Abstract
Background
In spite of the global implementation of surgical safety checklists to improve patient safety, patients undergoing surgical procedures remain vulnerable to a high risk of potentially preventable complications and adverse outcomes. The present study was designed to explore the surgical teams’ perceptions of patient safety culture, capture their perceptions of the risk for adverse events, and identify themes of interest for quality improvement within the surgical department.
Methods
This qualitative study had an explorative design with an abductive approach. Individual semi-structured in-depth interviews were conducted between 10/01/23 and 11/05/23. The participants were members of surgical teams (n = 17), general and orthopedic surgeons (n = 5), anesthesiologists (n = 4), nurse anesthetists (n = 4) and operating room nurses (n = 4). Middle managers recruited purposively from general and orthopedic surgical teams in two tertiary hospitals in Norway, aiming for a maximum variation due to gender, age, and years within the specialty. The data material was analyzed following Braun and Clarke’s method for reflexive thematic analysis to generate patterns of meaning and develop themes and subthemes.
Results
The analysis process resulted in three themes describing the participants’ perceptions of patient safety culture in the surgical context: (1) individual accountability as a safety net, (2) psychological safety as a catalyst for well-being and safe performance in the operating room, and (3) the importance of proactive structures and participation in organizational learning.
Conclusions
This study provided an empirical insight into the culture of patient safety in the surgical context. The study highlighted the importance of supporting the individuals’ competence, building psychological safety in the surgical team, and creating structures and culture promoting a learning organization. Quality improvement projects, including interventions based on these results, may increase patient safety culture and reduce the frequency of adverse events in the surgical context.
Similar content being viewed by others
Background
Patient safety culture has been a proxy for quality of care during the last two decades and is commonly assessed using questionnaires [1, 2]. The most used and recommended questionnaires are the Safety Attitude Questionnaire and the Hospital Survey on Patient Safety Culture [1,2,3]. A recent study categorizes patient safety culture dimensions into tangible and intangible themes [2]. Tangible themes, including leadership, teamwork climate, and organizational structures, can be effectively captured by questionnaires [2]. Intangible themes with more underlying cultural dimensions, such as power, trust, psychological safety, ethics, and cohesion, are less easily captured by quantitative methods and could be explored by qualitative studies [1,2,3].
Patient safety culture correlates with safety performance, healthcare professionals’ well-being, patient outcomes, reporting, and incidence of adverse events [4,5,6,7,8,9,10]. Adverse events represent unintentional errors or patient injuries resulting from omission or commission in healthcare delivery [11]. Globally, these events affect an average of 10% of hospitalized patients [12, 13], and up to half of the adverse events are estimated to be preventable [11,12,13]. A significant proportion of the adverse events are related to the surgical context [11,12,13], and events tend to be more severe, often necessitating additional treatments [14, 15]. These iatrogenic injuries influence the health of patients, their families, and the involved healthcare professionals, who often experience guilt and self-criticism [16]. Healthcare professionals involved in adverse events often experience adverse emotional and physical reactions [16, 17]. Previous retrospective studies from the surgical context demonstrate that human performance deficiencies caused adverse events more than patient-related, organizational, or technical causes [14, 15]. Prospective studies could provide better insight into cognitive errors and potential structural causes of adverse events [11, 14, 15], and an enhanced understanding of intangible cultural themes may prompt initiatives to reduce the frequency of such events [2].
Qualitative evidence assessing patient safety culture is sparse, and further research should be based on more conceptual and theoretical frameworks [18]. Interprofessional surgical teams treat complex cases of vulnerable patients in a high-technological environment, and the dynamic roles and collaboration [19] and the high frequency of adverse events related to surgery [11] necessitate qualitative studies that broaden the understanding of patient safety culture in the surgical context [1, 2, 10]. The objectives of this study were to explore surgical teams’ perceptions and experiences of patient safety culture, including intangible themes and responses to adverse events, to capture their perceptions of the risk for adverse events, and to identify themes for quality improvement and education within the surgical context.
