Abstract
Background
Diabetes-related foot disease (DFD) is a common, costly, and severe complication of diabetes mellitus. DFD is associated with high rates of morbidity and mortality and poses a significant burden on patients, healthcare systems and society. While the detrimental impact of DFD is widely recognised, the precise financial implications of its management in Australia remain unclear due to inconsistent and inconclusive contemporary data. Therefore, the aim of this review was to identify, summarise and synthesise existing evidence to estimate the costs associated with DFD management in Australia.
Methods
Searches were conducted in MEDLINE, Embase, AMED, CINAHL, Joanna Briggs Institute EBP, and the Cochrane Library from November 2011 to July 2023. Australian studies investigating costs associated with DFD management were eligible for inclusion. Two independent reviewers performed the study selection, data extraction and quality assessment steps. The Consolidated Health Economic Evaluation Reporting Standards (CHEERS 2022) checklist was used to assess study quality. A descriptive analysis was performed due to limited existing evidence and large heterogeneity between study populations to conduct meta-analyses.
Results
Three economic evaluations were included in the review. One study was rated as ‘poor’, one as ‘very good’ and one as ‘excellent’ when assessed against the CHEERS checklist. The estimated cost of DFD management varied between studies and comparisons were not possible due to the different methodological approaches and data sources. The studies were unable to provide an overall cost of DFD with respect to all aspects of care as they did not capture the multi-faceted level of care throughout the entire patient journey between sectors and over time.
Conclusion
There is limited contemporary evidence for the costs associated with DFD management within Australia, particularly related to direct costs and resource utilisation. Further research into the economic impact of DFD management is needed to inform optimisation of national service delivery and improve health outcomes for individuals with DFD in Australia. Integrating real-world data on impact of clinical interventions with parallel economic evaluation could be a valuable approach for future research, which would offer a more comprehensive understanding of the clinical and economic outcomes beyond solely model-based evaluations.
Trial registration
PROSPERO Registration No. CRD42022290910.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Diabetes mellitus affects over 537 million people worldwide and is associated with high morbidity and mortality [1]. A debilitating sequela of this chronic condition is diabetes-related foot disease (DFD), which is a limb-threatening complication encompassing diabetes-related foot ulceration (DFU), infection, ischaemia, and lower limb amputation [2]. DFD is a leading cause of hospitalisation, lower limb amputations, and is a large contributor to the global disability burden [2,3,4,5,6,7,8,9].
Prevalence studies have shown that DFU affects 6.3% of the global diabetes population [8] and has a lifetime incidence in people with diabetes between 19 to 34% [2, 10]. DFU recurrence is also frequent, where 40% of ulcers will reoccur within one year and 65% within three years [2, 10]. In Australia, the prevalence of DFD ranges from 1.2 to 1.5%, while the incidence of diabetes-related lower limb amputations is between 5.2 to 7.2 per 1000 person-years. DFD-related hospital admissions are common in Australians with diabetes and range from 5.2 to 36.6 per 1000 person-years [11].
The financial burden associated with DFD management varies greatly between countries and is contingent on many variables such as patient factors (e.g. ulcer severity), interventions used, and the length of stay for DFD-related hospital admissions for specialised care and rehabilitation [11]. Healthcare costs associated with DFD management may include medical appointments, wound care products and consumables, medications, pressure offloading and prosthetic devices, diagnostic tests, hospitalisations, and surgical interventions [12, 13].
In the United States (US), the direct annual costs for diabetes management is estimated at USD$237 billion, where one third is attributable to DFD [14]. Expenditure for DFD in the United Kingdom (UK) is estimated to be between £837 to £962 million per year (data from 2014–2015) [13]. In Europe, the total direct and indirect costs associated with DFD management (at the individual level) is between €7,722 to €20,064 per annum [15]. While the economic impact of DFD management has been well established in other countries [13,14,15], contemporary cost data within Australia remains ambiguous. Foot disease is considered to be one of the most costly acute complications of diabetes [16, 17]. Estimates of the direct costs for DFD management to the public hospital system and overall health system in Australia have been reported to be AUD$348 million and AUD$1.57 billion, respectively [18]. However, this data is based on modelling from a point prevalence study of less than 900 inpatients and extrapolated nation-wide. This included assumptions that every hospital had 600 inpatient beds and the average stay for DFD was 29 occupied bed days across all sites. As these assumptions resulted in a total of 4,385 hospital total bed days, this ultimately led to the AUD$1.57 billion cost estimate [19].
Considering the increasing prevalence of DFD and high rates of recurrence, it is unsurprising that the costs associated with its management are substantial. Hence, it is imperative to ascertain the current financial burden of DFD management within Australia. This is particularly important for ensuring optimal national service delivery and policy development for the provision of prevention strategies and best practice management. Consequently, the aim of this systematic review was to identify, summarise and synthesise existing evidence to estimate the costs associated with DFD management in Australia.
Methods
Registration
This systematic review was prospectively registered with The International Prospective Register of Systematic Reviews (PROSPERO)—Registration No. CRD42022290910. Detailed methods have been published elsewhere [20]. This review is reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines [21].
