Abstract
Background
Wolf–Hirschhorn (WHS) is a set of congenital physical anomalies and mental retardation associated with a partial deletion of the short arm of chromosome 4. To establish a genotype–phenotype correlation; we carried out a molecular cytogenetic analysis on two Tunisian WHS patients. Patient 1 was a boy of 1-year-old, presented a typical WHS phenotype while patient 2, is a boy of 2 days presented an hypospadias, a micropenis and a cryptorchidie in addition to the typical WHS phenotype. Both the array comparative genomic hybridization and fluorescence in situ hybridization techniques were used.
Results
Results of the analysis showed that patient 2 had a greater deletion size (4.8 Mb) of chromosome 4 than patient 1 (3.4 Mb). Here, we notice that the larger the deletion, the more genes are likely to be involved, and the more severe the phenotype is likely to be. If we analyze the uncommon deleted region between patient1 and patient 2 we found that the Muscle Segment Homeobox (MSX1) gene is included in this region. MSX1 is a critical transcriptional repressor factor, expressed in the ventral side of the developing anterior pituitary and implicated in gonadotrope differentiation. Msx1 acts as a negative regulatory pituitary development by repressing the gonadotropin releasing hormone (GnRH) genes during embryogenesis. We hypothesized that the deletion of MSX1 in our patient may deregulate the androgen synthesis.
Conclusion
Based on the MSX1 gene function, its absence might be indirectly responsible for the hypospadias phenotype by contributing to the spatiotemporal regulation of GnRH transcription during development.
Similar content being viewed by others
Background
Over the past decade, advanced molecular cytogenetic analysis such as array CGH has made valuable contributions to the knowledge and refinement of several chromosomal regions involved in birth defects and has led to the emergence of several well-established chromosomal syndromes. Among these syndromes, chromosome 4p16.3 deletion [OMIM#194190] is a contiguous gene deletion syndrome resulting in several clinical features, including growth and mental retardation, microcephaly, seizures, “Greek helmet” facies, and major malformations such as cleft lip and/or palate (CL/P), coloboma of the eye, congenital heart defects (CHD) and dental anomalies (oligodontia) [1, 2]. The WHS syndrome was first described by Hirschhorn and Cooper in a preliminary report in 1961 and later formalized with back-to-back publications by Wolf et al., and Hirschhorn et al., in Humangenetik in 1965 [3]. Its frequency ranges from 1 case per 50,000 births to 1 case per 20,000 births, occurring more frequently in females with a male to female ratio of 1:2 [4]. Several literature reports point to the great variability of the WHS phenotype, depending mostly on the variability of the underlying genomic defect based on different size deletions [5, 6]. Hence, previous studies of 4p16.3 deletion focused largely on postnatal growth delay, CHD, and oligodontia. However, hypospadias has not been lighted in the phenotype. In this paper, we report on an additional case of a 4p16.3 deletion associated with hypospadias, micropenis, dysmorphic features, microcephaly, heart disorder, and Platine crack. Here, by reviewing the literature, we emphasize Disorders of sex Development (DSD) traits in the phenotype and suggest a candidate gene.
Results
The chromosomal analysis of the first patient indicated a normal male karyotype 46, XY in all metaphases (Fig. 1a). Array CGH analysis revealed partial 4p deletion encompassing at least 3.4 Mb ranging from nucleotides 72,447 to 3,519,927 according to the Human reference genome hg18,46,XY.arr[hg18]4p16.3 (72,447_3,519,927) ×1 dn (Fig. 2a).
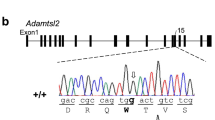
For the second patient, conventional Karyotype revealed a male karyotype with a terminal deletion of the short arm of chromosome 4;46,XY,del(4)(p16.3) (Fig. 1b). Parents’ R-banded karyotype from peripheral blood didn’t reveal any chromosomal anomalies in the resolution limit of banding detection. Array CGH characterized this deletion encompassing at least 4.8 Mb extending from nucleotides 62,447 to 19,065,971, according to the Human reference genome hg18,46,XY.arr[hg18]4p16.3(62,447–19,065,971) ×1 dn (Fig. 2b).
