Abstract
Background
Cardiac Hibernomas are very rare benign tumors and usually remain asymptomatic. Neonatal cardiogenic shock due to cardiac tumors is extremely very rare. Until this date a few cases of cardiac hibernoma have been reported in the literature.
Transthoracic echocardiography help in the differential diagnosis, but the definitive diagnosis is histological. The management strategy is not clearly codified.
The Aim is to report and discuss the clinical features of a cardiac Hibernoma and review the relevant literature.
Case presentation
We describe a case of a 2-day-old Caucasian full-term male neonate admitted in neonate intensive care with cardiogenic shock, having fluid resuscitation and inotropic drugs. Ventilatory support was started immediately with the subsequent reestablishment of normal blood pressure. Then he was transferred to the echocardiography laboratory.
Transthoracic echocardiography showed two echogenic masses in the right atrium and right ventricle.
The masses were extended to the pulmonary trunk. Pulmonary artery flow measurements showed the presence of pulmonary and tricuspid obstruction.
Surgery was rapidly considered since the baby was hemodynamically unstable.
Intraoperative evaluation showed a mass embedded in the interventricular septum that occupy the right ventricular cavity and the right atrium. The tumor involved also the chordae of the tricuspid. Partial resection was done. Tricuspid valve repair was performed by construction of new chordae from the autologous pericardium. The specimen was sent for histopathological analysis. The baby died immediately after surgery.
Histological examination of the surgical specimen revealed clear multivacuolated cells filled with lipid droplets and granular intense eosinophilic cytoplasm which confirms the diagnosis of Hibernoma.
Conclusion
Cardiac Hibernomas are rare benign tumors. The prognosis and treatment strategy is closely dependent on the location, initial clinical presentation and possible complications. The prognosis can be unfavorable if the tumor was obstructive and infiltrate the myocardium.
Similar content being viewed by others
Background
Cardiogenic shock is a primary cardiac disorder characterized by a low cardiac output state of circulatory failure that results in end-organ hypoperfusion and tissue hypoxia. The most common etiologies include congenital heart diseases with reduced cardiac output and systemic hypotension, cardiac muscle disorders, dysrhythmias and metabolic conditions [1]. Cardiogenic shock in neonates is a rare medical emergency. Transthoracic echocardiography plays a pivotal role in the diagnosis and management of infants and children presenting with cardiogenic shock.
Hibernoma is a rare benign tumor originating from remnants of fetal brown adipose tissue.
It can be found in numerous locations in the body, especially in the thigh, shoulder, and upper back [2]. Intracardiac location have been rarely described.
Cardiac Hibernomas usually remain asymptomatic, but they can cause arrhythmia, embolisation, pericardial effusion, or blood flow obstruction.
We report a case of a 2-day-old Caucasian full-term male neonate who was admitted in neonate intensive care with cardiogenic shock due to an obstructive a cardiac Hibernoma.
Case report
A 2-day-old Caucasian full-term male neonate was admitted in neonate intensive care with shock. There were no familial antecedents, no consanguinity and no infection or inflammation during pregnancy. However the tumor was suspected in fetal echocardiography.
At observation, he presented poor general status with marked hypotonia, immeasurable blood pressure, tachypnoea and retractions. Percutaneous oxygen saturation was 85% on room air. He had a mottled blue and white skin with prolonged capillary refill time (above 3 s). Cardiac auscultation showed rhythmic heart sounds without murmurs. On pulmonary auscultation, he had a symmetric entrance of air and without rales.
He was intubated and ventilated with conventional mechanical ventilation. We started intravenous fluid resuscitation, inotropic drugs (dobutamine), with the subsequent reestablishment of normal blood pressure. He was transferred to the echocardiography laboratory.
Transthoracic echocardiography showed two echogenic masses. The first one, was large, poly-lobed, and mobile mass in the right ventricle, which measured 37 mm × 29 mm. The mass was embedded in the interventricular septum (IVS) and right ventricle (RV) wall (Fig. 1). This mass was extended to the pulmonary trunk (Fig. 2). Pulmonary artery flow measurements showed the presence of pulmonary and tricuspid obstruction. The peak pressure gradient between the right ventricle and the pulmonary trunk was 60 mmHg.
The second one, was a large mass measuring 28 mm × 22 mm in the right atrium. Color Doppler flow imaging did not detect any flow signal inside the mass.
To further characterize the mass, cardiovascular Magnetic resonance imaging was indicated, however it was not performed because of unavailability of this exam in emergency. Surgery was rapidly considered since the baby was hemodynamically unstable. He was transferred operating room for emergency surgery the next day.