Search strategy
Searches were conducted in MEDLINE (Ovid), Embase (Ovid), AMED (Ovid), CINAHL (EBSCO), Joanna Briggs Institute EBP (Ovid), and the Cochrane Library from 1 November 2011 to 23 November 2021 without language restriction. The MEDLINE search strategy is available in the protocol article [20]. To ensure literature saturation, citation tracking was performed using Google Scholar and reference lists were screened for studies not identified in the initial search. The searches were re-run to 20 July 2023 (i.e. search timeframe 1 November 2011 to 20 July 2023) to ensure any new studies were captured in this review prior to publication.
Eligibility criteria
Peer-reviewed Australian studies investigating costs associated with DFD management between November 2011 to November 2021 were eligible for inclusion. Searches were re-run to 20 July 2023 to ensure all contemporary data were included. A ten-year timeframe was chosen to ensure current cost estimates within Australia were captured. For clarity, this timeframe was extended by 20 months (i.e. searches were re-run up to July 2023) prior to manuscript submission for publication.
The population of interest were adults with DFD (i.e. DFU, infection, ischaemia, amputation) in any clinical setting. All reported costs for DFD management were considered, however, costs of particular interest were visits to a healthcare professional, consumables (e.g., wound dressings, footwear, offloading and prosthetic devices), anti-infective agents, diagnostic tests/imaging, and/or surgical procedures (e.g., debridement, amputation). Single case reports/studies/series, expert opinion level V studies, protocols, abstracts without full text, conference proceedings, literature reviews, case–control, validity or reliability studies, letters, editorials, notes, and short surveys were excluded.
Data management
All citations were initially exported into EndNote 20 (Thomson Reuters, New York, USA) for automated removal of duplicates. To conduct the study selection process, the remaining unique citations were imported into the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) and any further identified duplicates were removed.
Study selection
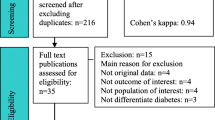
The Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) was used by two independent reviewers during the study selection process to screen titles and abstracts (NF and LS) and to perform the full-text review (NF and MRK). Conflicts were discussed and resolved at each stage of the study selection process. The above method was repeated for the citation tracking and bibliographic reference scanning steps [20].
Data extraction
A pre-specified data extraction form was implemented to extract relevant study information, participant characteristics and reported costs associated with DFD management (Table 1). Data extraction was performed by two authors (NF and MRK) and checked for accuracy and omissions by another author (LS). For further information on the data extraction process, we refer the reader to our protocol article [20]. On our request, authors from one study [22] provided their raw cost data.
Quality appraisal and risk of bias
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 checklist [23] was used to appraise study quality and risk of bias. The checklist contains 28 items that are specific to economic evaluations of health interventions [23]. Studies were assessed independently against the CHEERS checklist by two authors (NF and MRK) and a score was calculated out of 28. Based on the methods of a previous systematic review [24], studies were allocated one-point if the criterion was met in full (represented by ✓), 0.5-points if the criterion was partially met (represented by ≠) or 0-points if the criterion was not met (represented by ×) (Table 2). The total score was reduced by one-point for each criterion that was classified as not applicable (represented by N/A). Following the calculation of a percentile score, studies were classified as ‘excellent’ quality if scored 85% or higher, ‘very good’ quality if 70–85%, ‘good’ quality if 55–70% and ‘poor’ quality if below 55% [24].
Data synthesis
A descriptive analysis was performed due to limited existing evidence (n = 3) and large heterogeneity between study populations, methodology and data sources to conduct meta-analyses. To ensure that all cost data were reported in this review, the authors of one study [22] were contacted, of which the authors provided their raw data.
Results
Study characteristics
The study selection process followed the PRISMA guidelines (Fig. 1). The database searches identified 4,080 unique citations, however only one study initially met the eligibility criteria [22]. Through citation tracking and screening of reference lists, two additional studies were identified [24, 25]. Upon full-text review, one study [25] met the eligibility criteria, while the other [24] was deemed ineligible. After re-running the searches to 20 July 2023, three more articles [9, 26, 27] were identified. One study [26] satisfied the eligibility criteria, while two studies [9, 27] were excluded on full-text review. Overall, only three articles [22, 25, 26] satisfied the eligibility criteria and were included in the review. The characteristics of included studies are presented in Table 1.
Cheng et al. [22] adopted a healthcare system perspective to present a hypothetical cohort of people with diabetes mellitus at high risk of developing DFUs (i.e. those with previous DFU or amputation). Markov cohort simulations were used to evaluate the cost-effectiveness of ‘optimal care’ (including components of foot examination, debridement, wound dressings, pressure offloading, infection management and multidisciplinary care) versus ‘usual care’ for DFD management. The model used seven possible health states including: no DFU, uncomplicated DFU, complicated DFU with infection, post minor amputation, infected post minor amputation, post major amputation, and death. Model inputs were informed by published Australian and international literature, the Medicare Benefits Scheme (MBS), the Pharmaceutical Benefits Scheme (PBS), the Australian Refined Diagnosis Related Group (AR-DRG) codes, and by expert opinion. Separate simulations were also conducted for three age groups (35–54 years, 55–74 years, and 75 + years). The model presented AUD 2013 prices with a discount rate of 5% [22].
The study [22] presented costs for optimal care versus usual care across the three age groups and considered the following DFD costs: consultations with a general practitioner, podiatrist and/or multidisciplinary care team, consumables (e.g. scalpel blades for debridement, wound dressings), pressure offloading devices (e.g. Aircast), footwear, pathology, radiology, anti-microbials, and hospital costs associated with minor or major amputations (e.g. home care, prostheses, inpatient and outpatient care) [22].