Then, FISH assay confirmed the chromosomal rearrangement by showing a partial deletion on chromosome 4, in both patients, using Kreatech dual colour probes (Fig. 3a, b).
Discussion
The Wolf–Hirschhorn syndrome (WHS) is the first example of a human chromosomal deletion syndrome, described as a pathogenetic syndrome. It is usually caused by the deletion of the sub-telomeric short arm of chromosome 4 [1].
The spectrum and severity of WHS clinical features typically correlate with the deletion size [2,3,4,5]. This report focuses on the DSD as particular features in genotype–phenotype correlation analysis of WHS patients on two Tunisian patients and proposes a candidate gene to this developmental disorder.
The main characteristic of WHS is the typical face, usually referred to as a “Greek warrior helmet face”. Previous studies suggest a critical region that, when deleted, causes the recognizable syndrome. It has been narrowed to a 165 kb, about 1.9 Mb from the 4p telomere, and includes two purported regions, called WHSCR1 and WHSCR2 [6, 7]. So far, advanced molecular techniques such as FISH and array CGH provided the possibility of detecting smaller deletions with less evident phenotypes.
Our study focuses on variable features in two 4p deletions cases. Molecular and conventional cytogenetic analysis, showed a partial loss of 4p with different breakpoints and different size deletions. Both patients are clinically suspected to have WHS. Patient 1 has specific dysmorphic features, a severe psychomotor delay, failure to thrive and microcephaly. His clinical profile is suggestive of a mild form. However, patient 2 has a polymalformative syndrome including dysmorphic features: a microcephaly, a megalocornea, an hypertelorism, a microretrognatism and a growth delay. He presents a heart defect, a Palatine crack and a cryptorchidism, micropenis and hypospadias, all the three last features are suggestive of sex development disorder in atypical WHS case. Array-CGH exploration characterized the 4p loss of 3.4 Mb in the first patient and of 4.8 Mb in the second. We suggest that different deletion sizes and the variability of the involved genes could play an important role in the complex phenotype of WHS in each patient (Table 1).
In order to understand the genotype–phenotype correlation in both cases, we focus on the uncommon deleted region. However, the common deleted region, in both cases, involves three important genes implicated in the development of the main features of WHS. These genes are WHSC1, FGFRL1, and LETM1. The Wolf–Hirschhorn syndrome candidate 1 gene (WHSC1), also known as NSD2 (nuclear receptor SET domain containing) and MMSET (multiple myeloma SET domain containing) [OMIM#602952], is located in the WHSCR1 region and its loss is believed to be responsible for several features of the syndrome. It encodes a putative histone methyltransferase, and the resulting protein has several domains [8, 9].
The molecular features of WHSC1 suggest different functions such as a chromatin-remodeling enzyme function since its SET domains act as histone methylase. A deficiency could then deregulate multiple genes expression leading to a pleiotropic effect [10]. Recently, it has been proposed that deficiency in WHSC1 gene leads to defects in the DNA damage response as seen in WHS patients. The WHSC1 has been indeed localized at sites of DNA damage and replication stress and then is required for resistance to many DNA-damaging and replication stress-inducing agents [11, 12]. This function could then explain the neurological impairment in WHS. However, the hypothesis that typical WHS could be a single-gene disorder is unlikely. We think that the full WHS phenotype results from the haplo-insufficiency of several other candidate genes, especially those telomeric to WHSC1. The best possible interpretation of the currently available data, in patients 1 and 2, is that WHSC1, in combination with closely linked genes, are responsible for the core phenotypes.
