Abstract
Inborn metabolic diseases (IMD) are rare conditions that can be diagnosed during adulthood. Patients with IMD may have joint symptoms and the challenge is to establish an early diagnosis in order to institute appropriate treatment and prevent irreversible damage. This review describes the joint manifestations of IMD that may be encountered in adults. The clinical settings considered were arthralgia and joint stiffness as well as arthritis. Unspecific arthralgias are often the first symptoms of hereditary hemochromatosis, chronic low back pain may reveal an intervertebral disc calcification in relation with alkaptonuria, and progressive joint stiffness may correspond to a mucopolysaccharidosis or mucolipidosis. Gaucher disease is initially revealed by painful acute attacks mimicking joint pain described as “bone crises”. Some IMD may induce microcrystalline arthropathy. Beyond classical gout, there are also gouts in connection with purine metabolism disorders known as “enzymopathic gouts”. Pyrophosphate arthropathy can also be part of the clinical spectrum of Gitelman syndrome or hypophosphatasia. Oxalate crystals arthritis can reveal a primary hyperoxaluria. Destructive arthritis may be indicative of Wilson’s disease. Non-destructive arthritis may be seen in mevalonate kinase deficiency and familial hypercholesterolemia.
Similar content being viewed by others
Background
Inborn metabolic diseases (IMD) are due, in most cases, to a genetic deficiency of enzymes or transporters, resulting in the disruption of a metabolic pathway leading to synthesis or degradation of organic compounds. These abnormalities may be responsible for the accumulation of toxic substances among blood and organs upstream of the deficiency or downstream of a production defect. IMD are usually inherited in an autosomal recessive mode but the pattern of inheritance may also be X-linked or dominant [1].
IMDs are rare diseases with a large clinical spectrum. They are mostly symptomatic during childhood, mostly in the neonate period or during the first year of life, but some may be diagnosed in adolescence and adulthood [2]. There are also milder forms of IMD which are only detected in adulthood as well as adult-specific forms. Because these diseases are rare and labeled as “pediatric”, physicians are relatively ignorant about their existence in adults and therefore their diagnosis is significantly delayed. In some exceptional cases, some patients are diagnosed with IMD in the elderly [3]. Therapy of many IMD is mainly based on a specific dietary management but recent advances enabled the development of specific therapies such as enzymatic stimulation using co-factors or enzyme replacement therapy and chelating treatments [4].
In adults, most IMD are diagnosed through neuropsychiatric symptoms but some may also be revealed by joint manifestations [5, 6]. Thus, joint manifestations, whether or not associated with other systemic features, can lead the clinician to the diagnosis of IMD. Early diagnosis of these diseases may, when treatable, help in preventing the occurrence of irreversible joint destruction and deformity and influence global outcome for the patients. IMD are unknown from the majority of “non metabolic physicians”, although rheumatologists frequently encounter non-specific clinical manifestations as arthralgia or arthritis that can result in an important diagnosis delay [7].
The present review is part of an approach by physicians to recognize these diseases in adults, by recalling the main IMD with joint damage and proposing a useful diagnostic approach to the clinician. To this end, a literature search in Medline including the terms of Medical Subjects Headings (MeSH) “arthralgia”, “arthritis”, “joints”, and “metabolism, inborn errors”, with age limit above 19 years, including only French and English texts, was carried out. Given the rarity of some diseases, clinical cases and case studies were kept in our literature review. This review was complemented by reading the main works about IMDs and by experience gained in the IMD reference center of our university hospital over 20 years.
Main text
Arthralgia and joint stiffness
Arthralgia or joint stiffness may reveal an IMD in adulthood. They are most often non-specific, with a very broad clinical spectrum of varying severity. Thus, any “unexplained” arthralgia or joint pain occurring at a young age should suggest the diagnosis of IMD. Therefore, etiological orientation requires the family history, age of onset of joint symptoms and their evolution, as well as extra-articular symptoms. A detailed and focused physical examination should be carried out. Some biological and radiological features will help strengthening the etiologic orientation (Table 1).
Fabry disease was not included into this review since pain is neuropathic in this condition and therefore not directly related to joint involvement. Nonetheless, Fabry disease can be a difficult diagnosis that rheumatologists should know [7].
Hereditary hemochromatosis
Hereditary Hemochromatosis (HH) are a group of disorders of iron metabolism. The most common form, HFE hemochromatosis (HH type 1), is caused by biallelic variants in the HFE gene which encodes the homeostatic iron regulator (HFE), a membrane protein that increases the hepcidin production. The loss of function of HFE causes a reduction in the concentration of hepcidin and, therefore, an increase of intestinal absorption and recycling of iron in macrophages, leading to iron overload/storage in the liver, pancreas, heart, joints and endocrine glands. Transmission is autosomal recessive with variable penetrance. Prevalence of HH is 1/200. The most frequent pathogenic variant is p.Cys282Tyr [8].
Iron overload is determined by the elevation of the coefficient of saturation of transferrin > 45%. The diagnosis of HFE1 hemochromatosis is confirmed by genetic analysis. Iron overload is then assessed by serum ferritin (N < 200 µg/L in women and 300 µg/L in men) and quantitative liver MRI. Treatment is based upon phlebotomy, with a target of serum ferritin < 50 ng/mL. Phlebotomy has little or no effect on articular symptoms but can prevent other organs affection. Thus, treatment of joint manifestations is based on analgesics and non-steroid anti-inflammatory drugs. From the index case, a family investigation must be performed [8, 9].
The first symptoms usually appear after 35 years, after several years of biological iron overload. Chronic fatigue, arthralgia and elevated liver enzymes are the first symptoms of iron overload [10]. In the complete form of HH, clinical symptoms are, in order of frequency : arthralgia, liver disease, skin pigmentation, osteoporosis, diabetes, cardiomyopathy, sexual dysfunction and hypogonadotropic hypogonadism [11].
Arthralgia may be mono, oligo or polyarticular, of varying severity, mechanical or inflammatory, bilateral, affecting any joints. A suggestive presentation can be joint damage affecting a joint usually non affected by primary osteoarthritis, without history of trauma. In order of frequency, the metacarpophalangeal joints, proximal interphalangeal joints, knees, back and neck, feet, hips, wrists, shoulders, distal interphalangeal joints and ankles are involved [12]. However, the most suggestive and almost pathognomonic presentation is the involvement of metacarpophalangeal joints of the second and third fingers, which is characterized initially by a simple painful limitation of flexion referred to as the sign of “the painful handshake” or “iron salute” [13]. A chronic swelling of the 2nd and 3rd metacarpophalangeal joints or a non-inflammatory irreversible deformation may then develop. Such type of arthritis is found to occur in 37.6% of the patients with HH and is associated with age, male gender, hyperferritinemia, diabetes and hepatic cirrhosis [14]. The other joint manifestation linked to HH is the occurrence of acute attacks of pyrophosphate arthropathy, formerly chondrocalcinosis, concerning 1 patient out of 3 [15]. Damage to the hips and knees is the most disabling, with a 2 to 3-fold increased prevalence of prosthetic replacements as compared to the general population [16].
