Abstract
Background
The current study aimed to investigate the sleep quality of patients after valve replacement surgery due to infective endocarditis and identify risk factors for disturbed sleep post hospitalisation.
Methods
Eighty patients were assessed postoperatively using subjective scale measures, the Pittsburgh sleep quality index (PSQI) and the Epworth sleepiness scale, and an objective measure, actigraphy. Scale measures were assessed approximately 2 weeks and 6 months after surgery. Actigraphy monitoring was performed for 2 consecutive weeks during hospitalisation. Logistic regression was used to identify risk factors for disturbed sleep.
Results
The study population (n = 80) had an average age of 42.8 ± 14.2 years, and 67.5% were male. The median sleep efficiency was 85.3% in week 1 and 86.8% in week 2. The frequency of awakenings was significantly higher in week 1 (20.0 times vs. 19.3 times, p = 0.017). The scale measures showed significant improvement in sleep by 6 months after surgery compared to that during hospitalisation. Multivariable logistic regression analysis suggested that the possible risk factors for disturbed sleep 6 months after surgery included age (OR = 1.479, 95%CI 1.140–1.920) and a few parameters of early postoperative disturbed sleep quality (PSQI: OR = 2.921, 95%CI 1.431–5.963; sleep efficiency: OR = 0.402, 95%CI 0.206–0.783; and average duration of awakenings: OR = 0.006, 95%CI 0.000–0.827).
Conclusions
Disturbed sleep quality was witnessed in postoperative patients during hospitalisation and up to 6 months after surgery. Over time, the patients’ sleep quality improved significantly. Age and a few early postoperative sleep quality variables were risk factors for disturbed sleep 6 months after surgery.
Similar content being viewed by others
Background
Research of the impact of cardiac surgery on patients’ postoperative sleep quality started as early as the 1970s [1]. Emerging data have shown that poor sleep quality is commonly seen after cardiac surgery, especially coronary artery bypass grafting (CABG) [2,3,4,5,6,7,8,9]. Poor sleep quality may impact patients’ recovery rate, quality of life, morbidity, and even mortality [2,3,4,5, 7]. Redeker et al. summarised the possible intrinsic and extrinsic factors that may influence sleep quality during hospitalisation and the recovery period. These include a number of things: age, gender, illness, primary sleep disorders, environment, medical treatment, etc. [7].
Infective endocarditis (IE), also called bacterial endocarditis, refers to cardiac infection caused by microbial invasion of the endocardium and involves the valves in most of cases [10, 11]. Studies have shown that approximately half of the IE patients require heart valve replacement surgery. Also, early surgical treatment in patients with surgical indications improves the prognosis [12,13,14].
To date, the literature related to the sleep quality of patients who have undergone heart valve replacement surgery is very limited. Our previous study showed that 71 out of 117 patients (60.7%) experienced lower sleep efficiency (< 85%) after heart valve replacement surgery [15]. Therefore, in the present study, we aimed to evaluate patients’ sleep quality after heart valve replacement surgery using both subjective and objective measures and also to investigate the possible risk factors for disturbed sleep quality during the post-hospitalisation recovery period.
Methods
Study population and design
Patients who underwent heart valve replacement surgery due to IE between October 2016 and September 2018 in our hospital were included in the current study approximately 2 weeks after the surgery. These patients were admitted to the Department of Cardiac Surgery for surgical treatment first and then were transmitted to the cardiac intensive care unit (CICU) for critical postoperative care. Once a patient’s condition stabilised and was approved upon review by cardiac surgeons, they were transmitted to our ward for postoperative antibiotic and recovery treatment. The inclusion criteria for this study were: (1) aged at least 18 years old; and (2) being able to express thoughts and feelings. Patients who were delirious, unconscious or in coma were strictly excluded. It was made clear that participation in this study was completely voluntary and did not affect any further medical treatment for any participants or non-participants. The current study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital (No. GDREC2016222H (R2)) and was performed in accordance with the ‘Declaration of Helsinki’ and ethical standards. All patients provided a signed informed consent form.