Interestingly, the common deleted interval in both patients encompasses the Fibroblast Growth Factor Like-1 gene (FGFRL1) [OMIM#605830] considered as the most characterized gene in this region. Located on 4p16.3 outside and distal to the WHSCRs, the FGFRL1 gene encodes a member of the fibroblast growth factor receptor family [8]. Recent studies suggest that FGFRL1 represents a plausible second candidate gene for several other WHS features. Mouse models targeting FGFRL1 present growth delay, craniofacial defects, skeletal anomalies and congenital heart defects features that are in complete accordance with WHS phenotype, mainly the craniofacial phenotype [6, 13, 14]. In the proximal side of WHSC1, additional genes contributing to the core phenotypes may act to complete the pleiotropic WHS phenotype. Leucine zipper/EF-hand-containing transmembrane gene (LETM1) [OMIM#604407], an ubiquitous Ca2 + binding protein involved in Ca2 + homeostasis, is located at 1.8 Mb from the telomere. This gene has been suggested to cause seizures [7, 15] and seems to be the most likely candidate gene for epilepsy in WHS patients. Indeed, impaired Ca2 + homeostasis in nerve cells has been correlated with neurodegenerative disorders and seizures [16,17,18,19]. In the present study, while the LETM1 gene is deleted in both cases only the first patient presents epilepsy. Elsewhere, it has been previously reported a WHS patient suffering from seizures with a 1.4 Mb terminal 4p deletion preserving LETM1 gene [2]. In another study, six of eight subjects with terminal 4p deletions preserving LETM1 had seizures, whereas seven of seven with small interstitial deletions including LETM1, did not [7]. Taken together, it seems that LETM1 haploin sufficiency contributes to seizure genesis but epileptic phenotype genesis appears to be questionable and not fully elucidated and another gene or genes could be incriminated. As advanced elsewhere C-Terminal-binding protein 1, a transcriptional co-repressor gene (CTBP1) [OMIM#602618], could be a good candidate for seizures/epilepsy in WHS [20, 21].
The Wolf–Hirschhorn syndrome candidate 2 (WHSC2) [OMIM#606026], encodes a subunit of the negative elongation factor complex, involved in mRNA processing and the cell cycle [22, 23]. This complex seems to induce promoter-proximal pause by inhibiting RNA polymerase II early progression during elongation, and consequently altering the expression of its target genes [24]. Recently, WHSC2 has been implicated in the recruitment of Stem Loop Binding Protein (SLBP) [OMIM#602422] to the 3′ ends of histone pre-mRNAs [22]. Taken into account that the SLBP gene is included in the patients1 and 2 deletions, we suppose that haploinsufficiency of SLBP and/or WHSC2 supply microcephaly, pre- and postnatal growth retardation, the core clinical features of WHS. Employing a unique panel of patient-derived cell lines with differently-sized 4p deletions, underlies novel cellular defects associated with WHS. It has been demonstrated that haploinsufficiency of SLBP and/or WHSC2 contributes to delayed cell-cycle progression, impaired DNA replication and altered chromatine structure [25]. These results may explain the phenotype severity observed in the present patients too suggesting a functional relationship between both genes SLBP and WHSC2, commonly haploinsufficient in WHS.
In addition, in the present study, we report on the deletion of Chromosome 4 Open Reading Frame 48 (C4ORF48) [OMIM#614690], a gene located in a 191.5-kb region and associated to WHS patients presenting microcephaly and growth retardation. Interestingly, expression of C4ORF48 in different zones during cortical and cerebellar development, as well as in almost all cortical and subcortical regions of the adult mouse brain was proven [26]. This suggests a potential role of C4ORF48 in the development of human cerebral and cerebellar structures, and plasticity function in adult brain neurons. It indicates also that C4ORF48 hemizygosity might be partly involved in the WHS neurological aspects.
Otherwise, if we focus on the differential features and the non-overlapping region between the two patients 1 and 2 in the present report, we notice that the different genes involved may explain the presence of a sex development disorder in patient 2. A deep analysis of this region underlies a deletion of the MSX1 gene [OMIM#142983] at 4.9 Mb from the telomere. As previously seen monosomy of MSX1 was linked to the oligodontia observed in some WHS patients suggesting that selective tooth agenesis is a common phenotype in Wolf–Hirschhorn syndrome [27, 28]. It could be considered then as an obvious candidate gene for the cranio-facial structures and the anterior forebrain development [29]. MSX1 has been reported also as a transcriptional repressor of GnRH promoter activity that is expressed in the ventral side of the developing anterior pituitary. It is regulated by Bone Morphogenetic Protein (BMP), and implicated in gonadotropin neurons differentiation [30, 31].
Interestingly, some other studies mapped the critical region for hypospadias in WHS syndrome between 3 Mb and 4.0 Mb [2, 32]. Taken into account the deleted region of the second patient in the present report, it is possible that an haploinsufficiency of the MSX1 gene could explain the hypospadias phenotype.
