Abstract
Background
A favorable neurological outcome is closely related to patient characteristics and total cardiopulmonary resuscitation (CPR) duration. The total CPR duration consists of pre-hospital and in-hospital durations. To date, consensus is lacking on the optimal total CPR duration. Therefore, this study aimed to determine the upper limit of total CPR duration, the optimal cut-off time at the pre-hospital level, and the time to switch from conventional CPR to alternative CPR such as extracorporeal CPR.
Methods
We conducted a retrospective observational study using prospective, multi-center registry of out-of-hospital cardiac arrest (OHCA) patients between October 2015 and June 2019. Emergency medical service–assessed adult patients (aged ≥ 18 years) with non-traumatic OHCA were included. The primary endpoint was a favorable neurological outcome at hospital discharge.
Results
Among 7914 patients with OHCA, 577 had favorable neurological outcomes. The optimal cut-off for pre-hospital CPR duration in patients with OHCA was 12 min regardless of the initial rhythm. The optimal cut-offs for total CPR duration that transitioned from conventional CPR to an alternative CPR method were 25 and 21 min in patients with initial shockable and non-shockable rhythms, respectively. In the two groups, the upper limits of total CPR duration for achieving a probability of favorable neurological outcomes < 1% were 55–62 and 24–34 min, respectively, while those for a cumulative proportion of favorable neurological outcome > 99% were 43–53 and 45–71 min, respectively.
Conclusions
Herein, we identified the optimal cut-off time for transitioning from pre-hospital to in-hospital settings and from conventional CPR to alternative resuscitation. Although there is an upper limit of CPR duration, favorable neurological outcomes can be expected according to each patient’s resuscitation-related factors, despite prolonged CPR duration.
Similar content being viewed by others
Background
Longer cardiopulmonary resuscitation (CPR) duration in cases of out-of-hospital cardiac arrest (OHCA) is associated with reduced favorable neurological outcomes. Moreover, consensus is lacking regarding the optimal CPR duration before termination. Therefore, determining the upper limit of CPR duration is essential for stopping futile resuscitation efforts. Although several studies have investigated the CPR duration beyond which resuscitation may be futile, they did not include cases of in-hospital CPR duration and were based on pre-hospital CPR duration [1,2,3].
There are regional variations in emergency medical service (EMS) systems and the role of EMS providers, such as pre-hospital interventions and termination of resuscitation (TOR) [3,4,5]. Even if appropriate advanced life support is implemented, identifying and correcting all the causes of OHCA in the field is challenging.
Some studies showed that extracorporeal CPR (ECPR) for refractory cardiac arrest can obtain favorable neurological outcomes [6,7,8,9]. Moreover, in one study, insufficient short duration of CPR less than 20 min in the emergency department (ED) deceased survival to discharge [10]. These results give us the idea that we need sufficient time in-hospital CPR. Also considering ECPR is primarily provided in hospital settings, more likely to have sufficient CPR duration in hospital and prepare ECPR is necessary. Therefore, the allocation of adequate overall time for pre-hospital and in-hospital CPR is necessary.
In patients with OHCA, outcomes are associated with various factors, including age, comorbidities, initial cardiac rhythm, witnessed arrest, provision of bystander CPR, and resuscitation duration [11,12,13,14]. The optimal CPR duration to achieve a favorable neurological outcome is influenced by factors that determine resuscitation outcomes [1, 2, 15, 16]. Patients who achieve pre-hospital return of spontaneous circulation (ROSC) have better outcomes than those who do not [1, 17]. Most patients with OHCA do not achieve pre-hospital ROSC prior to hospital arrival, especially in regions where TOR is not allowed in the field.
This study aimed to identify the major factors of and determine the upper limit of total CPR duration and optimal cut-off for pre- or in-hospital total CPR duration to achieve favorable neurological outcomes.
