Abstract
CSF1R mutations cause autosomal-dominant CSF1R-related leukoencephalopathy with axonal spheroids and pigmented glia (CSF1R-ALSP) and autosomal-recessive brain abnormalities, neurodegeneration, and dysosteosclerosis (BANDDOS). The former is increasingly recognized, and disease-modifying therapy was introduced; however, literature is scarce on the latter. This review analyzes BANDDOS and discusses similarities and differences with CSF1R-ALSP.
We systematically retrieved and analyzed the clinical, genetic, radiological, and pathological data on the previously reported and our cases with BANDDOS. We identified 19 patients with BANDDOS (literature search according to the PRISMA 2020 guidelines: n = 16, our material: n = 3). We found 11 CSF1R mutations, including splicing (n = 3), missense (n = 3), nonsense (n = 2), and intronic (n = 2) variants and one inframe deletion. All mutations disrupted the tyrosine kinase domain or resulted in nonsense-mediated mRNA decay. The material is heterogenous, and the presented information refers to the number of patients with sufficient data on specific symptoms, results, or performed procedures. The first symptoms occurred in the perinatal period (n = 5), infancy (n = 2), childhood (n = 5), and adulthood (n = 1). Dysmorphic features were present in 7/17 cases. Neurological symptoms included speech disturbances (n = 13/15), cognitive decline (n = 12/14), spasticity/rigidity (n = 12/15), hyperactive tendon reflex (n = 11/14), pathological reflexes (n = 8/11), seizures (n = 9/16), dysphagia (n = 9/12), developmental delay (n = 7/14), infantile hypotonia (n = 3/11), and optic nerve atrophy (n = 2/7). Skeletal deformities were observed in 13/17 cases and fell within the dysosteosclerosis – Pyle disease spectrum. Brain abnormalities included white matter changes (n = 19/19), calcifications (n = 15/18), agenesis of corpus callosum (n = 12/16), ventriculomegaly (n = 13/19), Dandy-Walker complex (n = 7/19), and cortical abnormalities (n = 4/10). Three patients died in infancy, two in childhood, and one case at unspecified age. A single brain autopsy evidenced multiple brain anomalies, absence of corpus callosum, absence of microglia, severe white matter atrophy with axonal spheroids, gliosis, and numerous dystrophic calcifications.
In conclusion, BANDDOS presents in the perinatal period or infancy and has a devastating course with congenital brain abnormalities, developmental delay, neurological deficits, osteopetrosis, and dysmorphic features. There is a significant overlap in the clinical, radiological, and neuropathological aspects between BANDDOS and CSF1R-ALSP. As both disorders are on the same continuum, there is a window of opportunity to apply available therapy in CSF1R-ALSP to BANDDOS.
Similar content being viewed by others
Introduction
Mutations in the colony-stimulating factor-1 receptor (CSF1R) gene may account for up to 25% of adult-onset leukoencephalopathies [1, 2]. Most of the previously reported CSF1R mutation carriers had only one mutant allele and presented with an autosomal-dominant neurodegenerative disorder characterized by neuropsychiatric and motor symptoms, white matter lesions on magnetic resonance imaging (MRI), brain calcifications with stepping stone appearance on computed tomography, axonal spheroids and pigmented glia on neuropathological examination [3, 4]. The disease was previously known as hereditary diffuse leukoencephalopathy with spheroids (HDLS) or pigmentary orthochromatic leukodystrophy, but the expanding knowledge of leukoencephalopathies led to the new classification, and it was named adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP) [1, 2, 5, 6]. Most cases of ALSP are due to the CSF1R mutations; however, AARS2 mutations were reported in CSF1R-negative ALSP, a single Swedish HDLS family was found to carry an AARS1 mutation, and ALSP without CSF1R, AARS1 or AARS2 mutation was reported [7,8,9]. As of January 2023, approximately 300 cases of CSF1R-ALSP were reported, but with genetic testing available commercially, the disease is increasingly recognized, and at present, the prevalence is estimated at 30–75 cases/million [1].
Furthermore, few case reports have been published with patients carrying two mutant CSF1R alleles presenting with brain abnormalities, neurodegeneration, and dysosteosclerosis (BANDDOS), and a new entity has been recognized (MIM#618,476) [10]. The literature on BANDDOS is scarce, and the clinical presentation and radiological and neuropathological features are yet to be elucidated. Disease-modifying treatment is available for the CSF1R-ALSP, and an interventional clinical trial is underway (NCT05677659). As both BANDDOS and CSF1R-ALSP share a genetic basis, treatment of the latter could be potentially translated to the former. A better understanding of the BANDDOS would also benefit CSF1R-ALSP, which pathomechanism remains not fully understood.