As known, proper sexual maturation depends upon the correct function of the hypothalamic–pituitary–gonadal axis, initiated by a critical population of GnRH neurons [33] and then, by binding to the consensus homeodomain repeats (ATTA) in the enhancer and promoter, MSX1 could repress GnRH promoter activity and consequently participate in the regulation of GnRH gene expression network [32].
Thus, it may deregulate the androgen synthesis; which may lead to hypospadias during an embryogenesis critical phase. Indeed, recently, MSX1 has been proposed as a candidate gene for hypogonadism based on its function in the gonadotropic axis [34].
Curiously, the MSX1 deletion in the second patient is associated with hypospadias without the expected oligodontia. Here we could explain these controversies by variable expressivity or incomplete penetrance. Several mutations in the homeodomain of MSX1 are associated to tooth agenesis or orofacial clefts [35].
But to the best of our knowledge, no reported MSX1 gene mutations have been associated to DSD. Here, again we underlie the acting network in a multiple genes deleted syndrome as WHS.
In summary, we suggest MSX1 gene as an intriguing candidate gene for contribution to the hypogonadal phenotype. Functional studies for MSX1 gene should be considered to more understand its implication in the development of oligodontia and hypospadias.
Here we emphasize the phenotype-genotype correlation studies, which are considered as the core, the beginning, and the end of gene analysis. The use of a combined approach conventional cytogenetic and, chromosomal array associated with a deep analysis of a molecular and functional gene studies are necessary.
Based on the genome system theory, the correlation between the size of deletion and severity of diseases might be explained by the alteration of karyotype coding based on a “system inheritance” which consider genes and the genomic topology within the three-dimensional nucleus configuration [36]. Based on the new emergent genome, we have posited that chromosomal rearrangements with different size as seen here can reorganize different genomic information’s leading to an abnormal development and then pathologic phenotypes.
Taking all these facts into consideration, functional studies or more sophisticated technologies such as Hi-C technologies are highly recommended to better characterize the genetic interactions following 4p deletion. It is likely that more patients with WHS will present hypogonadism and therefore precise personal medical care is required.
Conclusion
In conclusion, WHS is a multigenic syndrome with a spectrum of phenotypic features, from very subtle and mild to a wide range of severe aberrations. Array CGH allowed us to better identify the breakpoints and genes likely to be involved in the WHS syndrome. Therefore, our work highlights new candidate genes such as MSX1 gene likely responsible of hypogonadism in WHS. It allows establishing a specific genotype–phenotype correlation and underlining the new genomic topology tools as relevant to understand the role of the different 4p genes in the WHS development.
Methods
Karyotype
Conventional cytogenetic analysis was performed on the peripheral blood lymphocytes according to standard procedures. Chromosome analysis was carried out applying R-banding at a 450 band resolution according to ISCN 2016 in both patients and their parents. Metaphase chromosome spreads were prepared from phytohemagglutinin—stimulated peripheral blood lymphocytes-based on standard protocol. Cell cultures were incubated for 72 h. At least 20 mitoses were investigated for each sample using Cytovision® Karyotyping software version 4.0.
Fluorescent in situ Hybridization (FISH)
FISH was performed on blood lymphocytes blocked on metaphases of each patient, according to the standard protocol. FISH followed manufacturer’s instructions, using probes for chromosome 4 (Vysis® Wolf Hirschhorn Region probe-LSI WHS (Red) and CEP 4 (Green) (Vysis, Abbott Laboratories, IL, USA). Probes were applied to metaphase slides and therefore co-denaturized for 7 min at 75 °C. After overnight hybridization at 37 °C, the slides were washed for 5 min in de 2XSSC/ NP40(Vysis, Illinois, Unites States) at 75 °C. Chromosomes were mounted with a 4,6 diamino-2-phenylindole and analyzed using an Axioskop Zeiss® fluorescent microscope.
Array CGH
Array comparative genomic hybridization (array CGH) was performed with Agilent Human Genome array CGH Kit 44 K, for both patients, according to the manufacturer’s instructions (Feature Extraction 9.1, CGH Analytics 4.5, and Santa Clara, California, United States). The coverage of the human genome was made with an average spatial resolution of 75,000 pair bases. A copy number variation was noted when at least three contiguous oligonucleotides presented an abnormal ratio greater than + 0.58 or lower than − 0.75.