Methods
Data source and data collection
The Korean Cardiac Arrest Research Consortium (KoCARC), a multicenter collaborative research network of 55 participating institutions, was developed to understand various studies in the resuscitation field of patients with OHCA and strengthen cooperative efforts. The KoCARC registry includes patients with OHCA of medical etiology transported to a participating ED with resuscitation efforts. The registry excludes patients with OHCA with a documented terminal illness, those under hospice care, those currently pregnant, and those with a previously documented “Do Not Resuscitate” card [18]. After 2018, advanced directives (AD) are able to guarantee the patient’s self-determination. When an AD is completed, it is registered with the National Agency for Management of Life-sustaining Treatment, and a registration card is issued [19]. This registration card is recognized as a “Do Not Resuscitate” card because it includes the rejection of CPR. Patients with OHCA of definite non-medical etiology, including trauma, drowning, poisoning, burn, asphyxia, or hanging, were also excluded [18]. Starting in October 2015, data were collected from EMS and hospital medical records via a standardized registry form and entered into a web-based electronic database registry according to Utstein style [18]. A quality management committee comprising emergency physicians, statisticians, local research coordinators, and investigators in each ED regularly monitored and reviewed the data quality [18].
Study design and setting
This retrospective observational study used a prospective, multi-center registry of OHCA patients between October 2015 and June 2019 from KoCARC. Patients aged < 18 years, for whom information or medical record data were missing, who were transferred from other hospitals, or who received ECPR were excluded. We extracted all data including baseline characteristics, pre-hospital environmental factors, EMS characteristics, laboratory data, in-hospital therapeutic interventions, CPR duration, and clinical outcomes from the KoCARC registry.
Pre-hospital CPR duration was defined as the time from the initiation of CPR to the achievement of sustained pre-hospital ROSC or hospital arrival. In-hospital CPR duration was defined as the time from the initiation of CPR at the hospital to the achievement of sustained ROSC or discontinuation of CPR. Total CPR duration was defined as the time from CPR initiation by EMS to the achievement of sustained ROSC or discontinuation of resuscitation.
The primary endpoint was a favorable neurological outcome at hospital discharge as determined by the cerebral performance category (CPC) score [20]. CPC scores of 1–2 were considered favorable, whereas those of 3–5 were considered poor neurological outcomes.
Korean EMS system
In the Republic of Korea, the EMS is a centralized governmental service provided by 16 provincial headquarters of the National Fire Department covering the entire nation [21]. As of 2019, the total surface area of Korea is 100,401.3 km2, with a population of 51,927,000. There are 12,033 paramedics and 1474 ambulances nationwide [22]. In Korea, there is no special team of doctors, and emergency medical technicians (EMTs) and nurses are in charge of dispatch. There are standard guidelines for on-site first aid from CPR in the field to hospital transportation. According to this guideline, an automated chest compression device can be used if one paramedic has to be in charge of CPR during the transfer. Additionally, the use of metronomes and chest compression quality measuring devices are recommended to monitor chest compression [23]. Two or three emergency paramedics work together, including at least one level 1 EMT who can administer intravenous fluids, perform endotracheal intubation, and apply an automatic external defibrillator (AED) on board a departing ambulance. However, the use of intravenous adrenaline is permitted only under direct medical instructions in limited locations. Paramedics are not legally allowed to declare death or terminate resuscitation attempts in the field unless the patients show obvious signs of death (e.g., corruption, rigor mortis) and medical physicians have confirmed the declaration via telephone. Therefore, most EMS-treated OHCA patients are transported to hospitals.
Statistical analyses
Overall, no imputation method for missing data was used. The chi-squared test was used to compare categorical variables between groups with favorable and unfavorable neurological outcomes. Furthermore, since continuous variables were not normally distributed, the Mann–Whitney U test was performed to analyze continuous variables. Values are presented as median (interquartile range [IQR]) for continuous variables and as percentages for categorical variables. Multivariable logistic regression was conducted for selected variables related to favorable neurological outcomes. Variables including age, sex, witnessed arrest, bystander CPR, initial shockable pre-hospital rhythm, and total CPR duration were selected based on previous studies [2, 3, 16, 24]. There were no more extra variables added to the logistic regression model.
Model calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test. As an estimate of effect size and variability, odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. We stratified patients into four subgroups by combining important variables that showed a high association with favorable outcomes based on the multivariable logistic regression analysis results.