In this paper, we add to the growing literature on the pathogenicity of CSF1R mutations and their genotype-phenotype associations by reviewing the clinical, genetic, radiological, and neuropathological features of BANDDOS. We analyzed three new BANDDOS patients from a Brazilian family and the previously published cases in the literature.
Methods
We collected the clinical, genetic, and radiological data on the family diagnosed with BANDDOS observed at the Hospital Pequeno Principe, Curitiba, Paraná, Brazil. Each individual was repeatedly evaluated by a multidisciplinary team, including geneticist, neurologist, psychologist, and radiologist. Genetic testing was performed in 5 individuals, including whole-exome sequencing (WES) in the proband and targeted sequencing in four others. WES was performed using an Agilent v5 SureSelect capture kit and Illumina HiSeq 2500 sequencing technology. Reads were aligned to a reference sequence (GRCh38), and sequence changes were identified and interpreted in the context of relevant transcripts. Targeted sequencing was performed with next-generation sequencing (NGS) technology. Brain 1.5 Tesla MRI was performed in 3 cases.
Next, we searched the MEDLINE, PubMed, Scopus, and Web of Science databases for papers on BANDDOS published until December 16, 2022. The literature search was conducted according to the PRISMA 2020 guidelines [11]. We applied the following search terms: “BANDDOS”, “CSF1R” and “homozygous”, “CSF1R” and “autosomal recessive”. We screened the titles and abstracts of the papers to check if they were relevant to the review. We searched the reference list of the relevant manuscripts and websites to identify other papers pertinent to the review.
Lastly, we extracted in a structured manner the data on the Brazilian family with BANDDOS and previously published cases identified in the literature. We retrieved the information on CSF1R mutation, demographics (sex, ethnicity, consanguinity of the parents, gestational age, birth weight, birth length, age of onset, follow-up duration, weight, and height at the last follow-up, age of death), brain autopsy, dysmorphic features, first symptoms, neurological status (infantile hypotonia, developmental delay, cognitive decline, seizures, optic nerve atrophy, dysphagia, speech disturbances, rigid-spasticity, hyperactive tendon reflexes, pathological reflexes), skeletal system symptoms (bone and tooth abnormalities), and brain imaging (Dandy-Walker malformation, ventriculomegaly, calcifications, agenesis of corpus callosum, white matter changes and cortical abnormalities).
Results
We identified three unreported siblings with homozygous CSF1R c.1754G > T (Gly585Val) mutations from Curitiba, Paraná, Brazil (Fig. 1). They were born to consanguineous parents (first cousins) and did not display dysmorphic features, bone abnormalities, or developmental delay in the first few years of their life. The III-1 developed cognitive regression and speech disturbances at 10 years, followed by seizures, dysphagia, and spastic tetraparesis over the following six years. The III-2 developed neuropsychiatric symptoms at the age of 15 years, whereas III-4 remained asymptomatic at the age of 9 years. All three had white matter changes on neuroimaging with MRI. The III-3 and II-1 were heterozygous for the Gly585Val mutation and remained asymptomatic, the II-2 refused genetic testing. In silico analysis predicted the newly identified mutation to be pathogenic (Combined Annotation Dependent Depletion score of 35) and it was likely pathogenic (PM1, PM2, PM5, PP2, PP3, PP4) according to the guidelines of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology [12].
(A) Pedigree. For family pedigree, standard pedigree symbols are used; arrow indicates the proband; circles indicate females; squares indicate males; black symbols indicate individuals diagnosed with brain abnormalities, neurodegeneration, and dysosteosclerosis (BANDDOS). (B) The Integrative Genomics Viewer snapshot displaying the newly identified CSF1R mutation.
Literature search for papers on BANDDOS yielded 124 records. After removing the duplicates (n = 87), we screened 37 papers, and subsequently excluded 30 that were not pertinent to the topic. We were able to retrieve 6/7 of the remaining manuscripts and assessed 4/6 to be relevant to the topic. We identified 3 additional papers on BANDDOS through citation and website searching, of which 2 were pertinent to the topic and were included in the review. The PRISMA 2020 flow diagram for the literature review on BANDDOS is presented in Fig. 2.
PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases, registers, and other sources
*Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers)
**If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
The demographics and CSF1R mutations of the patients with BANDDOS are presented in Table 1. The material is heterogenous, and the presented information refers to the number of patients with sufficient data regarding the specific symptoms, results, or performed procedures. Figure 3 presents the chart with the main features of BANDDOS and their frequency.