Through median sternotomy and systemic heparinization, the baby was cannulated for cardiopulmonary bypass employing direct bi-caval venous cannulation. After cardioplegic arrest a longitudinal right atriotomy was performed. During surgery, a mass was found to be embedded in the IVS, and to occupy the RV cavity and the right atrium (Fig. 3). The tumor involved also the chordae of the tricuspid. That is why, it was impossible to remove completely the tumor. Partial resection was done. Tricuspid valve repair was performed by construction of new chordae from the autologous pericardium. The baby died immediately after surgery before doing the echocardiography. This evolution is probably due of the right ventricle dysfunction. In fact the tumor was infiltrated the right ventricle and the tricuspid valve. The partial tumor resection of the tumors was insufficient to improve the right ventricle and the restoration of the hemodynamic state. The specimen was sent for histopathological analysis.
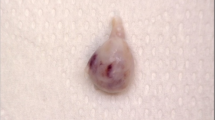
Histological examination of the surgical specimen revealed clear multivacuolated cells filled with lipid droplets and granular intense eosinophilic cytoplasm which confirms the diagnosis of Hibernoma (Figs. 4 and 5). The genetic analysis was not done.
Discussion
Primary cardiac tumors in newborns are extremely rare and more than 90% of them are benign. They occur approximately in 1 every 100,000 live births [2]. The most frequent tumors of the heart observed in pediatric patients are rhabdomyomas, fibromas and lipomas. Hibernoma is a rare, benign soft tissue tumor of brown fat origin. This is not genetic links. Less than 300 cases have been reported in the literature [3]. Its genesis is thought to be the result of nonspecific trauma to the brown fat cells, such as inflammation or infection. Intracardiac Hibernomas are very rare location and few cases were reported in the literature. Typical location described is the endocardium of the right atrium.
The first case of cardiac Hibernoma reported in the literature was a case of 64-year-old patient with a very rare cardiac Hibernoma located in the right atrium. Transesophageal echocardiography and computed tomography have been shown to be useful for differentiating between benign and malignant tumors. The tumor was excised with the use of cardiopulmonary bypass surgery. Histology confirmed diagnosis of a benign cardiac Hibernoma [4].
Luca Di Tommaso et al. reported a case of 51-year-old woman, with no clinical history, presented for an acute haemoptysis. A computerized tomography (CT) scan revealed a nodule of the lower left pulmonary lobe and a 4-cm lesion involving almost completely the interatrial septum and extending into the right atrium near the superior cava vein. A Magnetic Nuclear Resonance (MNR) excluded any relationship with the superior cava vein. The patient underwent surgery. The definitive histopathology diagnostic was cardiac Hibernoma [5].
Rebeca Mata-Caballero et al. reported a case of 73 -year-old woman, asymptomatic with previous history of breast cancer in complete remission. The tumour was a casual finding on an fluoro-D-glucose integrated with computed tomography (FDG PET/CT). Transthoracic, transesophageal echocardiography showed a mass in the right atrium and aroud the vena cava. Cardiac magnetic resonance help in the differential diagnosis of benign tumor. The mass was excised, allowing the definitive histological diagnosis of benign cardiac Hibernoma. The subsequent outcome was excellent [6].
A case of intrapericardial Hibernoma associated with constrictive pericarditis was also reported. The authors present the case of a 20-year-old male who underwent an operation for the treatment of constrictive pericarditis, in which an intrapericardial sessile lesion over the diaphragmatic surface of pericardial sac was incidentally discovered. The tumor was excised and diagnosed as Hibernoma. No recurrence was evident two years after the procedure [7].
The clinical symptoms vary largely depending on their size, location and mobility of the tumor. It ranges from incidental discovery on imaging tests indicated for other reasons to life-threatening presentations such as cardiac tamponade, arrhythmia, systemic embolization and obstruction. Obstructive symptoms include congestive heart failure, syncope and rarely cardiogenic shock.
To our knowledge, this is the first case report of neonatal cardiac Hibernoma. The fatal issue is due to its large size, the infiltrative and obstruction nature.
In our case the cardiogenic shock was attributed to the obstruction of the right ventricle outflow tract that reduced the cardiac output significantly.
Transthoracic echocardiography (TTE) remains the preferred tool for screening and diagnosing intra cardiac tumors. It allows to specify accurate location, mobility and extent of the tumor. Echocardiography typically reveals a homogeneous, hyperechoic mass, but these findings are not diagnostic of this lipomatous tumor [8].
