Abstract
Purpose
To observe the effect of the forearm rotation function reconstruction with an external fixator in treating congenital radioulnar synostosis.
Methods
From July 2017 to July 2023, 6 patients (9 sides) with congenital radioulnar synostosis who underwent reconstruction of the forearm rotation with the external fixator were retrospectively analyzed. The extent of flexion and rotation, the Modified An and Morrey functional rating index, and the grade according to the classification system proposed by Failla et al. were compared before and after the operation.
Results
All patients were followed up for an average of 12.00 (8.00, 38.50) months. The average range of rotation, the Modified An and Morrey functional rating index increased from 0°, 64.56 ± 1.33 points to 85.00° ± 25.86°, 83.71 ± 5.50 points, respectively. The differences were statistically significant (t = 9.86, P < 0.01, t = 11.20, P < 0.01). There was no significant difference in forearm flexion before and after the operation (Z = 1.34, P = 0.18). According to the Failla classification system, 2 forearms were classified as poor preoperatively, 6 as fair and 1 as good. 2 forearms were assessed as excellent, 6 as good and 1 as fair during the last follow-up.
Conclusion
Reconstruction of the forearm rotation function with an external fixator is safe and effective for treating congenital radioulnar synostosis. This technique can restore the partial rotational function of the forearm.
Similar content being viewed by others
Introduction
Congenital radioulnar synostosis (CRUS) is a rare congenital malformation with an incidence of approximately 0.2‰. It is characterized by a fixed pronation deformity and limited supination function of the forearm [1]. People who suffer from the malformation usually have trouble holding objects using their palms, dining with their hands holding bowls, and cleaning the perineum [2, 3].
Most studies suggest that surgery is indicated when the pronation deformity of the forearm is more than 60° [4, 5]. Surgical treatment mainly includes various rotational osteotomies and mobilization procedures [6]. Derotational osteotomy is currently an accepted treatment for synostosis, and it is easy to perform to some extent. However, it cannot restore forearm rotation. Mobilization can restore the partial rotational function of the forearm and is theoretically an ideal surgical method. However, requiring microvascular techniques and easy-to-get recurrent synostosis make it difficult to achieve wide acceptance [7]. Due to the complexity of CRUS deformities, the recovery of the rotational function is not satisfactory and the radial head may dislocate again after the operation [8, 9]. How to prevent the recurrence of ankylosis and gain satisfactory supination and pronation function without microsurgical technique is still a challenge [10,11,12]. Given these issues, we improved the mobilization procedure and devised reconstruction of the forearm rotation function with the external fixator for the deformity, which can gain a good rotation arc without microsurgical technique. Compared with previous mobilization procedures, our modified procedure is technically easier, takes less time, and has a satisfactory surgical result.
In this study, we report the results of this surgical method in 6 patients (9 forearms) and examine its effectiveness in the management of CRUS.
Materials and methods
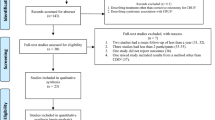
This was a series of retrospective cases from a single center. We treated 10 CRUS patients who underwent reconstruction of the forearm rotation function at our institute from July 2017 to July 2023. Except for 4 cases whose radial osteotomy sites were stabilized with a locking plate and screw system, the other 6 patients (9 forearms) all met the inclusion criteria and were included. The inclusion criteria were the children who were diagnosed with CRUS and underwent reconstruction of the forearm rotation function with an external fixator. The exclusion criteria were as follows: 1. Presence of other congenital malformations, 2. Previous history of surgery or trauma to the ipsilateral forearm, 3. Postoperative follow-up data were lost. There were 4 males and 1 female. The average age was 2.6 (2.4,7.4) years, and the average degree of forearm pronation before the operation was 65.00° ± 17.14°. (Table 1).
