Abstract
Background
The coronavirus disease (COVID‐19) and universal mitigation strategies have fundamentally affected peoples’ lives worldwide, particularly during the first two years of the pandemic. Reductions in physical activity (PA) and increased mental health (MH) problems among children and youth have been observed. This systematic review and meta-analysis investigated the relationship between physical activity (PA) and mental health (MH) among children and youth during the COVID‐19 pandemic.
Methods
Four electronic databases (EMBASE, PsycINFO, PubMed, and Web of Science) were systematically searched to identify studies that (1) examined the relationship between PA and MH among children and youth (aged 2–24 years old) and (2) were published in peer-reviewed journals in English between January 2020 and December 2021. Relationships between PA and two MH aspects (i.e., negative and positive psychological responses) among children and youth at different age ranges and those with disabilities or chronic conditions (DCC) were synthesized. Meta-analyses were also performed for eligible studies to determine the pooled effect size.
Results
A total of 58 studies were eventually included for variable categorization, with 32 eligible for meta-analyses. Our synthesis results showed that greater PA participation was strongly related to lower negative psychological responses (i.e., anxiety, depression, stress, insomnia, fatigue, and mental health problems) and higher positive psychological responses (i.e., general well-being and vigor) in children and youth during COVID-19. The pattern and strength of relations between PA and MH outcomes varied across age ranges and health conditions, with preschoolers and those with DCC receiving less attention in the existing research. Meta-analysis results showed that the magnitude of associations of PA with negative (Fisher’s z = − 0.198, p < 0.001) and positive (Fisher’s z = 0.170, p < 0.001) psychological responses among children and youth was weak. These results were linked to age of participants, study quality, and reporting of PA-related information.
Conclusions
PA participation and MH among children and youth deteriorated during the COVID-19 pandemic and were closely associated with each other. For the post-COVID-19 era, additional research on age- and health condition-specific relationships between PA and MH outcomes from a comprehensive perspective is warranted. (Word count: 344 words).
Similar content being viewed by others
Introduction
Mental Health (MH) problems constitute the largest health concern for children and youth worldwide in the twenty-first century [1]. Representing MH states are two psychological responses: negative, which consist of unpleasant feelings or emotions and symptoms related to clinically diagnosed ill-being [2, 3]; and positive, which consist of affective states and psychological well-being beneficial to one’s life [2, 4,5,6,7,8]. MH is influenced by many factors [9], including physical activity (PA), referred to as any type of physical movement that increases energy expenditure [10]. It has been documented that regular PA participation is protective for MH by preventing and managing negative psychological responses [10, 11]. Engaging in an adequate level of PA regularly is important for promoting people’s physical and mental health, especially for children and youth [12]. However, the majority of young people are not meeting WHO’s PA guideline (i.e., an average of 60 min per day of moderate-to-vigorous PA intensity), which has resulted in a worldwide critical public health issue [13]. Moreover, a number of studies have demonstrated that physical inactivity deteriorates as age increases [14, 15].
PA and MH are theoretically and empirically associated, and the relation is bidirectional [16]. For example, Sampasa-Kanyinga [17] reported that a low level of PA is closely related to high levels of negative psychosocial responses (e.g., anxiety, depression, stress, negative affect, and distress) among children and youth. Not surprisingly, other studies found that a high level of PA is related to positive outcomes, such as well-being, self-esteem, self-concept, and resilience [16,17,18]. As early as 2011, a meta-analysis based on randomized controlled trials (RCTs) revealed that increased levels of PA are significantly associated with improved MH among children [19]. In 2019, another meta-analysis reported that the effects of PA on psychological ill-being (effect size = 0.130, p = 0.007) and psychological well-being (effect size = 0.189, p = 0.001) among children and youth are small but significant [16]. Thus, as improvements in MH reflect fewer negative psychological responses and more positive ones [20, 21], both positive and negative psychological responses should be considered when facilitating a comprehensive understanding of the relation between PA and MH.
The coronavirus disease (COVID-19) is an ongoing pandemic caused by a novel coronavirus, the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) [22]. Many countries implemented physical distancing measures, national lockdowns, and travel restrictions to control the spread of COVID-19 during the first two years of the outbreak [23]. As a protection for children and youth, restrictions to physically attend a majority of schools and universities were implemented worldwide, with an estimated 1.5 billion students transitioning to online learning [24]. These school restrictions and other social behavioral adaptations (e.g., social distancing, isolation) severely impacted the 24 h lifestyle of many children and youth [25], resulting in decreased opportunities for PA and increased sedentary behavior [26].
Moreover, the outbreak of COVID-19 has been accompanied by significant global MH challenges [27]. For example, an increasing number of studies have reported higher levels of anxiety, depression, and stress among children (ages 6–12 years) who experienced family isolation and school closures during COVID-19 [28,29,30]. Other studies have shown that people who were able to maintain more total time in moderate to vigorous PA were 12–32% less likely to experience depressive symptoms and 15–34% less likely to experience anxiety during COVID-19 [28, 31,32,33]. Although several existing reviews published in 2021 and 2022 demonstrated the relation between PA and MH among children during COVID-19 [28, 31, 33,34,35,36], they focused mainly on specific negative psychological responses (i.e., anxiety, depression and stress) with only a limited number of eligible studies being included. Additionally, the impacts of COVID-19 on PA and MH appear to be greater among children and youth with disabilities or chronic conditions (DCC) than their peers without DCC [28, 37]. However, within the COVID-19 context, a comprehensive understanding of the relationship between PA and MH among children and youth, including those with DCC, is still lacking. The relationship between PA and MH may be stronger in children and youth during COVID-19 than before COVID-19; and the pattern and extent of this relationship may vary by age range and disability status.
According to the theory of positive psychology, an adversity can enhance the ability of certain populations to cope positively and creatively with stress and distress [38]. During the COVID-19 pandemic, some people with an optimistic mindset counteracted negative impacts by making the most of limited resources and by being physically active and exercising at home [38, 39]. It is important to encourage children and youth to overcome the negative impacts of the COVID-19 pandemic by using methods, such as PA participation, that foster positive emotions and optimism [40]. Therefore, the purpose of this systematic review and meta-analysis was to evaluate the association of PA with MH in terms of both negative and positive psychological responses among children and youth within the context of COVID-19. Specifically, we asked two questions: (1) Did close relationships between PA and MH outcomes occur among children and youth during COVID-19?; and (2) Did the pattern and magnitude of such relationships vary by age range and disability status? We hypothesized that: (1) there would be close relationships between PA and MH outcomes in terms of both negative and positive psychological responses among children and youth during COVID-19; and (2) the pattern and magnitude of the relationships would vary in different age ranges and health conditions (i.e., with and without DCC). Information gained in this systematic review and meta-analysis will not only facilitate a better understanding of the relation between PA and MH, but also inform new research on how to promote PA and MH among children and youth during any future COVID-19-type pandemic.
Method
The conduct and reporting of this review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [41]. Registration for this protocol was completed on the Prospero database (reference number: CRD42022303342).
Search strategy
Four electronic databases (i.e., Embase, PsycINFO, PubMed, and Web of Science) were systematically searched to identify relevant studies published between January 2020 and December 2021. This end date was chosen since the impact of COVID-19 on daily life, including isolation policies, gradually diminished in many countries starting in the second half of 2021 [42,43,44,45]. The search items were grouped into four components: (1) physical activity (physical activity OR exercise OR sport), (2) mental health (mental health OR mental problem OR mental illness OR mental disorder OR well-being OR depression OR anxiety OR stress OR happiness), (3) age group of interest (child OR adolescent OR youth), and (4) COVID-19 (COVID-19 OR SARS-CoV-2). An example of the search strategy can be found in Additional file 1: Table S1.