An in-silico analysis of the unbalanced region indicated by the analysis was made using UCSC Genome Browser (http://genome.ucsc.edu/), the Online Mendelian Inheritance in Man database (OMIM: https://omim.org/) and the Database of Genomic Variants (DGV: http://dgv.tcag.ca/dgv/app/ home).
Clinical description
Patient 1
Patient 1(III3) is a 1-year-old boy, suffering from epilepsy since the age of 17 months. In addition he presents a specific dysmorphic features, a psychomotor development delay, growth retardation (weight (− 3.8) SD; size (− 5.3) SD) and a microcephaly. It is noteworthy that the patient had a maternal aunt with malformation syndrome (Fig. 4).
Patient 2
Patient 2 is a newborn boy aged 2 days. At physical examination, he presents a polymalformative syndrome, suggestive of Wolf Hirshhorn syndrome, including dysmorphic features, microcephaly, a megalocornea, a hypertelorism, a microretrogandism, a heart disorder and a Platine crack. Furthermore, he had a disorder of sexual development type cryptorchidie, micropenis and hypospadias (Fig. 5).
Availability of data and materials
Data and materials are available from the corresponding author and available upon request.
Abbreviations
- Array CGH:
-
Array comparative genomic hybridization
- CHD:
-
Congenital heart defect
- DAPI:
-
Diamino-2-phenylindole
- DNA:
-
Desoxyribonucleic acid
- DSD:
-
Disorders of sex development
- FGFRL1:
-
Fibroblast growth factor like-1 gene
- FISH:
-
Fluorescence in situ hybridization
- GnRH:
-
Gonadotropin releasing hormone
- ISCN:
-
International System for Human Cytogenetic Nomenclature
- LETM1:
-
Leucine zipper/EF-hand-containing transmembrane gene
- MMSET:
-
Multiple myeloma SET domain containing
- MSX1:
-
Muscle Segment Homeobox
- NSD2:
-
Nuclear receptor SET domain containing
- OMIM:
-
Online Mendelian Inheritance in man
- SLBP:
-
Stem Loop Binding Protein
- WHS:
-
Wolf–Hirschhorn syndrome
- WHSCR1:
-
Wolf–Hirschhorn syndrome region 1
- WHSR2:
-
Wolf–Hirschhorn syndrome region 2
- WHSC1:
-
Wolf–Hirschhorn syndrome candidate 1 gene
- WHSC2:
-
Wolf–Hirschhorn syndrome candidate 2 gene
References
Battaglia A, Carey JC, South ST. Wolf–Hirschhorn syndrome: a review and update. Am J Med Genet Part C Semin Med Genet. 2015;169:216–23.
Andrieux J, et al. Genotype-phenotype correlation in 21 patients with Wolf–Hirschhorn syndrome using high resolution array comparative genome hybridisation (CGH). J Med Genet. 2007;45:71–80.
Battaglia A, Carey JC. Wolf–Hirschhorn syndrome and the 4p-related syndromes. Am J Med Genet Part C Semin Med Genet. 2008;148C:241–3.
Van Buggenhout G, et al. Mild Wolf–Hirschhorn syndrome: micro-array CGH analysis of atypical 4p16.3 deletions enables refinement of the genotype-phenotype map. J Med Genet. 2004;41:691–8.
Zampino G, et al. Genotype-phenotype correlations and clinical diagnostic criteria in Wolf–Hirschhorn syndrome. Am J Med Genet. 2002;94:254–61.
Wright TJ, et al. A transcript map of the newly defined 165 kb Wolf–Hirschhorn syndrome critical region. Hum Mol Genet. 1997;6:317–24.
Zollino M, et al. Mapping the Wolf–Hirschhorn syndrome phenotype outside the currently accepted WHS critical region and defining a new critical region, WHSCR-2. Am J Hum Genet. 2003;1:590–7.
Kook H, et al. Multiple myeloma-related WHSC1/MMSET isoform RE-IIBP is a histone methyltransferase with transcriptional repression activity. Mol Cell Biol. 2008;28:2023–34.
Zhou M-M, et al. The MMSET protein is a histone methyltransferase with characteristics of a transcriptional corepressor. Blood. 2007;111:3145–54.