Surgical technique
A tourniquet was applied to the involved limb while general anesthesia and brachial plexus block anesthesia were administered. A curved incision was made on the lateral aspect of the proximal forearm, approximately 5 cm long, with the ends of the incision in the plane of the ulna and the apex of the curve on the radial side of the forearm. The skin was incised and separated from the subcutaneous fat layer to the level of both ends of the incision. Next, the subcutaneous fat layer was incised, and the deep fascia was separated from the subcutaneous fat layer to the level of both ends of the incision, creating a tongue-shaped fat flap with the tip on the ulnar side. (Fig. 1) Blood exudation could be observed from the inside of the fat flap after the tourniquet was loosened. After the ulnar-radial fusion zone was exposed, a rongeur and grinding drill were used to resect the synostosis. Then, the forearm was rotated, and the forearm was visible to restore rotational function. After the fusion area was divided, the trauma area was covered with bone wax. Next, transverse osteotomy in the upper middle third of the ulna was conducted. Using the distal ulna as the axis of rotation, the forearm was rotated to half of the maximal supination position for the first time, and the ulnar deformity was rectified. For ulna fixation, a single Kirschner pin was inserted through the olecranon. A 0.5–1 cm shortening osteotomy of the radius was performed above the proximal and pronator teres muscles. Extreme supination rotation of the forearm was achieved at this time and the forearm was preserved in this position. The radial head was then reset, restoring the proximal radial line of force and the humero-radial alignment as much as possible. Two Schanz screws were inserted into both ends of the osteotomy site of the ulna and radius and then attached to the carbon fiber rods. The forearm was temporarily fixed with the external fixator in the maximum supination position. Under the C arm’s observation, the humerus-radius alignment was checked by flexing and extending the elbow joint when the forearm was in pronation, neutral, and supination separately. If there was an obvious dislocation of the radial head in the process, the radial head reset was carried out again until the humerus-radius alignment of the forearm was satisfactory in each direction of the activity, and finally, the external fixator was tightened (Fig. 2). The intercepted bone block was implanted in the radial osteotomy area. After wound irrigation and hemostasis, the tipped tongue-shaped fat flap was pulled to the palmar side through the ulna and radius, completely covering the region of ulnar trauma. Nonabsorbable sutures were used to suture the distal end of the fat flap to the palmar periosteum of the ulna and the surrounding soft tissues. The skin was sutured, drainage strips were placed, and sterile dressings were applied.
A Location of arc incision. B The skin was incised and separated from the subcutaneous fat layer, creating a tongue-shaped fat flap with a 5-cm tip on the ulnar side. C and D The inside and outside conditions of the pedicled fat flap with the tourniquet. E Blood exudation was visible on the pedicled fat flap after the tourniquet was released. The thickness of the skin flap is about 3-5 mm
Surgical schematic diagram simulated with Mimics Medical 21.0 software (Materialize, Belgium) A Bone surface model of CRUS before surgery. B Resect the synostosis. C Correct the ulnar deformity and rotate the forearm to half of the maximal supination position for the first time, a single Kirschner pin was inserted through the olecranon for ulna fixation. D A 1-cm shortening osteotomy of the radius. E Reset the radial head as much as possible and rotate the forearm to the maximal supination position at the second time. F and G Fixation by the external fixator
Postoperative care
The affected limb was elevated, and forearm swelling and the peripheral circulation of the fingers of the involved limb were monitored. Drainage strips were removed on the first day after surgery, and X-rays were reviewed one week after surgery to determine whether the alignment of the brachioradialis was fine (Fig. 3). One week after surgery, the external fixator was released during the day, and activities involving mild passive mobility and active motion were initiated right away. We just took out the rod during the procedure, which joined the ulna and radius collectively and kept the forearm in its most supinated posture. The ulna and radius osteotomy sites remained steadily fixed. The forearm was at the maximal supination position when the external fixator was tightened at night (Fig. 4). The external fixator and Kirschner's pin were removed after X-ray confirmation of bone healing at the osteotomy site approximately 3 months after surgery.