Graves and Zheng [25] used a probabilistic model to estimate the direct healthcare costs for treatments of four categories of chronic wounds (i.e. pressure ulcers, DFUs, venous ulcers and arterial ulcers) in hospital and residential care settings in Australia for 2010–2011. The parameters of the model included the incidence of the wounds, and the associated direct healthcare costs in the healthcare setting (e.g. hospital separations). Hospital separation was defined as an episode of admitted patient care, which was either total or part of a hospital stay (e.g. from acute care to rehabilitation). Model inputs were informed from a systematic literature search. Where Australian data were not available, international estimates were used for the economic modelling. Hospital separation data were sourced from the Australian Hospital Statistics 2010–2011 [29]. For patients with diabetes, hospital separation data were derived from Diabetes Hospitalisations in Australia 2003–2004 and Australian demographic statistics 2011 [30, 31]. The hospital separation data for the residential care setting were derived from the Australian residential aged care statistical review 2010–2011 [32]. The model reported the costs in USD 2012 prices. The types of DFU treatments and services provided were not reported [25].
Zhang et al. [26] employed a healthcare system perspective to present a prospective cohort of patients with DFU attending multiple outpatient Diabetic Foot Services. They used a discrete event simulation model based on a state-based Markov model previously described by Cheng et al. [22], to estimate the costs and quality-adjusted life years (QALYs) of seven hypothetical scenarios with increasing proportions of guideline-based care. The scenarios represented discrete episodes of disease which included healed DFU, recurrent DFU, hospitalisation (no amputation), minor amputation, major amputation, and death. The cost-effectiveness of each scenario was estimated by comparing to current practice. The definition of current practice (i.e. 30% of patients receiving guideline-based care and 70% receiving suboptimal care) was based on the observed findings of the authors’ prospective patient cohort [26, 33, 34].
The model incorporated inputs related to time-to-event, resource use and costs, and types of services. Two categories of costs were considered: care costs in the outpatient Diabetic Foot Services and event costs for hospitalisation (no amputation), minor amputation, and major amputation in an inpatient setting. The study used average weekly episode care costs for the outpatient Diabetic Foot Services, which were based on healthcare consultations, consumables (such as dressings), pressure offloading devices, footwear and antibiotics. Event costs associated with hospitalisation and for minor and major amputation procedures were estimated using national hospital pricing data based on AR-DRG codes. The model presented AUD 2020 prices with a discount rate of 5% per year. Comparisons were made between guideline-based care and current practice for the seven scenarios [26].
Quality appraisal and risk of bias
The included studies [22, 25, 26] were appraised according to the CHEERS 2022 checklist [23]. Table 2 provides the details of the quality appraisal. Cheng et al. [22] scored 22 (78.6%) out of a possible 28 and was rated as ‘very good’ on quality assessment. Graves and Zheng [25] scored 12 (50.0%) out of a possible 24 and was rated as ‘poor’ on quality assessment. Zhang et al. [26] scored 23.5 (90.4%) out of a possible 26 and was rated as ‘excellent’ on quality assessment. Across the three studies, 12 items were met in full (items 2–4, 7,11–16, 23, 26), five items were not met (items 18, 21, 25), and there was variation between studies for the remaining items (Table 2). Overall, items relating to the selection, measurement and valuation of outcomes, the measurement and valuation of resources and costs, the currency, price date and conversions, and the rationale and description of the model were addressed well, while the items concerning heterogeneity and the approach/effect of engagement with patients and stakeholders was lacking.
Economic evaluation characteristics
The study information, participant characteristics, costs of DFD (including unit costs) and economic evaluation characteristics are summarised in Table 1.
Cheng et al. [22] evaluated the cost-effectiveness of implementing optimal care versus usual care. Overall, the provision of optimal care for DFD using national evidence-based guidelines [28] yielded less costs than providing usual care, where the total five-year cost savings per patient (in AUD 2013) were $9,100 for the 35–54 years age group (0.13 QALYs), $9,392 for 55–74 years (0.13 QALYs) and $12,395 for 75 + years (0.16 QALYs). Five-year cost estimates per patient ranged from $6,681 to $7,066 for optimal care versus $15,781 to $19,461 for usual care. When costs were analysed according to age groups, estimated costs per patient rose with increasing age in both the optimal and usual care groups (Table 3).
Graves and Zheng [25] estimated total hospital care costs (in USD 2012) to be $238.69 million (standard deviation [SD], 123.98 million) and residential care costs to be $11 million (SD, 3.01 million). The total healthcare costs of DFU in both hospital and residential care settings was $249.67 million (SD, 124.02 million) [25].