The dynamic probability and cumulative proportion of favorable neurological outcomes at discharge were calculated for all eligible participants stratified by significant variables. The dynamic probability of favorable neurological outcome at discharge < 1% in the selected group indicates the proportion of the favorable neurological outcome at discharge was less than 1% in all patients in the selected group. The cumulative proportion > 99% refers 99% of patients with favorable neurological outcomes were discharged in the selected group. We measured the optimal cut-off time of pre-hospital and total CPR duration, which is the time of CPR duration that has maximum sensitivity and specificity for favorable neurological outcomes at discharge. The shortest distance between each point on the receiver operating characteristic curve and the upper left corner was considered the optimal cut-off CPR duration for a favorable neurological outcome at discharge.
Analyses were performed using R-project version 3.6.2 (package “rms” version 5.1), SAS (version 9.4), and SPSS version 22.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at P < 0.05.
Results
Characteristics and pre-hospital and in-hospital resuscitation-related variables
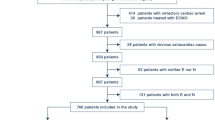
Among the 7914 participants, 577 (7.3%) had favorable neurological outcomes (Fig. 1). Baseline characteristics, resuscitation-related variables, laboratory values, and treatments were compared between patients with favorable and unfavorable outcomes (Table 1). Patients with favorable outcomes were younger, were predominantly male, had a higher rate of witnessed arrest, had a higher provision of bystander CPR, and had a pre-hospital shockable rhythm. No intergroup differences were observed in the EMS response time (from EMS call to scene arrival) or transport time (from scene departure to hospital arrival). The unfavorable neurological outcomes group had longer scene times (from scene arrival to scene departure) with a higher frequency of pre-hospital adrenaline use and pre-hospital advanced airway trials. In-patient interventions, such as therapeutic hypothermia and coronary angiography, were performed more frequently in patients with favorable neurological outcomes. Serum cardiac markers and initial serum lactate levels were lower in these patients despite higher hemoglobin and pH levels.
The patients with unfavorable neurological outcomes at discharge had longer pre-hospital and total CPR durations (median, 19.0 min [IQR 15.0–25.0] and 41.0 min [IQR 30.0–52.0], respectively) than patients with favorable neurological outcomes (median, 7.0 min [IQR 4.0–12.0] and 8.0 min [IQR 5.0–15.0], respectively).
Associated factors for favorable neurological outcomes at discharge
Table 2 shows the results of the multivariate logistic regression analysis of favorable neurological outcomes at discharge. An initial shockable rhythm (adjusted OR 10.7; 95% CI 8.0–13.9; P < 0.001) and witnessed arrest (adjusted OR 1.87; 95% CI 1.37–2.55; P < 0.001) were the main factors positively associated with favorable neurological outcomes at discharge. The total CPR duration (adjusted OR 0.89; 95% CI 0.88–0.90; P < 0.001) was inversely associated with a CPC of 1–2 at discharge. We stratified the patients into subgroups by combining the main associated factors (shockable rhythm + witnessed, non-shockable rhythm + witnessed, shockable + unwitnessed, and non-shockable + unwitnessed groups).
Dynamic probability of favorable neurological outcomes at discharge and cumulative proportion of total CPR duration
Figure 2 shows the dynamic probability and cumulative proportion of favorable neurological outcomes at discharge according to total CPR duration. After 30 min of CPR, the probability of favorable outcomes in the subgroups decreased in the following order: shockable rhythm + witnessed, shockable rhythm + unwitnessed, non-shockable rhythm + witnessed, and non-shockable rhythm + unwitnessed (21.0%, 14.6%, 1.5%, and 0.3%, respectively). After 40 min of CPR, the probabilities decreased to 8.6%, 5.1%, 0.4%, and 0.03%, respectively. For the same subgroups, the total CPR duration beyond which the dynamic probability of a favorable neurological outcome < 1% was 62 min, 55 min, 34 min, and 24 min, respectively (Fig. 2A, Additional file 1: Table S1), while the total CPR duration to achieve a > 99% cumulative proportion of a CPC of 1–2 at discharge was 53 min, 43 min, 71 min, and 45 min, respectively (Fig. 2B, Additional file 1: Table S1).