We identified a total of 19 cases (10 females, 7 males and 2 unreported sex) diagnosed with BANDDOS, including three new cases from the Brazilian family and 16 cases through the literature search [10, 13,14,15,16,17]. Most cases (n = 17/19) were born of consanguineous parents and carried homozygous mutations (n = 17/19), whereas only two were compound heterozygotes born of unrelated parents. We found 11 different CSF1R mutations, including splicing variants (n = 3), missense (n = 3), nonsense (n = 2), and intronic (n = 2) variants, and one inframe deletion. Further analysis revealed that all mutations led to functionally deficient CSF1R protein with disrupted tyrosine kinase domain or nonsense-mediated mRNA decay. Figure 4 depicts CSF1R gene and protein with mutations reported in BANDDOS, and Table 2 provides detailed information on them.
Patients were from different parts of the world and of various ethnic backgrounds, with Chaldean (n = 5), Brazilian (n = 4), Arab (n = 3), Turkish (n = 3), Indian (n = 2), Japanese, and Native American ancestry in individual cases. Most cases (9/11) were born full term, and only one was born prematurely. The mean weight and length at birth were 3600 g and 50 cm. Five cases became symptomatic before birth, 2 in infancy, and 5 in childhood, whereas only one showed first symptoms when adult. The mean follow-up duration was 9 years (8 months − 16 years). Dysmorphic features were present in 7 out of 17 cases, whereas weight and height were normal in 8/9 and 6/9, respectively, at the last evaluation at the mean age of 16 years (range 5–37 years).
Clinical characteristics of the patients with BANDDOS are presented in Table 3.
Neurological symptoms were observed in most cases (n = 15/17), including speech disturbances (n = 13/15), cognitive decline (n = 12/14), spasticity/rigidity (n = 12/15), hyperactive tendon reflex (n = 11/14), pathological reflexes (n = 8/11), seizures (n = 9/16), dysphagia (n = 9/12), developmental delay (n = 7/14), infantile hypotonia (n = 3/11), and optic nerve atrophy (n = 2/7). Skeletal deformities were observed in 13/17 cases and fell within the osteopetrosis spectrum. One case had enamel abnormalities, whereas the remaining cases with sufficient data (n = 6) had normally developed teeth.
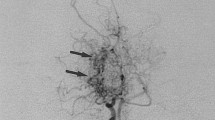
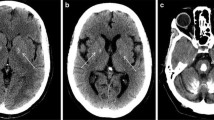
Table 4 provides the neuroimaging characteristics of the patients with BANDDOS. Brain abnormalities were present in all cases (n = 19) on neuroimaging, including white matter changes (n = 19/19), calcifications (n = 15/18), agenesis of corpus callosum (n = 12/16), ventriculomegaly (n = 13/19), Dandy-Walker complex (n = 7/19), and cortical abnormalities (n = 4/10).
Three patients died in infancy, two in childhood and one case at unspecified age, and a brain autopsy was performed in one case. Postmortem examination showed multiple brain anomalies, including an absence of corpus callosum, reduced volume of white matter, Dandy-Walker malformation, colpocephaly, numerous periventricular and brainstem calcifications, and heterotopia, abnormal gyration of hippocampi, and non-decussation of small pyramidal tracts [14]. Histological evaluation evidenced severe microglia deficiency with only rare spotting of abnormal microglia around the blood vessels, prominent white matter atrophy with axonal spheroids, gliosis, and numerous dystrophic calcifications predominantly in the periventricular white matter [14].
Discussion
In this study, we compiled data on the largest number of BANDDOS cases to date. Although it is an exceedingly rare disease, it was reported in different parts of the world, encompassing Asia and South and North America. Most cases were born of consanguineous marriages after an uncomplicated pregnancy, with normal weight and length. Figure 5 presents and compares the core features of BANNDOS and CSF1R-ALSP.
Schematic diagram of core features of the CSF1R-related adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (CSF1R-ALSP) and brain abnormalities, neurodegeneration, and dysosteosclerosis (BANDDOS). Both disorders are on the same continuum, albeit differ in the severity of CSF1R mutations’ consequences and phenotypes. WMLs – white matter lesions
Brain abnormalities were found in all cases and ranged from mild asymptomatic white matter changes to severe brain malformations. Similar to CSF1R-ALSP, white matter lesions were the most common finding on neuroimaging (in 100% of BANDDOS vs. 81% with CSF1R-ALSP cases), followed by calcifications (in 83% of BANDDOS vs. 75% with CSF1R-ALSP cases) and callosal abnormalities (agenesis in 75% of BANDDOS vs. atrophy in 29% with CSF1R-ALSP cases) [18]. Interestingly, calcifications in both disorders were present already at birth and shared a characteristic “stepping stone appearance” [2]. White matter lesions and callosal abnormalities were also present at birth in BANDDOS cases but were observed later in CSF1R-ALSP, in which they were seen around the time of the symptomatic disease onset in adulthood [2, 19]. Compared to CSF1R-ALSP, cases with BANDDOS also displayed other congenital brain anomalies, including Dandy-Walker malformation, ventriculomegaly, and cortical abnormalities.
