Abstract
Background
The role of allogeneic hematopoietic cell transplantation (alloHCT) in acute myeloid leukemia (AML) with mutated IDH1/2 has not been defined. Therefore, we analyzed a large cohort of 3234 AML patients in first complete remission (CR1) undergoing alloHCT or conventional chemo-consolidation and investigated outcome in respect to IDH1/2 mutational subgroups (IDH1 R132C, R132H and IDH2 R140Q, R172K).
Methods
Genomic DNA was extracted from bone marrow or peripheral blood samples at diagnosis and analyzed for IDH mutations with denaturing high-performance liquid chromatography, Sanger sequencing and targeted myeloid panel next-generation sequencing, respectively. Statistical as-treated analyses were performed using R and standard statistical methods (Kruskal–Wallis test for continuous variables, Chi-square test for categorical variables, Cox regression for univariate and multivariable models), incorporating alloHCT as a time-dependent covariate.
Results
Among 3234 patients achieving CR1, 7.8% harbored IDH1 mutations (36% R132C and 47% R132H) and 10.9% carried IDH2 mutations (77% R140Q and 19% R172K). 852 patients underwent alloHCT in CR1. Within the alloHCT group, 6.2% had an IDH1 mutation (43.4% R132C and 41.4% R132H) and 10% were characterized by an IDH2 mutation (71.8% R140Q and 24.7% R172K). Variants IDH1 R132C and IDH2 R172K showed a significant benefit from alloHCT for OS (p = .017 and p = .049) and RFS (HR = 0.42, p = .048 and p = .009) compared with chemotherapy only. AlloHCT in IDH2 R140Q mutated AML resulted in longer RFS (HR = 0.4, p = .002).
Conclusion
In this large as-treated analysis, we showed that alloHCT is able to overcome the negative prognostic impact of certain IDH mutational subclasses in first-line consolidation treatment and could pending prognostic validation, provide prognostic value for AML risk stratification and therapeutic decision making.
Similar content being viewed by others
Background
Isocitrate dehydrogenase (IDH) gene mutations are among the most common genetic alterations in acute myeloid leukemia (AML), detected in 15–20% of patients with AML [1, 2]. They represent mutational alterations in early leukemogenesis [3]. Still, their prognostic and predictive relevance is not fully resolved and standard AML risk stratification does not yet include IDH1 or IDH2 mutations [4]. However, there is growing evidence that IDH mutations contribute both prognostic and predictive value [2, 5, 6]. There have been inconsistent results regarding outcome, including complete remission (CR) rate, relapse-free survival (RFS) and overall survival (OS) depending on IDH1 and IDH2 mutational status, respectively [2, 7,8,9,10,11,12]. For example, some reports attribute a favorable prognosis to IDH mutations [8, 13], whereas other reports indicate an adverse prognosis for patients with IDH mutations [2, 10, 14,15,16]. Furthermore, some data suggest the existence of IDH mutations have no impact on survival [11, 12]. Supposedly, this is based on different biologic features of certain subtypes of mutations and co-mutational patterns.
To date, two isoforms of IDH are known to be potentially mutated in AML encoded on chromosome 2 band q33 (IDH1) and chromosome 15 band q26 (IDH2), respectively [15, 17, 18]. IDH1 is localized in the cytoplasm and IDH2 is found in mitochondria [19]. Their physiologic role is the enzymatic involvement in the citrate metabolism (Krebs cycle) catalyzing decarboxylation of isocitrate to α-ketoglutarate (α-KG) in an NADP+ associated manner. IDH mutations induce the loss of this catalytic activity, leading to reduction of α-KG and to the production of the oncometabolite 2-hydroyglutarate (2-HG) accumulating in leukemic cells [20, 21]. 2-HG potentially alters gene expression via DNA and histone hypermethylation and hereby blocks differentiation of hematopoietic progenitor cells [7, 22].
During the last decade, certain mutational subtypes including hotspot mutations affecting codon 132 of IDH1, as well as codon R140 and R172 of IDH2 were identified and have been associated with differential enzymatic potential, consequently suggesting these variants to contribute to disease heterogeneity as well as to contradictions in prognostic predictions [19, 23, 24].
From a therapeutic point of view, they represent attractive drugable targets in clinical routine, as IDH inhibitors (e.g., ivosidenib for IDH1 mutations and enasidenib for IDH2 mutations) have been introduced for patients with relapsed or refractory AML (r/r AML) and/or elderly/frail AML patients as firstline therapy harboring IDH mutations with promising results regarding response and survival [25,26,27]. Recent reports also demonstrated promising results with the combination of IDH inhibitors and hypomethylating agents as frontline therapy [28, 29]. Further, IDH inhibitors are investigated in prospective clinical phase I and II trials as maintenance therapy after allogeneic hematopoietic cell transplantation (alloHCT) and/or salvage strategies in case of relapse in the posttransplant setting (e.g., NCT03564821 and NCT04522895).
So far, the role of alloHCT for IDH mutated (IDHmut) AML patients is based on reports from studies with rather small patient numbers or from monocentric analyses [30, 31]. The aim of this study was to evaluate the predictive impact of defined IDH mutational subgroups on outcome of alloHCT in first complete remission (CR1) after intensive induction therapy in a well-defined, large multi-center cohort of IDHmut AML patients.
Patients and methods
Patients
For analysis, we studied a cohort that comprised a total of 3234 intensively treated AML patients under 70 years who either underwent alloHCT (n = 852) or chemo-consolidation (n = 2382) in CR1. Only patients with sufficient material of bone marrow (BM) and/or peripheral blood (PB) samples available were included in this study. Patients were enrolled within the prospective SAL AML registry (NCT03188874) or one of the following clinical trials: AML96 [32], AML2003 [33], AMLCG1999 [34], AML60+ [35], AMLCG2008 [36], and SORAML [37] (Additional file 1: Table S1). Briefly, intensive chemotherapy regimens consisted of anthracyclines combined with cytarabine in standard dosing. Patients were not treated with IDH1- or IDH2-inhibitors. Treatment response and outcome measures were classified according to standard criteria [4, 38, 39]. All patients gave their written informed consent on analyses of data. The study was approved by the respective ethics committees and conducted in accordance to the Declaration of Helsinki.