Cut-off for pre-hospital and total cpr duration for favorable neurological outcomes at discharge
Table 3 shows the cut-off for pre-hospital and total CPR duration for a favorable neurological outcome at discharge. In all patients, the cut-off for pre-hospital CPR duration for a favorable neurological outcome at discharge was 12 min regardless of the initial rhythm. In addition, the cut-offs for total CPR duration for favorable neurological outcomes at discharge were 25 min for patients with initial shockable rhythms and 21 min for patients with non-shockable rhythms. When pre-hospital ROSC was achieved, the minimum cut-offs for the pre-hospital CPR duration were 10 and 12 min in patients with shockable and non-shockable rhythms, respectively. However, when pre-hospital ROSC was not achieved, the cut-offs for pre-hospital and total CPR duration were 14 and 36 min in patients with shockable rhythm and 12 and 26 min in patients with non-shockable rhythm, respectively.
Dynamic probability and cumulative proportion of favorable neurological outcomes at discharge by total CPR duration in patients without pre-hospital ROSC
After 30 min of CPR, the probability of a favorable outcome according to the total CPR duration decreased to 8.7% and 0.7% in the shockable and non-shockable rhythm groups, respectively. The total CPR duration beyond which the dynamic probability of a favorable neurological outcome < 1% were 54 and 28 min, respectively, while the total CPR duration to achieve a > 99% cumulative proportion of a CPC of 1–2 at discharge were 83 min and 71 min, respectively (Fig. 3).
Discussion
This multicenter retrospective observational study based on reliable pre-hospital and in-hospital variables showed that the upper limits of resuscitation times and optimal pre-hospital and total CPR durations differed among the stratified groups by major determinant factors. Similar to other studies [2, 3, 16, 24], an initial shockable rhythm and witnessed arrest were major factors determining favorable neurological outcomes. This study showed that males had a high likelihood of favorable neurological outcomes. However, there were some etiological differences according to sex. The males were younger and likely to have initial shockable rhythms (Additional file 2: Table S2). These differences made male patients seem to have a better prognosis.
In this study, the upper limit of total CPR duration in the shockable rhythm group (55–62 min) was longer than that in the non-shockable rhythm group (24–34 min), a finding that was similar to the results of Grunau et al. [24], who showed that the total CPR duration with a probability of favorable neurological outcomes < 1% were 48 and 15 min in the shockable and non-shockable rhythm groups, respectively. The reason for this is the difference in the characteristics of shockable and non-shockable rhythms. A shockable rhythm is caused by electrical changes due to myocardial ischemia, while a non-shockable rhythm is caused by poor perfusion and tissue hypoxia due to non-cardiac causes or spontaneous or electrical termination of shockable rhythm. Patients with an initial non-shockable rhythm may have more comorbidities and delayed initial recognition and response [25, 26]. Therefore, favorable neurological outcomes are more likely in patients with a shockable rhythm, even if prolonged CPR is required. Different CPR durations are recommended for different patient groups stratified by their characteristics.
Grunau et al. recommended that patients be transported to hospitals for ECPR within 8–24 min [27]. Similarly, we recommend 12 min as the optimal pre-hospital CPR duration cut-off, within which patients with OHCA should be transported to the hospital for evaluation of the cause of the OHCA and clinical decisions about ECPR implementation. Furthermore, this study showed that total CPR durations of 25 and 21 min are optimal for transitioning to ECPR and achieving favorable neurological outcomes in patients with shockable and non-shockable rhythms. Similarly, Kim et al. showed that the optimal cut-off for total conventional CPR is 21 min, beyond which ECPR should be considered [7]. Moreover, French medical scientific societies recommend ECPR in patients with refractory cardiac arrest with CPR performed for > 30 min [28]. ECPR implemented within 60 min results in favorable neurological outcomes [6, 7, 29]. In patients with an initial shockable rhythm with and without witnessed arrest, we revealed that total CPR for 62 min and 55 min, respectively, are the upper limits of conventional CPR for the dynamic probability of favorable neurological outcomes < 1%. This finding supports the hypothesis that implementing ECPR within 60 min of cardiac arrest in selected patients with an initial shockable rhythm may result in favorable neurological outcomes. In most cases, a shockable rhythm is caused by ischemic events that maintain myocardial viability and have a good response to ECPR. Although the effectiveness of ECPR in patients with a non-shockable rhythm is debatable, several studies have shown favorable neurological outcomes in patients with non-shockable rhythms [7,8,9]. We showed that the upper limit of total CPR duration in patients with an initial non-shockable rhythm with or without witnessed arrest are 34 and 24 min, respectively. The effect of ECPR is considered negligible after this time, which is similar to that observed in patients with an initial shockable rhythm. Although there are differences in the time interval from team activation to ECMO pump “ON” time due to regional variations in EMS systems, it usually takes > 20 min. Therefore, in patients with a non-shockable rhythm, ECPR should be considered quickly because they have a shorter time window for ECPR compared than those with a shockable rhythm.