BANDDOS and CSF1R-ALSP mainly manifest with neurological deficits. However, in the former first symptoms were most often observed in the first weeks of life, and developmental delay was present in half of the cases, whereas in the latter, the first three decades of life were usually unremarkable, and the disease started in the 4th -6th decade of life [3]. The earlier age of disease onset with the frequent developmental delay reflects the greater severity of the disease in BANDDOS. Speech disturbances were the most common neurological symptom in BANDDOS and were present in 87% of cases, with dysarthria reported in more than half of cases. Speech disorders are frequently observed in CSF1R-ALSP with complex underpinnings involving language disturbances (aphasia in up to 42%), articulation disorders (dysarthria in up to 54%), and not infrequently, both. As all cases with BANDDOS with speech disturbances had accompanying cognitive decline or developmental delay, the multifaceted nature of speech dysfunction, as seen in CSF1R-ALSP, is most likely. Progressive cognitive dysfunction was present in 86% of BANDDOS cases and was not reported only in two clinically asymptomatic Brazilian cases. Likewise, cognitive impairment is frequent in CSF1R-ALSP and occurs in 94% of cases [3]. Pyramidal signs (spasticity, hyperactive tendon reflexes, and pathological reflexes) were present in up to 80% of BANDDOS cases, compared to up to 81% of CSF1R-ALSP cases [3]. Seizures were noted in 56% of cases in BANDDOS, compared to up to 32% of CSF1R-ALSP [3]. Dysphagia was common and reported in 75% of cases of BANDDOS, compared to 18% of CSF1R-ALSP [3]. As seizures usually reflect more widespread and severe brain injury, and dysphagia is observed in the later disease stages in CSF1R-ALSP, the higher reported frequency of these symptoms in BANDDOS may be attributed to a more devastating disease course. In addition, a minority of BANDDOS cases presented infantile hypotonia (27%) and atrophy of the optic nerve (29%), which were not reported in CSF1R-ALSP. Skeletal abnormalities were observed in 76% of cases of BANDDOS. However, the extent of skeletal involvement and presentation was variable and generally fell within the dysosteosclerosis – Pyle disease spectrum. Dysmorphic features were reported in 41% of cases of BANDDOS. Skeletal deformities and dysmorphic features were often associated with complex brain abnormalities and a more ominous clinical course; however, they were also observed in one case with the adult onset of the disease. Skeletal deformities and dysmorphic features have not been reported in CSF1R-ALSP. Therefore, the presence thereof may reflect more profound sequelae of the CSF1R mutations in the BANDDOS, which impacted organs beyond the central nervous system. Similar to other childhood-onset leukoencephalopathies, the quality of life of the patients and their caregivers is severely compromised [20,21,22].
Neuropathological evaluation of one case with BANDDOS evidenced significant overlap with CSF1R-ALSP [2, 9, 14]. Macroscopically both disorders shared extensive white matter degeneration, most prominent in the periventricular region, corpus callosum, and pyramidal tracts [2, 9, 14]. Likewise, histological evaluation evidenced a deficiency of microglia in the brain parenchyma, atrophic white matter with axonal spheroids, gliosis, and dystrophic calcifications in BANDDOS and CSF1R-ALSP [2, 9, 14]. However, the former had much greater severity of the disease process, as reflected by macroscopic (absence of corpus callosum, Dandy-Walker malformation, and other) and microscopic (almost complete absence of microglia) findings [14].
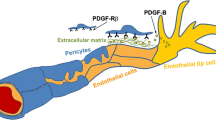
The CSF1R is a transmembrane tyrosine-protein kinase serving as a receptor for CSF1 (colony-stimulating factor-1) and interleukin-34 (IL34) [1, 23, 24]. It participates in the innate immunity and inflammatory response through the release of pro-inflammatory cytokines [23]. It also plays a crucial role in the development, proliferation, activation, and survival of the monocyte phagocytic system [1, 23, 25, 26]. Both microglia of the central nervous system and osteoclasts stem from the monocyte phagocytic system, and their differentiation process depends on CSF1R. Therefore, a properly functioning CSF1R is required for the development and mainantence of the central nervous system, bone and teeth, as well as, immune system. It was also demonstrated that CSF1R is important for developing milk ducts, acinar structures, and both female and male reproductive tracts [23].