X-rays show geodes encircled by condensation and positioned in the subchondral bone area, osteophytes with rounded edges or hook-like osteophytes, joint space narrowing as well as chondrocalcinosis of wrists, hips and knees joints [17].
The non-specific presentation often results in late diagnosis, although early diagnosis would help prevent organ damages due to the disease. Thus, the presence of arthralgia in a young person should readily lead the clinician to suspect HH and, in these cases, carry out an iron assessment.
Alkaptonuria-ochronosis
Alkaptonuria (AKU) was the first IMD to be described by Garrod in 1902. It is caused by biallelic pathogenic variations in the HDG gene which encodes the homogentisate 1,2-dioxygenase, an enzyme that acts downstream to the conversion of phenylalanine into tyrosine. In AKU, there is an increased serum and urinary levels of homogentisic acid. The accumulation of homogentisic acid, which has an “ochre-like” color in microscopy, is responsible for the formation of ochronotic bluish-black pigmented polymers which have a strong affinity for collagen that creates damage in all connective tissues. The transmission of AKU is autosomal recessive. Its prevalence is 1/1,000,000. Diagnosis is confirmed by high levels of homogentisic acid in the urine [18].
In AKU, there is a latency period before the onset of symptoms. This is known as the pre-ochronotic phase, with slow subclinical evolution followed by a rapidly progressive ochronotic phase [19]. On average symptoms develop at the age of 30–40 years. The initial symptomatology is dominated by chronic mechanical or inflammatory low back pain and spinal stiffness with radiological diffuse calcifications of the intervertebral discs [20, 21]. Secondly, within a period of about a decade, peripheral arthralgia appears. Large joints such as knees, hips or shoulders are preferentially affected. Episodes of joint effusion are possible. Other clinical aspects suggestive of AKU are dark-colored urine when alkalized or oxidized in air, bluish discoloration of the nose, ears and sclera. Ear examination can lead to the diagnosis when it discloses a contrast between a black tympanic membrane and discolored pale cerumen. Other possible affections are obstruction of the urinary tract, renal failure, aortic and mitral valve disease, conductive hearing loss and osteopenia [22, 23].
Synovial fluid is mechanical or inflammatory without microcrystals. Presence of homogentisic acid crystals have been reported. X-rays show joint destruction with narrowing joint space, osteophytosis, osteosclerosis,subchondral geodes and diffuse calcifications of the intervertebral discs [24, 25]. During surgery or arthroscopy, cartilage and synovial membranes are black in color [26].
AKU is treated with nitisinone, a competitive inhibitor of 4-hydroxyphenyl dioxygenase, enzyme of the tyrosine catabolism pathway, thereby preventing the accumulation of toxic intermediate products. An observational, long-term follow up study (SONIA-2) of patients treated with nitisinone at a dose of 10 mg daily has shown that nitisinone decreased ochronosis and improved clinical symptoms, indicating a slower disease progression [4]. Dietary protein restriction, low in phenylalanine and tyrosine, is effective in patients who are below 12 years old but the effectiveness of such diet has not been shown in older patients [27]. Joint replacement surgery has been described as successful in patients with alkaptonuria, although they may carry an higher risk of complication as compared to other patients [28].
Mucopolysaccharidoses (moderate forms)
Mucopolysaccharidoses (MPS) are lysosomal storage disorders in which the enzyme deficiency is responsible for intra-lysosomal accumulation of glycosaminoglycans (GAG) that causes systemic tissue dysfunction. This group of disorders presents a great heterogeneity in clinical presentation. Indeed, there are 12 types of MPS in which we will discuss 5 types that may initially occur through isolated joint symptoms in their moderate form. These are MPS 1 or Scheie syndrome, MPS 2 or Hunter syndrome, MPS 4a or Morquio A syndrome, MPS 6 or Maroteaux-Lamy syndrome and MPS 7 or Sly syndrome. The inheritance of MPS is autosomal recessive, except for MPS 2 which is X-linked. The combined prevalence of all MPS is 1/22,000. The diagnosis of MPS is confirmed by a high concentration or an abnormal urinary GAG profile and by specific enzyme assay. This assay should be carried out despite an analysis of normal urinary GAGs if the patient has symptoms attributable to MPS [29].
The main initial manifestation of MPS moderate forms is progressive joint stiffness and contracture, often starting within the first decade. The affected joints are mainly the hands and shoulders, without inflammatory signs. Hip dysplasia, kyphoscoliosis, multiple dysostosis, short stature, spinal deformities and cervical cord compression are also described. In MPS 4, joint hypermobility is observed and its occurrence at a young age should systematically suggest such diagnosis., especially since the other symptoms are often poor. The presence of muscle-tendon contractures manifested by “claw hand” is characteristic of MPS 1 [30,31,32]. Non-articular clinical manifestations are recurrent inguinal and umbilical hernia, corneal clouding, mental retardation, facial dysmorphia, hepatosplenomegaly, valvular diseases, hearing loss, sleep apnea syndrome, infections and repeated respiratory tract infections [29].
Treatment for these moderate forms consists in enzyme replacement therapy available for MPS 1, 2, 4a, 6 and 7. Orthopedic surgery may improve quality of life and function [33]. Early diagnosis of these moderate forms by rheumatologist is essential since specific treatment is now available for some subtypes and might, if given early, slow down the development of tissue damage, which is unfortunately irreversible [30].
Type 3 mucolipidosis : pseudo-hurler polydystrophy
Type 3 Mucolipidosis is a lysosomal disease due to the N-acetylglucosaminyl-1-phosphotransferase deficiency, an enzyme responsible for targeting lysosomal enzymes to lysosome through the mannose-6-phosphate (M6P) signal. It can be caused by biallelic pathogenic variants in the GNPTAB gene (Mucolipidosis type 3-alpha/beta) or in the GNPTG (Mucolipidosis type 3-gamma). The inheritance is autosomal recessive. Diagnosis is confirmed through the detection of the increased activity of acid hydrolases in serum and their corresponding decrease in fibroblasts. Treatment is only symptomatic [34].