Molecular and cytogenetic analyses
Pre-treatment BM or PB samples were used for genomic DNA isolation. After DNA extraction, samples were screened for IDH1 and IDH2 mutations. Samples collected until 2016 were analyzed in a batched fashion, from 2016 onwards, samples were analyzed in real time. AML patients treated within trials of the SAL registry were screened by denaturing high-performance liquid chromatography (DHPLC) as previously described [40]. In case of aberrant DHPLC-chromatograms, samples were analyzed either by Sanger sequencing or by sensitive ultradeep next-generation sequencing (NGS) [41]. Another NGS-based myeloid panel approach (TruSight Myeloid Panel, Illumina, San Diego, CA, USA) focusing on genes frequently mutated in hematopoietic myeloid entities was used for a subset of SAL registry AML patients [42]. Concordant results were obtained in all SAL patient samples when samples were analyzed with both methods. Concordance was analyzed based on a set of 50 samples representing all mutational variants. A custom targeted NGS assay was deployed for patients enrolled in AML-CG trials [43]. Further mutational profiles (e.g., FLT3 and NPM1 mutations) were analyzed as described previously [44, 45]. The lower limit of detection was determined with 0.1% for ultradeep NGS and 1–5% for DHPLC and panel NGS.
Statistical analyses
Statistical as-treated analyses on the impact of different IDH1 or IDH2 mutational subclasses were carried out using the free statistical computing environment R (Version 4.0.3). Continuous variables were compared using the Kruskal–Wallis test, while the Chi-square test was used to compare categorical variables between mutational groups. OS is reported for the whole cohort from study entry until date of death and was censored on date of last follow-up, if no death occurred; RFS is reported from date of CR1 until disease relapse or death and was censored on date of last follow-up. CR and survival rates were evaluated according to the current standard ELN criteria [4]. Effects of alloHCT were estimated using Cox regression models with alloHCT modeled as time-dependent covariate. Simon–Makuch plots were applied to visualize survival according to transplant status. To reduce bias toward benefit of alloHCT due to very early deaths of patients, landmarks of three months for OS (estimated time including two courses of induction therapy and scheduling alloHCT) and one month for RFS (anticipated time from CR1 after induction therapy until alloHCT) were implemented. Due to the time-dependent modeling of alloHCT, all patients start in the non-alloHCT group. Therefore, number at risk in the non-alloHCT groups at start of observational period includes also patients transplanted later. Number at risk of the alloHCT groups at time 0 reflects the number of patients at risk that changed from the non-alloHCT group to the alloHCT group until the first event or censoring was observed in that group, but not earlier than the landmark. Cox regression was also applied to identify independent prognostic variables for survival and to estimate univariate and adjusted hazard ratios (HR). Multivariable analysis included alloHCT in CR1, age at diagnosis, ELN risk group, secondary AML, therapy-related AML and ECOG performance status at diagnosis. The significance level was set at 0.05. For interaction analysis, we used multivariate Cox proportional hazard regression to analyze survival with respect to several variables simultaneously and to provide the hazard ratio for each factor. Furthermore, we performed multivariate Cox regression analysis to study the effect of the interaction of alloHCT and the respective IDH submutational groups on outcome.
Results
Patients’ characteristics
The study cohort consisted of 3234 patients with AML, whereof a total of 852 patients received alloHCT in CR1 after intense induction therapy. Patients carrying an IDHmut were significantly older than patients carrying the wildtype allele (IDHWT) (p < 0.001). Compared to IDHWT and IDH1mut, patients with IDH2mut were characterized by a significantly lower serum LDH (p = 0.012), whereas IDH1mut patients showed a median higher count of peripheral blasts compared to IDHWT and IDH2mut patients (p < 0.001) and bone marrow blasts (p < 0.001) at diagnosis, respectively. Regarding other laboratory findings, IDH1mut and IDH2mut patients had comparable platelet counts at diagnosis, which were significantly higher than those found in IDHWT patients (< 0.001). The IDHmut cohort harbored a significantly lower rate of complex karyotypes (p < 0.001), with IDH1mut patients being associated with the lowest rate. Also, patients harboring IDH1 mutations were more likely to be associated with the ELN2017 favorable-risk and less likely associated with the ELN 2017 adverse-risk category (p < 0.001), while patients without IDH mutations and IDH2mut patients showed similar distributions. No differences in gender, AML subtype (de novo AML, secondary AML, therapy-related AML), white blood count or hemoglobin were detected between IDHmut and IDHWT patients. An overview of relevant results is depicted in Table 1.
IDH mutations and mutational subgroups
In our cohort of AML patients undergoing either alloHCT or chemo-consolidation in CR1, 18.4% (n = 596) had an IDHmut with a median variant allele frequency (VAF) of 39% (IQR 26.2–43.2) for IDH1 and 38.1% (IQR 31.7–43.6) for IDH2. A total of 7.8% (n = 253) had mutated IDH1, 10.9% (n = 353) had mutated IDH2, while 0.3% (n = 10) had mutations in both IDH1 and IDH2. The most common IDH1 mutational subgroups were R132C (36%) and R132H (47%), while R132G, R132L and R132S were present in only few patients (7%, 5% and 6%, respectively). The two most frequent IDH2 mutations were R140Q (77%) and R172K (19%) with only a minority of patients (4%) carrying R140G, R140L, R140W, R172S, V161L or WT subtypes.
The patients’ distributions were as follows (Fig. 1): Among the 852 patients undergoing alloHCT in CR1, 16.2% (n = 138) harbored an IDHmut. Here, a similar distribution of IDHmut could be seen: 6.2% (n = 53) harbored an IDH1 mutation, and again the two major subgroups were R132C (43.4%) and R132H (41.5%) with small numbers of patients mutated in R132G, R132L and R132S (1.9%, 9.4% and 3.8%, respectively). IDH2 mutations were found in 10% (n = 85) of alloHCT patients, also with similar distributions of IDH2 subgroups R140Q (71.8%) and R172K (24.7%), with a minority of patients carrying R140L (2.4%) and R140W (1.2%). No patients of the alloHCT group had mutations in both IDH1 and IDH2. The non-alloHCT consolidation group included 19.2% (n = 458) IDHmut patients. Among these patients, 8.4% (n = 200) and 11.3% (n = 268) carried IDH1 and IDH2 mutations, respectively. Only a minority were characterized by mutations in both IDH1 and IDH2 (0.4%). In line with the data of the alloHCT group, the two major IDH1 subgroups in the non-alloHCT cohort were R132C (34.5%) and R132H (48%) and few patients harbored R132G, R132L and R132S (8%, 3.5% and 6%, respectively). Comparing the alloHCT and the non-alloHCT group regarding IDH mutational distribution, the alloHCT cohort was characterized by a significant lower percentage of IDH1 mutations (p = 0.042), while there was no statistically differential distribution of IDH2 mutations between these two groups (p = 0.306).