Zhang et al. [26] used real-world cohort data obtained from the Queensland High Risk Foot Database in Australia. Overall, the provision of 100% guideline-based care (based on international guidelines [35]) over a three-year time horizon yielded a cost saving (in AUD 2020) of $1,843 per patient and an additional 0.056 QALYs per person. The total cost for current practice over a three-year period was estimated to be $49,918 per patient. The breakdown of costs was $15,065 for outpatient DFU care, $27,916 for hospitalisation, $4,521 for minor amputation, and $2,415 for major amputation. Comparatively, the optimal scenario with 100% guideline-based care estimated total costs to be $48,075 per patient; $22,872 attributed to outpatient DFU care, $19,949 for hospitalisation, $3,313 for minor amputation, and $1,940 for major amputation. The cost estimates pertaining to all seven scenarios (i.e. 40%-100% of patients receiving guideline-based care) are outlined in Table 4. In the majority of scenarios, total costs reduced with increasing proportions of guideline-based care (average cost saving between $278 and $1,381 per person). The costs of outpatient DFU care increased with larger proportions of guideline-based care received, but this was offset by reduced costs pertaining to DFU-related hospitalisations as well as for minor and major amputation procedures [26].
Discussion
Summary of findings
This systematic review aimed to identify, summarise, and synthesise existing evidence to estimate the costs associated with DFD management in Australia. Our findings revealed a paucity of contemporary evidence on the financial burden of DFD within Australia, particularly in relation to the frequency and variation of services and resources required. Furthermore, there is variation in the reported cost estimates within the Australian literature. Despite the limited evidence at present, this review found that by adhering to evidence-based guidelines, health outcomes can be improved and can bear significant cost savings for the Australian healthcare system.
The variation of reported DFD cost estimates within the Australian literature could be attributed to the differing methodological approaches seen within the included studies, such as the characteristics of study cohorts, the definitions of care/comparators used, the sources of the cost data, and the analyses performed. While the two cost-effectiveness analyses [22, 26] comparing ‘usual care’ to ‘guideline-based care’ used similar modelling methods, the first study [22] used a hypothetical cohort of patients with diabetes at high risk of developing DFUs, while the second study [26] used a large prospective real-world cohort of people with DFU attending Diabetic Foot Services within one state of Australia. As observed in the latter study [26], the method of using individual patient-level data (as opposed to aggregated data) may have better informed the model parameters for guideline-based care versus current practice (i.e. usual care) thus reducing the risk of sampling bias associated with trial-informed time-to-event parameterisation [22, 26]. In addition, the patient-level data allowed for use of a discrete event simulation model in this study, with the flexibility to add specific attributes to each person simulated in the model [26].
When comparing the reported costs for DFD in these cost-effectiveness studies, the first study [22] estimated a total five-year cost per patient (expressed in 2013 AUD) to be between $15,781 and $19,461 (~ $3,156 to $3,892 per year) for usual care, and between $6,681 and $7,066 (~ $1,336 to $1,413 per year) for guideline-based care. The second study [26] estimated a total three-year cost per patient (expressed in 2020 AUD) of $49,918 (~ $16,639 per year) for current practice (i.e. sub-optimal care) and $48,075 (~ $16,025 per year) for guideline-based care. Even despite the inflation of costs between 2013 and 2020, the largely differing cost estimates reported in these studies may also be explained by their respective definitions of ‘guideline-based care’. The first study [22] defined guideline-based care as per the optimal care program outlined in the 2011 National Evidence-based Guideline: Prevention, Identification and Management of Foot Complications in Diabetes [28], while the second study [26] defined guideline-based care as per the core principles of DFU care outlined in international guidelines [35] and included costs associated with healthcare consultations, consumables (i.e. dressings, pressure offloading devices, footwear) and antibiotics. This study [26] further defined healthcare consultations, whereby all visits must have been ≤ 21 days since the previous visit and ≥ 75% of visits must have documented ulcer classification, sharp debridement, appropriate wound dressings, knee-high offloading, and antibiotics prescribed (only if the wound was classified as infected) [26]. Based on the two studies’ definitions of guideline-based care, particularly in relation to the frequency of healthcare consultations, it is apparent that the latter study [26] was more comprehensive in its approach to DFU care than the former study [22]. Hence why the cost estimates may have been significantly larger in this study. It is also important to note that the earlier study [22] reported costs in 2013 AUD, while the other [26] reported costs in 2020 AUD. Therefore, the cost estimates of the earlier study [22] may not be as representative of the current economic burden of DFD. Importantly, both studies [22, 26] demonstrated overall cost savings and improved health outcomes associated with guideline-based care compared to usual care. Accordingly, it is likely that the increase in outpatient costs to perform guideline-based care in these studies were offset by the reduced costs associated with DFU-related hospitalisation and costs of minor and major amputation procedures [26].
The third study [25] included in this review used probabilistic economic modelling to estimate and compare healthcare costs for chronic wounds (including DFUs) in hospital and residential care settings in Australia. In 2012, it was estimated that the total cost for DFU management in hospitals was more than USD$238 million (~ $18,591 per patient), while the total cost in residential care was close to USD$11 million (~ $21,315 per patient). Based on the average conversion rate in 2012 (i.e.1 AUD = 1.0358 USD) [36], this equates to a cost of ~ AUD$17,948 per patient in the hospital setting and ~ AUD$20,578 per patient in the residential care setting. While this study has shown that a large proportion of costs associated with DFD management are incurred in the hospital system (as opposed to residential care services), it is important to consider that these estimates may not be a true reflection of the cost burden in Australia; a large proportion of the inputs for the economic model (i.e. unit costs and incidence of DFU) were informed from international studies, rather than from Australian data. Furthermore, the reported cost estimates showed large standard deviations, which also adds to the uncertainty of the economic modelling in this study [25].