For Mucolipidosis type 3-gamma, the clinical presentation is close to Scheie syndrome (MPS 1), but with no/mild corneal clouding. There is an initial predominant articular symptomatology such as progressive joint stiffness which often begins within the first decade and primarily affects hands and shoulders without any inflammatory signs. The disease can also affect hips and the temporomandibular joint [35, 36]. Other musculoskeletal manifestations are carpal tunnel syndrome, dysostosis multiplex, short stature, spinal deformities and cervical cord compression (with odontoid dysplasia and atlanto-axial dislocation). Other clinical manifestations are hepatosplenomegaly, valvular diseases, deafness, moderate psychomotor retardation and mild facial dysmorphia [5, 34].
Type 1 gaucher disease
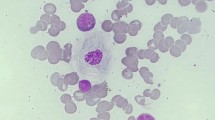
Gaucher disease (GD) is a lysosomal storage disease of the sphingolipidoses group, due to beta-glucocerebrosidase deficiency associated with GBA gene mutations. This deficit is responsible for an intra-lysosomal accumulation of a glycosphingolipid, glucocerebroside, in tissue macrophages. GD type 1 is the non-neurological form, diagnosed in adolescence or adulthood. In the GD French registry, the mean age at diagnosis was 22 years with extremes ranging from 0 to 84 years [37]. The transmission of the disease is autosomal recessive. Its prevalence is 1/50,000 to 1/40,000. Diagnosis is based on the detection of a deficient enzyme glucocerebrosidase activity in leukocytes followed by genetic analysis.
Patients present with pain that mimic joint manifestation, but which correspond to epiphyseal bone infarction known as “bone crisis”, affecting mainly the femoral heads, lumbar vertebrae, the proximal portions of the tibia and humerus. Bone infarction can mimic osteomyelitis and infection should be ruled out. Such infarctions may further lead tosecondary osteoarthritis or mechanical spinal pain associated with post fracture hyperkyphosis. Other musculoskeletal manifestations are the occurrence of pathological fractures on osteoporosis or small in size lytic lesions [38].
The abnormalities that can be identified in X-rays (secondary to epiphyseal bone infarction) look like an Erlenmeyer flask with metaphyseal diaphyseal widening of long bones predominant in distal femoral or proximal tibial and cortical thinning. X-ray may also show localized areas of condensation also known as “bone in the bone” (calcified sequelae of ischemic areas) and sometimes localized pseudo-tumoral lytic foci wrongly suggestive of suspected bone lesions [39]. Systemic manifestations of the disease are asthenia, hepatosplenomegaly, anemia and thrombocytopenia, dysglobulinemia or multiple myeloma and, rarely, interstitial lung disease or portal hypertension.
Therapy of GD is based upon enzyme replacement therapy [40,41,42] or substrate reduction therapy along with symptomatic measures (including hip arthroplasty if necessary) [43]. Regular MRI follow-up of the femoral heads, osteodensitometry and X-rays of the symptomatic areas are primordial. Because secondary osteoarthritis and osteoporotic fractures occurs in at least 20% of the patients, it is important for rheumatologists to detect and treat GD as earlier as possible.
Arthritis
Arthritis, destructive or not, microcrystalline or otherwise, may also reveal an IMD in adulthood. Thus, any arthritis, including any crystal-induced arthritis occurring at a young age, should suggest the diagnosis of IMD. Etiological orientation requires an enhanced history taking, including family history, age of onset of symptoms and their evolution and attendant symptoms (Table 2). The type of arthritis should also be able to guide the diagnosis. Crystal-induced arthritis with uric acid crystals may be secondary to a so-called “enzymopathic” gout, that with calcium pyrophosphate crystals secondary to Gitelman syndrome or hypophosphatasia, and that with oxalate crystals to primary hyperoxaluria. The clinician should therefore always look for associated renal impairment. Non-destructive recurrent acute arthritis may suggest a mevalonate kinase deficiency.
“Enzymopathic” gout
Gout can be secondary to a purine metabolism disorder such as hypoxanthine-guanine phosphoribosyltransferase (HPRT) deficiency, which can be partial or complete in the Lesch-Nyhan syndrome. The transmission of these diseases is X-linked. The biological profile includes hyperuricemia (usually greater than patients with primary gout) with hyperuricosuria. Diagnosis is made by measuring the activity of the enzyme on erythrocytes and fibroblasts in culture [44].
HPRT deficiency combines neurological and behavioral disorders with uric acid overproduction symptoms as gout or recurrent nephrolithiasis that may lead to renal failure. Clinical symptoms usually appear in the first years of life but some moderate forms exist without neurological manifestations with the first symptoms onset in adolescence or adulthood up to 30 years. Joint manifestations are the same as those of primary gout but onset is earlier, causing severe chronic urate arthropathy with significant joint deformity. Similarly, patients present with early onset urate nephropathy with recurrent urinary lithiasis and early evolution to renal impairment [45, 46].
Treatment is similar to primary gout, based on allopurinol and symptomatic measures. Since gout in the young adult can sometimes be the only symptom of the disease, rheumatologists must be aware of this condition, especially because these young patients can unknowingly pass the disease to their offspring [44].
Gitelman syndrome
Gitelman syndrome, also known as familial hypokalemia-hypomagnesemia, is well known by nephrologists and is due to a mutation of the NCCT/SLC12A3 gene encoding the Na-Cl cotransporter sensitive to thiazide diuretics located at the distal convoluted tubule. The transmission of the disease is autosomal recessive. Its prevalence is approximately 1/40,000. Biological abnormalities lead to this diagnosis: hypokalemia, hypomagnesemia, metabolic alkalosis, hypocalciuria, urinary sodium loss despite an elevation of renine-angiotensine serum levels. The diagnosis is confirmed by genetic analysis. Acquired Gitelman syndrome can also occur in patients with primary Sjögren syndrome [47, 48].
In most cases, symptoms begin after the age of six years and the disease is usually diagnosed during adolescence or adulthood. Symptoms are poor, marked by transient episodes of muscle weakness and cramps, paresthesia, and sometimes abdominal pain and vomiting. Arterial blood pressure is low. The joint manifestation is represented by chondrocalcinosis and is directly linked to hypomagnesemia [47]. Joint manifestations may start before the age of 50 years, with destructive or non-destructive polyarthritis, which develops by recurrent attacks known as “pseudo-gout” [49]. After the age of 50 years, another clinical form is described with more aggressive oligoarticular presentation leading to destructive chronic microcrystalline arthropathy [50].