Methods
Study design
This study had an exploratory design with a qualitative abductive approach to improve the understanding of patient safety culture in a surgical context [20,21,22]. With an abductive approach, the research involves iterative movements between inductive and deductive strategies [21, 22]. We used Braun and Clarke’s recommendations for quality practice in thematic analysis to ensure the reporting of the study [23].
Participants
The participants were 17 members of surgical teams in two Norwegian tertiary hospitals in the South-Eastern Norway Regional Health Authority. In collaboration with middle managers, we purposively recruited and aimed for maximum variation regarding gender, age, and number of years in the specialty [22]. The included participants worked clinically in orthopedic and general surgical teams in departments operating acute and planned surgery on a 24/7 basis. The participation was based on voluntariness, and healthcare professionals in administrative functions or management were excluded.
Data collection
MV conducted individual in-person interviews between 10/01/23 and 11/05/23. The participants received a mind map to enhance their reflections and note their unsolicited experiences before the interviews [24] (see Additional file 1). The purpose of the mind map was to increase information richness and reduce recall bias [24]. Half the participants brought the mind map and looked at it during the interviews. The mind map was developed on the main topics in the semi-structured interview guide. The interview guide consisted of open-ended questions, allowing participants the flexibility to share broad and in-depth descriptions of their perceptions and experiences [22]. Despite the open-ended questions, the questions were developed from theory, and detailed descriptions and narratives were searched to provide insight into the underlying dimensions of patient safety culture. The main topics of the interview guide were patient safety, adverse events, and near-miss incidents (see Additional file 2). The interviews were conducted close to the participants’ clinical workplace of the participants’ choice and without disruptions. The interview setting was introduced with information about the project and MV, written informed consent, and questions about demographical characteristics. A digital recorder audiotaped and encrypted the dialogues, each lasting between 35 and 90 min. We recruited participants until the data had information richness according to Malterud’s model for evaluating information power [25].
Data analysis
The analysis process followed Braun and Clarke’s 6 phases for reflexive thematic analysis [26]. MV wrote field notes and transcribed the interviews verbatim to initiate analytic reflections and data familiarization [27]. Each interview provided 9 to 21 transcribed pages, resulting in 230 pages. The initial coding was inductive, semantic, and descriptive, and each of the 81 codes represented ‘an idea’ presented by the participants. The second coding resulted in 56 revised codes. MV used the software NVivo version 12 for analysis transparency, an overview of characteristics across the heterogenous dataset, and memos on reflexivity and interpretations. MV clustered codes with similar ‘core ideas’ and abstracted them into 6 candidate themes relevant to the study’s objectives. MV and SOD discussed the initial coding, initial themes, interpretations, and conceptual abstraction to generate ‘patterns of meaning/shared ideas’ across the dataset. MV generated the results by an iterative process over 3 months, moving between the data, interpretations, and revisions, inspired by literature and discussions with ECTD, ASH, and SOD. This panel of researchers included a physician, an anesthesia nurse, and an operating room nurse. Interpretations were iteratively and critically discussed, close to the raw data material, and related to a contextual understanding and relevant theory. Braun and Clarke describe their process of developing themes through reflexivity, subjectivity, and sensitivity [26]. The analytical process of reflexive thematic analysis is detailed in a table (Additional File 3).
Results
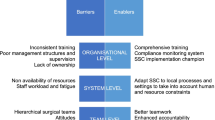
Demographic characteristics of the 17 participants are presented in Table 1. The analysis dissected the data on the surgical teams’ perceptions and generated 3 themes and 8 subthemes of shared understandings, as illustrated in Fig. 1. Each participant provided data fitting the themes. The themes are described in the text, and quotations and the number of participants providing data for the subthemes are presented in Table 2.