One limitation of all three studies is the reliance on international data to inform specific model inputs, due to the limited published Australian cost and resource utilisation data available. This lack of local data is likely due to fragmented DFD care provision often seen in Australia, but particularly for Aboriginal and/or Torres Strait Islander Peoples [37]. For example, DFD care is commonly shared in the community by general practitioners, podiatrists and nurses, and/or within hospital outpatient specialist clinics and high-risk foot services in the public health system [22, 38]. This lack of local data is further compounded by the limited rebateable services for DFD care, resulting in difficulties for relevant data to be collated and applied to economic evaluations. When comparing Australian and international economic evaluations, it is apparent that data collection methods in Australia may be lacking, particularly when compared to the US and the UK [39, 40]. A more comprehensive system to record item numbers and resources utilised for DFD care within the overall Australian healthcare system may enable a more realistic and representative cost estimate to be determined. With the inception of the National Association of Diabetes Centres (NADC) High Risk Foot Services database [41], and in combination with International Classification of Diseases codes from tertiary care, this could address some of these knowledge gaps, particularly surrounding service provision and resource utilisation within hospital outpatient services across Australia. However, a gap in resource utilisation still remains with DFD services accessed in the community.
Another finding of this review was the variation between the three studies in which Australian healthcare settings (i.e. cost data sources) were included. The first study [22] that used a hypothetical cohort sourced health system data from the Medicare Benefits Scheme (MBS) and the Pharmaceutical Benefits Scheme (PBS), which only partially covers costs of healthcare services and consumables. The second study [26] that used a large prospective real-world cohort presented two categories of care costs, including outpatient DFU services and event costs for hospitalisation and for minor and major amputations in an inpatient setting. This study sourced health system data from the Independent Hospital Pricing Authority and the PBS. For the hospital outpatient data (i.e. from Diabetic Foot Services) this was obtained from only one state in Australia. Therefore, the cost estimates may not be representative of outpatient DFU services throughout Australia. Finally, the third study [25] used total cost data limited to residential care facilities and hospital admissions, therefore, the estimated DFD care costs did not include costs of services and resources from the broader community or outpatient setting. Interestingly, none of the included studies were able to provide an overall cost estimate of DFD with respect to all aspects of care as they did not capture the multi-faceted level of community care throughout the entire patient journey between sectors and over time.
In reference to other Australian studies that were excluded from this review, two out of the three studies (excluded following full-text review) did not provide specific information or costings for DFD management, while the third [24] was a systematic review that included duplicate data from one of our already included studies [22]. Wilkie et al. [27] aimed to determine the actual cost of wound care using a survey to identify the number, type of wounds and their treatment costs including consumables and labour in Australian hospitals, residential aged care facilities, general practitioners, and community providers. Although the data collected on foot ulcers was categorised by the underlying aetiology (e.g. ischaemic, neuropathic, neuro-ischaemic), it was not clear which of these ulcers were directly attributed to DFD, and therefore, this study was excluded. Rather than an economic evaluation of the financial burden of DFD, Ahmed et al. [42] estimated the prevalence of DFD and the sociodemographic and health-related characteristics among people aged 45 years and over in New South Wales, Australia.
There are many challenges when reviewing economic health evaluations due to substantial variability in the standard of care across and within healthcare systems [43]. Economic health evaluations based on assumptions and probabilities of disease states have inherent limitations. They rely on making projections and estimated costs based on various assumptions. These limitations are due to unpredictable factors such as uncertainty of the actual course of the disease, assumptions of human behaviour such as adherence with preventative measures, or data reliability which may affect the accuracy and reliability of the evaluations. It is also acknowledged that systematic reviews of economic evaluations commonly have wide variations in population characteristics, study settings and healthcare systems, therefore reviews are unlikely to generate a one size fits all analysis regarding cost-effectiveness and their comparators [43,44,45].
Limitations and strengths
While this systematic review was designed to be comprehensive in capturing contemporary data for the costs associated with DFD management within the Australian context, its findings should be considered in relation to several limitations. First, the quality of the evidence in this review is limited by the small number of included studies. While there were only three economic evaluations identified, two were rated as either ‘very good’ or ‘excellent’ on quality assessment, therefore the findings from these studies [22, 26] are likely to be valid. Second, studies eligible for inclusion in the review were exclusively from Australia, and therefore, cost comparisons with other countries were not extrapolated. Third, searches were limited to the last decade, as we wanted to ensure that cost estimates were representative of present day. Therefore, not all economic evaluations conducted in Australia may have been included in this review. Fourth, as only three studies met the eligibility criteria and there was heterogeneity of the data, pooling of cost data in meta-analyses was not possible. Fifth, we did not find any published Australian data concerning indirect costs (e.g. cessation or reduction of work productivity) associated with DFD management, therefore, only the direct costs have been presented.
That being said, there are several notable strengths of this review. A robust and comprehensive search strategy was employed, and pre-determined decision rules were followed throughout all stages [20]. For example, the study selection, data extraction and quality appraisal steps were conducted by two independent reviewers, with conflicts resolved through consultation with a third party. The reporting of data and the results underwent cross-checking by all authors, ensuring we were transparent and unbiased in our findings.
