension on first attempt (DASH-1A) success in traumatically injured patients undergoing prehospital intubation. Prehosp Emerg Care. 2020;24(4):470–7.
Lockey DJ, Crewdson K, Davies G, Jenkins B, Klein J, Laird C, et al. AAGBI: Safer pre-hospital anaesthesia 2017: association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2017;72(3):379–90.
Hiltunen P, Jantti H, Silfvast T, Kuisma M, Kurola J. Airway management in out-of-hospital cardiac arrest in Finland: current practices and outcomes. Scand J Trauma Resusc Emerg Med. 2016;24:49.
Crewdson K, Rehn M, Lockey D. Airway management in pre-hospital critical care: a review of the evidence for a “top five” research priority. Scand J Trauma Resusc Emerg Med. 2018;26(1):89.
Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M, Cooper DJ, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury a randomized controlled trial. Ann Surg. 2010;252(6):959–65.
Cudnik MT, Newgard CD, Daya M, Jui J. The impact of rapid sequence intubation on trauma patient mortality in attempted prehospital intubation. J Emerg Med. 2010;38(2):175–81.
Stockinger ZT, McSwain NE Jr. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56(3):531–6.
Nutbeam T. ABC of Prehosital Emergency Medicine. 1st edition ed. Chichester: Wiley-Blackwell; 2013.
von Vopelius-Feldt J, Benger J. Who does what in prehospital critical care? An analysis of competencies of paramedics, critical care paramedics and prehospital physicians. Emerg Med J. 2014;31(12):1009–13.
Louka A, Stevenson C, Jones G, Ferguson J. Intubation success after introduction of a quality assurance program using video laryngoscopy. Air Med J. 2018;37(5):303–5.
Broderick ED, Sauerberg N, Reed JJ. EMS pros and cons of drug-assisted intubation. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
von Vopelius-Feldt J, Benger JR. Prehospital anaesthesia by a physician and paramedic critical care team in Southwest England. Eur J Emerg Med. 2013;20(6):382–6.
Sunde GA, Kottmann A, Heltne JK, Sandberg M, Gellerfors M, Krüger A, et al. Standardised data reporting from pre-hospital advanced airway management: a nominal group technique update of the Utstein-style airway template. Scand J Trauma Resusc Emerg Med. 2018;26(1):46.
Reichert RJ, Gothard M, Gothard MD, Schwartz HP, Bigham MT. Intubation success in critical care transport: a multicenter study. Prehosp Emerg Care. 2018;22(5):571–7.
Rhode MG, Vandborg MP, Bladt V, Rognås L. Video laryngoscopy in pre-hospital critical care: a quality improvement study. Scand J Trauma Resusc Emerg Med. 2016;24:84.
Lyon RM, Perkins ZB, Chatterjee D, Lockey DJ, Russell MQ. Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia. Crit Care. 2015;19:134.
Fakhry SM, Scanlon JM, Robinson L, Askari R, Watenpaugh RL, Fata P, et al. Prehospital rapid sequence intubation for head trauma: conditions for a successful program. J Trauma. 2006;60(5):997–1001.
Knapp J, Eberle B, Bernhard M, Theiler L, Pietsch U, Albrecht R. Analysis of tracheal intubation in out-of-hospital helicopter emergency medicine recorded by video laryngoscopy. Scand J Trauma Resusc Emerg Med. 2021;29(1):49.
Delorenzo A, St Clair T, Andrew E, Bernard S, Smith K. Prehospital rapid sequence intubation by intensive care flight paramedics. Prehosp Emerg Care. 2018;22(5):595–601.
Price J, Lachowycz K, Steel A, Moncur L, Major R, Barnard EBG. Intubation success in prehospital emergency anaesthesia: a retrospective observational analysis of the Inter-Changeable Operator Model (ICOM). Scand J Trauma Resusc Emerg Med. 2022;30(1):44.
Mosier JM, Sakles JC, Stolz U, Hypes CD, Chopra H, Malo J, et al. Neuromuscular blockade improves first-attempt success for intubation in the intensive care unit: a propensity matched analysis. Ann Am Thorac Soc. 2015;12(5):734–41.
Wilcox SR, Bittner EA, Elmer J, Seigel TA, Nguyen NT, Dhillon A, et al. Neuromuscular blocking agent administration for emergent tracheal intubation is associated with decreased prevalence of procedure-related complications. Crit Care Med. 2012;40(6):1808–13.
Jacoby J, Heller M, Nicholas J, Patel N, Cesta M, Smith G, et al. Etomidate versus midazolam for out-of-hospital intubation: a prospective, randomized trial. Ann Emerg Med. 2006;47(6):525–30.
Macke C, Gralla F, Winkelmann M, Clausen JD, Haertle M, Krettek C, et al. Increased first pass success with C-MAC videolaryngoscopy in prehospital endotracheal intubation: a randomized controlled trial. J Clin Med. 2020;9(9).
Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The physiologically difficult airway. West J Emerg Med. 2015;16(7):1109–17.
Lockey D, Crewdson K, Weaver A, Davies G. Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians. Br J Anaesth. 2014;113(2):220–5.
Acknowledgements
We want to acknowledge the contribution of the Ornge Education Department to this publication, in particularly Sean Hackett and Michael Kennedy. We would also like to thank Mahvareh Ahghari for her help with data extraction.
Funding
None of the authors received funding for this research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. JVVF and BN collected and analysed the data and prepared the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Ornge Research and Scholarly Activities Committee and research ethics approval was granted by the University of Toronto (REB: 30628).
Consent for publication
Not applicable.
Competing interests
All authors work for Ornge in a clinical capacity and have no other competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
von Vopelius-Feldt, J., Peddle, M., Lockwood, J. et al. The effect of a multi-faceted quality improvement program on paramedic intubation success in the critical care transport environment: a before-and-after study. Scand J Trauma Resusc Emerg Med 31, 9 (2023). https://doi.org/10.1186/s13049-023-01074-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-023-01074-0