Treatment is symptomatic with magnesium and potassium supplementation. The treatment for joint crises is the same as that of idiopathic pyrophosphate arthropathy. Rheumatologists should consider this metabolic disorder when chondrocalcinosis occurs in younger patients.
Hypophosphatasia
Hypophosphatasia is caused by a deficiency in the activity of serum alkaline phosphatase due to ALPL gene mutations. The mode of transmission may be autosomal recessive or dominant. The diagnosis is made by a sharp decline in serum alkaline phosphatase activity after excluding other diseases that may reduce serum alkaline phosphatase. Biological assessment may show hypercalcemia and hypercalciuria. ALPL gene testing confirm the diagnosis [51].
There is a wide clinical variability. Several clinical forms are currently recognized: pediatric forms, adult form and odontohypophosphatasia. The adult form is characterized by pyrophosphate arthropathy associated with bone demineralization manifesting as multiple fractures. Non-specific muscle and bone pain is often reported. Calcified periarthritis due to apatite crystal deposition may occur. Calcium deposits in skin, nose and fingers are described. Delayed bone healing and dental disorders with cavities, tooth fractures or early loss of teeth are often associated. Other signs include myopathy, nephrocalcinosis and ophthalmic calcification [52, 53].
X-ray examination is non-specific and may show bone demineralization, osteomalacia-like changes, bowed long bones, epiphyseal lucencies, osteophytises specifically in the fibula and the ulna, fractures and pseudo-fractures and chondrocalcinosis [51].
Enzyme replacement therapy by asfotase alpha is available but dedicated to the most severe pediatric forms. Teriparatide has been shown to improve pain, mobility and fracture repair in adult patients. Monoclonal antisclerostin antibodies has been shown to increase bone mineral density in patients with hypophosphatasia [51, 54].
Fractures linked to hypophosphatasia can be confused with osteoporotic fractures, thus rheumatologists should adjust treatment in consequence. Indeed, bisphosphonate and denosumab may worsen the disease and vitamin D supplementation may induce and aggravate hypercalcemia [51].
Primary hyperoxaluria
There are 3 types of primary hyperoxaluria or oxalosis. Type 1 is the most common (80%) and is related to deficiency in a hepatic peroxisomal enzyme, alanine glyoxylate aminotransferase (AGT), in relation with AGTX gene mutations. The transmission of the disease is autosomal recessive. The prevalence is 1-2.9/1 000 000. There are secondary causes of hyperoxaluria in patients with fat malabsorption following bariatric surgery procedures, or chronic pancreatitis. Diagnosis is suggested by the presence of hyperoxaluria or in case of kidney failure with nephrocalcinosis. It is confirmed by genetic analysis with possible prenatal diagnosis, or by measuring AGT activity on liver biopsy [55].
Symptoms usually appear between 1 and 25 years but the diagnosis is often made later. The first symptoms are the occurrence of recurrent urinary lithiases, complicated by progressive renal impairment due to nephrocalcinosis. Oxalate accumulates within the tissues and causes multisystem disease with hypertension, arterial disease of the limbs, anemia, heart rhythm disorders, ocular signs [56].
From a joint perspective, primary hyperoxaluria is responsible for microcrystalline arthropathy which is expressed as arthralgias, acute or chronic predominantly distal symmetric polyarthritis (proximal interphalangeal and metacarpophalangeal joints, knees, elbows and ankles), tenosynovitis, bursitis and/or calcium skin deposits. X rays reveal calcification, pyrophosphate arthropathy, fractures and pseudofractures, sclerosis, cystic bone changes, dense metaphyseal bands and subperiosteal resorption adjacent to oxalate deposits. Synovial fluid shows some polymorphic intracellular oxalate crystals [57].
Treatment of primary hyperoxaluria relies on the prevention of complications with hyper-hydration, urine alkalinization, dietetic measures and pyridoxine phosphate intake (vitamin B6, the AGT coenzyme). The only curative treatment is liver transplantation with or without kidney transplantation. New RNA therapy lumisaran, has been approved in Europe and USA [58, 59]. Diagnosis is made early in only 30% patients although undelayed diagnosis is the key because the effectiveness of the treatment depends on early onset [55, 57].
Wilson’s disease
Wilson’s disease (WD) is a copper metabolism disorder due to mutations of the ATP7B gene encoding for a hepatocyte copper carrier that induces an inability of the liver cell to evacuate copper as well as a significant decrease in the synthesis of circulating ceruloplasmin. This results in liver tissue copper accumulation and then extrahepatic accumulation by releasing free copper into the general circulation. The disease is transmitted in an autosomal recessive mode. Its prevalence is estimated at 1/30,000 [60].
Diagnosis is difficult and is based on a range of clinical and biological biomarkers. This is a combination of a low or collapsed serum ceruloplasmin and high urinary copper concentrations. Rarely, a liver biopsy to measure copper levels can be useful [61]. Genetic analysis is performed for diagnosis confirmation or family screening but the negativity of the test does not rule out the diagnosis even with recent progress on the subject [62].
The onset of clinical manifestations is from 5 to 35 years and clinical presentation varies widely from one individual to another. The revealing symptoms are often hepatic or neurological. The hepatic form is revealed by acute hepatitis, but may also present as chronic hepatitis or cirrhosis. The neurological form gradually associates tremor, dysarthria, dystonia, swallowing disorders and psychiatric symptoms in varying degrees. The late onset form is characterized by a significant liver injury but relatively mild neurological symptoms [60, 63].
In case of neurological impairment, brain MRI shows pronounced T1 hypointense lesions and T2 hyperintense lesions affecting the basal ganglia. Mesencephalic damage gives a “Face of the Giant Panda” appearance. Other possible manifestations of WD are hematological hemolysis, renal tubulopathies, osteomalacia and osteoporosis and cardiomyopathies with arrhythmias. A Kayser-Fleischer ring can be observed by slit lamp biomicroscopy [60].
WD can also manifest through joint symptoms that usually appear after the age of 20 years such as destructive symmetric arthritis of the large joints, affecting spine, wrists, elbows, shoulders, hips, knees and metacarpophalangeal joints. X-rays show joint damage with joint space narrowing, osteophytes, subchondral sclerosis, subchondral geodes, periarticular osteopenia. Pyrophosphate arthropathy can occur in some cases [64, 65].