Future directions
This systematic review has demonstrated the paucity of evidence regarding not only the costs of DFD management, but also the frequency and variations of services and resources required for management of this patient cohort. There is also a lack of data comparing Australians living in metropolitan, regional or remote communities, and in particular the First Nations population. Of the few studies conducted on DFD prevalence in Australia [8, 11, 42, 46], the data obtained has been predominantly from hospital-based diabetes populations and defined geographic areas, so they may not be reflective of the overall DFD burden within Australian communities [9].
Given the detrimental impact of DFD and its substantial financial burden on the Australian healthcare system, there is a pressing requirement for further economic evaluations utilising up-to-date Australian data. The recent publication of the 2021 evidenced-based Australian guidelines for diabetes-related foot disease [47,48,49,50,51,52] may inform future Australian economic evaluations concerning the cost-effectiveness of implementing these guidelines (versus usual care), which may prove invaluable for informing national service delivery and improving health and economic outcomes. Within future economic evaluations, it is also crucial to consider the diverse cultural backgrounds, geographic locations and socioeconomic disparities within Australia, as these factors play an important role in evaluating cost implications. Since the Australian DFD guidelines were adapted from international guidelines and tailored to the Australian context by incorporating considerations for First Nations peoples and those living in rural and remote regions, there is now an opportunity to conduct cost-effectiveness analyses for guideline-based care with the Australian context in mind.
To produce robust baseline data across Australia against which improvement to care, access, management and surveillance can be benchmarked, data capture using compatible systems that incorporate the entire patient journey between sectors and over time would be required. Such data could also be used to compare with other countries.
Ideally, the total cost of DFD should be established to understand the true financial impact of DFD to the Australian healthcare system. Data inputs for economic modelling should include the cost of the multidisciplinary team, equipment/consumables, diagnostic tests, medications, hospital and procedure costs, and labour costs. In the absence of alternative data sources to inform these parameters, an additional approach may be to obtain clinical expert opinion to generate estimates of resource utilisation. Multisource data is required to inform real-world resource utilisation and costs associated with care for patients with DFD. This information would enable policy makers the financial incentive to improve access to optimal care for DFD and ultimately reduce the financial burden to both the patient and the Australian healthcare system.
Conclusions
This review has demonstrated the paucity of contemporary evidence for not only the cost of DFD management within Australia, but also the frequency and variation of services and resources required. While economic evaluations based on assumptions and probabilities of disease states have inherent limitations, they do provide an estimate of the burden, which can be further improved with real-world data. The research to date has highlighted variation in cost estimates for DFU management within Australia. Further research into the economic impact of DFD management and resource utilisation using a national database that captures costs throughout the entire clinical journey between sectors and over time is needed to inform optimisation of national service delivery (e.g. guideline-based care) and to improve health outcomes. Despite the limited evidence at present, this review found that by adhering to evidence-based guidelines, health outcomes can be improved and can bear significant cost savings for the Australian healthcare system.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- AR-DRG:
-
Australian Refined Diagnosis-Related Groups
- AUD:
-
Australian Dollar
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- CKD:
-
Chronic Kidney Disease
- CVD:
-
Cardiovascular Disease
- DFD:
-
Diabetes-Related Foot Disease
- DFU:
-
Diabetes-Related Foot Ulceration
- DM:
-
Diabetes Mellitus
- ESRD:
-
End-Stage Renal Disease
- GP:
-
General Practitioner
- ICER:
-
Incremental Cost-Effectiveness Ratio
- MBS:
-
Medicare Benefits Scheme
- NADC:
-
National Association of Diabetes Centres
- NMB:
-
Net Monetary Benefit
- PBS:
-
Pharmaceutical Benefits Scheme
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- QALY:
-
Quality-Adjusted Life Years
- SD:
-
Standard Deviation
- UK:
-
United Kingdom
- US:
-
United States
- USD:
-
United States Dollar
References
International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels, Belgium: International Diabetes Federation; 2021. Available from: https://www.diabetesatlas.org.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–75. https://doi.org/10.1056/NEJMra1615439.
Lazzarini PA, Hurn SE, Kuys SS, Kamp MC, Ng V, Thomas C, et al. The silent overall burden of foot disease in a representative hospitalised population. Int Wound J. 2017;14(4):716–28. https://doi.org/10.1111/iwj.12683.
Lazzarini PA, Pacella RE, Armstrong DG, van Netten JJ. Diabetes-related lower-extremity complications are a leading cause of the global burden of disability. Diabet Med. 2018;35(9):1297–9. https://doi.org/10.1111/dme.13680.
Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care. 2020;43(5):964–74. https://doi.org/10.2337/dc19-1614.
Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res. 2018;28(6):1413–27. https://doi.org/10.1007/s11136-018-2082-2.
Raghav A, Khan ZA, Labala RK, Ahmad J, Noor S, Mishra BK. Financial burden of diabetic foot ulcers to world: a progressive topic to discuss always. Ther Adv Endocrinol Metab. 2018;9(1):29–31. https://doi.org/10.1177/2042018817744513.
Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017;49(2):106–16. https://doi.org/10.1080/07853890.2016.1231932.
Ahmed MU, Tannous WK, Agho KE, Henshaw F, Turner D, Simmons D. The burden of diabetes-related foot disease among older adults in Australia. Int Wound J. 2022;19(7):1758–68. https://doi.org/10.1111/iwj.13781.