Co-mutational characteristics
Regarding co-mutational aspects, the majority of the study cohort had at least two different mutations, with only 3.5% of the IDHWT patients, 0.9% of patients carrying an IDH1mut and none of the patients with an IDH2mut without any co-mutation at all (p = 0.012). On the other hand, significant results could be found in the following co-mutational pairs: a significantly higher rate of concomitant NPM1 mutations was seen in IDHmut patients, with IDH1mut patients being characterized by the highest rate of co-occurring NPM1 mutations (IDH1mut 59.1% vs. IDH2mut 45.3% vs. IDHWT 32%, p < 0.001). In contrast, the FLT3-ITD co-mutational frequency was not significantly different between IDHWT and IDHmut patients (p = 0.741). Despite small number of events, other mutations affecting signaling still showed significant lower rates in the presence of IDHmut, including mutations in NRAS (IDH1mut 6.1% vs. IDH2mut 5.6% vs. IDHWT 12.3%, p = 0.006). Biallelic mutations in CEBPA were found with a significantly lower frequency in IDHmut patients (IDH1mut 0.5% vs. IDH2mut 1.1% vs. IDHWT 6.4%, p < 0.001). Further, we detected possible co-mutational patterns with tumor suppressors like WT1 (IDH1mut 1.7% vs. IDH2mut 2.2% vs. IDHWT 7%, p = 0.006). Epigenetic modifiers like mutations in DNMT3A and TET2 were also significantly differentially mutated according to IDHmut status (IDH1mut 26.1% vs. IDH2mut 32.8% vs. IDHWT 17.4%, p < 0.001 and IDH1mut 3.5% vs. IDH2mut 7.2% vs. IDHWT 12.4%, p = 0.003, respectively). Also, mutations in transcription factor GATA2 and cohesion complex STAG2 significantly differed between the IDHmut and IDHWT population (IDH1mut 0.9% vs. IDH2mut 2.2% vs. IDHWT 6.5%, p = 0.005 and IDH1mut 4.3% vs. IDH2mut 6.7% vs. IDHWT 2.9%, p = 0.029, respectively). An overview of co-mutational distributions is given in Fig. 2 and Table 2.
Heatmap of frequent co-mutations according to IDH mutation status. Heatmap grouped for epigenetic, signaling, transcription, cohesion and splicing pathways of AML patients achieving CR1 with IDH wildtype (IDH-wt) or mutated IDH (IDH-mut). Only patients from the SAL registry with a full dataset of myeloid panel sequencing were included
Impact of alloHCT on survival according to IDH mutational subgroups
Regarding the whole cohort undergoing alloHCT or conventional chemo-consolidation in CR1, a significant survival benefit for alloHCT in both IDHWT and IDHmut group was revealed (Fig. 3). This positive effect for alloHCT is valid for OS (HR = 0.8, 95% CI 0.69–0.96, p = 0.012; Fig. 3a), as well as RFS (HR = 0.6, 95% CI 0.54–0.73, p < 0.001; Fig. 3b). Median OS was 49 months (IDHWT non-alloHCT) versus 46 months (IDHmut non-alloHCT) versus 110 months (IDHWT alloHCT), while the IDHmut cohort receiving alloHCT did not reach median OS. Median RFS was 17 months (IDHWT non-alloHCT) versus 17 months (IDHmut non-alloHCT) vs. 74 months (IDHWT alloHCT), while median RFS was also not reached in the IDHmut cohort receiving alloHCT. Interestingly, when undergoing alloHCT, a trend toward better OS and RFS could be detected in the IDHmut group compared with the IDHWT group. Vice versa, a negative trend for survival was revealed in IDHmut patients compared with IDHWT patients when receiving chemo-consolidation only (Fig. 3). Overall, there was no statistical difference in OS of either consolidation strategy for patients carrying an IDH1 mutation (5-year OS 40% [non-alloHCT] vs. 47% [alloHCT], p = 0.27; Fig. 4a), alloHCT led to a better RFS in univariate analysis (5-year RFS 30% [non-alloHCT] vs. 51%, p = 0.009; Fig. 4b). In contrast, IDH2mut patients gained an advantage in OS when undergoing alloHCT in univariate analysis (5-year OS 46% [non-alloHCT] vs. 61% [alloHCT], p = 0.026; Fig. 4a) and RFS was significantly better for alloHCT in multivariable analysis (5-year RFS 30% [non-alloHCT] vs. 60% [alloHCT]; HR = 0.49, 95% CI 0.3–0.8, p = 0.004; Fig. 4b).