The CSF1R protein consists of 972 amino acids, including regulatory juxtamembrane domain (amino acids 542–574), tyrosine kinase domain (amino acids 582–910), and activation loop domain (amino acids 796–818) [23]. Both juxtamembrane and activation loop domains have regulatory functions, and phosphorylation thereof induces conformational changes and activates the tyrosine kinase domain [23]. In CSF1R-ALSP, more than 106 pathogenic mutations in CSF1R were identified [1]. Similar to CSF1R-ALSP, most of the identified CSF1R mutations in BANDDOS (n = 9/11) affected the tyrosine kinase domain; however, severe variants were much more common in the letter. In the CSF1R-ALSP, almost 80% of variants are missense mutations [3]. Although the genotype-phenotype relationships in CSF1R-ALSP are not well understood, patients with variants causing CSF1R protein truncation or nonsense-mediated mRNA decay were shown to have an earlier age of onset [1]. In BANDDOS, missense variants accounted for less than a third of all mutations. In one case with a missense variant outside the mutational “hot spot” (Pro132Leu), there was a protein-truncating variant (Gln481*) on the other allele leading to the CSF1R protein completely devoid of the tyrosine kinase domain. Furthermore, in BANDDOS, the splicing and nonsense variants leading to a severe loss of CSF1R protein function were the most common type of mutation.
To date, no identical mutation has been reported to occur in both disorders. In 2019 Oosterhof et al. [14] reported a patient with a bi-allelic Gly585_Lys619delinsAla mutation which had been previously reported in CSF1R-ALSP by Radamekers et al. [27]; however, the mutations were not identical on the coding level. Different substitution mutation at the same base pair position was reported in BANDDOS, c.2498 C > T [16], and in CSF1R-ALSP, c.2498 C > A [28, 29]. Therefore, we think the apparent “dichotomy” in mutations between CSF1R-ASLP in BANDDOS is due to the rarity of the disorders rather than different pathomechanisms. As the genetic testing becomes more readily available and CSF1R mutations are increasingly recognize worldwide, we predict the genetic landscapes of both disorders will soon be bridged [1, 3, 4, 30,31,32].
BANDDOS and CSF1R-ALSP share a genetic basis and a significant overlap of clinical, radiological, and pathological features. Therefore, both disorders are on the same continuum, albeit they differ in the severity of CSF1R mutations’ consequences and phenotypes. This opens windows of opportunity for applying already available therapy in CSF1R-ALSP in BANDDOS. Bone marrow transplant (BMT) was shown to be effective CSF1R-ALSP [33, 34]. Another clinical trial with a TREM2 agonist, which could rescue or compensate for CSF1R protein deficiency, is underway (NCT05677659) [1]. In addition, CSF1R protein was shown to play a role in other neurodegenerative diseases, and its inhibitors showed promising results in preclinical studies [35]. Therefore, further studies on CSF1R-related disorders may lead to a better understanding of these disorders and pave the way toward curative therapy in other neurological disorders.
The main limitation of the present study is the relatively low number of cases included into the analsysis. However, this is due to the rarity of the BANDDOS and the present paper presents the largest analysis on patients with BANDDOS to date. Secondly, the patients carried different CSF1R mutations, occasionally in the compund heterozygous state, and it was not possible to determine genotype-phenotype correlations. As the genetic testing with NGS is becoming more readily available, we speculate that more patients will be identified with variants of unknown significance within CSF1R gene, in isolation or in combination with other known CSF1R pathogenic mutations. Therefore, more research is needed to determine the pathophysiology of CSF1R-related neurodegeneration and genotype-phenotype correlations.
Conclusions
BANDDOS is an exceedingly rare disorder with a wide spectrum of the age of onset and disease severity; however, in most cases, it starts in the perinatal period or infancy and has a devastating course with congenital brain abnormalities, developmental delay, neurological deficits, osteopetrosis, and dysmorphic features. There is a significant overlap in the clinical, radiological, and neuropathological aspects between BANDDOS and CSF1R-ALSP. Both disorders share a genetic basis and are manifestations of CSF1R protein deficiency, albeit of different extents of disease severity. Therefore is a window of opportunity for translating treatment from CSF1R-ALSP to BANDDOS.
Data Availability
Data available on request from the corresponding author.