Bus SA, Sacco ICN, Monteiro-Soares M, Raspovic A, Paton J, Rasmussen A, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2023 update) Diabetes Metab Res Rev. 2023;11:e3651. https://doi.org/10.1002/dmrr.3651.
Zhang Y, van Netten JJ, Baba M, Cheng Q, Pacella R, McPhail SM, et al. Diabetes-related foot disease in Australia: a systematic review of the prevalence and incidence of risk factors, disease and amputation in Australian populations. J Foot Ankle Res. 2021;14(1):8. https://doi.org/10.1186/s13047-021-00447-x.
Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: The economic case for the limb salvage team. J Vasc Surg. 2010;52(3):17S–22S. https://doi.org/10.1016/j.jvs.2010.06.003.
Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995–1002.
Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. 2020;13(1):16. https://doi.org/10.1186/s13047-020-00383-2.
Prompers L, Huijberts M, Schaper N, Apelqvist J, Bakker K, Edmonds M, et al. Resource utilisation and costs associated with the treatment of diabetic foot ulcers Prospective data from the Eurodiale Study. Diabetologia. 2008;51(10):1826–34. https://doi.org/10.1007/s00125-008-1089-6.
Clarke PP, Leal JM, Kelman CP, Smith MP, Colagiuri SF. Estimating the cost of complications of diabetes in Australia using administrative health-care data. Value Health. 2008;11(2):199–206. https://doi.org/10.1111/j.1524-4733.2007.00228.x.
Lazzarini PA, Gurr JM, Rogers JR, Schox A, Bergin SM. Diabetes foot disease: the Cinderella of Australian diabetes management? J Foot Ankle Res. 2012;5(1):24. https://doi.org/10.1186/1757-1146-5-24.
van Netten JJ, Lazzarini PA, Fitridge R, Kinnear E, Griffiths I, Malone M, et al. Australian diabetes-related foot disease strategy 2018–2022: The first step towards ending avoidable amputations within a generation. Brisbane: Diabetic Foot Australia, Wound Management CRC, Australia; 2017. Available from: https://www.diabeticfootaustralia.org/for-researchers/australian-diabetes-related-foot-disease-strategy-2018-20222018.
Lazzarini PA. The burden of foot disease in inpatient populations [PhD by Publication]. QUT ePrints: Queensland Univeristy of Technology; 2016.
Frescos N, Jansen S, Stopher L, Kaminski MR. The financial burden of diabetes-related foot disease in Australia: a protocol for a systematic review. Wound Pract Res. 2022;30(4):223–7.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. https://doi.org/10.1136/bmj.g7647.
Cheng Q, Lazzarini PA, Gibb M, Derhy PH, Kinnear EM, Burn E, et al. A cost-effectiveness analysis of optimal care for diabetic foot ulcers in Australia. Int Wound J. 2017;14(4):616–28. https://doi.org/10.1111/iwj.12653.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMC Med. 2022;20(1):23. https://doi.org/10.1186/s12916-021-02204-0.
Woods T-J, Tesfay F, Speck P, Kaambwa B. Economic evaluations considering costs and outcomes of diabetic foot ulcer infections: A systematic review. PLoS ONE. 2020;15(4):e0232395. https://doi.org/10.1371/journal.pone.0232395.
Graves N, Zheng H. Modelling the direct healthcare costs of chronic wounds in Australia. Wound Practice & Research. 2014;22(1):20–33. https://doi.org/10.3316/informit.272218893716909.
Zhang Y, Carter HE, Lazzarini PA, Cramb S, Pacella R, van Netten JJ, et al. Cost-effectiveness of guideline-based care provision for patients with diabetes-related foot ulcers: A modelled analysis using discrete event simulation. Diabet Med. 2023;40(1):e14961. https://doi.org/10.1111/dme.14961.
Wilkie J, Carville K, Fu SC, Kerr R, Finlayson K, Tuffrey T, et al. Determining the actual cost of wound care in Australia. Wound Practice Research. 2023;31(1):7–18.
Baker IDI Heart and Diabetes Institute. National evidence-based guideline on prevention, identification and management of foot complications in diabetes (part of the National Health & Medical Research Council Approved Guidelines on Management of Type 2 diabetes). Melbourne: Baker IDI Heart & Diabetes Institute; 2011.
Australian Institute of Health and Welfare. Australian hospital statistics 2010–11. Canberra: AIHW; 2012.
Australian Institute of Health and Welfare, O'Brien K, Thow A, Ofei S. Diabetes hospitalisations in Australia, 2003–04. Canberra: AIHW; 2006.
Australian Bureau of Statistics (ABS), Australian demographic statistics 2011. Canberra: ABS; 2011.
Australian Institute of Health and Welfare. Residential aged care in Australia 2010–11: a statistical overview. Canberra: AIHW; 2012.
Zhang Y, Cramb S, McPhail SM, Pacella R, van Netten JJ, Cheng Q, et al. Factors associated with healing of diabetes-related foot ulcers: observations from a large prospective real-world cohort. Diabetes Care. 2021;44(7):e143–5. https://doi.org/10.2337/dc20-3120.