Overall survival and relapse-free survival according to IDH mutation status and allogeneic hematopoietic cell transplantation in CR1. Simon–Makuch plots for a overall survival and b relapse-free survival of AML patients with IDH wildtype (WT) or mutated (mut) IDH treated with allogeneic hematopoietic cell transplantation (blue for IDHWT and violet for IDHmut) or conventional consolidation (red for IDHWT and green for IDHmut), respectively; p-values were determined with Cox model with time-dependent modeling of alloHCT; time in months
Overall survival according to IDH, IDH1 and IDH2 mutational status and allogeneic hematopoietic cell transplantation in CR1. Simon–Makuch plots for a overall survival and b relapse-free survival of AML patients with mutated (mut) IDH, IDH1 and IDH2 treated with allogeneic hematopoietic cell transplantation (blue) or conventional consolidation (red), respectively; p‐values were determined with Cox model with time‐dependent modeling of alloHCT; time in months; ns = not significant
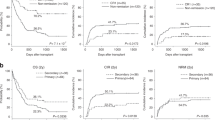
More importantly, the relevance of mutational subtypes in IDH1 and IDH2 on survival could be delineated in our analysis (Fig. 5). Patients with IDH1 R132C had a higher OS when undergoing alloHCT in univariate analysis (5-year OS 40% [non-alloHCT] vs. 73% [alloHCT], p = 0.017; Fig. 5a), which was even more pronounced for RFS in multivariable analysis (5-year RFS 27% [non-alloHCT] vs. 55% [alloHCT]; HR = 0.42, 95% CI 0.17–1, p = 0.048; Fig. 5b). However, IDH1 R132H was not associated with superior survival (Fig. 5a,b). AlloHCT patients carrying IDH2 variant R140 mutations showed no significant difference in OS regarding the respective consolidation strategy (Fig. 5c), but significantly higher RFS compared with the chemo-consolidation group in multivariable analysis (5-year RFS 31% [non-alloHCT] vs. 58% [alloHCT]; HR = 0.4, 95% CI 0.23–0.7, p = 0.002; Fig. 5d). IDH2 variant R172 was associated with increased OS and RFS when undergoing alloHCT in univariate analysis (5-year OS 43% [non-alloHCT] vs. 68% [alloHCT], p = 0.049; Fig. 5c and 5-year RFS 25% [non-alloHCT] vs. 64% [alloHCT]; p = 0.009, respectively; Fig. 5d).
Overall survival and relapse-free survival according to IDH1 and IDH2 mutational subgroups and allogeneic hematopoietic cell transplantation in CR1. Simon–Makuch plots for a and c overall survival and b and d relapse-free survival of AML patients with mutated IDH1 R132C, IDH1 R132H, IDH2 R140 and IDH2 R172 mutational subgroups treated with allogeneic hematopoietic cell transplantation (blue) or conventional consolidation (red), respectively; p-values were determined with Cox model with time-dependent modeling of alloHCT; time in months; ns = not significant
Multivariable analysis
Further multivariable modeling of established factors affecting survival of AML patients (Additional file 1: Fig. S1) revealed significant results regarding age (HR = 1.03, p < 0.001), favorable (HR = 0.6, p < 0.001) and adverse (HR = 1.7, p < 0.001) risk category according to ELN risk stratification and ECOG performance status 0–1 (HR = 0.7, p < 0.001) on OS when analyzing the whole cohort. RFS was also significantly influenced by age (HR = 1.02, p < 0.001), ELN favorable (HR = 0.6, p < 0.001) and adverse (HR = 1.5, p < 0.001) and ECOG performance status 0–1 (HR = 0.8, p = 0.001). Including IDH submutational groups into multivariable analysis, IDH2 R172 was an independent predictor for better OS (HR = 0.5, p = 0.02), which was even more pronounced for RFS (HR = 0.4, p < 0.001). IDH1 mutational subclasses were associated with a trend toward better OS (R132C, HR = 0.86, p = 0.5; R132H, HR = 0.89, p = 0.6), whereas IDH2 R140 showed a trend toward inferior OS (HR = 1.1, p = 0.35). Similar results were obtained in multivariable analysis for RFS where IDH1 R132C showed a trend toward better RFS (HR = 0.77, p = 0.19) and IDH2 R140 a trend toward worse RFS (HR = 1.2, p = 0.1).
Interaction analysis
For studying the effect of the interaction of alloHCT and the respective IDH submutational groups on outcome, we performed interaction analysis with the interaction of alloHCT and IDHWT AML patients as the reference term (Fig. 6a for OS, Fig. 6b for RFS). Interaction analysis demonstrated a trend toward improved outcomes for the interaction of alloHCT and IDH1 R132C (OS, HR = 0.52, p = 0.15; RFS, HR = 0.64, p = 0.28) and IDH2 R172 (OS, HR = 0.31, p = 0.1; RFS, HR = 0.43, p = 0.15), although they did not reach statistical significance. In contrast, interaction analysis of alloHCT and IDH1 R132H predicted a trend toward worse OS (HR = 1.42, p = 0.4). The interaction of alloHCT and IDH1 R132H for RFS (HR = 0.96, p = 0.93), as well as the interaction of alloHCT and IDH2 R140Q (OS, HR = 0.98, p = 0.94; RFS, HR = 1, p = 0.97) predicted similar outcomes like the IDHWT cohort that was allografted. Other mutational IDH subgroups in the alloHCT cohort were almost at double risk for decreased outcome (OS, HR = 1.99, p = 0.18; RFS, HR = 2.11, p = 0.14). In contrast, the effect of the interaction of IDHWT and IDH mutational subclasses and chemo-consolidation only predicted worse outcome, which was mostly pronounced in the terms of IDHWT (OS, HR = 1.25, p = 0.006; RFS, HR = 1.61, p < 0.001), IDH1 R132H (RFS, HR = 1.68, p = 0.008), IDH2 R140Q (OS, HR = 1.43, p = 0.023; RFS, HR = 2.02, p < 0.001) and other IDH mutational subgroups (RFS, HR = 1.74, p = 0.043). However, the interaction term of chemo-consolidation and IDH2 R172K demonstrated a trend toward improved outcome (OS, HR = 0.65, p = 0.139; RFS, HR = 0.74, p = 0.245).
Multivariable Cox model with single interaction terms. Single interaction terms for a overall survival and b relapse-free survival for IDH submutational groups IDH1 R132C, IDH1 R132H, IDH2 R140Q and IDH2 R172K, other IDH mutational subgroups (other) or IDH wildtype (wt) with either allogeneic hematopoietic cell transplantation (alloHCT) or chemo-consolidation (noHCT); p-values and hazard ratios were determined with Cox model
Discussion
Here, we report that the unfavorable prognostic impact of specific IDH mutational subgroups on survival can be mitigated by alloHCT as frontline consolidation strategy in a well-defined AML study cohort. To the best of our knowledge, this is the largest multicenter analysis to determine the prognostic effect of IDH mutations in the course of alloHCT, comprising a cohort of 852 AML patients transplanted in CR1.