In the current study, both subjective scale measures and objective actigraphy were employed to evaluate sleep quality. Subjective scale measures included the Pittsburgh sleep quality index (PSQI) and the Epworth sleeping scale (ESS), which were employed in the assessments for all included patients on their second day of being transmitted to our ward and also at 6 months after surgery. The objective method used in this study was actigraphy. All included patients were required to wear an Actigraph monitor on the wrist of their dominant side for a consecutive 2-week time period starting on the same day when they were assessed with the scale measures. During the same time period, the patients were guided to also keep a standard sleep diary for further reference.
Subjective sleep measures
The PSQI is a self-reported questionnaire which evaluates sleep quality and disturbance over a 1-month time period retrospectively. Consisting of 19 individual items, the questionnaire generates 7 aspect scores, which are summed to one global score. The aspects include: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of medication, and daytime dysfunction. Each component is weighted on a 0 to 3 interval scale, which gives a total score from 0 to 21. A lower score indicates better sleep quality [16,17,18]. A result of PSQI ≥ 8 points indicates poor sleep quality and disturbance, while a PSQI < 8 points represents good sleep quality [19].
The ESS is a very short questionnaire designed to evaluate daytime sleepiness. The questionnaire consists of 8 questions, each of which illustrates a situation that the subject may encounter in daily life. The subjects are required to rate the possibility of falling asleep for each item from 0 to 3, with 0 being very unlikely. Similar to the PSQI, an overall score is obtained by summing the scores for all 8 questions. A total score ≥ 9 is considered indicative of daytime sleepiness according to the latest published guideline in China [20].
Objective sleep measures
An Actigraph monitor is a wearable device which records a subject’s gross physical activity over a certain period of time. It was designed to collect information regarding the subject’s activity and stillness using a built-in accelerometer [21, 22]. The Actigraph GT3X + model (Actigraph, Pensacola, FL, USA) [23] was employed in this study to measure sleep latency, total duration of time in bed, total sleep time, nocturnal frequency of awakenings, duration of awakenings, and sleep efficiency. Sleep latency, or sleep onset latency, refers to the time required for the subject to transition from full wakefulness to sleep. Sleep efficiency was defined as the ratio of total sleep time to total time in bed as a percentage. A widely accepted normal range for sleep efficiency is above 85%.
After 2 weeks of monitoring, the Actigraphs were collected from patients together with their sleep diaries. ActiLife 6, which is a data analysis software package bundled with the Actigraph units, was used to download and analyse the data from the monitors. The function of ‘automatic interpretation and review’ was used for early-stage data processing. Based on the results from automatic interpretation, manual correction was conducted using the patients’ sleep diaries as references.
Statistical analysis
Statistical analyses were performed using SPSS (version 22.0, SPSS Inc., Chicago, IL, USA). Descriptive statistics are presented as mean and standard deviation (SD) or median and interquartile range (25th and 75th percentile) where appropriate. Numerical data are presented as quantity and percentage (%). Subjective scale results and actigraphy data at different times were compared using Wilcoxon signed-rank test and McNemar test where appropriate. Univariable logistic regression analysis was performed to detect the possible risk factors for disturbed sleep quality at 6 months after surgery (p < 0.05). These factors were then analysed using a multivariable logistic regression model to obtain the final results. A p value of < 0.05 was considered statistically significant.
Results
Basic demographic and clinical characteristics
At the end of the recruitment, 80 patients were included in the current study. The average age of the study population was 42.8 ± 14.2 years. Among these patients, 67.5% (n = 54) were male, while 32.5% (n = 26) were female. The average body mass index (BMI) was 20.4 ± 3.1 kg/m2.