Theme 1: Individual accountability as a safety net
With their competence and genuine ambitions for quality in patient treatment, the healthcare professionals experienced that they constituted a safety net for the patient in the surgical context. The individuals within the surgical team emphasized being well prepared, obtaining patient information, and having an overview of the situation. The team members strived to identify and prevent the risk of adverse events and to reduce the extent of injuries.
Subtheme 1a: Role understanding and interprofessional accountability
Surgical team members emphasized the importance of experience and an in-depth understanding of their and others’ roles in the operating room. This insight was considered crucial to ensure that the omission and commission actions were conducted correctly and at the right time. Additionally, a comprehensive overview enabled team members to contribute to vigilance, availability, and responsibility beyond their expertise. Experience in the operating room was also underscored as essential for building situational awareness, and team members should know when and how to respond and communicate during the surgical procedure.
Subtheme 1b: Competence and commitment to healthcare delivery
Competence, professional involvement, and patient engagement were shared values among surgical team members. They expressed their dedication and loyalty to their profession and aimed for effective and high-quality patient treatment by meticulously preparing and verifying the available information to prevent adverse events. Team members felt ethically obliged to provide respect, information, and person-centered care. Parallel to this, physicians conveyed personal ambitions and placed high prestige on their healthcare delivery and careers. This prestige culture led to work beyond regular working hours and a risk of a non-complaining culture, where the physicians had to prove their dedication and capability. The high prestige was considered positive for the patient’s treatment. However, it could also increase the workload and emotional demand, thus increasing hazards and risks. The physicians expressed that when an event occurred, the prestigious culture could increase feelings of shame and blame. Concerns about one’s career could make it appealing to keep events secret, increasing the emotional stress and the risk of encountering further incidents.
Subtheme 1c: Balancing work demands and patient safety on a knife edge
Surgical team members noted that efficiency demands threatened patient safety. Heavy workload, complex patient cases, lack of time for preparation, and severe consequences of making errors involved moral distress and exhaustion. Additionally, a culture of not speaking up regarding workload, especially among physicians, could affect patient safety and personal health. Experience and robustness were required to demand time to investigate ambiguous situations further. Anesthesia professionals were often worried about their workload and having too few resources for readiness. The heavy workload entailed challenges in training new colleagues, and such training contributed to an even higher workload. For nurses, being measured for effectiveness rather than professionalism could lead to demotivation and thoughts of leaving the profession. Experienced physicians indicated that they were less worried about the workload. However, they sought policy guidelines for treatments hospitals should and should not offer. Additionally, the physicians highlighted that the frontline professionals’ autonomy in patient treatment, involvement in administrative processes, and reduced clerical burdens were required to solve these challenges. They experienced that the workload threatened continuity in patient treatment and information.
Theme 2: Psychological safety as a catalyst for well-being and safe performance in the operating room
A teamwork climate based on respect, cohesion, and psychological safety was considered essential for the surgical patient’s safety. Performed leadership and communication style influenced each team member’s performance and the team’s total achievement. Psychological safety and a culture of openness were encouraged to promote patients’ and healthcare professionals’ safety and to learn from events.
Subtheme 2a: Leadership and empowering communication
The participants had experienced various ways to lead and communicate in a surgical team. The surgeon was regarded as the leader and could lead and communicate in an empathic and empowering manner or a more authoritarian style with condescending communication. Participants from all specialties had experienced the negative effect of condescending communication. They described that such communication decreased the quality of their performance. The participants perceived that hierarchical and authoritarian leadership still existed in the operating room. However, the common perception was that empathic and egalitarian values gradually replaced this leadership style. Assertive leadership and affirmative communication increased the team members’ psychological safety, involvement, and performance quality. Team members were expected to be situationally aware of tense moments and condescending communication to empower the teamwork climate. Operating room nurses should ensure communication with the anesthetic professionals when the surgeons are in challenging situations. Inexperienced personnel found it more difficult to speak up, and experienced nurses built trust and respect by speaking up. The leading surgeon should encourage team members to speak up and emphasize their accountability.