Eligibility criteria
Inclusion criteria were: (1) participants were children and youth aged 2 to 24 years with and without DCC; (2) studies reported a potential relationship between any type of PA and at least one MH outcome in the context of COVID-19, which enabled evidence for specific correlates to be determined; (3) studies used a cross-sectional, longitudinal, or experimental design; and (4) articles were published in a peer-reviewed journal in English. Qualitative studies, reviews, books, dissertations, conference proceedings, commentaries, and studies without full-text were excluded.
Study selection
After conducting the initial search and removing all duplicates, two reviewers (BL, JY) were trained to independently perform title/abstract and full-text screening for the inclusion of records with a yes, unsure, or no approach. Inter-rater reliability between the two reviewers at the two screening phases was calculated using the κ statistic. κ values between 0.60 and 0.74 were deemed as having good agreement, and values > 0.75 were deemed as having excellent agreement [46]. Any discrepancy between the two reviewers at any stage was jointly reviewed and discussed with a third reviewer (JJY) until a consensus was achieved.
Quality assessment
Two reviewers (BL, JY) independently rated the methodological quality of all the included studies. Inter-rater reliability was calculated using the intraclass correlation coefficient. To assess observational studies employing cross-sectional and longitudinal designs, we used the modified Newcastle–Ottawa Scale [47], which included seven items consisting of three quality components: selection (4 items, maximum 5 points), comparability (1 item, maximum 2 points), and outcome (2 items, maximum 3 points). Each criterion received zero to two points and summed to a final score (maximum 10 points). The methodological quality of a specific study was considered high if it was scored as 9 to 10, medium if scored as 5 to 8, and low if scored as 4 or less. To assess studies involving RCTs, we used the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool [18], which included six quality components: selection bias, design, confounders, blinding, data collection, withdrawal and dropout. An overall rating was determined based on the ratings of the above constructs. RCT studies were categorized as high quality if no weak ratings were present, medium if there was only one weak rating, and low if there were two or more weak ratings.
Data extraction
All data from the included records were extracted by one reviewer (BL) and double checked by a second reviewer (JY). For each study, we coded the following bibliographic information: (1) first author’s name, (2) publication year, and (3) study location. We then coded the following variables from each study: (1) study design type (observational or experimental), (2) participant characteristics (age, sample size, and the number of girls and boys), (3) measures and outcomes of PA (e.g., custom questionnaire, the accelerometer) and MH, (4) main findings (relationship between PA and MH). Follow-up time was extracted for longitudinal studies, and experimental conditions and intervention components, were extracted for experimental studies.
Evidence synthesis
The relationship between PA and MH in different age ranges was determined by examining the percentage of studies that reported a statistically significant relationship [48]. Referring to previous studies [16, 50] and the definition of age ranges of youth by United Nations [49], participants were categorized as follows: age group 1 (2–5 years), age group 2 (6–12 years), age group 3 (13–18 years), and age group 4 (19–24 years). The relationship between PA and MH in participants with DCC was synthesized separately.
The coding rules were: MH outcomes with different terms but the same concepts were combined into a single identification factor. If a study examined the relationship between PA and one or more sub-dimensions of an MH outcome and most of the sub-dimensions had consistent associations with PA, this could be summarized as a general result of the association of PA with that MH outcome. Various statistical techniques (e.g., t-test, analysis of variance, linear regression, and logistic regression) were used in the included studies to estimate the associations between MH and PA outcomes. For each article, a statistically significant relationship between MH and PA was coded as “relevant” while a statistically insignificant one was coded as “irrelevant” [48]. A summary code of the relationship between each MH outcome and PA was obtained by dividing the number of findings supporting a specific MH outcome associated with PA by the total number of studies that examined the relationship between PA and that particular MH outcome. If 0–33% of the studies reported a statistically significant relationship between PA and MH, the result was categorized as “no association” (0). If 34–59% of the studies reported a statistically significant relationship between PA and MH, the result was categorized as “inconsistent” or “uncertain” (?). If 60–100% of the studies reported a positive or negative relationship between PA and MH, the result was coded as a “positive association” or “negative association” (+)/(–). Double summary codes were indicated as (00), (??), (+ +), or (– –) when three or more studies consistently supported no association, inconsistent, or positive or negative association, respectively. Evidence for the relationship between a specific MH outcome and PA was considered as sufficient only if such relationship obtained a double summary code.
Meta-analysis
We selected a minimum of ten studies investigating the same MH dimension or outcome for the meta-analysis. All values of the correlations between PA and MH were transformed into Fisher’s z scores and eventually used in the meta-analysis. The Fisher transformation of the correlation coefficient was chosen because the assumption of normality of the results obtained after the transformation would be more plausible [51]. The Fisher’s z transformation was a two-step process that first converted the relevant data describing the relationship between PA and MH (e.g., regression coefficient β, odds ratio, or other effect sizes) into a correlation coefficient r using Psychometrica (https://www.psychometrica.de/effect_size.html). This step was not necessary if the correlation coefficient r was reported in the study. Using the online platform Practical Meta-Analysis Effect Size Calculator, we transformed all correlation coefficient r values to Fisher’s z scores to obtain standardized data for conducting the subsequent meta-analysis (http://www.campbellcollaboration.org/escalc/html/EffectSizeCalculatorHome.php). When an article reported multiple quantitative values of the relationship between PA and MH (e.g., the correlation coefficient between PA and MH for boys and girls was reported separately), we calculated Fisher’s z scores for boys and girls separately based on the reported values and the corresponding number of participants. Fisher’s z scores of 0.12, 0.24, and 0.41 were interpreted as a small, medium, and large effect, respectively [36].
The Stata software version 16.0 (Stata Corp, College Station, TX, USA) was used to perform the meta-analysis. Owing to the anticipated heterogeneity across studies, we conducted a random-effects model. Heterogeneity was quantified with Q statistic and I2. Q test (p < 0.10) and an I2 > 75% indicated a significant high-level heterogeneity [52]. When a high-level heterogeneity appeared, subgroup analyses were performed. If the subgroup analyses could not resolve the high heterogeneity, appropriate univariate meta-regression analyses were performed to explore potential influencing factors, including age of participants, report of total and dimensions (duration, frequency, intensity) of PA, study design (interventional, observational), and disability population group [52, 53]. Additionally, funnel plots and Egger’s tests were performed to assess the risk of publication bias. Funnel plots provided a visual representation of the symmetric distribution of the studies. When the funnel plot was asymmetric, Egger’s tests were conducted to further assess the risk of publication bias. If the Egger’s test was significant (p < 0.05), the trim-and-fill method was used to adjust for the suspected publication bias and recalculate the pooled effect size [54, 55].
Results
Study selection
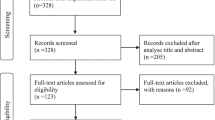
The search yielded a total of 3953 records. After removing duplications and screening for titles, abstracts, and full-texts, 58 records were included in this systematic review for categorization of variables, with 32 of them applicable for the meta-analysis. The inter-rater reliability between the two reviewers was good for the title and abstract screening (κ = 0.88) and full-text screening (κ = 0.82). The flowchart for the selection process is shown in Fig. 1.
Overview of studies
This systematic review included 58 articles conducted in 18 countries: China (n = 23), The United States (n = 7), Canada (n = 6), Italy (n = 3), Korea (n = 3), Brazil (n = 2), Germany (n = 2), The United Kingdom (n = 2), Bangladesh (n = 1), The Czech Republic (n = 1), Greece (n = 1), Hungary (n = 1), Iran (n = 1), Israel (n = 1), Lithuania (n = 1), Pakistan (n = 1), Poland (n = 1), and Saudi Arabia (n = 1). Of the included studies, 49 (84%) were published in 2021 (first quarter, n = 6; second quarter, n = 11; third quarter, n = 12; fourth quarter, n = 20), 51 were cross-sectional, four were experimental, and three were longitudinal. The number of participants ranged from 64 to 1,199,320, and their ages ranged from 2 to 24 years old. The most frequently studied age range was 13–18 years (n = 38), followed by 6–12 years (n = 22), 19–24 years (n = 16), and 2–5 years (n = 2). Additionally, 13 of the 58 included studies involved individuals with DCC (e.g., obesity, ADHD, mental illness).