Drennan et al. [30] disclosed that the application of the basic life support TOR rule (arrest not witnessed by EMS personnel, no ROSC, and no AED shock) at 20 min of resuscitation identified > 99% of survivors and favorable neurological outcomes. Similarly, we showed that the upper limit of total CPR duration for patients with an initial non-shockable rhythm with or without witnessed arrest were 34 and 24 min, respectively. Therefore, it might be feasible to apply the TOR rule within this time window to patients with a non-shockable rhythm in the field. However, the total CPR duration with a cumulative proportion of favorable neurological outcomes > 99% in patients with an initial non-shockable rhythm with and without witnessed arrest was 71 and 45 min, respectively. Thus, if prolonged CPR is performed, some patients with an initial non-shockable rhythm may have favorable neurological outcomes. Similarly, in patients with an initial shockable rhythm but without pre-hospital ROSC, the total CPR duration with a > 99% cumulative proportion of favorable neurological outcomes was 83 min, while the dynamic probability of < 1% favorable neurological outcomes was 54 min. Therefore, we recommend that treatment not be abandoned too early, even in patients with an initial non-shockable rhythm and in those without pre-hospital ROSC.
There have been many attempts to determine the upper limit of CPR duration beyond which resuscitation may be futile [1,2,3,4, 16, 17, 24]. Some studies focused on the upper limit of the pre-hospital CPR duration [1,2,3]. Even if few of these studies focused on total CPR duration, they excluded patients who underwent TOR in the field [4, 16, 24] and included patients who received bystander CPR only [17]. In conclusion, they determined the upper limit of CPR duration in limited patient groups. Conversely, this study focused on patients who did not experience TOR in the field and included all patients who underwent CPR by EMS at the pre-hospital level. Likewise, the present study could aid healthcare providers more clearly determine the appropriate duration of CPR performed at the pre-hospital level and the time to transfer from conventional CPR to ECPR in the hospital within the upper limit of CPR duration.
Limitations
This study had some limitations. First, we included all OHCA patient data but did not consider the no-flow time that could affect favorable neurological outcomes. Second, CPR quality (compression rate, depth, and fraction rate) in pre-hospital and in-hospital settings can affect neurological outcomes; however, data in the KoCARC registry to estimate this are insufficient. Third, all patients, except those with traumatic OHCA, were enrolled in this study. Therefore, etiology may be a confounding factor affecting CPR duration and OHCA outcomes. Finally, the impact of witnessed arrest on the dynamic probability and cumulative proportion of favorable neurological outcomes was confirmed in all patients with OHCA but not in those without pre-hospital ROSC or an optimal cut-off time for favorable neurological outcomes. The OR of witnessed arrest (1.87) was less than that of the initial shockable rhythm (10.56). Since the impact of witnessed arrest on the dynamic probability and cumulative proportion of favorable neurological outcomes was small irrespective of the total CPR duration, this probably did not significantly impact the study results.
Conclusions
The optimal cut-off for total CPR duration to achieve favorable neurological outcomes was 21–25 min. Thereafter, the effect of conventional CPR may decline, and the use of alternative CPR methods, such as ECPR, are recommended. Although the upper limits for CPR duration in patients with initial shockable and non-shockable rhythms are 55–62 min and 24–34 min, respectively, favorable neurological outcomes can be achieved with prolonged CPR according to each patient’s resuscitation-related factors.
Availability of data and materials
The data that support the findings of this study are available from the Korean Cardiac Arrest Research Consortium, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Korean Cardiac Arrest Research Consortium.