Considering the significant biological and molecular heterogeneity of AML, the ideal consolidation therapy is one of the main foci of scientific and clinical interest. Previous studies generated partly controversial results, either associating IDHmut with better outcome [8, 13] and studies reporting a negative impact on outcome [2, 14, 16]. More recently, it was shown that IDH mutational subgroups associated with different biological features have different prognostic impact, suggesting to provide an explanation for inconsistent results concerning prognosis and survival so far [6, 23, 46]. To add a next level of complexity, different mutational IDH variants are associated with differential co-mutational patterns or karyotypes, incorporating prognostic value and even potentially defining distinct genomic categories in AML [10, 15, 23, 46,47,48,49]. As recently shown, considering differential co-mutational rates of epigenetic modifiers like DNMT3A and TET2 in combination with the hypermethylating ability of IDHmut, some suppose IDHmut to be predictive of susceptibility to hypomethylating agents [50, 51]. These results indicate the need for more clarification in the clonal composition, hierarchy and development in the concept of disease biology of IDHmut AML, as latest data suggest [52].
In accordance with previous reports, nearly 20% of the patients analyzed were characterized by IDHmut. Similar to our recent analysis [6], a significantly higher rate of NPM1/IDH co-mutations was seen. In the presence of IDHmut, our present analysis also revealed significant differential co-mutational distributions compared with IDHWT patients. These patterns, as well as their prognostic impact, have to be considered when analyzing outcomes in AML patients, as our study did not include these co-mutational aspects. Also in line with previous data, our IDHmut cohort was characterized by significantly older age, as well as lower LDH concentration (especially for IDH2mut patients) and a higher count of peripheral blasts (pronounced in IDH1mut patients) and bone marrow blasts [48] .
Most importantly, our present data is demonstrating a beneficial effect of alloHCT for IDHmut AML patients, which is in line with recently published data of Duchmann et al. who demonstrated superior OS for IDHmut AML patients treated with alloHCT in CR1 [46], but also contrary to previous studies associating IDH mutations with higher rates of relapse after alloHCT [30]. IDHmut patients showed a trend toward prolonged OS and improved RFS compared with their wildtype counterparts when undergoing alloHCT and shorter OS and RFS compared with IDHWT patients when receiving chemo-consolidation after CR1. Focusing on IDH1 mutations, R132C was characterized by an improved OS and RFS if transplanted in CR1, an effect which could not be shown for R132H. This improvement in survival was shown previously only regarding OS and without discriminating between R132 variants [46]. Whether the difference in prognosis implicated by R132H is due to increased 2-HG levels causing blockage of differentiation in hematopoiesis needs further investigation [53]. Interestingly, R132C patients had the worst 5-year OS compared with the other three analyzed subtypes when consolidated with chemotherapy after CR1 in our study, but the highest 5-year OS of all IDH subgroups when treated with alloHCT in CR1, begging the question of differential susceptibility to allografting among IDH mutational subgroups. Furthermore, when incorporating our recently published data including co-mutational patterns of IDHmut patients into our current analysis, we did not see a clear correlation between improved OS and a high frequency of NPM1 co-mutations, as IDH1 R132C was the subgroup characterized by the lowest rate of co-occurring NPM1 mutations among all IDH1mut patients (IDH1 R132C 24.2% vs. IDH1 R132H 71% vs. IDH1 other 64.2%) and was also less likely to harbor NPM1 mutations compared to IDHWT patients (28.4%) [6]. The same trend is seen for FLT3-ITD, another mutation known to benefit from alloHCT, with IDH1 R132C characterized by the lowest rate of co-occurring FLT3-ITD mutations [6]. On the other hand, IDH1 R132H, which is associated with the highest rate of co-occurring NPM1 mutations (71% of patients) according to our recently published data, demonstrates the worst 5-year OS when undergoing transplantation. These retrospective data suggest that IDH1 R132C could be a clear profiteer from alloHCT, as our recent analysis also revealed a trend toward reduced OS in patients carrying IDH1 variant R132C after intensive induction chemotherapy, and that there could be a beneficial aspect of alloHCT alone independent of NPM1 or FLT3-ITD mutation status, providing a chance to overcome the worse prognosis for patients lacking “favorable” mutations like NPM1. However, low patient numbers in these subgroups of our analysis need to be taken into account and further validation is needed.
Patients with IDH2 subtype R140 had no differential OS probability, but significantly prolonged RFS after alloHCT in CR1. In contrast, IDH2 R172 was characterized by significant higher OS, as well as higher RFS in the alloHCT cohort. These data suggest that allografting AML patients with an IDH2 R172 mutation as consolidation strategy is a considerable option for these patients. Recently, Linch et al. also reported improved survival of AML patients carrying IDH2 R172 variant compared with a historical IDH2 R172 cohort presenting with poor prognosis, relating increased use of alloHCT as consolidation after CR1 with longer OS in the later cohort, as induction strategy was almost unchanged and patients of the later cohort were even significantly older [54]. Additionally, high levels of 2-HG as an oncometabolite and prognostic indicator are paralleled by unfavorable outcome and R172 has been shown to induce higher levels of 2-HG than R140 [24, 55,56,57]. However, our present data reveal an independent beneficial prognostic impact on survival of IDH2 R172. Again, although our IDH2 cohort was bigger and provided more statistical power, small patient numbers and underlying co-mutational patterns have to be considered when interpreting these data, although IDH2 R172 seems to define a distinct genetic AML subgroup, being mutually exclusive from class-defining genetic aberrations like NPM1 mutations as reported previously [6, 23, 49]. Duchmann and colleagues recently attributed co-occurring NPM1 mutations in IDH1 and IDH2 R140-mutated patients as the main prognostic component for improved survival [46]. However, these results were not analyzed in patients undergoing alloHCT or only in a small transplant cohort, respectively. In our non-alloHCT cohort, we could evaluate corresponding results when incorporating our recent results on IDH mutations and co-mutations [6]. Briefly, IDH subtypes with the highest 5-year OS in our present analysis (e.g., IDH1 R132H with 51% and IDH2 R140 with 46%) were also the subgroups with the highest frequencies of co-occurring NPM1 mutations (IDH1 R132H with 71% and IDH2 R140 with 49% of patients carrying additional NPM1 mutations). Along with these results, the IDH subgroup with a lower rate NPM1 mutation (IDH1 R132C with 24%) had the worst 5-year OS in our non-alloHCT cohort (40%). Again, IDH2 R172 was characterized by improved prognosis (5-year OS of 68%) independent of NPM1 mutations (with 2% of patients carrying NPM1) [6]. Hence, our results are in line with the data Duchmann et al., with an implied association that seems to arise between improved survival and NPM1 mutation status.