Regarding the measurement of PA, 29 (50%) of the included studies used custom questionnaires, 27 (47%) used known questionnaires (e.g., International Physical Activity Questionnaire) with psychometric properties reported, and 4 (7%) used device based measures. The majority (n = 52, 90%) of included studies used validated questionnaires or scales to evaluate MH outcomes. The top five most frequently used measurements of MH included Patient Health Questionnaire-9 (n = 6), The Depression Anxiety Stress Scale (n = 6), Generalized Anxiety Disorder Scale-7 (n = 5), Center for Epidemiologic Studies Depression Scale (n = 5), and Strengths and Difficulties Questionnaire (n = 4). Additionally, eight included studies either directly selected sub-scale(s) from a validated measurement or developed a new scale based on an existing measurement with adaptations. For example, the COVID-19 Fear Scale was developed in one study as an adaptation of the SARS Fear Scale [59].
A variety of MH outcomes consisting of 36 negative responses and 16 positive responses were investigated in the included studies. Of the negative responses, depression (n = 23), anxiety (n = 21), and stress (n = 11) were investigated most frequently, followed by insomnia (n = 6), COVID-19 stress (n = 3), fatigue (n = 3), mental health problems (n = 3), negative affect (n = 3), anger (n = 2), boredom (n = 2), confusion (n = 2), distress (n = 2), emotional and behavioral problems (n = 2), loneliness (n = 2), tension (n = 2), tiredness (n = 2), aggressiveness (n = 1), being more stressed (n = 1), COVID-19 fear (n = 1), event-specific distress (n = 1), exercise dependence (n = 1), feeling more horrified (n = 1), feeling more apprehensive (n = 1), feeling more helpless (n = 1), feelings of loss of control (n = 1), having greater study pressure (n = 1), hyperactive-impulsive (n = 1), irritability (n = 1), inattention (n = 1), internalizing and functioning problems (n = 1), negative arousal (n = 1), pessimism (n = 1), perceived vulnerability (n = 1), psychosocial and behavioral problems (n = 1), post-traumatic stress disorder (PTSD) (n = 1), and sadness (n = 1). In contrast, general well-being (n = 13) was the most frequently studied positive response, followed by positive affect (n = 3), self-esteem (n = 3), vigor (n = 3), health-related quality of life (n = 2), life satisfaction (n = 2), resilience (n = 2), happiness (n = 1), mental health performance (n = 1), mental health importance (n = 1), optimism (n = 1), positive energy (n = 1), positive outlook (n = 1), prosocial behavior (n = 1), perceived health (n = 1), and relaxation (n = 1). The details of each included observational and experimental study are summarized in, Tables 1, 2, respectively.
Quality assessment
Of the 58 included studies, 53 (91%) were rated as medium in the quality assessment, three were rated as high, and two were rated as low. For the methodological quality ratings (see Tables 1, 2), the inter-rater reliability between the two reviewers was good (intraclass correlation coefficient = 0.77).
Data syntheses
Changes in physical activity and mental health of children and youth during COVID-19
In the present review, 11 included studies reported a significant decrease in PA among children and youth during COVID-19. For example, one study revealed that only 3.6% of children (5–11 years) and 2.6% of youth (12–17 years) in Canada participated in moderate to vigorous PA for at least 60 min per day during COVID-19 [114]. Another study showed that Spanish children spent 91 min per day less on PA during COVID-19 than before [25]. Such PA reductions were reflected in various components, including duration, frequency, and intensity [57, 68, 78, 80, 83, 84, 115,116,117].
Regarding the impact of COVID-19 on MH, 25 included studies showed that the MH of children and youth deteriorated during the pandemic. For example, one study found that COVID-19 caused significantly elevated levels of anxiety in youth [118], while another showed an increase in depressive symptoms in the 6–12- and 13–18-year-old groups [91]. Additional studies reported a significant increase in psychological distress [119] and an indirect increase in stress levels [107] among youth. As mentioned earlier, COVID-19 not only impacted common negative responses such as depression, anxiety, and stress among children and youth, but also led to increased occurrences of less common mental problems. One study, for instance, showed that during COVID-19, children and youth became more attached, inattentive, and irritable, and preschoolers were more likely to manifest signs of clinginess and fear [120]. Positive responses were also affected, including significant decreases in levels of well-being and overall mental health among children and youth [68, 78, 80, 121]. It is worth noting that children and youth with DCC exhibited a higher incidence of severe psychosocial dysfunction and a lower level of PA compared to their peers without DCC [56, 57, 76, 88, 108].
The relationship between physical activity and mental health among children and youth during COVID-19
Overall findings
As shown in Table 3, PA was strongly and negatively correlated with depression (21 of 23 studies, 91.3%), anxiety (14 of 21 studies, 66.7%), stress (7 of 11 studies, 63.6%), insomnia (4 of 6 studies, 66.7%), fatigue (3 of 3 studies, 100%), and mental health problems (3 of 3 studies, 100%). Although PA was negatively related to COVID-19 stress, negative affect, anger, confusion, distress, emotional and behavioral problems, COVID-19 fear, exercise dependence, feelings of loss of control, irritability, negative arousal, pessimism, psychosocial and behavioral problems, and sadness, and positively related to hyperactive/impulsive and perceived vulnerability, the evidence was considered insufficient since less than three studies consistently supported a specific association. PA’s relationship with each of the remaining negative response outcomes was either inconsistent or no association. Regarding positive psychological responses, PA showed strong and positive associations with general well-being (11 of 13 studies, 84.6%) and vigor (3 of 3 studies, 100%). Although PA was positively related to positive affect, self-esteem, health-related quality of life, life satisfaction, resilience, happiness, mental health performance, mental health importance, optimism, positive energy, positive outlook, prosocial behavior, perceived health, and relaxation, the evidence was considered insufficient.
Findings across age ranges
The present systematic review showed PA was strongly and negatively correlated with depression and strongly and positively correlated with general well-being in all age groups. However, different correlations between PA and negative responses occurred in different age groups. In the 6–12-year-old group, PA was not associated with stress, but was strongly and negatively correlated with anxiety and mental health problems. In the 13–18-year-old group, PA was strongly and negatively correlated with anxiety, stress, insomnia, and fatigue. In the 19–24-year-old group, findings on PA’s associations with anxiety, stress, and insomnia were inconsistent. Furthermore, PA was negatively correlated with fatigue though evidence was insufficient in the 13–18- and 19–24-year-old groups. Among the positive responses, PA was strongly and positively correlated with vigor in the 13–18-year-old group, and positively correlated in the 6–12- and 19–24-year-old groups though the evidence was insufficient. As with negative responses, we found that the 13–18-year-old group demonstrated the greatest variety of positive responses, indicating that researchers were most concerned about the responses of this age group during the COVID-19 pandemic.
Findings among children and youth with disabilities or chronic conditions (DCC)
Only eight negative psychological responses and four positive ones were investigated regarding the association of PA and MH among children and youth with DCC. The synthesized results showed that PA was strongly and negatively correlated with depression and anxiety in this population group (see Table 3). For example, one included study showed that children with ADHD who engaged in less than one hour of exercise per day were more likely to exhibit increased depressive symptoms during COVID-19 [94]. However, the associations of PA with all positive psychological responses were considered insufficient.
Meta-analytic results
The relationship between physical activity and negative psychological responses
The meta-analysis results showed PA was weakly and negatively correlated with negative responses (Fisher’s z = − 0.170, 95% CI [− 0.22, − 0.12], p < 0.001, I2 = 92.42%) (see Fig. 2). Because Egger’s test for publication bias was significant (t = -2.50, p < 0.05), the trim-and-fill method was performed. After eliminating publication bias, there was a potential moderate and negative relationship between PA and negative responses (Fisher’s z = − 0.198, 95% CI [− 0.25, − 0.15], p < 0.001). Specifically, PA showed significant and negative associations with anxiety (Fisher’s z = − 0.180, 95% CI [− 0.27, − 0.09]; p < 0.001), depression (Fisher’s z = − 0.160, 95% CI [− 0.23, − 0.09], p < 0.001), and stress (Fisher’s z = − 0.170, 95% CI [− 0.24, − 0.10], p < 0.001) (see Fig. 2).