Magnetic resonance imaging (MRI) and cardiac computerized tomography scan are useful modalities for diagnosis and characterization of intracardiac masses, studying the limits, basis of implantation, and relation ship to surrounding structures.
Cardiac MRI provides the possibility of diagnosing the nature of the tumor by studying its signal features. The specific sign being the complete signal loss of the mass on fat suppression sequence. It is considered to be the diagnostic gold standard [9].
The need for sedation and anesthesia for pediatric population, limits its use in cases of severe symptoms and hemodynamic instability. Such as the case of our patient who was deemed too unstable to undergo sedation and transthoracic echocardiography was sufficient to indicate intervention.
No clear guidelines have been established due to the low incidence of cardiac Hibernoma, but there is consensus that surgical resection of the cardiac tumor is the optimal method of treatment in symptomatic patients. Conservative management may be implemented for asymptomatic patient and prophylactic resection should also be considered [7].
In our case, surgery is indicated and complete resection of the tumor is recommended, but the overgrowth and myocardial infiltration has led to an unsuccessful complete resection.
Long term recurrence of cardiac Hibernoma after surgical resection is possible. Incomplete removal due to diffuse infiltration in the myocardium seems to be the contributing factor for recurrence.
Conclusion
Cardiac Hibernomas are very rare benign tumors that usually remain asymptomatic. However the prognosis can be unfavorable if the tumor was obstructive and infiltrate the myocardium.
Availability of data and materials
The data that support the findings of this report are available from cardiology department in Sahloul university Hospital. The author can make it available upon reasonable request.
Abbreviations
- CT:
-
Computerized tomography
- FDG:
-
fluoro-D-glucose
- LPA:
-
Left pulmonary artery
- LV:
-
left ventricle
- IVS:
-
Interventricular septum
- MNR:
-
Magnetic Nuclear Resonance
- MRI:
-
Magnetic resonance imaging
- PA:
-
Pulmonary artery
- RPA:
-
Right pulmonary artery
- RV:
-
Right ventricle
- RVOT:
-
Right ventricle outflow tract
- TTE:
-
Transthoracic echocardiography
References
Albrecht GT. Cardiogenic shock in the neonate. Indian J Pediatr. 1993;60(3):381–91. https://doi.org/10.1007/BF02751199.
Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics. 2004;24(5):1433–66. https://doi.org/10.1148/rg.245045120.
Isaacs H Jr. Fetal and neonatal cardiac tumors. Pediatr Cardiol. 2004;25(3):252–273. https://doi.org/10.1007/s00246-003-0590-4.
Strecker T, Reimann A, Voigt JU, Papadopoulos T. A very rare cardiac hibernoma in the right atrium: a case report. Heart Surg Forum. 2006;9(3):E623–E625. https://doi.org/10.1532/HSF98.2005-1185.
Di Tommaso L, Chiesa G, Arena V, Guanella G, Galli C, Roncalli M. Cardiac hibernoma: a case report. Histopathology. 2012;61(5):985–987. https://doi.org/10.1111/j.1365-2559.2012.04264.x.
Mata-Caballero R, Saavedra-Falero J, López-Pais J, Molina-Blázquez L, María T, Vela A, et al. Hibernoma cardiaco en la aurícula derecha y alrededor de la vena cava superior. Reporte de un caso. Cirugía Cardiovasc. 2017;24(5):314–6. https://doi.org/10.1016/j.circv.2016.11.004.
Ucak A, Inan K, Onan B, Yilmaz AT. Resection of intrapericardial hibernoma associated with constrictive pericarditis. Interact CardioVasc Thoracic Surg. 2009;9(4):717–9. https://doi.org/10.1510/icvts.2009.209247.
Braunwald E. Heart disease: a textbook of cardiovascular medicine. 6th ed. Philadelphia: WB Saunders Co; 2001.
Butany J, Nair V, Naseemuddin A, Nair GM, Catton C, Yau T. Cardiac tumours: diagnosis and management. Lancet Oncol. 2005;6(4):219–228. https://doi.org/10.1016/S1470-2045(05)70093-0.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Clear consent has been given for this publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gribaa, R., Kacem, M., Ouannes, S. et al. Neonatal cardiogenic shock revealing obstructive cardiac Hibernoma: case report. J Cardiothorac Surg 16, 222 (2021). https://doi.org/10.1186/s13019-021-01582-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01582-z