Subtheme 2b: A supportive parachute and a culture of openness
The surgical team members understood that colleagues and managers would support them if an adverse event occurred. Nurses emphasized informal openness and individual learning from one another’s experiences. Physicians tended to seek support from a smaller number of allies they trusted and described previous experiences of cultures where events should be kept hidden due to hierarchy and prestige. Formal and informal role models provided essential guidance to create and maintain a supportive culture of openness. Managers and skilled, informal role models should share their adverse event experiences, promote the idea that everyone may experience an adverse event, and support colleagues who experience such an event. Managers and experienced role models should share their adverse event experiences to underscore that anyone can experience severe adverse events. The healthcare professionals’ demanding accountability and high levels of risk required a work environment that supported their psychological safety. They experienced a need for an immediate debrief after an adverse event, followed by a more systematic one. Managers should provide leaders or peer support for the involved parties. The surgical team members suggested that a culture without openness and support could result in healthcare professionals not processing their feelings after adverse events; They might become anxious, hurting their performance and threatening patient safety.
Subtheme 2c: Continuity and cohesion in the team
Team continuity and cohesion were accentuated to cultivate a teamwork climate that promoted patient safety, believed to be perceptible to the patients themselves, according to the healthcare professionals. They perceived that having trusted relationships with colleagues and knowing their competence contributed to a positive working environment and workflow, which could help maintain mental and physical balance during a surgical procedure. The surgical safety checklist was valuable for establishing a focused team with a shared understanding of the procedure. An extra ‘time out’ was considered effective to re-establish overview and communication if a situation turned chaotic and complex. Continuity during surgical procedures was pointed out as essential for the flow of information. Rapid changes in healthcare professionals, explicit use of substitute staff, and shift changes were considered potential threats to patient safety due to the lack of information transfer. The continuity of experienced personnel, few disruptions, and adequate staffing in the surgical department were perceived as facilitators for a calm and organized teamwork climate. Working environment and team cohesion were most mentioned and essential for nurses because the operating room is their primary work location.
Theme 3: The importance of proactive structures and participation in organizational learning
The healthcare professionals identified a need for improved structural systems for reporting and learning from adverse events, near-miss incidents, and successful performance. They desired that hospital management emphasized the prioritization of patient safety and the statement that management and frontline personnel had a common goal: quality in healthcare delivery.
Subtheme 3a: Forum for discussing risk, safety, and events among allied healthcare professionals
Few forums existed for discussing patient safety and risk, especially interprofessional ones. Interprofessional forums for discussing operation plans, reviewing adverse events, and establishing a common understanding of safety hazards and prevention were pointed out to contribute to organizational learning and practical procedure improvements. The participants experienced that the information about reported adverse events was random and that patient safety should instead be on the agenda daily, weekly, and periodically, both within and between specialties. They wanted near-miss incidents and successful narratives to be shared along with adverse events in these forums. A need to reduce the barriers to discussing adverse events with staff from other specialties was identified. Additionally, the frontline experienced a gap between the patient safety work performed by administrators and frontline staff and wanted managers at different levels to establish physical contact and dialogue with frontline staff to focus on patient safety, a good work environment, and increased staff motivation. The participants highlighted that synchronizing the voices of frontline staff with academic and administrative work and decisions could improve surgical care.
Subtheme 3b: An efficient and formal system for reporting and learning from adverse events
The members of the surgical teams had varied attitudes toward and trust in the existing reporting systems. Nurses felt obliged to report events and emphasized the learning perspective of adverse events. However, they perceived the reporting process as time-consuming and needed more feedback about how the reports were handled and their consequences. The lack of feedback demotivated nurses from writing new adverse event reports, which made them worried about reduced insights and learning from adverse events. Physicians preferred to talk with involved parties after an event and avoid criticism of themselves or colleagues. However, they sometimes recorded the events in patient journals and emphasized the importance of explaining adverse events to patients. A need for a trusted, well-defined, open, and time-effective reporting system to facilitate improvement was identified. Frontline staff requested insight into administrative handling, involvement in event analysis, and discussions on pertinent improvement efforts. In addition, they thought that clinical registers and staff surveys could be used more systematically for organizational development and learning.