In summary, a better survival for AML patients with mutated IDH undergoing alloHCT in CR1 could be illustrated, with modest to statistically significant differences depending on the underlying IDH1/2 mutational variant. The improved prognostic effect of alloHCT was mostly pronounced in the mutational subgroups IDH1 R132C and IDH2 R172. However, limitations of this retrospective analysis include the lack of information about donor availability, patients’ performance status after induction therapy and small patient numbers for subgroup analysis. Still, the compiled results highlight the urgent need for increased knowledge about disease biology and the relevance of prognostic and predictive markers in order to apply individually adjusted treatment decisions and optimized consolidation strategies in AML. Ongoing studies are currently investigating the implementation of IDH inhibitors in the frontline setting of induction therapy (NCT03839771 and NCT04493164), which will add valuable data for the re-evaluation of the role of alloHCT in IDHmut patients when pre-treated with IDH inhibitors during induction, consolidation or as a maintenance therapy after alloHCT.
Conclusion
On the basis of our results, it is arguable that defined IDH mutational subgroups introduce predictive and prognostic potential in different therapeutic settings. Furthermore, the differential responsiveness and “alloreactivity” of single IDH subclasses to alloHCT in CR1 should initiate further prospective investigations to validate these findings, especially in respect of co-mutational patterns influencing the predictive value of IDH mutations, offering the chance to add information for refined AML risk classifications to improve survival for AML patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 2-HG:
-
2-Hydroyglutarate
- α-KG:
-
α-Ketoglutarate
- alloHCT:
-
Allogeneic hematopoietic cell transplantation
- AML:
-
Acute myeloid leukemia
- AML-CG:
-
AML-Cooperative Group
- BM:
-
Bone marrow
- CEBPA :
-
CCAAT/enhancer-binding protein alpha
- CI:
-
Confidence interval
- CR1:
-
First complete remission
- DHPLC:
-
Denaturing high-performance liquid chromatography
- DNMT3A :
-
DNA (cytosine-5)-methyltransferase 3A
- ECOG:
-
Eastern Cooperative Oncology Group
- ELN:
-
European Leukemia Net
- Fig.:
-
Figure
- FLT3 :
-
Fms-like tyrosine kinase 3
- GATA2 :
-
GATA-binding factor 2
- HR:
-
Hazard ratio
- IDH :
-
Isocitrate dehydrogenase
- IDH mut :
-
IDH Mutated
- IDH WT :
-
IDH Wildtype
- LDH:
-
Lactate dehydrogenase
- NCT:
-
National clinical trial
- NGS:
-
Next-generation sequencing
- NPM1 :
-
Nucleophosmin 1
- NRAS :
-
Neuroblastoma RAS
- OS:
-
Overall survival
- PB:
-
Peripheral blood
- RFS:
-
Relapse-free survival
- r/r:
-
Relapsed/refractory
- SAL:
-
Study Alliance Leukemia
- STAG2 :
-
Stromal Antigen 2
- TET2 :
-
Tet methylcytosine dioxygenase 2
- VAF:
-
Variant allele frequency
- vs.:
-
Versus
- WT1 :
-
Wilms Tumor 1
References
Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373(12):1136–52.
Paschka P, Schlenk RF, Gaidzik VI, Habdank M, Krönke J, Bullinger L, et al. IDH1 and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internal tandem duplication. J Clin Oncol. 2010;28(22):3636–43.
Yang H, Ye D, Guan KL, Xiong Y. IDH1 and IDH2 mutations in tumorigenesis: mechanistic insights and clinical perspectives. Clin Cancer Res. 2012;18(20):5562–71.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Boissel N, Nibourel O, Renneville A, Gardin C, Reman O, Contentin N, et al. Prognostic impact of isocitrate dehydrogenase enzyme isoforms 1 and 2 mutations in acute myeloid leukemia: a study by the acute leukemia french association group. J Clin Oncol. 2010;28(23):3717–23.
Middeke JM, Metzeler KH, Röllig C, Kramer M, Eckardt JN, Stasik S, et al. Differential impact of IDH1 / 2 mutational subclasses on outcome in adult AML: results from a large multicenter study. Blood Adv. 2022;6(5):1394–405.
Medeiros BC, Fathi AT, DiNardo CD, Pollyea DA, Chan SM, Swords R. Isocitrate dehydrogenase mutations in myeloid malignancies. Leukemia. 2017;31(2):272–81.
Patel JP, Gönen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079–89.
Green CL, Evans CM, Zhao L, Hills RK, Burnett AK, Linch DC, et al. The prognostic significance of IDH2 mutations in AML depends on the location of the mutation. Blood. 2011;118(2):409–12.
Yamaguchi S, Iwanaga E, Tokunaga K, Nanri T, Shimomura T, Suzushima H, et al. IDH1 and IDH2 mutations confer an adverse effect in patients with acute myeloid leukemia lacking the NPM1 mutation. Blood. 2013;122(21):4977–4977.
Abbas S, Lugthart S, Kavelaars FG, Schelen A, Koenders JE, Zeilemaker A, et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia: prevalence and prognostic value. Blood. 2010;116(12):2122–6.
Chotirat S, Thongnoppakhun W, Promsuwicha O, Boonthimat C, Auewarakul CU. Molecular alterations of isocitrate dehydrogenase 1 and 2 (IDH1 and IDH2) metabolic genes and additional genetic mutations in newly diagnosed acute myeloid leukemia patients. J Hematol Oncol. 2012;5:5. https://doi.org/10.1186/1756-8722-5-5.
Chou WC, Lei WC, Ko BS, Hou HA, Chen CY, Tang JL, et al. The prognostic impact and stability of Isocitrate dehydrogenase 2 mutation in adult patients with acute myeloid leukemia. Leukemia. 2011;25(2):246–53.