In the current cohort, 66 patients (82.5%) were diagnosed with cardiac comorbidities before surgery. These included 26 (32.5%) cases with rheumatic heart disease, 21 (26.3%) cases with congenital heart disease, 16 (20.0%) cases with degenerative valve disease, and 3 cases (3.75%) with other conditions. Nineteen cases (23.75%) were complicated by embolism identified via radiological assessments, including 12 cases of cerebral infarction, 3 cases of splenic embolism, 3 cases of limb arterial embolism, and 1 case of renal artery embolism.
All these patients had undergone surgical treatment, which included 73 cases of single valve surgery and 7 cases of multi valve surgery. Single valve surgery included mitral valvuloplasty (MVP) in 21 cases, mitral valve replacement (MVR) in 19 cases, aortic valve replacement (AVR) in 31 cases, the Bentall procedure in 1 case, and tricuspid valvuloplasty (TVP) in 1 case. Multi valve surgery included double valve replacement (DVP) in 4 cases, MVR complicated with TVP in 2 cases, and AVR complicated with TVP in 1 case.
All the patients completed the sleep scale assessments during hospitalisation and at 6 months after surgery. Also, all the patients provided actigraphy data for 2 weeks during hospitalisation. There was no major concern about wearing the Actigraph monitor among the patients. No adverse event or withdrawal was observed in this study. All demographic and clinical characteristics of the study population are presented in Table 1.
Sleep quality assessment
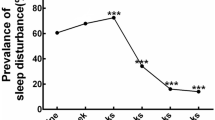
The PSQI and ESS scale evaluation was conducted in all 80 patients approximately 2 weeks after surgery during hospitalisation and at 6 months after surgery. Analysis of the scale results showed that the median scores of the two scales were 6.5 and 5 points, respectively, at 6 months after surgery. These values were significantly lower than the median scores obtained during hospitalisation, which were both 7 points (both p < 0.001). The number of cases with a PSQI of ≥ 8 and an ESS ≥ 9 at 6 months after surgery were 35 (43.75%) and 11 (13.80%), respectively. There were no significances in the number of patients with a PSQI of ≥ 8 and an ESS of ≥ 9 during hospitalization or at 6 months after surgery (p = 1.000, p = 0.093). Additional results regarding the scale measures are presented in Table 2 and Additional file 1: Fig. S1.
The actigraphy data showed that 43 out of 80 patients (53.75%) had a sleep efficiency greater than 85% during hospitalisation, and thus, for 37 patients (46.25%) the sleep efficiency was less than 85%. Generally, the median total time in bed was 492.7 min, the median total sleep time was 406.0 min, and the median sleep efficiency was 85.6%. The median sleep latency was 5.9 min, and the median frequency of nocturnal awakenings was 19.5 times. The median duration of awakenings was 73.5 min, with an average of 3.7 min each time.
Compared with the first week, significant differences were observed in sleep efficiency, sleep latency, total sleep time, frequency of awakenings and the number of cases with a sleep efficiency ≥ 85% in the second week. In week 2, sleep efficiency, the number of cases whose sleep efficiency was ≥ 85%, and total sleep time were significantly greater (p < 0.001; p = 0.046; p = 0.027) than those in week 1, while sleep latency and the frequency of awakenings were significantly lower (p < 0.001; p = 0.016). However, no significant differences were found for total time in bed (p = 0.100), duration of awakenings (p = 0.139), or average awakening duration (p = 0.881) between the first and second week. The actigraphy results are detailed in Table 3.
Risk factors for poor sleep quality
When processing data related to potential risk factors for poor sleep quality in the posthospitalisation period, univariable logistic regression analysis showed that age, PSQI score during hospitalisation, sleep efficiency, total sleep time, duration of awakenings, and frequency of awakenings may be relevant (all p < 0.05; Table 4). With these variables taken into consideration, multivariable logistic regression analysis revealed that only four were statistically significant, including age (odds ratio [OR] = 1.191, 95% confidence interval [CI] 1.082–1.311), early postoperative PSQI score (OR = 1.646, 95%CI 1.226–2.210), early postoperative sleep efficiency (OR = 0.607 95%CI 0.433–0.852), and average duration of awakenings (OR = 0.960, 95%CI 0.922–1.000). The complete results are presented in Table 5.