Discussion
The results illustrated that patient safety culture in the surgical context needed to be addressed in processes and structures at multiple levels. At the individual level, this study’s participants emphasized ethical commitment and high-quality patient-centered care. In clinical processes at the team level, the teamwork climate was crucial for patient safety, healthcare professionals’ well-being, and organizational learning. In addition, the participants pointed to structural factors influencing the patient safety culture. This complexity aligned with Donabedian’s model for assessing healthcare quality and previous studies reporting that structural interventions, such as the safe surgery checklist, improve care processes and patient outcomes [28,29,30].
This study highlighted psychological safety in clinical processes as crucial for patient safety in the operating room. Psychological safety is characterized by a trusting and respectful collaboration in which team members feel free to speak up without interpersonal risk [31]. To feel free to speak up and challenge authorities is connected to safety culture [32]. Building and sustaining trust may be difficult, especially in hierarchical healthcare teams [6]. Participants in this study described how assertive leadership styles and empowering communication methods made them engage rather than withdraw from situations. These non-technical skills are considered essential for safety culture and are included in the ‘formula for survival in surgery’ for improved quality [33]. Leadership influences psychological safety, hence the team’s total involvement and performance [19, 34]. Encouraging and involving the whole team to share ideas and ask questions about patient safety, in and between specialties, can prevent adverse events, reduce costs, and increase patient satisfaction [32, 35, 36]. This study added that each team member must acknowledge their responsibility to speak up and build a trusting working relationship. Education, experience, and knowledge are individual characteristics that increase the confidence to speak up [37]. The results underlined the importance of retaining experienced team members, minimizing temporary replacements, and providing inexperienced team members with education and supervision. Simulation and communication training could improve the teamwork climate [32, 38, 39]. However, feeling confident to speak up begins with team familiarity, supportive leadership, and having a shared understanding of safety, checklists, and transparency regarding events [32, 35, 37, 38, 40].
Psychological safety enables a culture of openness and organizational learning [34]. The results of this study emphasized the importance of informal role models in creating communication openness and learning, especially in prestigious cultures. Supervisors and experienced personnel may contribute by fostering the acceptance of events, sharing their stories, and developing an environment conducive to learning from adverse events [34]. The participants described the feeling of shame and blame as inescapable emotions due to the commitment to maintain the patient`s safety and personal prestige. The literature supports this result [17, 41,42,43], and experiencing adverse events is associated with symptoms of emotional exhaustion, burnout, and turnover intentions [17]. Burnout among surgical residents is described as an epidemic, and the stress in the surgical context is described as constant [35]. This knowledge clarifies that support when an adverse event occurs is essential to prevent negative emotions such as anxiety and fear of future adverse events that influence cognitive functions [17]. This study added weight to the suggestion that healthcare professionals’ well-being may affect patient safety [38, 44, 45]. A previous review and this study highlighted the absence of structured peer support and debriefing after an adverse event [43]. These organizational processes may enable healthcare professionals to remain in their profession without experiencing intractable fear [16, 17, 41, 42].