Abbreviations
- BANDDOS:
-
Brain abnormalities, neurodegeneration, and dysosteosclerosis
- CSF1R:
-
Colony-stimulating factor-1 receptor
- CSF1R-ALSP:
-
CSF1R-related leukoencephalopathy with axonal spheroids and pigmented glia
References
Papapetropoulos S, Pontius A, Finger E, Karrenbauer V, Lynch DS, Brennan M, et al. Adult-onset Leukoencephalopathy with Axonal Spheroids and pigmented glia: review of clinical manifestations as foundations for Therapeutic Development. Front Neurol. 2021;12:788168.
Konno T, Kasanuki K, Ikeuchi T, Dickson DW, Wszolek ZK. CSF1R-related leukoencephalopathy: a major player in primary microgliopathies. Neurology. 2018;91(24):1092–104.
Konno T, Yoshida K, Mizuno T, Kawarai T, Tada M, Nozaki H, et al. Clinical and genetic characterization of adult-onset leukoencephalopathy with axonal spheroids and pigmented glia associated with CSF1R mutation. Eur J Neurol. 2017;24(1):37–45.
Konno T, Yoshida K, Mizuta I, Mizuno T, Kawarai T, Tada M, et al. Diagnostic criteria for adult-onset leukoencephalopathy with axonal spheroids and pigmented glia due to CSF1R mutation. Eur J Neurol. 2018;25(1):142–7.
Wider C, Van Gerpen JA, DeArmond S, Shuster EA, Dickson DW, Wszolek ZK. Leukoencephalopathy with spheroids (HDLS) and pigmentary leukodystrophy (POLD): a single entity? Neurology. 2009;72(22):1953–9.
Marotti JD, Tobias S, Fratkin JD, Powers JM, Rhodes CH. Adult onset leukodystrophy with neuroaxonal spheroids and pigmented glia: report of a family, historical perspective, and review of the literature. Acta Neuropathol. 2004;107(6):481–8.
Lynch DS, Zhang WJ, Lakshmanan R, Kinsella JA, Uzun GA, Karbay M, et al. Analysis of mutations in AARS2 in a series of CSF1R-Negative patients with adult-onset Leukoencephalopathy with Axonal Spheroids and pigmented glia. JAMA Neurol. 2016;73(12):1433–9.
Sundal C, Carmona S, Yhr M, Almström O, Ljungberg M, Hardy J, et al. An AARS variant as the likely cause of swedish type hereditary diffuse leukoencephalopathy with spheroids. Acta Neuropathol Commun. 2019;7(1):188.
Dulski J, Koga S, Dickson DW, Wszolek ZK. Report of A Family with Adult-Onset Leukoencephalopathy with Axonal Spheroids and pigmented glia (ALSP) without mutations in CSF1R, AARS1 or AARS2. Mov Disord Clin Pract. 2023;10(2):307–12.
Guo L, Bertola DR, Takanohashi A, Saito A, Segawa Y, Yokota T, et al. Bi-allelic CSF1R mutations cause skeletal dysplasia of dysosteosclerosis-pyle Disease Spectrum and degenerative encephalopathy with Brain Malformation. Am J Hum Genet. 2019;104(5):925–35.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Monies D, Maddirevula S, Kurdi W, Alanazy MH, Alkhalidi H, Al-Owain M, et al. Autozygosity reveals recessive mutations and novel mechanisms in dominant genes: implications in variant interpretation. Genet Med. 2017;19(10):1144–50.
Oosterhof N, Chang IJ, Karimiani EG, Kuil LE, Jensen DM, Daza R, et al. Homozygous mutations in CSF1R cause a Pediatric-Onset Leukoencephalopathy and can result in congenital absence of Microglia. Am J Hum Genet. 2019;104(5):936–47.
Kındış E, Simsek-Kiper P, Koşukcu C, Taşkıran EZ, Göçmen R, Utine E, et al. Further expanding the mutational spectrum of brain abnormalities, neurodegeneration, and dysosteosclerosis: a rare disorder with neurologic regression and skeletal features. Am J Med Genet Part A. 2021;185(6):1888–96.
Tamhankar PM, Zhu B, Tamhankar VP, Mithbawkar S, Seabra L, Livingston JH, et al. A Novel Hypomorphic CSF1R Gene Mutation in the biallelic state leading to fatal Childhood Neurodegeneration. Neuropediatrics. 2020;51(4):302–6.
Helman G, Lajoie BR, Crawford J, Takanohashi A, Walkiewicz M, Dolzhenko E, et al. Genome sequencing in persistently unsolved white matter disorders. Ann Clin Transl Neurol. 2020;7(1):144–52.