Discussion
To our knowledge, the current study is the first one designed to evaluate patients’ sleep quality after undergoing heart valve replacement surgery due to IE using both subjective and objective measures. The literature relevant to the topic of patients’ sleep quality after cardiac surgery is rather limited, and most studies to date have focused on CABG cases only [2, 4, 5, 8, 18, 24,25,26,27]. These studies investigated sleep quality in patients who underwent CABG surgery, either over a short-term or a longer period of up to 6 months. Use of a scale measure/questionnaire on site or via telephone interview was commonly seen in these studies. A few of them did however use both subjective and objective measures for evaluation [2, 6, 9, 18, 26, 27]. Sleep efficiency was one of the common interests shared in these studies, which was usually based on actigraphy measurement. Redeker et al. [6] reported that the mean sleep efficiency was 71% at 4 weeks and 74% at 8 weeks postoperatively. In the study by Yilmaz and Iskesen [9], it was revealed that the mean sleep efficiency was 66.55 ± 11.00% for male and 67.80 ± 13.72% for female at postoperative first week, and 94.01 ± 0.94% for males and 94.10 ± 1.21% for females at postoperative second month. Our previous study [15] showed that, of 117 patients with an average sleep efficiency of 80.81 ± 8.52%, 71 (60.7%) had sleep efficiency below 85%. The findings from the current study suggest that the overall postoperative sleep efficiency about 2 weeks after surgery during hospitalisation was 85.6%, which is consistent with the results obtained in the earlier studies.
Previous studies also attempted to include multiple evaluation time-points to monitor changes in sleep patterns after cardiac surgery and to discover when a significant improvement could be observed. Schaefer et al. [5] conducted telephone interviews with patients at 1 week, 1 month, 3 months and 6 months after surgery. According to the patients’ feedback, sleep disturbance occurred less often as more time passed. Redeker et al. [6] observed sleep disturbance rates of 64% at 4 weeks and 47% at 6 weeks after cardiac surgery. In another study by Redeker et al. sleep disturbance was observed to be higher at 1 week than at 4 weeks and at 8 weeks after surgery [26]. An even earlier publication by the same research team also supported the idea that more consolidated night sleep was seen in the late posthospitalisation period rather than early stage as 1 week after surgery [27]. In the present study, for short-term outcomes, sleep efficiency and a few parameters measured by actigraphy were significantly improved in week 2 when compared to week 1. For longer term outcomes, both the PSQI and ESS results were also significantly lower at 6 months after surgery than during hospitalisation. It is worth noting that disturbed sleep mainly manifested as frequent micro awakenings at early postoperative period. These results together with those of previous studies indicate that sleep quality is disturbed during the early postoperative period, but a trend of gradual recovery in sleep quality occurs over time after surgery.
Research findings have shown that disturbed sleep quality is a process affected by multiple, correlating factors [7]. It also has been well accepted that surgical trauma, anaesthesia, admission, etc., which all patients who undergo any surgery will experience, have a severe impact on patterns of sleep quality [28, 29]. Our results from the current study showed that age, early postoperative PSQI score, sleep efficiency, and average duration of awakenings are risk factors for poor sleep quality at 6 months after cardiac surgery for IE. The latter three variables are not singular but rather are affected by many other factors. A low early postoperative PSQI score may be related to all of the surgical elements mentioned above, and possibly a change in environment or postoperative complications, if they occur. Similar explanations can be applied to early postoperative sleep efficiency and average duration of awakenings as well. Therefore, a more precise way of analysing how severely these potential risk factors contribute to disturbed sleep quality will be a question for future studies.