Furthermore, the meta-regression analyses results showed that age (p = 0.001), report of total (p = 0.001) and specific dimensions (duration and intensity) of PA (p = 0.001), and study quality (p = 0.001) were the primary origins of heterogeneity in the included studies for the relationship between PA and negative responses (see Table 4).
The relationship between physical activity and positive psychological responses
As illustrated in Fig. 3, PA was weakly and positively correlated with positive responses (Fisher’s z = 0.170, 95% CI [0.08, 0.25], p < 0.001, I2 = 92.42%; see Fig. 3). No significant publication bias was detected (p = 0.465 ). Meta-regression results showed that age (p = 0.002), report of total PA (p = 0.028), and study quality (p = 0.008) were the primary origins of heterogeneity in the included studies for the relationship between PA and positive responses (see Table 4).
Discussion
This systematic review and meta-analysis examined the relationship between PA and MH among children and youth during the COVID-19 pandemic. The impacts of age group and other factors on this relationship are further discussed.
An overview of physical activity and mental health among children and youth during COVID-19
During COVID-19, children and youth worldwide demonstrated a decreased level in PA participation that was significantly larger than before COVID-19 (36–61% of US children and youth showed declining PA levels, 50% in Ireland, 39% in Poland, 39% in Finland, 38% in The Czech Republic, and 33% in China) [39, 68, 84, 92, 109, 122,123,124,125,126]. Additional studies showed that only 3.6% of children (5–11 years) and 2.6% of youth (12–17 years) in Canada participated in at least 60 min of moderate to vigorous PA per day, with 49–64% of children and youth spending less PA time [80, 83, 94, 114, 127]. Another study showed that 18.9% fewer youth in Hungary engaged in moderate-intensity PA [78]. People with disabilities were also at risk for low levels of PA due to a lack of opportunities, physical education, and interventions [128]. We found studies in some countries that reported the same or even increased levels of PA among children and youth during COVID-19 compared to pre COVID-19 [102, 129,130,131]. However, in view of the prevalence of physical inactivity among children and youth before COVID-19 [132], PA deterioration during the pandemic and its potential health consequences deserve more attention [13].
Although COVID-19 has a significant negative impact on MH among children and youth globally, the extent of this impact varies slightly by region. For example, evidence has shown that 74% of American parents reported that their child’s MH deteriorated during the COVID-19 restriction period, and that the MH-related emergency department visiting rate of American children and youth increased by 7% [68, 133]. Similarly, it has been reported that youth with poor MH in China increased by 12% [89, 109], while in Canada, 31–44% of children felt their overall MH had declined [80, 83]. This MH deterioration among children and youth may have resulted from alienation due to physical isolation, exposure to negative news, fear that they or their loved ones would be infected by the virus, and even fear of death [30, 124].
The relationship between physical activity and negative psychological responses
The present systematic review found that depression, anxiety, stress, insomnia, fatigue, and mental health problems were the most common negative response variables investigated during COVID-19, and all of them were significantly and negatively correlated with PA. Specifically, increases in depression and anxiety were closely related to the lack of PA, which is consistent with findings before COVID-19 [16, 17, 33]. Our meta-analysis results showed a weak and negative relationship between PA and negative psychological responses during COVID-19 (Fisher’s z = − 0.198), a finding in line with a meta-analysis published in 2019 that reported the beneficial effects of PA on negative psychological responses among children and youth [16]. Before COVID-19, the lack of PA among children and youth might have been compensated to some extent by daily commuting and school activities [33, 134]. However, COVID-19-related lockdowns and school closures resulted in at-home/indoor physical inactivity, fear, and loneliness among children and youth that ultimately amplified the impact of PA on MH [28], which in turn may have led to a further loss of interest in PA [33, 135, 136].
Additionally, our results of variable categorization showed that the correlations of PA with anxiety, stress, and insomnia among children and youth during COVID-19 was mixed in the 19–24-year-old group rather than other age groups. One reason for this may be due to that the 19–24-year-olds may have better emotional self-management ability (e.g., managing stress) with a relatively matured cognitive control system being developed in this older group than minors [137, 138]. Another possible reason is that the influencing factors on MH in the 19–24-year-old group could be more complex than that in other age ranges, thus the impact of PA on the above negative psychological responses might be diminished [139]. These findings indicate that COVID-19 not only deepened the link between PA and negative psychological responses, but also led to diverse negative response symptoms among children and youth.
COVID-19 engendered a plethora of uncommon negative psychological responses, including COVID-19 stress, fatigue, mental health problems, and negative affect [58, 61, 68, 76, 90, 105]. COVID-19 stress, as a new negative psychological response that emerged during the pandemic [65], may have been for most youth an adaptive response that prompted them to take precautions (e.g., frequent hand washing and social distancing) to protect themselves from the virus. However, some youth almost certainly experienced excessive COVID-19 stress [65], which, if not taken seriously, may have developed into post-traumatic stress when the outbreak subsided [140]. This problem, unlike depression and anxiety, can be easily overlooked and cause serious consequences to children and youth [61, 76, 89, 105, 141]. Thus, future research should pay more attention to the causes of negative psychological responses and explore further how to prevent and treat them.
Another finding from our review is that, during COVID-19, PA was significantly and negatively associated with depression, regardless of age group. We argue that school closures and physical alienation increased loneliness and decreased PA for all children and youth, which resulted in the further prevalence of depression and indirectly strengthened the connection between PA and MH [61, 112]. In addition, we found that the relationships between PA and anxiety, stress, and insomnia varied across age ranges but were strongest among 13–18-year-olds. One possible explanation is that this age group followed news about COVID-19 via social media more frequently than the other groups, which may have negatively impacted their MH [136]. Furthermore, students between 13 and 18 years of age are generally under considerable academic pressure, which may contribute further to anxiety, stress, and insomnia [61, 89, 95, 109, 142]. We also found that 13–18-year-olds presented the greatest variety of negative psychological responses during the COVID-19 pandemic. One possible reason for this was the disruption of routine due to the long-term absence of a structured school framework, which is a more important adaptation mechanism for this age group than for others [143]. The above results suggest that 13–18-year-olds were most at risk for MH problems during COVID-19. Thus, researchers need to continuously monitor members of this group since the negative psychological responses triggered by COVID-19 (e.g., COVID-19 stress and COVID-19 fear) may become long-term post-traumatic stress responses persistently affecting their MH in the post-pandemic period [144].
After experiencing COVID-19, children and youth should be informed about the prevalence of negative psychological responses during adversity, how to minimize their impact, and how to quickly achieve “closure” and move on from them [40]. Thus, instead of focusing primarily on negative psychological responses, children and youth should learn to view the loss and pain of a difficult situation with detached values.
The relationship between physical activity and positive psychological responses
Our results demonstrated a weak and positive correlation between PA and positive psychological responses during COVID-19 (Fisher’s z = 0.17). Results of variable categorization also showed that PA was positively correlated with positive psychological responses. Specifically, PA was significantly and positively correlated with general well-being and vigor. For youth, sufficient PA can relieve psychological stress, increase mental stability, and further enhance general well-being and vigor [56]. For children, general well-being is more likely to be influenced by factors other than PA, including family cohesion, social connections with peers, and parents’ emotional states [143]. Given that fewer studies have addressed positive, compared to negative, psychological responses during COVID-19, it seems that the important relationship between PA and positive psychological responses has been to some extent overlooked. The few studies that examined this issue have demonstrated that positive psychological responses are not only closely related to PA, but also help to alleviate negative emotions [101, 145]. Thus, future research should investigate further the relationships between PA and positive psychological responses among children and youth.