Abbreviations
- AD:
-
Advanced directives
- AED:
-
Automated external defibrillator
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass graft
- CAG:
-
Coronary angiography
- CI:
-
Confidence interval
- CPC:
-
Cerebral performance category
- CPR:
-
Cardiopulmonary resuscitation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- ED:
-
Emergency department
- EMS:
-
Emergency medical service
- EMT:
-
Emergency medical technician
- ICD:
-
Implantable cardioverter defibrillator
- IQR:
-
Interquartile range
- KoCARC:
-
Korean Cardiac Arrest Research Consortium
- OHCA:
-
Out-of-hospital cardiac arrest
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- PEA:
-
Pulseless electrical activity
- PVT:
-
Pulseless ventricular tachycardia
- ROSC:
-
Return of spontaneous circulation
- TOR:
-
Termination of resuscitation
- TPA:
-
Tissue plasminogen activator
- VF:
-
Ventricular fibrillation
References
Goto Y, Funada A, Goto Y. Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: a prospective, nationwide, population-based cohort study. J Am Heart Assoc. 2016;5: e002819.
Nagao K, Nonogi H, Yonemoto N, Gaieski DF, Ito N, Takayama M, et al. Duration of prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation. 2016;133:1386–96.
Funada A, Goto Y, Tada H, Teramoto R, Shimojima M, Hayashi K, et al. Duration of cardiopulmonary resuscitation in patients without prehospital return of spontaneous circulation after out-of-hospital cardiac arrest: results from a severity stratification analysis. Resuscitation. 2018;124:69–75.
Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128:2488–94.
Girotra S, van Diepen S, Nallamothu BK, Carrel M, Vellano K, Anderson ML, et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133:2159–68.
Sakamoto T, Morimura N, Nagao K, Asai Y, Yokota H, Nara S, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2014;85:762–8.
Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. 2014;18:535.
Nee J, Koerner R, Zickler D, Schroeder T, Enghard P, Nibbe L, et al. Establishment of an extracorporeal cardio-pulmonary resuscitation program in Berlin—outcomes of 254 patients with refractory circulatory arrest. Scand J Trauma Resusc Emerg Med. 2020;28:96.
Conrad SA, Rycus PT. Extracorporeal membrane oxygenation for refractory cardiac arrest. Ann Card Anaesth. 2017;20:S4-10.
Cha WC, Lee EJ, Hwang SS. The duration of cardiopulmonary resuscitation in emergency departments after out-of-hospital cardiac arrest is associated with the outcome: a nationwide observational study. Resuscitation. 2015;96:323–7.
Adrie C, Cariou A, Mourvillier B, Laurent I, Dabbane H, Hantala F, et al. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J. 2006;27:2840–5.
Goto Y, Maeda T, Goto Y. Decision-tree model for predicting outcomes after out-of-hospital cardiac arrest in the emergency department. Crit Care. 2013;17:R133.
Maupain C, Bougouin W, Lamhaut L, Deye N, Diehl JL, Geri G, et al. The CAHP (Cardiac Arrest Hospital Prognosis) score: a tool for risk stratification after out-of-hospital cardiac arrest. Eur Heart J. 2016;37:3222–8.
Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81.
Adnet F, Triba MN, Borron SW, Lapostolle F, Hubert H, Gueugniaud PY, et al. Cardiopulmonary resuscitation duration and survival in out-of-hospital cardiac arrest patients. Resuscitation. 2017;111:74–81.
Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016;134:2084–94.
Matsuyama T, Kitamura T, Kiyohara K, Nishiyama C, Nishiuchi T, Hayashi Y, et al. Impact of cardiopulmonary resuscitation duration on neurologically favourable outcome after out-of-hospital cardiac arrest: a population-based study in Japan. Resuscitation. 2017;113:1–7.
Kim JY, Hwang SO, Shin SD, Yang HJ, Chung SP, Lee SW, et al. Korean Cardiac Arrest Research Consortium (KoCARC): rationale, development, and implementation. Clin Exp Emerg Med. 2018;5:165–76.
Lee JE, Goo A, Shin DW, Yoo JH, Korean Geriatrics Society End-of-Life Research. Korean medical professionals’ attitudes and experiences on advance care planning for noncancerous disease. Ann Geriatr Med Res. 2019;23:63–70.
Rittenberger JC, Raina K, Holm MB, Kim YJ, Callaway CW. Association between Cerebral Performance Category, Modified Rankin Scale, and discharge disposition after cardiac arrest. Resuscitation. 2011;82:1036–40.
Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013;84:547–57.
National Emergency Medical Center (KR). Statistical yearbook of emergency medical service, 2019. https://www.e-gen.or.kr/nemc/statistics_annual_report.do. Accessed 15 Dec 2021.
National Fire Agency (KR). Paramedics on-site first aid standard guideline, 2020. https://www.nfa.go.kr/nfa/publicrelations/legalinformation/0017/0003/?boardId=bbs_0000000000001097&mode=view&cntId=4&category=&pageIdx=&searchCondition=&searchKeyword=. Accessed 15 Dec 2021.
Grunau B, Reynolds JC, Scheuermeyer FX, Stenstrom R, Pennington S, Cheung C, et al. Comparing the prognosis of those with initial shockable and non-shockable rhythms with increasing durations of CPR: informing minimum durations of resuscitation. Resuscitation. 2016;101:50–6.
Luqman N, Sung RJ, Wang CL, Kuo CT. Myocardial ischemia and ventricular fibrillation: pathophysiology and clinical implications. Int J Cardiol. 2007;119:283–90.
Myerburg RJ, Halperin H, Egan DA, Boineau R, Chugh SS, Gillis AM, et al. Pulseless electric activity: definition, causes, mechanisms, management, and research priorities for the next decade: report from a National Heart, Lung, and Blood Institute workshop. Circulation. 2013;128:2532–41.
Grunau B, Reynolds J, Scheuermeyer F, Stenstom R, Stub D, Pennington S, et al. Relationship between time-to-ROSC and survival in out-of-hospital cardiac arrest ECPR candidates: when is the best time to consider transport to hospital? Prehosp Emerg Care. 2016;20:615–22.
French Ministry of Health. Guidelines for indications for the use of extracorporeal life support in refractory cardiac arrest. Ann Fr Anesth Reanim. 2009;28:182–90.
Lee SW, Han KS, Park JS, Lee JS, Kim SJ. Prognostic indicators of survival and survival prediction model following extracorporeal cardiopulmonary resuscitation in patients with sudden refractory cardiac arrest. Ann Intensive Care. 2017;7:87.
Drennan IR, Case E, Verbeek PR, Reynolds JC, Goldberger ZD, Jasti J, et al. A comparison of the universal TOR Guideline to the absence of prehospital ROSC and duration of resuscitation in predicting futility from out-of-hospital cardiac arrest. Resuscitation. 2017;111:96–102.
Acknowledgements
We would like to acknowledge and thank the investigators from all participating hospitals in KoCARC, the steering committee, the National Fire Agency for providing pre-hospital EMS data, and the Korean Association of Cardiopulmonary Resuscitation for their support.
Funding
This work was supported by a Korea University grant funded by Korea University (#K2014021) and a research grant (#NRF-2019R1A2C1007110) funded by the National Research Foundation of Korea. Su Jin Kim received funding from Korea University and the National Research Foundation of Korea. This funding source had no role in the study design, data collection, data analysis, data interpretation, or report writing.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: SJ Kim, EJ Lee. Data curation: SJ Lee, DH Jang. Formal analysis: SJ Park. Funding acquisition: SJ Kim. Investigation: SJ Lee, DH Jang. Methodology: SJ Kim. Software: JS Lee. Validation: SJ Kim, SW Lee. Supervision: SW Lee, Visualization: DH Jang, EJ Lee. Writing—original draft: Park SJ. Writing—review & editing: SJ Kim. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The KoCARC data collection protocol was reviewed and approved by the institutional review board of each participating hospital. The KoCARC registry was registered at clinicaltrials.gov (protocol NCT03222999). This study was approved by the Institutional Review Board of Korea University (2021AN0141).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Probability of favorable neurological outcome (A) and cumulative proportion (B) of favorable neurological outcome at discharge by total CPR duration stratified by initial shockable rhythm and witnessed arrest
Additional file 2: Table S2.
Comparison of characteristics by sex
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, S., Lee, S.W., Han, K.S. et al. Optimal cardiopulmonary resuscitation duration for favorable neurological outcomes after out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med 30, 5 (2022). https://doi.org/10.1186/s13049-022-00993-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-022-00993-8