Stec I, et al. WHSC1, a 90 kb SET domain-containing gene, expressed in early development and homologous to a Drosophila dysmorphy gene maps in the Wolf–Hirschhorn syndrome critical region and is fused to IgH in t(4;14) multiple myeloma. Hum Mol Genet. 1998;7:1071–82.
Cappuccio G, et al. A case of 14q11.2 microdeletion with autistic features, severe obesity and facial dysmorphisms suggestive of Wolf–Hirschhorn syndrome. Am J Med Genet Part A. 2013;164:190–3.
Hajdu I, Ciccia A, Lewis SM, Elledge SJ. Wolf–Hirschhorn syndrome candidate 1 is involved in the cellular response to DNA damage. Proc Natl Acad Sci. 2011;108:13130–4.
Kratsios P, et al. Multiple congenital malformations of Wolf–Hirschhorn syndrome are recapitulated in Fgfrl1 null mice. Dis Model Mech. 2009;2:283–94.
Engbers H, et al. Wolf–Hirschhorn syndrome facial dysmorphic features in a patient with a terminal 4p16.3 deletion telomeric to the WHSCR and WHSCR 2 regions. Eur J Hum Genet. 2009;17:129–32.
Endele S, Fuhry M, Pak SJ, Zabel BU, Winterpacht A. LETM1, a novel gene encoding a putative EF-hand Ca2+-binding protein, flanks the Wolf–Hirschhorn syndrome (WHS) critical region and is deleted in most WHS patients. Genomics. 1999;60:218–25.
Burgess DL, Jones JM, Meisler MH, Noebels JL. Mutation of the Ca2+channel β subunit gene Cchb4 is associated with ataxia and seizures in the lethargic (lh) mouse. Cell. 1997;88:385–92.
Schlickum S, et al. LETM1, a gene deleted in Wolf–Hirschhorn syndrome, encodes an evolutionarily conserved mitochondrial protein. Genomics. 2004;83:254–61.
Dimmer KS, et al. LETM1, deleted in Wolf–Hirschhorn syndrome is required for normal mitochondrial morphology and cellular viability. Hum Mol Genet. 2008;17:201–14.
McQuibban AG, et al. A Drosophila mutant of LETM1, a candidate gene for seizures in Wolf–Hirschhorn syndrome. Hum Mol Genet. 2010;19:987–1000.
Misceo D, et al. 1.5Mb deletion of chromosome 4p16.3 associated with postnatal growth delay, psychomotor impairment, epilepsy, impulsive behavior and asynchronous skeletal development. Gene. 2012;507:85–91.
Limongelli I, et al. Dravet phenotype in a subject with a der(4)t(4;8)(p16.3;p23.3) without the involvement of the LETM1 gene. Eur J Med Genet. 2013;56:551–5.
Narita T, et al. NELF interacts with CBC and participates in 3′ end processing of replication-dependent histone mRNAs. Mol Cell. 2007;26:349–65.
Sun J, Li R. Human negative elongation factor activates transcription and regulates alternative transcription initiation. J Biol Chem. 2010;285:6443–52.
Chiba K, Yamamoto J, Yamaguchi Y, Handa H. Promoter-proximal pausing and its release: molecular mechanisms and physiological functions. Exp Cell Res. 2010;316:2723–30.
Colnaghi R, et al. Characterizing the functional consequences of haploinsufficiency of NELF-A (WHSC2) and SLBP identifies novel cellular phenotypes in Wolf–Hirschhorn syndrome. Hum Mol Genet. 2012;21:2181–93.
Schlickum S, Winterpacht A, Endele S, Bördlein A, Nelkenbrecher C. C4ORF48, a gene from the Wolf–Hirschhorn syndrome critical region, encodes a putative neuropeptide and is expressed during neocortex and cerebellar development. Neurogenetics. 2011;12:155–63.
Zhang H, Catron KM, Abate-Shen C. A role for the Msx-1 homeodomain in transcriptional regulation: residues in the N-terminal arm mediate TATA binding protein interaction and transcriptional repression. Proc Natl Acad Sci. 2002;93:1764–9.
Bendall AJ, Bendall CA-S. 2000 Roles for Msx and Dlx homeoproteins…pdf. Gene. 2000;247:17–31.