Treatment is based on the use of either copper chelators such as D-penicillamine or triethylenetetramine, or zinc which reduces copper absorption [66]. An unexplained polyarthritis in a patient with liver and neurological symptoms should push the clinicians to screen for Wilson’s disease.
Mevalonate kinase deficiency
Mevalonate kinase deficiency (MKD), formerly known as “Hyper-IgD syndrome”, is related to a deficiency in an enzyme involved in cholesterol biosynthesis that results in the accumulation of mevalonic acid. Transmission is autosomal recessive and the mutation affects the MVD gene. Diagnosis is mainly clinical but biological arguments can be found by detection of urinary mevalonic acid during febrile attacks or dosing lymphocytic mevalonate kinase activity. An increased polyclonal IgD and IgA serum levels is present in most patients during the crisis along with an important elevation of C-reactive protein and/or neutrophilic leukocytosis. The search for a mutation in the gene encoding MVK is then carried out to confirm diagnosis [67].
MKD is a systemic autoinflammatory disease (SAID) defined as abnormal activation of innate immunity in the absence of autoimmunity. Because of their genetic nature, these diseases often have an early onset, but some patients can develop symptoms during adulthood. They are rare diseases and clinical spectrum is wide. Some SAID are characterized by recurrent flares of systemic inflammation associating fever, rash, serositis and lymphadenopathy separated by symptom-free intervals. Others present a more chronic course [68].
For the rheumatologist, SAIDs can mimic autoimmune disease. Early onset, family history, absence of auto-immunity, acute inflammatory flares and no effect of conventional disease-modifying anti-rheumatic drugs (cDMARDs) should raise suspicion.
Concerning MKD, the moderate adult form is characterized by a clinical picture dominated by recurrent febrile crises that begin in the first years of life, with a duration of 3 to 7 days every 2 to 8 weeks, with a frequency that decreases with age. Patients remain asymptomatic outside crisis. During acute crisis, they may suffer from, in order of frequency, asthenia, lymphadenopathy (that can be painful), abdominal pain, arthralgia, maculopapular rash, headache, pharyngitis, uveitis mood disorders and sometimes from severe neurological symptoms. Complications are AA amyloidosis, joint stiffness and abdominal adhesions [67, 69].
Acute MKD crises may be accompanied by inflammatory polyarthralgia with or without arthritis, non-erosive, symmetric, affecting large joints, especially knees and hips and sometimes metacarpophalangeal joint [69].
Prognosis of MKD is usually good, carrying a normal life expectancy, although the quality of life is significantly affected. The treatment strategy consists in on-demand therapy during flares by corticosteroids or anti-IL1 agents (canakinumab). A continuous therapy is used in most patients depending on the evolution. Anti-TNF alpha may also be effective [70].
Heterozygous familial hypercholesterolemia
Familial hypercholesterolemia (FH) is a lipid metabolism disorder characterized by a sustained elevation of circulating low density lipoprotein (LDL), by default of endocytosis, linked with mutations in the encoding genes for LDLR, APOB and PCSK9 proteins. There are two main clinical forms: a less noisy heterozygous form and a more severe homozygous form. Transmission is autosomal dominant. Prevalence is estimated at 1/500 in the heterozygous form. The heterozygous form is characterized by an LDL cholesterol of around 3 g/L (7–8 mmol/L). The Dutch lipid score is commonly used for the probability estimation of FH [71].
In the heterozygous form, tendon xanthomas, subcutaneous xanthomas at the elbow, corneal arch and xanthelasma (eyelid xanthoma) appear within the second and third decade, and finally arterial disease often appears after the age of 30 years. In the homozygous form, the same manifestations are seen earlier, with cutaneous xanthomas and manifest arterial disease before the age of 10 years [72].
Joint manifestations occur in 40% these patients affected by FH, and begin around the age of 18–20 years. The main manifestation is represented by recurrent episodes of subacute pain in the Achilles tendons, responsible for a limp, with or without signs of localized inflammation, spontaneously evolving favorably within two-three days [73]. Some old reviews mention episodes of arthritis spontaneously evolving favorably within ten days without joint destruction [74].
Treatment for heterozygous FH consists of a lipid-lowering diet and treatment aimed at reducing LDL cholesterol by 50% with the prescription of statin +/- ezetimibe. Two PCSK9 inhibitors, evolucumab and alirocumab, may be prescribed in patients who do not reach the LDL-cholesterol target at the maximum tolerated dose of statin [72, 75]. The aim of the treatment is mainly to prevent ischemic heart disease and early clinical identification of tendon xanthomas is essential in that way [76]. Usually, tendon xanthomas resolves after the start of the lipid-lowering treatment [73].
Sitosterolemia
Sitosterolemia, also known as phytosterolemia, is an autosomal recessive lipid metabolism disorder resulting in increased serum concentrations of plant sterols. Sitosterolemia is linked with mutations of ABCG5 and ABCG8 gene (that play an important role in excreting sterols from the liver and intestine). Prevalence is roughly estimated at 1 in 200 000 (but is difficult to assess because patients are often misdiagnosed as FH). Diagnosis is done measuring serum sitosterol and is confirmed if FH is eliminated by genetic analysis [77].
Clinical manifestations are globally similar to FH, but with a wide variability, and usually appear in young adults. Tendon xanthomas and subcutaneous xanthomas are often described as the first manifestations of the disease. Cytopenia with or without splenomegaly and hepatic fibrosis can happen. In the end, without treatment, arterial disease usually appears [78]. Arthralgias occur with recurrent episodes and may be misdiagnosed as an inflammatory rheumatic disease. Few details about joint manifestations are available given to the rarity of the disease [79, 80].
Tratment for sitosterolemia consists in a plant sterol lowering diet, with lipid lowering treatment. Statins are often ineffective, and ezetimibe is the main molecule to use. An optimal treatment results in prevention of arterial disease and can help to reduce joint manifestations [77].
Conclusions
Joint manifestations in adults, such as arthralgias, epiphyseal pain, joint stiffness, periarthritis or arthritis may help discover late-onset IMD. The clinical presentation of these essentially pediatric diseases, when they occur in adulthood, can then take unexpected forms. Lack of knowledge of adult physicians leads to an underestimation of their frequency and management that is often delayed, with potentially severe rheumatological or systemic sequelae. In addition, considerable progress has been made in the treatment of IMD in recent years, with the development of more targeted therapies, hence the importance of identifying them the earlier as possible. When such diagnosis is suspected, it is advisable to refer patients to specialized centers for the management of IMD.
Data Availability
Not applicable.