This study highlighted the need for interprofessional arenas where the surgical team could work on a shared understanding of patient and psychological safety and learn from adverse events. O’Donovan [38] supports this need, claiming that learning across specialties is essential in complex collaborations, such as a surgical team. A recent review of ‘Morbidity and Mortality Meetings’ reports that well-implemented and administered meetings are related to organizational learning and patient safety culture facilitates the effect of these meetings [46]. Additionally, this latter review points to the need for clinical engagement in quality improvement [46]. O’Donovan [38] supports the need for arenas where hospital leadership meets the frontline workers to understand their perspectives on the quality of care. The lack of these organizational processes and structural factors, such as a heavy workload and administrative burden, could threaten patient safety [35]. This raised some suggestions for improvement in the surgical context. Quality improvement should be grounded in the current context and considered according to other processual and structural variables [38]. The ‘human errors’ described in the literature [14, 15] should be analyzed with frontline workers and include structural perspectives, such as staff change, workload, time pressure, ergonomics, and equipment [47]. Likewise, there could be justifications for exploring patients’ perceptions and experiences regarding adverse events. Finally, leaders should promote proactive learning from successful pathways for a positive learning perspective because of the high number of successful surgical procedures [38, 44, 48]. Focusing on success and learning from excellence represent a new paradigm of safety, described as the ‘safety 2-perspective’ and ‘resilience engineering’ in the literature [48,49,50]. ‘Safety 2’ represents approaches and methodologies to learn from success, and resilience refers to the robustness and the ability to adjust the healthcare performance due to variations in the actual conditions. Thus, understanding and increasing resilience at multiple organizational levels should complement the traditional ‘safety 1-perspective’ focusing on understanding adverse events retrospectively to prevent errors [49].
This study had multiple strengths. First, there was a high information power in the data. Second, the shared ideas and common patterns of meaning generated from a heterogeneous dataset were valuable [22]. Third, methodological integrity and rigorous analysis increased trustworthiness. Audit trails, author analysis meetings, and presented quotations ensured credibility, confirmability, and authenticity. The descriptive data of the participants increased the dependability and the reader’s possibility to evaluate the relevance in other settings. However, this study also had limitations. First, safety cultural perspectives were contextually bonded and limited to general and orthopedic surgeries in two large, urban Norwegian hospitals. Second, the reflexivity in the analytical process may have influenced the authors’ interpretations. Finally, the participants shared what they felt like, which could constitute self-selection bias and influence the potential to capture the intangible dimensions.
Conclusion
This explorative study contributed to increased knowledge of patient safety culture in a surgical context by highlighting the importance of healthcare professionals’ experience and competence, psychological safety in surgical teams, and structural systems promoting organizational learning. Further research might include processual interventions for creating a culture of psychological safety and openness and structural improvements as a trusted reporting system, interprofessional forums, and forums for frontline personnel and the administration to discuss patient safety. Finally, the perspectives of the surgical team could be complemented by surgical patients’ perspectives.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Churruca K, Ellis LA, Pomare C, Hogden A, Bierbaum M, Long JC, et al. Dimensions of safety culture: a systematic review of quantitative, qualitative and mixed methods for assessing safety culture in hospitals. BMJ Open. 2021;11(7): e043982.
Malik RF, Buljac-Samardžić M, Akdemir N, Hilders C, Scheele F. What do we really assess with organisational culture tools in healthcare? An interpretive systematic umbrella review of tools in healthcare. BMJ Open Qual. 2020;9(1): e000826.
de Carvalho REFL, Bates DW, Syrowatka A, Almeida I, Sousa L, Goncalves J, et al. Factors determining safety culture in hospitals: a scoping review. BMJ Open Quality. 2023;12(4): e002310.
Kalteh HO, Mortazavi SB, Mohammadi E, Salesi M. The relationship between safety culture and safety climate and safety performance: a systematic review. Int J Occup Saf Ergon. 2021;27(1):206–16.
Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety – development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016;16:281.
Falcone ML, Van Stee SK, Tokac U, et al. Adverse event reporting priorities: an integrative review. J Patient Saf. 2022;18(4):e727–40.
Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11): e017708.
Lee SE, Scott LD, Dahinten VS, Vincent C, Lopez KD, Park CG. Safety culture, patient safety, and quality of care outcomes: a literature review. West J Nurs Res. 2019;41(2):279–304.
DiCuccio MH. The relationship between patient safety culture and patient outcomes: a systematic review. J Patient Saf. 2015;11(3):135–42.