The relationship between physical activity and mental health among children and youth with disabilities or chronic conditions (DCC)
In this review, eight negative and four positive psychological response outcomes were investigated for children and youth with DCC. Of the 12 outcomes, a significant relationship between PA and MH was evident in only two negative psychological responses (i.e., anxiety and depression). The rest lacked sufficient evidence to determine a relationship with PA. Research has suggested that, due to their failure during COVID-19 to receive adequate health screenings and usual interventions, children and youth with DCC experienced more negative MH effects than their peers without DCC [56, 146]. Moreover, individuals with DCC appear to have more barriers that impede their accrual of sufficient PA, which might cause deterioration of their MH status [57, 76, 88, 147]. Although previous studies have indicated that the pandemic’s negative impacts on PA and MH were more acute for children and youth with DCC than those without [88, 108], the exact relationship between PA and MH among children and youth with DCC cannot be determined due to the limited number of studies focusing on this population group in our systematic review. Therefore, in the post COVID-19 era, researchers should focus more on PA and MH issues of children and youth with DCC.
Limitations and recommendations for future research
Because most of the studies included in this review focused on typically developing children and youth, a meta-analysis on the relationship between PA and MH among children and youth with DCC could not be performed. Therefore, more studies on individuals with DCC should be conducted when investigating the relationship between PA and MH among children and youth. Furthermore, this review shows that studies did not include details of PA could have an impact on the relationship between PA and MH. Future studies should report PA details, such as total amount, intensity, frequency, and duration, as much as possible to avoid a one-dimensional assessment of PA.
We only included studies published up until December 2021, it was thus impossible to include research that have been conducted in the first two years of the outbreak but not yet published by the end of 2021. It is worth noting that this review included few studies with high methodological quality, which may impact the robustness of our findings. Furthermore, as only a limited number of experimental studies were eligible for this review, our meta-analyses on the magnitude of the relationship between PA and MH outcomes were based primarily on findings reported in observational studies. Thus, a cause-effect relationship between PA and MH could not be determined. Future research investigating the relationship between PA and MH among children and youth should include more studies with an experimental design and high methodological quality.
Finally, our review found that age impacted the relationship between MH and PA during COVID-19. Specifically, the most common MH problems are not the same at different ages. Future research should focus on age-specific MH problems (e.g., anxiety, stress, insomnia, and fatigue) and not limit their studies to the most common negative psychological responses, such as depression. It is important to note that limited research was conducted on preschoolers during COVID-19, which should also be addressed in future studies. Additionally, most of the existing studies were conducted in China, The United States, and Canada. In view of the potential influence of social cultural environment on the relationship between PA and MH in children and youth, future research from more countries worldwide is warranted.
Conclusion
The present systematic review and meta-analysis confirms a close relationship between PA and MH among children and youth in terms of both negative and positive psychological responses during the COVID-19 pandemic. Negative psychological responses received disproportionately more attention than positive ones. Specifically, PA’s associations with anxiety, depression, stress, insomnia, fatigue, mental health problems, general well-being, and vigor appeared to be stronger than its associations with other MH outcomes among children and youth. In addition, the pattern and strength of relations between PA and MH outcomes varied across age ranges and health conditions, with preschoolers and those with DCC receiving less attention in the existing research. Given the importance of PA and MH for healthy development of children and youth, future research with high methodological quality should focus on (1) age-range specific relationships between PA and MH outcomes from a comprehensive perspective during the post COVID-19 era, and (2) children and youth with DCC.
Availability of data and materials
All data are included in the manuscript and additional file.
Notes
References marked with an asterisk indicate studies included in the systematic review and meta-analysis.
Abbreviations
- COVID‐19:
-
The coronavirus disease
- PA:
-
Physical activity
- MH:
-
Mental health
- RCTs:
-
Randomized controlled trials
- WHO:
-
World health organization
- DCC:
-
Disabilities or chronic conditions
References
References marked with an asterisk indicate studies included in the systematic review and meta-analysis.
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–8.
Ryff CD, Love GD, Urry HL, Muller D, Rosenkranz MA, Friedman EM, et al. Psychological well-being and ill-being: do they have distinct or mirrored biological correlates? Psychother Psychosom. 2006;75(2):85–95.
Peng S, Luo X, Liang S, Deng F, Liu Y, Zeng H, et al. Psychological and emotional responses during different stages of the COVID-19 pandemic based on a survey of a mental health hotline. Int J Ment Health Promot. 2022;24(5):711–24.
Chew QH, Wei KC, Vasoo S, Chua HC, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Med J. 2020;61(7):350–6.
Kharel M, Sakamoto JL, Carandang RR, Ulambayar S, Shibanuma A, Yarotskaya E, et al. Impact of COVID-19 pandemic lockdown on movement behaviours of children and adolescents: a systematic review. BMJ Glob Health. 2022;7(1):e007190.
Lawrance EL, Jennings N, Kioupi V, Thompson R, Diffey J, Vercammen A. Psychological responses, mental health, and sense of agency for the dual challenges of climate change and the COVID-19 pandemic in young people in the UK: an online survey study. Lancet Planetary Health. 2022;6(9):E726–38.
Wang QF, Feng HL, Wang MY, Xie Y, Hou BT, Lu XZ, et al. Mental health and psychological responses during the coronavirus disease 2019 epidemic: a comparison between Wuhan and other areas in China. Psychosom Med. 2021;83(4):322–7.
Huppert FA, Whittington JE. Evidence for the independence of positive and negative well-being: implications for quality of life assessment. Br J Health Psychol. 2003;8(1):107–22.
Campbell F, Blank L, Cantrell A, Baxter S, Blackmore C, Dixon J, et al. Factors that influence mental health of university and college students in the UK: a systematic review. BMC Public Health. 2022;22(1):1778.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56.
Marconcin P, Werneck AO, Peralta M, Ihle A, Gouveia ER, Ferrari G, et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. 2022;22(1):209.
World Health Organization. Benefits and risks of physical activity and sedentary behavior. 2022. https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed 5 October 2022.
Aubert S, Barnes JD, Demchenko I, Hawthorne M, Abdeta C, Abi Nader P, et al. Global matrix 4.0 physical activity report card grades for children and adolescents: results and analyses from 57 countries. J Phys Activity Health. 2022;19(11):700–28.
Alley SJ, Duncan MJ, Schoeppe S, Rebar AL, Vandelanotte C. 8-year trends in physical activity, nutrition, TV viewing time, smoking, alcohol and BMI: a comparison of younger and older queensland adults. PLoS ONE. 2017;12(3):e0172510.
Knai C, Petticrew M, Scott C, Durand MA, Eastmure E, James L, et al. Getting England to be more physically active: are the public health responsibility deal’s physical activity pledges the answer? Int J Behav Nutr Phys Act. 2015;12:107.
Rodriguez-Ayllon M, Cadenas-Sanchez C, Estevez-Lopez F, Munoz NE, Mora-Gonzalez J, Migueles JH, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383–410.
Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang JL, Podinic I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):72.
Andermo S, Hallgren M, Nguyen TTD, Jonsson S, Petersen S, Friberg M, et al. School-related physical activity interventions and mental health among children: a systematic review and meta-analysis. Sports Med Open. 2020;6(1):25.
Ahn S, Fedewa AL. A meta-analysis of the relationship between children’s physical activity and mental health. J Pediatr Psychol. 2011;36(4):385–97.
Antaramian SP, Huebner ES, Hills KJ, Valois RF. A dual-factor model of mental health: toward a more comprehensive understanding of youth functioning. Am J Orthopsychiatry. 2010;80(4):462–72.
Seligman MEP, Csikszentmihalyi M. Positive psychology-an introduction. Am Psychol. 2000;55(1):5–14.
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–7.