Abbreviations
- IMD:
-
Inborn metabolic diseases
- HH:
-
Hereditary Hemochromatosis
- AKU:
-
Alkaptonuria
- MPS:
-
Mucopolysaccharidoses
- GAG:
-
Glycosaminoglycans
- GD:
-
Gaucher disease
- HPRT:
-
Hypoxanthine-guanine phosphoribosyltransferase
- AGT:
-
Alanine glyoxylate aminotransferase
- WD:
-
Wilson’s disease
- MKD:
-
Mevalonate kinase deficiency
- SAID:
-
Autoinflammatory disease
- FH:
-
Familial hypercholesterolemia
- LDL:
-
Low density lipoprotein
References
Saudubray J-M, Sedel F. Inborn errors of metabolism in adults. Ann Endocrinol. 2009;70. https://doi.org/10.1016/j.ando.2008.12.004
Sirrs S, Hollak C, Merkel M, et al. The frequencies of different inborn errors of metabolism in adult metabolic Centres: Report from the SSIEM Adult Metabolic Physicians Group. JIMD Rep. 2015;27. https://doi.org/10.1007/8904_2015_435
Fouchard A-A, Corcia P, Allais C, et al. Inborn errors of metabolism in Elderly adults. J Am Geriatr Soc. 2016;64. https://doi.org/10.1111/jgs.14333
Ranganath LR, Psarelli EE, Arnoux J-B, et al. Efficacy and safety of once-daily nitisinone for patients with alkaptonuria (SONIA 2): an international, multicentre, open-label, randomised controlled trial. Lancet Diabetes Endocrinol. 2020;8. https://doi.org/10.1016/S2213-8587(20)30228-X
Brik R, Mandel H, Aizin A et al. Mucolipidosis III presenting as a rheumatological disorder. J Rheumatol 1993;20.
Finsterer J, Melichart-Kotig M, Woehrer A. Mitochondrial disorder mimicking rheumatoid disease. Z Rheumatol. 2019;78. https://doi.org/10.1007/s00393-018-0551-1
Moiseev S, Karovaikina E, Novikov PI, et al. What rheumatologist should know about fabry disease. Ann Rheum Dis. 2020;79. https://doi.org/10.1136/annrheumdis-2019-215476
Brissot P, Pietrangelo A, Adams PC, et al. Haemochromatosis. Nat Rev Dis Primer. 2018;4. https://doi.org/10.1038/nrdp.2018.16
Contributors, Taskforce HI, Adams P, Altes A, et al. Therapeutic recommendations in HFE hemochromatosis for p.Cys282Tyr (C282Y/C282Y) homozygous genotype. Hepatol Int. 2018;12. https://doi.org/10.1007/s12072-018-9855-0
Gasser B, Courtois F, Hojjat-Assari S et al. Hereditary hemochromatosis: presenting manifestations and diagnostic delay. Rev Med Interne 2014;35.
Lange U, Teichmann J, Dischereit G. Molekulargenetische Analyse und klinische Aspekte bei Patienten mit hereditärer Hämochromatose. Orthop. 2014;43. https://doi.org/10.1007/s00132-014-2318-y
Schumacher HR, Straka PC, Krikker MA, et al. The Arthropathy of Hemochromatosis.: recent studies. Ann N Y Acad Sci. 1988;526. https://doi.org/10.1111/j.1749-6632.1988.tb55508.x
Romas E. The “iron salute” in haemochromatosis. Aust Fam Physician 2009;38.
Nguyen C-D, Morel V, Pierache A, et al. Bone and joint complications in patients with hereditary hemochromatosis: a cross-sectional study of 93 patients. Ther Adv Musculoskelet Dis. 2020;12. https://doi.org/10.1177/1759720X20939405
Sahinbegovic E, Dallos T, Aigner E et al. Musculoskeletal disease burden of hereditary hemochromatosis. Arthritis Rheum 2010;62.
Wijarnpreecha K, Aby ES, Panjawatanan P, et al. Hereditary hemochromatosis and risk of joint replacement surgery: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2021;33. https://doi.org/10.1097/MEG.0000000000001704
Carroll GJ, Breidahl WH, Bulsara MK, et al. Hereditary hemochromatosis is characterized by a clinically definable arthropathy that correlates with iron load. Arthritis Rheum. 2011;63. https://doi.org/10.1002/art.30094
Faridi W, Dhamoon AS. Ochronosis (Book), edited by StatPearls Publishing, 2022. http://www.ncbi.nlm.nih.gov/books/NBK560534/ (accessed Oct 2022).
Ranganath LR, Cox TF. Natural history of alkaptonuria revisited: analyses based on scoring systems. J Inherit Metab Dis 2011;34.
Khan UN, Wenokor C, Altschuler EL. Back Pain in a middle-aged man: Alkaptonuria. Am J Phys Med Rehabil 2015;94.
Khan AH, Afroze B, Majid H, et al. Musculoskeletal manifestations in Alkaptonuria: a cross-sectional study. Med (Baltim). 2021;100. https://doi.org/10.1097/MD.0000000000028241
Mannoni A, Selvi E, Lorenzini S et al. Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin Arthritis Rheum 2004;33.
Ladjouze-Rezig A, Rodriguez de Cordoba S, Aquaron R. Ochronotic rheumatism in Algeria: clinical, radiological, biological and molecular studies—a case study of 14 patients in 11 families. Joint Bone Spine. 2006;73. https://doi.org/10.1016/j.jbspin.2005.03.010
Cetinus E, Cever I, Kural C, et al. Ochronotic arthritis: case reports and review of the literature. Rheumatol Int. 2005;25. https://doi.org/10.1007/s00296-004-0538-x
Demir S. Alkaptonuric ochronosis: a case with multiple joint replacement arthroplasties. Clin Rheumatol. 2003;22. https://doi.org/10.1007/s10067-003-0760-z
Raaijmaakers M, Steenbrugge F, Dierickx C. Ochronosis, arthroscopy of a black knee: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2008;16. https://doi.org/10.1007/s00167-007-0413-x
de Haas V, Weber ECC, de Klerk JBC, et al. The success of dietary protein restriction in alkaptonuria patients is age-dependent. J Inherit Metab Dis. 1998;21. https://doi.org/10.1023/A:1005410416482
Rajkumar N, Soundarrajan D, Dhanasekararaja P, et al. Clinical and radiological outcomes of total joint arthroplasty in patients with ochronotic arthropathy. Eur J Orthop Surg Traumatol Orthop Traumatol. 2020;30. https://doi.org/10.1007/s00590-020-02651-0
Khan SA, Peracha H, Ballhausen D, et al. Molecular Genetics and Metabolism. Mol Genet Metab. 2017;121. https://doi.org/10.1016/j.ymgme.2017.05.016
Mitrovic S, Gouze H, Gossec L, et al. Mucopolysaccharidoses seen in adults in rheumatology. Joint Bone Spine. 2017;84. https://doi.org/10.1016/j.jbspin.2017.01.008
Cimaz R, Coppa GV, Koné-Paut I et al. Joint contractures in the absence of inflammation may indicate mucopolysaccharidosis. Pediatr Rheumatol Online J 2009;7.