Mickeviciute GC, Valiuskyte M, Plattén M, Wszolek ZK, Andersen O, Danylaité Karrenbauer V, et al. Neuroimaging phenotypes of CSF1R-related leukoencephalopathy: systematic review, meta-analysis, and imaging recommendations. J Intern Med. 2022;291(3):269–82.
Dulski J, Middlebrooks EH, Wszolek ZK. Novel Application of 7T MRI in CSF1R-Related Leukoencephalopathy. Neurology. 2022.
Sevin C, Barth M, Wilds A, Afriyie A, Walz M, Dillon A, et al. An international study of caregiver-reported burden and quality of life in metachromatic leukodystrophy. Orphanet J Rare Dis. 2022;17(1):329.
Ammann-Schnell L, Groeschel S, Kehrer C, Frölich S, Krägeloh-Mann I. The impact of severe rare chronic neurological disease in childhood on the quality of life of families-a study on MLD and PCH2. Orphanet J Rare Dis. 2021;16(1):211.
Corre CS, Grant N, Sadjadi R, Hayden D, Becker C, Gomery P, et al. Beyond gait and balance: urinary and bowel dysfunction in X-linked adrenoleukodystrophy. Orphanet J Rare Dis. 2021;16(1):14.
The UniProt C. UniProt: the Universal protein knowledgebase in 2023. Nucleic Acids Res. 2023;51(D1):D523–D31.
Marzan DE, Brügger-Verdon V, West BL, Liddelow S, Samanta J, Salzer JL. Activated microglia drive demyelination via CSF1R signaling. Glia. 2021;69(6):1583–604.
Chitu V, Biundo F, Shlager GGL, Park ES, Wang P, Gulinello ME, et al. Microglial homeostasis requires balanced CSF-1/CSF-2 receptor signaling. Cell Rep. 2020;30(9):3004–19e5.
Biundo F, Chitu V, Shlager GGL, Park ES, Gulinello ME, Saha K, et al. Microglial reduction of colony stimulating factor-1 receptor expression is sufficient to confer adult onset leukodystrophy. Glia. 2021;69(3):779–91.
Rademakers R, Baker M, Nicholson AM, Rutherford NJ, Finch N, Soto-Ortolaza A, et al. Mutations in the colony stimulating factor 1 receptor (CSF1R) gene cause hereditary diffuse leukoencephalopathy with spheroids. Nat Genet. 2011;44(2):200–5.
Ayrignac X, Carra-Dallière C, Codjia P, Mouzat K, Castelnovo G, Ellie E, et al. Evaluation of CSF1R-related adult onset leukoencephalopathy with axonal spheroids and pigmented glia diagnostic criteria. Eur J Neurol. 2022;29(1):329–34.
Codjia P, Ayrignac X, Mochel F, Mouzat K, Carra-Dalliere C, Castelnovo G, et al. Adult-onset Leukoencephalopathy with Axonal Spheroids and pigmented glia: an MRI study of 16 french cases. AJNR Am J Neuroradiol. 2018;39(9):1657–61.
Konno T, Miura T, Harriott AM, Mezaki N, Edwards ES, Rademakers R, et al. Partial loss of function of colony-stimulating factor 1 receptor in a patient with white matter abnormalities. Eur J Neurol. 2018;25(6):875–81.
Wszolek ZK. First polish case of CSF1R-related leukoencephalopathy. Neurol Neurochir Pol. 2021;55(3):239–40.
Żur-Wyrozumska K, Kaczmarska P, Mensah-Glanowska P. Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia associated with an A792D mutation in the CSF1R gene in a polish patient. Neurol Neurochir Pol. 2021;55(3):322–4.
Dulski J, Heckman MG, White LJ, Żur-Wyrozumska K, Lund TC, Wszolek ZK. Hematopoietic stem cell transplantation in CSF1R-Related Leukoencephalopathy: retrospective study on predictors of outcomes. Pharmaceutics. 2022;14(12).
Tipton PW, Kenney-Jung D, Rush BK, Middlebrooks EH, Nascene D, Singh B, et al. Treatment of CSF1R-Related Leukoencephalopathy: breaking New Ground. Mov Disord. 2021;36(12):2901–9.
Han J, Chitu V, Stanley ER, Wszolek ZK, Karrenbauer VD, Harris RA. Inhibition of colony stimulating factor-1 receptor (CSF-1R) as a potential therapeutic strategy for neurodegenerative diseases: opportunities and challenges. Cell Mol Life Sci. 2022;79(4):219.