Apart from using both subjective and objective measures for sleep quality, another advantage of the present study is that we chose the study time to be about 2 weeks after the surgery during hospitalisation. In this case, the effects of anaesthesia were almost completely eliminated. Also, because the patients had stabilised before being transmitted to our ward, any impact from early postoperative reactions, such as severe pain or inability to move, was also minimised.
This study also has limitations. We were unable to collect information for all patients’ preoperative sleep quality and psychological status. This flaw in the study design was due to the nature of our ward, which is allocated to stabilised postoperative patients only. Therefore, we are unable to draw the conclusion that sleep efficiency was worse postoperatively versus preoperatively, even though this was suggested by other studies [2, 27]. Secondly, this study was performed in patients after valve replacement for IE, which might reduce the heterogeneity and also limits the generalisability of the findings. Another limitation, which was discussed before, is the selection of potential risk factors for logistic regression analysis. Future studies are needed to expand our knowledge of how much these different risk factors contribute to the onset of disturbed sleep quality.
Conclusions
In the current study, we employed both subjective and objective measures to evaluate sleep quality in patients who underwent heart valve replacement surgery. Disturbed sleep quality was witnessed in early postoperative period and up to 6 months after surgery. However, an improvement in sleep quality was also observed over the recovery period. Age and a few early postoperative sleep quality variables, including PSQI score, sleep efficiency and average duration of awakenings, may indicate poor sleep quality in the later recovery period. Interventions to improve patients’ sleep during hospitalisation and posthospitalisation are in urgent need.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- IE:
-
Infective endocarditis
- CICU:
-
Cardiac intensive care unit
- PSQI:
-
The Pittsburgh sleep quality index
- ESS:
-
The Epworth sleeping scale
- SD:
-
Standard deviation
- PCT:
-
Procalcitonin
- WBC:
-
White blood cell
- Hb:
-
Haemoglobin
- Alb:
-
Albumin
- CRP:
-
C-reactive protein
- OR:
-
Odds ratio
References
Johns MW, Large AA, Masterton JP, Dudley HA. Sleep and delirium after open heart surgery. Br J Surg. 1974;61:377.
Yilmaz H, Iskesen I. Objective and subjective characteristics of sleep after coronary artery bypass graft surgery in the early period: a prospective study with healthy subjects. Heart Surg Forum. 2007;10:E16-20.
Tack BB, Gilliss CL. Nurse-monitored cardiac recovery: a description of the first 8 weeks. Heart Lung. 1990;19:491–9.
King KB, Parrinello KA. Patient perceptions of recovery from coronary artery bypass grafting after discharge from the hospital. Heart Lung. 1988;17:708–15.
Schaefer KM, Swavely D, Rothenberger C, Hess S, Williston D. Sleep disturbances post coronary artery bypass surgery. Prog Cardiovasc Nurs. 1996;11:5–14.
Redeker NS, Ruggiero JS, Hedges C. Sleep is related to physical function and emotional well-being after cardiac surgery. Nurs Res. 2004;53:154–62.
Redeker NS, Hedges C. Sleep during hospitalization and recovery after cardiac surgery. J Cardiovasc Nurs. 2002;17:56–68 (quiz 82–3).
Simpson T, Lee ER. Individual factors that influence sleep after cardiac surgery. Am J Crit Care. 1996;5:182–9 (quiz 90-1).
Yilmaz H, Iskesen I. Follow-up with objective and subjective tests of the sleep characteristics of patients after cardiac surgery. Circ J. 2007;71:1506–10.
European Society of Cardiology. The ESC guidelines for the management of infective endocarditis. Eur Heart J. 2015;2015(36):3036–7.
Prendergast BD, Tornos P. Surgery for infective endocarditis: Who and when? Circulation. 2010;121:1141–52.