Cimaz R, Vijay S, Haase C et al. Attenuated type I mucopolysaccharidosis in the differential diagnosis of juvenile idiopathic arthritis: a series of 13 patients with Scheie syndrome. Clin Exp Rheumatol 2006;24.
Williams N, Challoumas D, Eastwood DM. Does orthopaedic surgery improve quality of life and function in patients with mucopolysaccharidoses? J Child Orthop. 2017;11. https://doi.org/10.1302/1863-2548.11.170042
Umehara F, Matsumoto W, Kuriyama M et al. Mucolipidosis III (pseudo-hurler polydystrophy); clinical studies in aged patients in one family. J Neurol Sci 1997;146.
Khalifa H, Grubisa HS, Lee L, et al. Enlarged follicles and temporomandibular joint abnormalities in mucolipidosis type III. Dento Maxillo Facial Radiol. 2013;42. https://doi.org/10.1259/dmfr/22822014
Lewis JRP, Gibson PH. Bilateral hip replacement in three patients with lysosomal storage disease: mucopolysaccharidosis type IV and mucolipidosis type III. J Bone Joint Surg Br. 2010;92. https://doi.org/10.1302/0301-620X.92B2.23104
Stirnemann J, Vigan M, Hamroun D, et al. The french Gaucher’s disease registry: clinical characteristics, complications and treatment of 562 patients. Orphanet J Rare Dis. 2012;7. https://doi.org/10.1186/1750-1172-7-77
Javier R-M, Hachulla É. Atteintes ostéoarticulaires de la maladie de gaucher chez l’adulte: de la physiopathologie au traitement. Presse Médicale. 2007;36. https://doi.org/10.1016/j.lpm.2007.04.012
Manger B, Mengel E, Schaefer RM. Rheumatologic aspects of lysosomal storage diseases. Clin Rheumatol. 2007;26. https://doi.org/10.1007/s10067-006-0299-x
Weinreb NJ, Goldblatt J, Villalobos J et al. Long-term clinical outcomes in type 1 gaucher disease following 10 years of imiglucerase treatment. J Inherit Metab Dis 2013;36.
Serratrice C, Bengherbia M, Alessandrini M et al. Effects of switching from imiglucerase to velaglucerase alfa without dose reduction nor wash out in type 1 gaucher disease. Blood Cells Mol Dis 2014;53.
Pastores GM, Petakov M, Giraldo P et al. A phase 3, multicenter, open-label, switchover trial to assess the safety and efficacy of taliglucerase alfa, a plant cell-expressed recombinant human glucocerebrosidase, in adult and pediatric patients with gaucher disease previously treated with imiglucerase. Blood Cells Mol Dis 2014;53.
Cox TM, Drelichman G, Cravo R, et al. Eliglustat compared with imiglucerase in patients with Gaucher’s disease type 1 stabilised on enzyme replacement therapy: a phase 3, randomised, open-label, non-inferiority trial. Lancet Lond Engl. 2015;385. https://doi.org/10.1016/S0140-6736(14)61841-9
Doucet BP, Jegatheesan D, Burke J. Late diagnosis of Lesch-Nyhan disease variant. BMJ Case Rep 2013;2013. doi:https://doi.org/10.1136/bcr-2013-201997
Saigal R, Chakraborty A, Yadav RN et al. Partial HPRT deficiency (Kelley-Seegmiller syndrome. J Assoc Physicians India 2006;54.
Madeo A, Di Rocco M, Brassier A, et al. Clinical, biochemical and genetic characteristics of a cohort of 101 french and italian patients with HPRT deficiency. Mol Genet Metab. 2019;127. https://doi.org/10.1016/j.ymgme.2019.06.001
Favero M, Calò LA, Schiavon F, et al. Miscellaneous non-inflammatory musculoskeletal conditions. Bartter’s and Gitelman’s diseases. Best Pract Res Clin Rheumatol. 2011;25. https://doi.org/10.1016/j.berh.2011.10.013
Kim YK, Song HC, Kim W-Y, et al. Acquired Gitelman Syndrome in a patient with primary Sjögren Syndrome. Am J Kidney Dis. 2008;52. https://doi.org/10.1053/j.ajkd.2008.07.025
Martínez Tomàs A, Rueda Cid A, Campos Fernández C, et al. Carpal arthritis as the initial manifestation of Gitelman’s syndrome. Reumatol Clínica Engl Ed. 2012;8. https://doi.org/10.1016/j.reumae.2011.11.006
Chotard E, Blanchard A, Ostertag A, et al. Calcium pyrophosphate crystal deposition in a cohort of 57 patients with Gitelman syndrome. Rheumatology. 2022;61. https://doi.org/10.1093/rheumatology/keab578
Bangura A, Wright L, Shuler T. Hypophosphatasia: current literature for pathophysiology, clinical manifestations, diagnosis, and treatment. Cureus. 2020. https://doi.org/10.7759/cureus.8594
Dahir KM, Seefried L, Kishnani PS, et al. Clinical profiles of treated and untreated adults with hypophosphatasia in the Global HPP Registry. Orphanet J Rare Dis. 2022;17. https://doi.org/10.1186/s13023-022-02393-8
Szabo SM, Tomazos IC, Petryk A, et al. Frequency and age at occurrence of clinical manifestations of disease in patients with hypophosphatasia: a systematic literature review. Orphanet J Rare Dis. 2019;14. https://doi.org/10.1186/s13023-019-1062-0
Michigami T, Ohata Y, Fujiwara M, et al. Clinical practice guidelines for Hypophosphatasia. Clin Pediatr Endocrinol. 2020;29. https://doi.org/10.1297/cpe.29.9
Martin M et al. Delayed diagnosis of primary hyperoxaluria in a young patient with advanced chronic renal failure. Nefrología 2011. doi:https://doi.org/10.3265/Nefrologia.pre2010.Nov.10725
Verbruggen LA, Bourgain C, Verbeelen D. Late presentation and microcrystalline arthropathy in primary hyperoxaluria. Clin Exp Rheumatol 1989;7.