Aref S, Kamel Areida ES, Abdel Aaal MF, Adam OM, El-Ghonemy MS, El-Baiomy MA, et al. Prevalence and clinical effect of IDH1 and IDH2 mutations among cytogenetically normal acute myeloid leukemia patients. Clin Lymphoma Myeloma Leuk. 2015;15(9):550–5.
Marcucci G, Maharry K, Wu YZ, Radmacher MD, Mrózek K, Margeson D, et al. IDH1 and IDH2 gene mutations identify novel molecular subsets within de novo cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B Study. J Clin Oncol. 2010;28(14):2348–55.
Feng JH, Guo XP, Chen YY, Wang ZJ, Cheng YP, Tang YM. Prognostic significance of IDH1 mutations in acute myeloid leukemia: a meta-analysis. Am J Blood Res. 2012;2(4):254–64.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med. 2009;361(11):1058–66.
Willander K, Falk IJ, Chaireti R, Paul E, Hermansson M, Gréen H, et al. Mutations in the isocitrate dehydrogenase 2 gene and IDH1 SNP 105C > T have a prognostic value in acute myeloid leukemia. Biomark Res. 2014;2(1):18.
Dang L, Jin S, Su SM. IDH mutations in glioma and acute myeloid leukemia. Trends Mol Med. 2010;16(9):387–97.
Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA, et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting α-ketoglutarate to 2-hydroxyglutarate. Cancer Cell. 2010;17(3):225–34.
Clark O, Yen K, Mellinghoff IK. Molecular pathways: isocitrate dehydrogenase mutations in cancer. Clin Cancer Res. 2016;22(8):1837–42.
Lu C, Ward PS, Kapoor GS, Rohle D, Turcan S, Abdel-Wahab O, et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483(7390):474–8.
Meggendorfer M, Cappelli LV, Walter W, Haferlach C, Kern W, Falini B, et al. IDH1R132, IDH2R140 and IDH2R172 in AML: different genetic landscapes correlate with outcome and may influence targeted treatment strategies. Leukemia. 2018;32(5):1249–53.
Ward PS, Lu C, Cross JR, Abdel-Wahab O, Levine RL, Schwartz GK, et al. The potential for isocitrate dehydrogenase mutations to produce 2-hydroxyglutarate depends on allele specificity and subcellular compartmentalization. J Biol Chem. 2013;288(6):3804–15.
DiNardo CD, Stein EM, de Botton S, Roboz GJ, Altman JK, Mims AS, et al. Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J Med. 2018;378(25):2386–98.
Stein EM, DiNardo CD, Pollyea DA, Fathi AT, Roboz GJ, Altman JK, et al. Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood. 2017;130(6):722–31.
Botton S, Brandwein JM, Wei AH, Pigneux A, Quesnel B, Thomas X, et al. Improved survival with enasidenib versus standard of care in relapsed/refractory acute myeloid leukemia associated with IDH2 mutations using historical data and propensity score matching analysis. Cancer Med. 2021;10(18):6336–43.
Montesinos P, Recher C, Vives S, Zarzycka E, Wang J, Bertani G, et al. Ivosidenib and azacitidine in IDH1-mutated acute myeloid leukemia. N Engl J Med. 2022;386(16):1519–31.
DiNardo CD, Schuh AC, Stein EM, Montesinos P, Wei AH, de Botton S, et al. Enasidenib plus azacitidine versus azacitidine alone in patients with newly diagnosed, mutant-IDH2 acute myeloid leukaemia (AG221-AML-005): a single-arm, phase 1b and randomised, phase 2 trial. Lancet Oncol. 2021;22(11):1597–608.
Salhotra A, Afkhami M, Yang D, Mokhtari S, Telatar M, Gu D, et al. Allogeneic hematopoietic cell transplantation outcomes in patients carrying isocitrate dehydrogenase mutations. Clin Lymphoma Myeloma Leuk. 2019;19(7):e400–5.
Chen EC, Li S, Eisfeld AK, Luskin MR, Mims A, Jones D, et al. Outcomes for patients with IDH-mutated acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Transpl Cell Ther. 2021;27(6):479.e1-479.e7.
Röllig C, Thiede C, Gramatzki M, Aulitzky W, Bodenstein H, Bornhäuser M, et al. A novel prognostic model in elderly patients with acute myeloid leukemia: results of 909 patients entered into the prospective AML96 trial. Blood. 2010;116(6):971–8.
Schaich M, Parmentier S, Kramer M, Illmer T, Stölzel F, Röllig C, et al. High-dose cytarabine consolidation with or without additional amsacrine and mitoxantrone in acute myeloid leukemia: results of the prospective randomized AML2003 trial. J Clin Oncol. 2013;31(17):2094–102.
Buchner T, Berdel WE, Haferlach C, Schnittger S, Haferlach T, Serve H, et al. Long-term results in patients with acute myeloid leukemia (AML): the influence of high-dose AraC, G-CSF priming, autologous transplantation, prolonged maintenance, age, history, cytogenetics, and mutation status. Data of the AMLCG 1999 trial. Blood. 2009;114(22):485.
Röllig C, Kramer M, Gabrecht M, Hänel M, Herbst R, Kaiser U, et al. Intermediate-dose cytarabine plus mitoxantrone versus standard-dose cytarabine plus daunorubicin for acute myeloid leukemia in elderly patients. Ann Oncol. 2018;29:973–8.
Braess J, Amler S, Kreuzer KA, Spiekermann K, Lindemann HW, Lengfelder E, et al. Sequential high-dose cytarabine and mitoxantrone (S-HAM) versus standard double induction in acute myeloid leukemia—a phase 3 study. Leukemia. 2018;32(12):2558–71.
Röllig C, Serve H, Hüttmann A, Noppeney R, Müller-Tidow C, Krug U, et al. Addition of sorafenib versus placebo to standard therapy in patients aged 60 years or younger with newly diagnosed acute myeloid leukaemia (SORAML): A multicentre, phase 2, randomised controlled trial. Lancet Oncol. 2015;16:1691–9.
Döhner H, Estey EH, Amadori S, Appelbaum FR, Büchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115(3):453–74.