Aksoy O, Sexton DJ, Wang A, Pappas PA, Kourany W, Chu V, et al. Early surgery in patients with infective endocarditis: a propensity score analysis. Clin Infect Dis. 2007;44:364–72.
Gálvez-Acebal J, Almendro-Delia M, Ruiz J, de Alarcón A, Martínez-Marcos FJ, Reguera JM, et al. Influence of early surgical treatment on the prognosis of left-sided infective endocarditis: a multicenter cohort study. In: Mayo clinic proceedings. Elsevier; 2014, pp. 1397–405.
Kang DH, Kim YJ, Kim SH, Sun BJ, Kim DH, Yun SC, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366:2466–73.
Hu X, Wei W, Lu F, Li X, Lin C, Huang D, et al. Correlation study of sleep efficiency with C-reactive protein and IL-6 in patients with infective endocarditis. S China J Cardiol. 2019;20:103–7.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh sleep quality index. J Psychosom Res. 1998;45:5–13.
Hedges C. Sleep, memory, and learning in off-pump coronary artery bypass patients. Res Nurs Health. 2005;28:462–73.
Liu XC, Tang MQ. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. 1996;29:29103–7.
Chinese Medical Association, Chinese Medical Journals Publishing House, of CS, General Practice, Sleep Related Breathing Disorders Group of Chinese Thoracic Society, Editorial Board of Chinese Journal of General Practitioners of Chinese Medical Association, et al. Guideline for primary care of adult obstructive sleep apnea (2018) (In Chinese). Zhonghua Quanke Yishi Zazhi. 2019;18:21–9.
Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18:288–302.
Natale V, Plazzi G, Martoni M. Actigraphy in the assessment of insomnia: a quantitative approach. Sleep. 2009;32:767–71.
Jean-Louis G, Kripke DF, Cole RJ, Assmus JD, Langer RD. Sleep detection with an accelerometer actigraph: comparisons with polysomnography. Physiol Behav. 2001;72:21–8.
Hedner J, Caidahl K, Sjöland H, Karlsson T, Herlitz J. Sleep habits and their association with mortality during 5-year follow-up after coronary artery bypass surgery. Acta cardiol. 2002;57:341–8.
Caruana N, McKinley S, Elliott R, Gholizadeh L. Sleep quality during and after cardiothoracic intensive care and psychological health during recovery. J Cardiovasc Nurs. 2018;33:E40–9.
Redeker NS, Ruggiero J, Hedges C. Patterns and predictors of sleep pattern disturbance after cardiac surgery. Res Nurs Health. 2004;27:217–24.
Redeker NS, Mason DJ, Wykpisz E, Glica B. Sleep patterns in women after coronary artery bypass surgery. Appl Nurs Res. 1996;9:115–22.
Rosenberg J. Sleep disturbances after non-cardiac surgery. Sleep Med Rev. 2001;5:129–37.
Madsen MT, Rosenberg J, Gögenur I. Actigraphy for measurement of sleep and sleep-wake rhythms in relation to surgery. J Clin Sleep Med. 2013;9:387–94.
Acknowledgements
None.
Funding
This work was supported by Science and Technology Planning Project of Guangdong Province (No. A2016057).
Author information
Authors and Affiliations
Contributions
All authors contributed to this study. Clinical work, data collection, and analysis were performed by XMH, WTW, DYH, CDL, FL, XML, HSL, ZHY, XPW, SBW, CLH. The manuscript was written by XMH and FJJ. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project reported here has been approved by the Ethics Committee of the Guangdong Provincial People's Hospital (No. GDREC2016222H (R2)). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants included in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
The PSQI and ESS scores at 2 weeks after surgery during hospitalisation and at 6 months after surgery.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, XM., Wei, WT., Huang, DY. et al. Sleep patterns and potential risk factors for disturbed sleep quality in patients after surgery for infective endocarditis. J Cardiothorac Surg 17, 121 (2022). https://doi.org/10.1186/s13019-022-01828-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01828-4