Vikan M, Haugen AS, Bjørnnes AK, Valeberg BT, Deilkås ECT, Danielsen SO. The association between patient safety culture and adverse events – a scoping review. BMC Health Serv Res. 2023;23(1):300.
Jung JJ, Elfassy J, Jüni P, Grantcharov T. Adverse events in the operating room: definitions, prevalence, and characteristics. A Systematic Review World J Surg. 2019;43(10):2379–92.
de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17(3):216–23.
Schwendimann R, Blatter C, Dhaini S, Simon M, Ausserhofer D. The occurrence, types, consequences and preventability of in-hospital adverse events - a scoping review. BMC Health Serv Res. 2018;18(1):521.
Suliburk JW, Buck QM, Pirko CJ, Massarweh NN, Barshes NR, Singh H, et al. Analysis of human performance deficiencies associated with surgical adverse events. JAMA Netw Open. 2019;2(7): e198067.
Zegers M, de Bruijne MC, de Keizer B, Merten H, Groenewegen PP, van der Wal G, et al. The incidence, root-causes, and outcomes of adverse events in surgical units: implication for potential prevention strategies. Patient Saf Surg. 2011;5:1–11.
Buhlmann M, Ewens B, Rashidi A. The impact of critical incidents on nurses and midwives: a systematic review. J Clin Nurs. 2021;30(9–10):1195–205.
Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and psychosomatic symptoms of second victims of adverse events: a systematic review and meta-analysis. J Patient Saf. 2020;16(2):e61–74.
Alqattan H, Morrison Z, Cleland JA. A narrative synthesis of qualitative studies conducted to assess patient safety culture in hospital settings. Sultan Qaboos Univ Med J. 2019;19(2):e91–8.
Kumar H, Morad R, Sonsati M. Surgical team: improving teamwork, a review. Postgrad Med J. 2019;95(1124):334–9.
Maxwell JA. Qualitative research design: an interactive approach. 3rd ed. Los Angeles: Sage; 2013.
Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29–34.
Patton MQ. Qualitative research & evaluation methods: integrating theory and practice. 4th ed. Los Angeles: Sage; 2015.
Braun V, Clarke V. Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol Rev. 2023;17(4):695–718.
Wheeldon J, Faubert J. Framing experience: concept maps, mind maps, and data collection in qualitative research. Int J Qual Methods. 2009;8(3):68–83.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Braun V, Clarke V. Thematic analysis: a practical guide. Los Angeles: Sage; 2022.
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. Los Angeles: Sage; 2013.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–8.
Haugen AS, Wæhle HV, Almeland SK, Harthug S, Sevdalis N, Eide GE, et al. Causal analysis of World Health Organizationʼs surgical safety checklist implementation quality and impact on care processes and patient outcomes: secondary analysis from a large stepped wedge cluster randomized controlled trial in Norway. Ann Surg. 2019;269(2):283–90.
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–9.
Edmondson AC, Lei Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43.
Pattni N, Arzola C, Malavade A, Varmani S, Krimus L, Friedman Z. Challenging authority and speaking up in the operating room environment: a narrative synthesis. Br J Anaesth. 2019;122(2):233–44.
Søreide K. A formula for survival in surgery. Patient Saf Surg. 2023;17(1):1–5.
Edmondson AC, Bransby DP. Psychological safety comes of age: Observed themes in an established literature. Annu Rev Organ Psychol Organ Behav. 2023;10(1):55–78.
Swendiman RA, Edmondson AC, Mahmoud NN. Burnout in surgery viewed through the lens of psychological safety. Ann Surg. 2019;269(2):234–5.
Jones A, Blake J, Adams M, Kelly D, Mannion R, Maben J. Interventions promoting employee “speaking-up” within healthcare workplaces: A systematic narrative review of the international literature. Health Policy. 2021;125(3):375–84.
Wawersik DM, Boutin ER, Gore T, Palaganas JC. Individual characteristics that promote or prevent psychological safety and error reporting in healthcare: a systematic review. J Healthc Leadersh. 2023;15:59–70.