Funding
JD is partially supported by the Polish National Agency for Academic Exchange (BPN/WAL/2022/1/00007/U/00001), and the Haworth Family Professorship in Neurodegenerative Diseases fund; ZKW is partially supported by the NIH/NIA and NIH/NINDS (1U19AG063911, FAIN: U19AG063911), Mayo Clinic Center for Regenerative Medicine, the gifts from the Donald G. and Jodi P. Heeringa Family, the Haworth Family Professorship in Neurodegenerative Diseases fund, and The Albertson Parkinson’s Research Foundation. He serves as PI or Co-PI on Biohaven Pharmaceuticals, Inc. (BHV4157-206) and Vigil Neuroscience, Inc. (VGL101-01.002, VGL101-01.201, PET tracer development protocol, Csf1r biomarker and repository project, and ultra-high field MRI in the diagnosis and management of CSF1R-related adult-onset leukoencephalopathy with axonal spheroids and pigmented glia) projects/grants. He serves as Co-PI of the Mayo Clinic APDA Center for Advanced Research and as an external advisory board member for the Vigil Neuroscience, Inc., and as a consultant on neurodegenerative medical research for Eli Lilli & Company.
Author information
Authors and Affiliations
Contributions
JD contributed to the project’s design, retrieved data from the literature, compiled and analyzed all the data, and took the lead in writing the manuscript. JS and MLC collected the data on the new cases and reviewed the manuscript. ZKW directed the project, reviewed, and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval statement
The information on the newly reported 3 patients was collected under the approval of the local Institutional Review Boards. The information on the remaining 17 patients was collected through the literature review, and IRB consent was not required.
Patient consent statement
Informed consent was obtained from the newly reported 3 cases.
Conflict of interest
The authors declare no conflict of interest.
Detailed disclosures
Jaroslaw Dulski:
Stock Ownership in medically-related fields: none.
Intellectual Property Rights: none.
Consultancies: none.
Expert Testimony: none.
Advisory Boards: none.
Employment: Medical University of Gdansk, Copernicus PL Ltd., MJ Jarosław Dulski.
Partnerships: none.
Contracts: none.
Honoraria: VM Media Ltd., Radosław Lipiński 90 Consulting, Ipsen.
Royalties: none.
Grants: Polish National Agency for Academic Exchange (BPN/WAL/2022/1/00007/U/00001), the Haworth Family Professorship in Neurodegenerative Diseases fund.
Other: none.
Josiane Souza.
Stock Ownership in medically-related fields: none.
Intellectual Property Rights: none.
Consultancies: none.
Expert Testimony: none.
Advisory Boards: none.
Employment: Hospital Pequeno Pricnipe; Medical University of PUCPR; Federal Medical Expert in the Ministry of Social Security; Curitiba, Paraná, Brazil.
Partnerships: none.
Contracts: none.
Honoraria: none.
Royalties: none.
Grants: none.
Other: none.
Mara Lúcia Santos.
Stock Ownership in medically-related fields: none.
Intellectual Property Rights: none.
Consultancies: none.
Expert Testimony: none.
Advisory Boards: none.
Employment: Hospital Pequeno Pricnipe;
Partnerships: none.
Contracts: none.
Honoraria: none.
Royalties: none.
Grants: none.
Other: none.
Zbigniew K. Wszolek: ZKW is partially supported by the NIH/NIA and NIH/NINDS (1U19AG063911, FAIN: U19AG063911), Mayo Clinic Center for Regenerative Medicine, the gifts from the Donald G. and Jodi P. Heeringa Family, the Haworth Family Professorship in Neurodegenerative Diseases fund, and The Albertson Parkinson’s Research Foundation. He serves as PI or Co-PI on Biohaven Pharmaceuticals, Inc. (BHV4157-206) and Vigil Neuroscience, Inc. (VGL101-01.002, VGL101-01.201, PET tracer development protocol, Csf1r biomarker and repository project, and ultra-high field MRI in the diagnosis and management of CSF1R-related adult-onset leukoencephalopathy with axonal spheroids and pigmented glia) projects/grants. He serves as Co-PI of the Mayo Clinic APDA Center for Advanced Research and as an external advisory board member for the Vigil Neuroscience, Inc., and as a consultant on neurodegenerative medical research for Eli Lilli & Company.
Consent for publication
was collected from the parents of the three newly reported Brazilian cases.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dulski, J., Souza, J., Santos, M.L. et al. Brain abnormalities, neurodegeneration, and dysosteosclerosis (BANDDOS): new cases, systematic literature review, and associations with CSF1R-ALSP. Orphanet J Rare Dis 18, 160 (2023). https://doi.org/10.1186/s13023-023-02772-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02772-9