Chtourou H, Trabelsi K, H’mida C, Boukhris O, Glenn JM, Brach M, et al. Staying physically active during the quarantine and self-isolation period for controlling and mitigating the COVID-19 pandemic: a systematic overview of the literature. Front Psychol. 2020;11:1708.
Ropero-Padilla C, Rodriguez-Arrastia M, Martinez-Ortigosa A, Salas-Medina P, Ayora AF, Roman P. A gameful blended-learning experience in nursing: a qualitative focus group study. Nurse Educ Today. 2021;106:105109.
Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGIproject. Pediatr Obes. 2021;16(4):e12731.
Bates LC, Zieff G, Stanford K, Moore JB, Kerr ZY, Hanson ED, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children-Basel. 2020;7(9):138.
Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I. Covid-19 pandemia and public and global mental health from the perspective of global health security. Psychiatr Danub. 2020;32(1):6–14.
Samji H, We J, Ladak A, Vossen C, Stewart E, Dove N, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth-a systematic review. Child Adolesc Mental Health. 2022;27(2):173–89.
Violant-Holz V, Gallego-Jimenez MG, Gonzalez-Gonzalez CS, Munoz-Violant S, Rodriguez MJ, Sansano-Nadal O, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17(24):9419.
Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429.
Okuyama J, Seto S, Fukuda Y, Funakoshi S, Amae S, Onobe J, et al. Mental health and physical activity among children and adolescents during the COVID-19 pandemic. Tohoku J Exp Med. 2021;253(3):203–15.
Theis N, Campbell N, De Leeuw J, Owen M, Schenke KC. The effects of COVID-19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disabil Health J. 2021;14(3):101064.
Wolf S, Seiffer B, Zeibig JM, Welkerling J, Brokmeier L, Atrott B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? a rapid systematic review. Sports Med. 2021;51(8):1771–83.
Chang JJ, Ji Y, Li YH, Pan HF, Su PY. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. 2021;292:242–54.
Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;301:113863.
Wunsch K, Kienberger K, Niessner C. Changes in physical activity patterns due to the COVID-19 pandemic: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19(4):2250.
Diaz A, Baweja R, Bonatakis JK, Baweja R. Global health disparities in vulnerable populations of psychiatric patients during the COVID-19 pandemic. World J Psychiatry. 2021;11(4):94–108.
Waters L, Algoe SB, Dutton J, Emmons R, Fredrickson BL, Heaphy E, et al. Positive psychology in a pandemic: buffering, bolstering, and building mental health. J Posit Psychol. 2022;17(3):303–23.
Ng K, Cooper J, McHale F, Clifford J, Woods C. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport Exerc Med. 2020;6(1):e000919.
Walsh F. Loss and resilience in the time of COVID-19: meaning making, hope, and transcendence. Fam Process. 2020;59(3):898–911.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ British Med J. 2015;350:g7647.
Jiao J, Shi LY, Zhang YY, Chen HQ, Wang XH, Yang MF, et al. Core policies disparity response to COVID-19 among BRICS countries. Int J Equity Health. 2022;21(1):9.
Karako K. Relaxation of all-case reporting of COVID-19 cases in Japan. Drug Discov Ther. 2022;16(6):316–7.
Soljak M, Majeed A. Reducing the covid-19 isolation period in England: a policy change that needs careful evaluation. BMJ Brit Med J. 2022;376:o184.
Yang JY, Shi LY, Chen HQ, Wang XH, Jiao J, Yang MF, et al. Strategies comparison in response to the two waves of COVID-19 in the United States and India. Int J Equity Health. 2022;21(1):57.
Yu JJ, Burnett AF, Sit CH. Motor skill interventions in children with developmental coordination disorder: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(10):2076–99.
Modesti PA, Reboldi G, Cappuccio FP, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE. 2016;11(1):e0147601.
Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–75.
Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–40.
Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, El Bcheraoui C, Moradi-Lakeh M, et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2016;387(10036):2383–401.
Welz T, Doebler P, Pauly M. Fisher transformation based confidence intervals of correlations in fixed- and random-effects meta-analysis. Br J Math Stat Psychol. 2022;75(1):1–22.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Valiengo L, Maia A, Cotovio G, Gordon PC, Brunoni AR, Forlenza OV, et al. Repetitive transcranial magnetic stimulation for major depressive disorder in older adults: systematic review and meta-analysis. J Gerontol Ser A Biol Sci Med Sci. 2022;77(4):851–60.
Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98.
Waldron M, Fowler R, Heffernan S, Tallent J, Kilduff L, Jeffries O. Effects of heat acclimation and acclimatisation on maximal aerobic capacity compared to exercise alone in both thermoneutral and hot environments: a meta-analysis and meta-regression. Sports Med. 2021;51(7):1509–25.
*Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. BMI status and associations between affect, physical activity and anxiety among US children during COVID-19. Pediatr Obes. 2021;16(9):e12786.
*Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. Prenatal exposure to gestational diabetes is associated with anxiety and physical inactivity in children during COVID-19. Clin Obesity. 2021;11(1):e12422.
*Awais MA, Chaudhery MM, Khan MS, Butt AUA, Malik AR, Khan MN, et al. Factors contributing to distress among school and college-going adolescents during COVID-19 lockdown: a cross-sectional study conducted in Sibi Balochistan, Pakistan. J Educ Health Promot. 2021;10(1):317.
*Bosselmann V, Amatriain-Fernandez S, Gronwald T, Murillo-Rodriguez E, Machado S, Budde H. Physical activity, boredom and fear of COVID-19 among adolescents in Germany. Front Psychol. 2021;12:624206.
*Breidokiene R, Jusiene R, Urbonas V, Praninskiene R, Girdzijauskiene S. Sedentary behavior among 6–14-year-old children during the COVID-19 lockdown and its relation to physical and mental health. Healthcare. 2021;9(6):756.
*Chi XL, Liang KX, Chen ST, Huang QM, Huang LY, Yu Q, et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. 2021;21(3):100128.
*Constantini K, Markus I, Epel N, Jakobovich R, Gepner Y, Lev-Ari S. Continued participation of israeli adolescents in online sports programs during the COVID-19 pandemic is associated with higher resilience. Int J Environ Res Public Health. 2021;18(8):4386.
*Cosma A, Pavelka J, Badura P. Leisure time use and adolescent mental well-being: insights from the COVID-19 Czech spring lockdown. Int J Environ Res Public Health. 2021;18(23):12812.
*Deng CH, Wang JQ, Zhu LM, Liu HW, Guo Y, Peng XH, et al. Association of web-based physical education with mental health of college students in wuhan during the COVID-19 outbreak: cross-sectional survey study. J Med Internet Res. 2020;22(10):e21301.
*Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci Revue Canadienne des Sciences du Comportement. 2020;52(3):177–87.
*Fang JDD, Teng PC, Wang FJ. The impact of physical education classes on health and quality of life during the COVID-19. Appl Sci. 2021;11(19):8813.
*Ghorbani S, Afshari M, Eckelt M, Dana A, Bund A. Associations between physical activity and mental health in Iranian adolescents during the COVID-19 pandemic: an accelerometer-based study. Children. 2021;8(11):1022.
*Gilbert AS, Schmidt L, Beck A, Kepper MM, Mazzucca S, Eyler A. Associations of physical activity and sedentary behaviors with child mental well-being during the COVID-19 pandemic. BMC Public Health. 2021;21(1):1770.
*Huang Y, Huang JY, Wang TT, Xu SY, Li JL. The impact of the corona virus disease 2019 pandemic on Chinese middle school students’ self-perceived emotional states: a Wuhan perspective. Front Psychol. 2021;12:740879.
*Kang SF, Sun YL, Zhang XX, Sun FJ, Wang BQ, Zhu WF. Is physical activity associated with mental health among Chinese adolescents during isolation in COVID-19 pandemic? J Epidemiol Global Health. 2021;11(1):26–33.
*Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. 2020;277:121–8.