Cheson BD, Bennett JM, Kopecky KJ, Büchner T, Willman CL, Estey EH, et al. Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2003;21(24):4642–9.
Damm F, Thol F, Hollink I, Zimmermann M, Reinhardt K, van den Heuvel-Eibrink MM, et al. Prevalence and prognostic value of IDH1 and IDH2 mutations in childhood AML: a study of the AML–BFM and DCOG study groups. Leukemia. 2011;25(11):1704–10.
Stasik S, Schuster C, Ortlepp C, Platzbecker U, Bornhäuser M, Schetelig J, et al. An optimized targeted Next-Generation Sequencing approach for sensitive detection of single nucleotide variants. Biomol Detect Quantif. 2018;15:6–12.
Gebhard C, Glatz D, Schwarzfischer L, Wimmer J, Stasik S, Nuetzel M, et al. Profiling of aberrant DNA methylation in acute myeloid leukemia reveals subclasses of CG-rich regions with epigenetic or genetic association. Leukemia. 2019;33(1):26–36.
Metzeler KH, Herold T, Rothenberg-Thurley M, Amler S, Sauerland MC, Görlich D, et al. Spectrum and prognostic relevance of driver gene mutations in acute myeloid leukemia. Blood. 2016;128(5):686–98.
Thiede C, Creutzig E, Illmer T, Schaich M, Heise V, Ehninger G, et al. Rapid and sensitive typing of NPM1 mutations using LNA-mediated PCR clamping. Leukemia. 2006;20(10):1897–9.
Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99(12):4326–35.
Duchmann M, Micol JB, Duployez N, Raffoux E, Thomas X, Marolleau JP, et al. Prognostic significance of concurrent gene mutations in intensively treated patients with IDH -mutated AML: an ALFA study. Blood. 2021;137(20):2827–37.
Falini B, Spinelli O, Meggendorfer M, Martelli MP, Bigerna B, Ascani S, et al. IDH1-R132 changes vary according to NPM1 and other mutations status in AML. Leukemia. 2019;33(4):1043–7.
DiNardo CD, Ravandi F, Agresta S, Konopleva M, Takahashi K, Kadia T, et al. Characteristics, clinical outcome, and prognostic significance of IDH mutations in AML: IDH mutations in AML. Am J Hematol. 2015;90(8):732–6.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374(23):2209–21.
Figueroa ME, Abdel-Wahab O, Lu C, Ward PS, Patel J, Shih A, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010;18(6):553–67.
Emadi A, Faramand R, Carter-Cooper B, Tolu S, Ford LA, Lapidus RG, et al. Presence of isocitrate dehydrogenase mutations may predict clinical response to hypomethylating agents in patients with acute myeloid leukemia: response to DNMTIs in mIDH AML. Am J Hematol. 2015;90(5):E77–9.
Lachowiez C, DiNardo CD, Morita K, Furudate K, Wang F, Tanaka T, et al. Longitudinal next generation sequencing reveals the clonal hierarchy of IDH mutated clones and impact on survival in NPM1 Mutated AML. Blood. 2021;138(Supplement 1):607–607.
Losman J-A, Looper RE, Koivunen P, Lee S, Schneider RK, McMahon C, et al. (R)-2-Hydroxyglutarate Is sufficient to promote leukemogenesis and its effects are reversible. Science. 2013;339(6127):1621–5.
Linch DC, Hills RK, Burnett AK, Russell N, Gale RE. Therapy for isocitrate dehydrogenase 2 (IDH2)R172‐mutant acute myeloid leukaemia. Br J Haematol. 2021; bjh.17981.
Janin M, Mylonas E, Saada V, Micol JB, Renneville A, Quivoron C, et al. Serum 2-hydroxyglutarate production in IDH1 - and IDH2 -mutated de novo acute myeloid leukemia: a study by the acute leukemia French Association Group. J Clin Oncol. 2014;32(4):297–305.
Wang JH, Chen WL, Li JM, Wu SF, Chen TL, Zhu YM, et al. Prognostic significance of 2-hydroxyglutarate levels in acute myeloid leukemia in China. Proc Natl Acad Sci. 2013;110(42):17017–22.
DiNardo CD, Propert KJ, Loren AW, Paietta E, Sun Z, Levine RL, et al. Serum 2-hydroxyglutarate levels predict isocitrate dehydrogenase mutations and clinical outcome in acute myeloid leukemia. Blood. 2013;121(24):4917–24.
Acknowledgements
The authors thank all participating patients, without whom the continuous improvement of clinical care and growing scientific insights would not be possible. The authors acknowledge all contributing physicians, study nurses and laboratories for their support of the trials, and thank all SAL and AMLCG centres for their commitment in the conduction of the respective trials and registry.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Contributions
DK, JMM and FS designed the study. GE and MB provided administrative support. All authors collected clinical and/or genetic data and provided patient samples. CT and SS performed molecular diagnostics. DK, MK, JS, JMM and FS analyzed and interpreted the data; all authors had access to primary clinical trial data. DK drafted the manuscript; JMM and FS provided critical revision. All authors read the manuscript and gave their final approval for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study included samples from patients enrolled in NCT03188874, NCT00180115, NCT00180102, NCT00266136, NCT00180167, NCT01382147 and NCT00893373. The trials were approved by the respective ethics committees and conducted in accordance with the Declaration of Helsinki. All patients gave their written informed consent including analysis of data. The studies were monitored continuously by clinical and medical monitors. Safety reports were generated and submitted to an independent Data and Safety Monitoring Board (DSMB). Data quality controls were performed regularly and the medical monitors verified that the clinical trials, as well as data acquisition were conducted in compliance with the International Conference on Harmonization Good Clinical Practice (ICH GCP), the study protocol and all applicable regulatory requirements.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
Overview of the clinical trials the study patients were selected from. Figure S1 Forrest Plot of variables evaluated in univariate analysis. Multivariate Cox proportional hazard regression for (A) overall survival and (B) relapse-free survival.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kunadt, D., Stasik, S., Metzeler, K.H. et al. Impact of IDH1 and IDH2 mutational subgroups in AML patients after allogeneic stem cell transplantation. J Hematol Oncol 15, 126 (2022). https://doi.org/10.1186/s13045-022-01339-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-022-01339-8