Zhang Y, Cramb S, McPhail SM, Pacella R, van Netten JJ, Cheng Q, et al. Multiple factors predict longer and shorter time-to-ulcer-free in people with diabetes-related foot ulcers: Survival analyses of a large prospective cohort followed-up for 24-months. Diabetes Res Clin Pract. 2022;185:109239. https://doi.org/10.1016/j.diabres.2022.109239.
Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):1–10.
Reserve Bank of Australia. Exchange rates – Daily – 2010 to 2013. Available from: https://www.rba.gov.au/statistics/historical-data.html.
Chuter V, West M, Hawke F, Searle A. Where do we stand? The availability and efficacy of diabetes related foot health programs for Aboriginal and Torres Strait Islander Australians: a systematic review. J Foot Ankle Res. 2019;12(1):17. https://doi.org/10.1186/s13047-019-0326-1.
Norman RE, Gibb M, Dyer A, Prentice J, Yelland S, Cheng Q, et al. Improved wound management at lower cost: a sensible goal for Australia. Int Wound J. 2016;13(3):303–16. https://doi.org/10.1111/iwj.12538.
Rice JB, Desai U, Cummings AKG, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37(3):651–8. https://doi.org/10.2337/dc13-2176.
Guest JF, Fuller GW, Vowden P. Diabetic foot ulcer management in clinical practice in the UK: costs and outcomes: Health economic impact of DFUs in the UK. Int Wound J. 2018;15(1):43–52. https://doi.org/10.1111/iwj.12816.
Lasschuit JWJ, Wischer N, Andrikopoulos S, Frank G, Lazzarini PA, Twigg S. The Australian Diabetes Foot Registry: Standardising national data collection and key learnings from our inaugural report. In: The 9th International Symposium on the Diabetic Foot: 2023: The Hague, The Netherlands.
Ahmed MU, Tannous WK, Agho KE, Henshaw F, Turner D, Simmons D. Prevalence and burden of diabetes-related foot disease in New South Wales, Australia: Evidence from the 45 and up study survey data linked with health services data. Int J Environ Res Public Health. 2021;18(21):11528. https://doi.org/10.3390/ijerph182111528.
Jacobsen E, Boyers D, Avenell A. Challenges of systematic reviews of economic evaluations: A review of recent reviews and an obesity case study. Pharmacoeconomics. 2020;38(3):259–67. https://doi.org/10.1007/s40273-019-00878-2.
Gomersall JS, Jadotte YT, Xue Y, Lockwood S, Riddle D, Preda A. Conducting systematic reviews of economic evaluations. Int J Evid Based Healthc. 2015;13(3):170-8. https://doi.org/10.1097/XEB.0000000000000063.
Chapel JM, Wang G. Understanding cost data collection tools to improve economic evaluations of health interventions. Stroke Vasc Neurol. 2019;4(4):214–22. https://doi.org/10.1136/svn-2019-000301.
Australian National Diabetes Audit. Australian Quality Clinical Audit 2021 Annual Report. Australian Government Department of Health; 2021.
Kaminski MR, Golledge J, Lasschuit JWJ, Schott K-H, Charles J, Cheney J, et al. Australian guideline on prevention of foot ulceration: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15(1):53. https://doi.org/10.1186/s13047-022-00534-7.
Chen P, Carville K, Swanson T, Lazzarini PA, Charles J, Cheney J, et al. Australian guideline on wound healing interventions to enhance healing of foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15(1):40. https://doi.org/10.1186/s13047-022-00544-5.
Chuter V, Quigley F, Tosenovsky P, Ritter JC, Charles J, Cheney J, et al. Australian guideline on diagnosis and management of peripheral artery disease: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15(1):51. https://doi.org/10.1186/s13047-022-00550-7.
Fernando ME, Horsley M, Jones S, Martin B, Nube VL, Charles J, et al. Australian guideline on offloading treatment for foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15(1):31. https://doi.org/10.1186/s13047-022-00538-3.
Commons RJ, Charles J, Cheney J, Lynar SA, Malone M, Raby E, et al. Australian guideline on management of diabetes-related foot infection: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15(1):47. https://doi.org/10.1186/s13047-022-00545-4.
Hamilton EJ, Scheepers J, Ryan H, Perrin BM, Charles J, Cheney J, Twigg SM, Australian Diabetes-related Foot Disease Guidelines & Pathways Project. Australian guideline on wound classification of diabetes-related foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2021;14(1):60. https://doi.org/10.1186/s13047-021-00503-6.
Acknowledgements
Not applicable.
Funding
An unconditional grant was received from Urgo Medical Australia, however they had no role in the conceptualisation, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
NF, MRK, LS and SJ conceived the idea for the study and contributed to the design. NF and LS performed the title and abstract review, with conflicts resolved by MRK. NF and MRK performed the full-text review, within conflicts resolved by LS. NF and MRK extracted the data, with conflicts resolved by LS. NF and MRK assessed the methodological quality, with conflicts resolved by LS. NF and MRK were involved in the formal analysis and interpretation of the data. NF and MRK drafted the manuscript with input from LS and SJ. All authors approved the final version of the manuscript and take full responsibility for the integrity and accuracy of all aspects of the review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Frescos, N., Stopher, L., Jansen, S. et al. The financial burden of diabetes-related foot disease in Australia: a systematic review. J Foot Ankle Res 16, 92 (2023). https://doi.org/10.1186/s13047-023-00688-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13047-023-00688-y