*Lai AYK, Lee L, Wang MP, Feng YB, Lai TTK, Ho LM, et al. Mental health impacts of the COVID-19 pandemic on international university students, related stressors, and coping strategies. Front Psych. 2020;11:584240.
*Lee DJ. Relationships among the degree of participation in physical activity, self-concept clarity, and COVID-19 stress in adolescents. Healthcare. 2021;9(4):482.
*Lee SM, So WY, Youn HS. Importance-performance analysis of health perception among Korean adolescents during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(3):1280.
*Li W, Wang Z, Wang G, Ip P, Sun X, Jiang Y, et al. Socioeconomic inequality in child mental health during the COVID-19 pandemic: first evidence from China. J Affect Disord. 2021;287:8–14.
*Lindoso L, Astley C, Queiroz LB, Gualano B, Pereira RMR, Tannuri U, et al. Physical and mental health impacts during COVID-19 quarantine in adolescents with preexisting chronic immunocompromised conditions. Jornal de Pediatria. 2021;98(4):350–61.
*Lu CP, Chi XL, Liang KX, Chen ST, Huang LY, Guo TY, et al. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol Res Behav Manag. 2020;13:1223–33.
*Lukacs A. The impact of physical activity on psychological well-being and perceived health status during coronavirus pandemic in university students. J King Saud University Sci. 2021;33(6):101531.
*Masse LC, Edache IY, Pitblado M, Hutchison SM. The impact of financial and psychological wellbeing on children’s physical activity and screen-based activities during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(16):8694.
*Maximova K, Khan MKA, Dabravolskaj J, Maunula L, Ohinmaa A, Veugelers PJ. Perceived changes in lifestyle behaviours and in mental health and wellbeing of elementary school children during the first COVID-19 lockdown in Canada. Public Health. 2022;202:35–42.
*McArthur BA, Racine N, McDonald S, Tough S, Madigan S. Child and family factors associated with child mental health and well-being during COVID-19. Eur Child Adolesc Psychiatry. 2021;24:1–11.
*McGuine TA, Biese K, Hetzel SJ, Schwarz A, Kliethermes S, Reardon CL, et al. High school sports during the COVID-19 pandemic: the impact of sport participation on the health of adolescents. J Athl Train. 2021;57(1):51–8.
*Mitra R, Waygood EOD, Fullan J. Subjective well-being of Canadian children and youth during the COVID-19 pandemic: the role of the social and physical environment and healthy movement behaviours. Prev Med Rep. 2021;23:101404.
*Moriarty T, Bourbeau K, Fontana F, McNamara S, da Silva MP. The relationship between psychological stress and healthy lifestyle behaviors during COVID-19 among students in a US midwest university. Int J Environ Res Public Health. 2021;18(9):4752.
*Morres ID, Galanis E, Hatzigeorgiadis A, Androutsos O, Theodorakis Y. Physical activity, sedentariness, eating behaviour and well-being during a COVID-19 lockdown period in Greek adolescents. Nutrients. 2021;13(5):1449.
*Oliva S, Russo G, Gili R, Russo L, Di Mauro A, Spagnoli A, et al. Risks and protective factors associated with mental health symptoms during COVID-19 home confinement in Italian children and adolescents: the #understandingkids study. Front Pediatr. 2021;9:664702.
*Pigaiani Y, Zoccante L, Zocca A, Arzenton A, Menegolli M, Fadel S, et al. Adolescent lifestyle behaviors, coping strategies and subjective wellbeing during the COVID-19 pandemic: an online student survey. Healthcare. 2020;8(4):472.
*Qi H, Liu R, Feng Y, Luo J, Lei SM, Cheung T, et al. Prevalence of depression and its associated factors among adolescents in China during the early stage of the COVID-19 outbreak. PeerJ. 2021;9:e12223.
*Qin J, Ding YY, Gao J, Wu Y, Lv H, Wu J. Effects of COVID-19 on mental health and anxiety of adolescents aged 13–16 years: a comparative analysis of longitudinal data from China. Front Psych. 2021;12:695556.
*Qin ZG, Shi L, Xue YQ, Lin H, Zhang JC, Liang PY, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. 2021;4(1):e2035487.
*Ren HG, He X, Bian XH, Shang XH, Liu JS. The protective roles of exercise and maintenance of daily living routines for chinese adolescents during the COVID-19 quarantine period. J Adolesc Health. 2021;68(1):35–42.
*Sikorska IM, Lipp N, Wrobel P, Wyra M. Adolescent mental health and activities in the period of social isolation caused by the COVID-19 pandemic. Adv Psychiatry Neurol. 2021;30(2):79–95.
*Song HH, Lee DJ. Structural relationship between Korean adolescent’s sports participation, optimism, pessimism, self-regulation, and coronavirus-related stress in the pandemic situation. Int J Environ Res Public Health. 2021;18(20):10645.
*Swansburg R, Hai T, MacMaster FP, Lemay JF. Impact of COVID-19 on lifestyle habits and mental health symptoms in children with attention-deficit/hyperactivity disorder in Canada. Paediatr Child Health. 2021;26(5):E199-207.
*Szwarcwald CL, Malta DC, Barros MBD, de Souza PRB, Romero D, de Almeida WD, et al. Associations of sociodemographic factors and health behaviors with the emotional well-being of adolescents during the COVID-19 pandemic in Brazil. Int J Environ Res Public Health. 2021;18(11):6160.
*Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children’s physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Netw Open. 2021;4(10):e2127892.
*Thomas J, Bowes N, Meyers R, Thirlaway K. Mental well-being and physical activity of young people experiencing homelessness before and during COVID-19 lockdown: a longitudinal study. Ment Health Phys Act. 2021;21:100407.
*Wang JY, Wang YY, Lin HJ, Chen XX, Wang H, Liang HB, et al. Mental health problems among school-aged children after school reopening: a cross-sectional study during the COVID-19 post-pandemic in east China. Front Psychol. 2021;12:773134.
*Wang L, Chen L, Jia F, Shi X, Zhang Y, Li F, et al. Risk factors and prediction nomogram model for psychosocial and behavioural problems among children and adolescents during the COVID-19 pandemic: a national multicentre study risk factors of childhood psychosocial problems. J Affect Disord. 2021;294:128–36.
*Wang MT, Scanlon CL, Hua M, Belmont AM, Zhang AL, Del Toro J. Social distancing and adolescent psychological well-being: the role of practical knowledge and exercise. Acad Pediatr. 2022;22(3):402–12.
*Wright LJ, Williams SE, van Zanten JJCSV. Physical activity protects against the negative impact of coronavirus fear on adolescent mental health and well-being during the COVID-19 pandemic. Front Psychol. 2021;12:580511.
*Wunsch K, Nigg C, Niessner C, Schmidt SCE, Oriwol D, Hanssen-Doose A, et al. The impact of COVID-19 on the interrelation of physical activity, screen time and health-related quality of life in children and adolescents in Germany: results of the motorik-modul study. Children-Basel. 2021;8(2):520.
*Xu YY, Su SZ, Jiang ZD, Guo SH, Lu QD, Liu L, et al. Prevalence and risk factors of mental health symptoms and suicidal behavior among university students in Wuhan, China during the COVID-19 pandemic. Front Psych. 2021;12:695017.
*Zhang XD, Shi X, Wang Y, Jing HQ, Zhai QQ, Li KH, et al. Risk factors of psychological responses of Chinese university students during the COVID-19 outbreak: cross-sectional web-based survey study. J Med Internet Res. 2021;23(7):e29312.
*Zhang XX, Zhu WF, Kang SF, Qiu LK, Lu ZJ, Sun YL. Association between physical activity and mood states of children and adolescents in social isolation during the COVID-19 epidemic. Int J Environ Res Public Health. 2020;17(20):7666.
*Zhang Y, Wu X, Tao S, Li S, Ma L, Yu Y, et al. Associations between screen time, physical activity, and depressive symptoms during the 2019 coronavirus disease (COVID-19) outbreak among Chinese college students. Environ Health Prev Med. 2021;26(1):107.