O’Donovan R, Ward M, De Brún A, McAuliffe E. Safety culture in health care teams: a narrative review of the literature. J Nurs Manag. 2019;27(5):871–83.
Park O, Jeon M, Kim M, Kim B, Jeong H, editors. The Effects of a Simulation-Based Patient Safety Education Program on Compliance with Patient Safety, Perception of Patient Safety Culture, and Educational Satisfaction of Operating Room Nurses. Healthcare; 2023;11:2824
O’Donovan R, McAuliffe E. A systematic review of factors that enable psychological safety in healthcare teams. Int J Qual Health Care. 2020;32(4):240–50.
Bamdad MC, Vitous CA, Rivard SJ, Anderson M, Lussiez A, De Roo A, et al. What we talk about when we talk about coping: a qualitative study of surgery resident’s coping after complications and deaths. Ann Surg. 2023;278(2):e422–8.
Sandhu H, Foote DC, Evans J, Santosa KB, Kemp MT, Donkersloot, et al. “The story I will never forget”: Critical incident narratives in surgical residency. Ann Surg. 2023;277(3):e496–502.
Sattar R, Johnson J, Lawton R. The views and experiences of patients and health-care professionals on the disclosure of adverse events: a systematic review and qualitative meta-ethnographic synthesis. Health Expect. 2020;23(3):571–83.
Ellis LA, Falkland E, Hibbert P, Wiig S, Ree E, Schultz TJ, et al. Issues and complexities in safety culture assessment in healthcare. Front Public Health. 2023;11:1217542.
Adair KC, Heath A, Frye MA, Frankel A, Proulx J, Rehder KJ, et al. The Psychological Safety Scale of the Safety, Communication, Operational, Reliability, and Engagement (SCORE) Survey: A Brief, Diagnostic, and Actionable Metric for the Ability to Speak Up in Healthcare Settings. J Patient Saf. 2022;18(6):513–20.
Steel EJ, Janda M, Jamali S, Winning M, Dai B, Sellwood K. Systematic Review of Morbidity and Mortality Meeting Standardization: Does It Lead to Improved Professional Development, System Improvements, Clinician Engagement, and Enhanced Patient Safety Culture? Journal of Patient Safety. 2023;10:10–1097.
Kolodzey L, Trbovich P, Kashfi A, Grantcharov TP. System factors affecting intraoperative risk and resilience: applying a novel integrated approach to study surgical performance and patient safety. Ann Surg. 2020;272(6):1164–70.
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care. 2015;27(5):418–20.
Plunkett A, Plunkett E. Positive approaches to safety: learning from what we do well. Pediatr Anesth. 2022;32(11):1223–9.
Ellis LA, Churruca K, Clay-Williams R, Pomare C, Austin EE, Long JC, et al. Patterns of resilience: A scoping review and bibliometric analysis of resilient health care. Saf Sci. 2019;118:241–57.
Acknowledgements
We appreciate the participants dedicating their time and sharing their experiences, and Scribendi for language editing.
Funding
Open access funding provided by OsloMet - Oslo Metropolitan University No funding was received for this study.
Author information
Authors and Affiliations
Contributions
MV led the study, conducted the data collection and analysis, and wrote the article. SOD supervised and contributed to all parts of the study: Conceptualising and design, analysis and writing process. ECD and ASH contributed to the analysis meetings, and all authors reviewed and revised the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Norwegian Agency for Shared Services in Education and Research approved the study, reference number 307019, and the participants signed a consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Mind Map.
Additional file 2.
Interview Guide.
Additional file 3.
Reflexive Thematic Analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vikan, M., Deilkås, E.C., Valeberg, B.T. et al. The anatomy of safe surgical teams: an interview-based qualitative study among members of surgical teams at tertiary referral hospitals in Norway. Patient Saf Surg 18, 7 (2024). https://doi.org/10.1186/s13037-024-00389-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-024-00389-w