Lorenz EC, Michet CJ, Milliner DS, et al. Update on Oxalate Crystal Disease. Curr Rheumatol Rep. 2013;15. https://doi.org/10.1007/s11926-013-0340-4
Michael M, Groothoff JW, Shasha-Lavsky H, et al. Lumasiran for Advanced primary hyperoxaluria type 1: phase 3 ILLUMINATE-C trial. Am J Kidney Dis Off J Natl Kidney Found. 2022. https://doi.org/10.1053/j.ajkd.2022.05.012
Cochat P, Hulton S-A, Acquaviva C, et al. Primary hyperoxaluria type 1: indications for screening and guidance for diagnosis and treatment. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2012;27. https://doi.org/10.1093/ndt/gfs078
Guindi M. Wilson disease. Semin Diagn Pathol. 2019;36. https://doi.org/10.1053/j.semdp.2019.07.008
Salman HM, Amin M, Syed J, et al. Biochemical testing for the diagnosis of Wilson’s disease: a systematic review. J Clin Lab Anal. 2022;36. https://doi.org/10.1002/jcla.24191
Espinós C, Ferenci P. Are the new genetic tools for diagnosis of Wilson disease helpful in clinical practice? JHEP Rep. 2020;2. https://doi.org/10.1016/j.jhepr.2020.100114
Zhu Q, Zhu K, Wang J, et al. Relationship between genetic mutations and clinical phenotypes in patients with Wilson disease. Med (Baltim). 2019;98. https://doi.org/10.1097/MD.0000000000018284
Wickrematilake GW. Calcium pyrophosphate Dihydrate Deposition Disease in Young Patients: two case reports. Arch Rheumatol. 2016;32. https://doi.org/10.5606/ArchRheumatol.2017.6015
Misra AK, Biswas A, Ganguly G et al. Arthropathic presentation of Wilson’s disease. J Assoc Physicians India 2004;52.
Appenzeller-Herzog C, Mathes T, Heeres MLS, et al. Comparative effectiveness of common therapies for Wilson disease: a systematic review and meta-analysis of controlled studies. Liver Int Off J Int Assoc Study Liver. 2019;39. https://doi.org/10.1111/liv.14179
ter Haar NM, Jeyaratnam J, Lachmann HJ, et al. The phenotype and genotype of mevalonate kinase Deficiency: a series of 114 cases from the Eurofever Registry. Arthritis Rheumatol. 2016;68. https://doi.org/10.1002/art.39763
Georgin-Lavialle S, Ducharme-Benard S, Sarrabay G, et al. Systemic autoinflammatory diseases: clinical state of the art. Best Pract Res Clin Rheumatol. 2020;34. https://doi.org/10.1016/j.berh.2020.101529
van der Hilst JCH, Bodar EJ, Barron KS, et al. Long-term follow-up, clinical features, and quality of life in a series of 103 patients with hyperimmunoglobulinemia D syndrome. Med (Baltim). 2008;87. https://doi.org/10.1097/MD.0b013e318190cfb7
Romano M, Arici ZS, Piskin D, et al. The 2021 EULAR/American College of Rheumatology points to consider for diagnosis, management and monitoring of the interleukin-1 mediated autoinflammatory diseases: cryopyrin-associated periodic syndromes, tumour necrosis factor receptor-associated periodic syndrome, mevalonate kinase deficiency, and deficiency of the interleukin-1 receptor antagonist. Ann Rheum Dis. 2022;81. https://doi.org/10.1136/annrheumdis-2021-221801
Wadsack D, Sattler H, Kleber ME, et al. Recurrent tendosynovitis as a rare manifestation of a lipid disorder. J Clin Lipidol. 2019;13. https://doi.org/10.1016/j.jacl.2018.10.005
Turgeon RD, Barry AR, Pearson GJ. Hypercholestérolémie familiale. Can Fam Physician 2016;62.
Tsouli SG, Kiortsis DN, Argyropoulou MI, et al. Pathogenesis, detection and treatment of Achilles tendon xanthomas. Eur J Clin Invest. 2005;35. https://doi.org/10.1111/j.1365-2362.2005.01484.x
Wysenbeek AJ, Shani E, Beigel Y. Musculoskeletal manifestations in patients with hypercholesterolemia. J Rheumatol 1989;16.
Tarpley AJ. New Frontier in lipids: PCSK9 inhibitors and implications for the Life Insurance Industry. J Insur Med N Y N. 2018;47. https://doi.org/10.17849/insm-47-4-1-6.1
Fujiwara R, Yahiro R, Horio T, et al. Achilles tendon thickness is associated with coronary lesion severity in acute coronary syndrome patients without familial hypercholesterolemia. J Cardiol. 2022;79. https://doi.org/10.1016/j.jjcc.2021.09.021
Tada H, Nomura A, Ogura M, et al. Diagnosis and management of sitosterolemia 2021. J Atheroscler Thromb. 2021;28. https://doi.org/10.5551/jat.RV17052
Wang Z, Cao L, Su Y, et al. Specific macrothrombocytopenia/hemolytic anemia associated with sitosterolemia. Am J Hematol. 2014;89. https://doi.org/10.1002/ajh.23619
Cao LJ, Yu ZJ, Jiang M, et al. Clinical features of 20 patients with phytosterolemia causing hematologic abnormalities. Zhonghua Yi Xue Za Zhi. 2019;99. https://doi.org/10.3760/cma.j.issn.0376-2491.2019.16.007
Zhou Z, Su X, Cai Y, et al. Features of chinese patients with sitosterolemia. Lipids Health Dis. 2022;21. https://doi.org/10.1186/s12944-021-01619-1
Acknowledgements
Not applicable.
Funding
The authors does not have funding sources to declare.
Author information
Authors and Affiliations
Contributions
AL performed an extensive bibliographic review and was a major contributor in writing the manuscript. CJ also participated in bibliographic research and was also a major contributor in writing the manuscript. FM oversaw this work. IS provided comprehensive advices on the content of the manuscript. SM, AB, HB, AA and DM participated in enriching this work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Loret, A., Jacob, C., Mammou, S. et al. Joint manifestations revealing inborn metabolic diseases in adults: a narrative review. Orphanet J Rare Dis 18, 239 (2023). https://doi.org/10.1186/s13023-023-02810-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02810-6