Nieminen P, et al. MSX1 gene is deleted in Wolf–Hirschhorn syndrome patients with oligodontia. J Dent Res. 2003;82:1013–7.
Scully KM, Rosenf MG. Pituitary Development: regulatory codes in mammalian organogenesis. Science (80–). 2010;2231:2231–5.
MacKenzie A, Ferguson MW, Sharpe PT. Hox-7 expression during murine craniofacial development. Development. 1991;113:601–11.
Mellon PL, et al. Developmental regulation of gonadotropin-releasing hormone gene expression by the MSX and DLX homeodomain protein families. J Biol Chem. 2005;280:19156–65.
Wu TJ, Gibson MJ, Silverman AJ. Gonadotropin-releasing hormone (GnRH) neurons of the developing tectum of the mouse. J Neuroendoocrinol. 1995;7:899–902.
Guimaraes L, et al. New genetic findings in a large cohort of congenital hypogonadotropic hypogonadism. Eur Soc Endocrinol. 2019. https://doi.org/10.1530/EJE-18-0764
Liang J, et al. MSX1 mutations and associated disease phenotypes: genotype-phenotype relations. Eur J Hum Genet. 2016. https://doi.org/10.1038/ejhg.2016.78.
Ye CJ, Stilgenbauer L, Moy A, Liu G, Heng HH. What is karyotype coding and why is genomic topology important for cancer and evolution? Front Genet. 2019;10:1–8.
Flipsen-ten Berg K, et al. Unmasking of a hemizygous WFS1 gene mutation by a chromosome 4p deletion of 8.3 Mb in a patient with Wolf-Hirschhorn syndrome. Eur J Hum Genet. 2007;15:1132–8.
Chen CP, et al. Wolf-Hirschhorn (4p-) syndrome: prenatal diagnosis, molecular cytogenetic characterization and association with a 1.2-Mb microduplication at 8p22-p21.3 and a 1.1-Mb microduplication at 10p15.3 in a fetus with an apparently pure 4p deletion. Taiwan J Obstet Gynecol. 2011;50:506–11.
Sifakis S, et al. Prenatal diagnosis of Wolf-Hirschhorn syndrome confirmed by comparative genomic hybridization array: report of two cases and review of the literature. Mol Cytogenet. 2012;5:1–7.
Malvestiti F, et al. Recombinant chromosome 4 from a familial pericentric inversion: prenatal and adulthood Wolf-Hirschhorn phenotypes. Case Rep Genet. 2013;2013:1–4.
Venegas-Vega CA, Fernández-Ramírez F, Zepeda LM, Nieto-Martínez K, Gómez-Laguna L, Garduño-Zarazúa LM, Berumen J, Kofman S, Cervantes A. Diagnosis of familial Wolf-Hirschhorn syndrome due to a paternal cryptic chromosomal rearrangement by conventional and molecular cytogenetic techniques. BioMed Res Int. 2013;2013:1–8.
Acknowledgements
We are very grateful to the family members for their kind participation and for their continuous interest in this study. We also thank the scientific and technical team of the cytogenetics Department at Farhat Hached University Teaching Hospital (Sousse, Tunisia) and Mr. M. Msaoura for English editing.
Funding
NA.
Author information
Authors and Affiliations
Contributions
SMZ contributed to conception and design. KR contributed to all experimental work, analysis and interpretation of data. IHH and AJ contributed partially to the experiment and analysis work. OK, HA and NM referred the patients and assured medical monitoring. SMZ and AJ were responsible for the consultation. SMZ and AS were responsible for overall supervision. KR drafted the manuscript, which was revised by SMZ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local Ethics Board of the University Teaching Hospital Farhat Hached approved the present study (IRB00008931) and written consents were taken from the parents for photo publication.
Consent for publication
The local Ethics Board approved the present study (IRB00008931) and written consents were taken from the parents for photo publication.
Competing interests
The authors have no conflicts of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rjiba, K., Ayech, H., Kraiem, O. et al. Disorders of sex development in Wolf–Hirschhorn syndrome: a genotype–phenotype correlation and MSX1 as candidate gene. Mol Cytogenet 14, 12 (2021). https://doi.org/10.1186/s13039-021-00531-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-021-00531-8