*Zhang Y, Zhang HY, Ma XD, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int J Environ Res Public Health. 2020;17(10):3722.
*Zhou JJ, Yuan XF, Qi H, Liu R, Li YQ, Huang HH, et al. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Global Health. 2020;16(1):69.
*Zhu SM, Zhuang YQ, Ip P. Impacts on children and adolescents’ lifestyle, social support and their association with negative impacts of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(9):4780.
*Chen J, Sang GQ, Zhang Y, Jiang AF. Intervention effect of the integration model on negative emotions of adolescents during the outbreak of corona virus disease 2019. Psychiatr Danub. 2021;33(1):86–94.
*De Candia M, Carvutto R, Galasso L, Grimaldi M. The exercise dependence at the time of COVID-19 pandemic: The role of psychological stress among adolescents. J Human Sport Exerc. 2021;16:S1937–45.
*Hamed NS, Abdel-aziem AA, Muhsen BA, Eid MM, Allam HA, El-Gendy AM, et al. The effect of aerobic training versus cognitive behavioral therapy in management of anxiety, depression and stress related to COVID 19 pandemic among university students: a randomized controlled trial. Med Sci. 2021;25(115):2233–46.
*Zheng YF, Wang W, Zhong YX, Wu FC, Zhu ZT, Tham YC, et al. A peer-to-peer live-streaming intervention for children during COVID-19 homeschooling to promote physical activity and reduce anxiety and eye strain: cluster randomized controlled trial. J Med Internet Res. 2021;23(4):e24316.
Gonzalez-Valero G, Zurita-Ortega F, Lindell-Postigo D, Conde-Pipo J, Grosz WR, Badicu G. Analysis of self-concept in adolescents before and during COVID-19 lockdown: differences by gender and sports activity. Sustainability. 2020;12(18):7792.
Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):85.
Bronikowska M, Krzysztoszek J, Lopatka M, Ludwiczak M, Pluta B. Comparison of physical activity levels in youths before and during a pandemic lockdown. Int J Environ Res Public Health. 2021;18(10):5139.
Pelletier CA, Cornish K, Sanders C. Children’s independent mobility and physical activity during the COVID-19 pandemic: a qualitative study with families. Int J Environ Res Public Health. 2021;18(9):4481.
Ruiz-Roso MB, Padilha PD, Matilla-Escalante DC, Brun P, Ulloa N, Acevedo-Correa D, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during COVID-19 pandemic: an observational study. Nutrients. 2020;12(8):2289.
Qiu JY, Shen B, Zhao M, Wang Z, Xie B, Xu YF. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33(2):e100213.
Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91(3):841–52.
Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–6.
Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1):e000960.
Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351.
Ng K, Cosma A, Svacina K, Boniel-Nissim M, Badura P. Czech adolescents’ remote school and health experiences during the spring 2020 COVID-19 lockdown. Prev Med Rep. 2021;22:101386.
Ng K, Koski P, Lyyra N, Palomaki S, Mononen K, Blomqvist M, et al. Finnish late adolescents’ physical activity during COVID-19 spring 2020 lockdown. BMC Public Health. 2021;21(1):2197.
Xiang M, Zhang ZR, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63(4):531–2.
Loewen OK, Maximova K, Ekwaru JP, Faught EL, Asbridge M, Ohinmaa A, et al. Lifestyle behavior and mental health in early adolescence. Pediatrics. 2019;143(5):e20183307.
Ng K. Adapted physical activity through COVID-19. Eur J Adapt Phys Activ. 2020;13(1):1–3.
Nigg C, Oriwol D, Wunsch K, Burchartz A, Kolb S, Worth A, et al. Population density predicts youth’s physical activity changes during Covid-19-results from the MoMo study. Health Place. 2021;70:102619.
Nystrom CD, Alexandrou C, Henstrom M, Nilsson E, Okely AD, El Masri SW, et al. International study of movement behaviors in the early years (SUNRISE): results from SUNRISE Sweden’s pilot and COVID-19 study. Int J Environ Res Public Health. 2020;17(22):8491.
Schmidt SCE, Anedda B, Burchartz A, Eichsteller A, Kolb S, Nigg C, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2021;11(1):21780.
Rhodes RE, Spence JC, Berry T, Faulkner G, Latimer-Cheung AE, O’Reilly N, et al. Parental support of the Canadian 24-hour movement guidelines for children and youth: prevalence and correlates. BMC Public Health. 2019;19(1):1–12.
Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic-United States, january 1-october 17, 2020. Morb Mortal Wkly Rep. 2020;69(45):1675–80.
Stone JE, Phillips AJK, Chachos E, Hand AJ, Lu S, Carskadon MA, et al. In-person vs home schooling during the COVID-19 pandemic: differences in sleep, circadian timing, and mood in early adolescence. J Pineal Res. 2021;71(2):e12757.
Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol. 2020;25(9):1155–63.
Marciano L, Ostroumova M, Schulz PJ, Camerini AL. Digital media use and adolescents’ mental health during the COVID-19 pandemic: a systematic review and meta-analysis. Front Public Health. 2022;9:793868.
Kross E, Ayduk O. Self-distancing: theory, research, and current directions. Adv Exp Soc Psychol. 2017;55:81–136.
Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J Pers Soc Psychol. 2001;80(1):136–51.
Wang D, Chen H, Zhai S, et al. Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J Affect Disord. 2021;287:261–7.
Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7(1):105–10.
Xu WX, Shen W, Wang S. Intervention of adolescent? mental health during the outbreak of COVID-19 using aerobic exercise combined with acceptance and commitment therapy. Child Youth Serv Rev. 2021;124:105960.
Ma ZR, Ma WH, Idris S, Pan QW, Baloch Z. COVID-19 impact on high school student’s education and mental health: a cohort survey in China. World J Psychiatry. 2021;11(6):232–41.
Stassart C, Wagener A, Etienne AM. Parents’ perceived impact of the societal lockdown of COVID-19 on family well-being and on the emotional and behavioral state of walloon belgian children aged 4 to 13 years: an exploratory study. Psychologica Belgica. 2021;61(1):186–99.
Zhu Y, Zhang LH, Zhou X, Li CX, Yang D. The impact of social distancing during COVID-19: a conditional process model of negative emotions, alienation, affective disorders, and post-traumatic stress disorder. J Affect Disord. 2021;289:131–7.
Santxo NB, Mondragon NI, Ozamiz-Etxebarria N, Dosil-Santamaria M. Well-being of adolescents in de-escalation situation: physical, emotional, social, and academic impact. Front Psychol. 2021;12:646027.
Pettinicchio D, Maroto M, Chai L, Lukk M. Findings from an online survey on the mental health effects of COVID-19 on Canadians with disabilities and chronic health conditions. Disabil Health J. 2021;14(3):101085.
Lopez-Sanchez GF, Lopez-Bueno R, Gil-Salmeron A, Zauder R, Skalska M, Jastrzebska J, et al. Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur J Pub Health. 2021;31(1):161–6.
Acknowledgements
Not applicable.
Funding
This work is funded by The National Social Science Fund of China (22BTY098) and Zhejiang Provincial Philosophy and Social Science Planning Project (22NDJC043YB). The funding agency had no role in the design, analyses, interpretation, writing, or publication of this study.
Author information
Authors and Affiliations
Contributions
BL and JJY conceptualized this work and wrote the original draft of manuscript; BL conducted literature searches, evidence synthesis, and data analysis; BL and JY performed records screening, data extraction, and risk of bias assessment; KN, XT, and XZ interpreted data and critically edited the manuscript; JJY designed the methodology, supervised the entire process of review, interpreted data, and obtained funding. All authors have contributed to, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they had no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Details of search strategy
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, B., Ng, K., Tong, X. et al. Physical activity and mental health in children and youth during COVID-19: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health 17, 92 (2023). https://doi.org/10.1186/s13034-023-00629-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13034-023-00629-4