Evaluation of efficacy
Before surgery, the degree of pronation was measured. The angle between the longitudinal axis of the humerus and the line connecting the radial and ulnar styloid processes was measured with a goniometer with the patient's elbow held fixed to the side of the chest and the forearm at 90 degrees of flexion [5]. Postoperatively, the same method was used to measure the maximum pronation and supination degree, and the forearm rotational range of motion was calculated. Three examiners in our team were involved in the assessment of the patients before and after surgery. Before evaluating the patients, ROM measurements were standardized among all the examiners. The Modified An and Morrey functional rating index [13] were used to score the preoperative and postoperative elbow range of motion, muscle strength, joint stability, and pain. Preoperative and postoperative forearm functions were assessed using the classification system proposed by Failla et al. [14, 15].
Statistical analysis
SPSS Statistics 26.0 was used for the data analysis. Shapiro–Wilk test was applied to assess the normality of measurement data. Normally distributed data were expressed as \(\overline{x }\pm s\), and comparisons before and after surgery were analyzed using paired t-tests; nonnormally distributed data were expressed as M(P25, P75), and comparisons before and after treatment were analyzed using Wilcoxon signed-rank tests. Differences between pre- and postoperative Failla classification grades were also examined with the Wilcoxon signed-rank test. P < 0.05 was regarded as statistically significant.
Results
No radial nerve palsy occurred in any of the patients. One patient (one forearm) suffered a nail tract infection and recovered after appropriate therapy. Bone union was achieved, the humerus-radius relationship was well aligned, there was no recurrent synostosis, and the forearms could perform active motion of pronation and supination. The external fixator and Kirschner pin were removed (11.89 ± 0.78) weeks after surgery. Six patients were followed up for a mean of 12.0(8.00,41.00) months. The mean preoperative pronation angle was 65.00° ± 17.14°. At the last follow-up, the mean maximal pronation arc, maximal supination arc, and arc of the forearm rotation were 50.00° ± 18.51°, 35.00° ± 13.69°, and 85.00° ± 25.86°, respectively. The mean forearm rotational mobility, and the Modified An and Morrey functional rating index before and after surgery increased from 0°, (64.56 ± 1.33) to 85.00° ± 25.86°, (83.71 ± 5.50) respectively, and the differences were statistically significant (t = 9.86, P < 0.01, t = 11.20, P < 0.01). (Table 1 and Fig. 5) The difference in the change in elbow flexion mobility before and after surgery was not statistically significant (Z = 1.34, P = 0.18). According to the Failla classification system, 2 forearms were classified as poor preoperatively, 6 as fair and 1 as good. Two forearms were assessed as excellent,6 as good and 1 as fair during the last follow-up. (Tables 2, 3).
A 4-year-old boy who had proximal radioulnar synostosis in his left forearm. (Cleary-Omer III types). A and B Preoperative anteroposterior and lateral X-ray image showing left proximal radioulnar synostosis. C and D His left forearm was fixed at a pronation angle of roughly 70°. E and F 3 years after the operation, X-rays showing no recurrent ankylosis. G and H 3 years after the operation, the active pronation of the left forearm achieved 75 degrees and the active supination achieved 25 degrees
Discussion
Congenital radioulnar synostosis is a relatively rare congenital deformity. There is no standard indication for CRUS surgery [14, 16]. Simmons et al. [4] concluded that pronation of more than 60° was a clear indication for surgery. Sakamoto et al. [12] reported that the indication for surgery should be based on the patient's ability to perform daily activities, and surgery was not required if the patient could perform daily activities with the aid of shoulder or wrist. Jia et al. [17] reported that surgery should be performed after the proximal radial epiphysis is closed (approximately 7 years of age), which could prevent damage to the epiphyseal plate and avoid adverse effects on bone union. We found that the older the patients were, the more severe the bony malformations and soft tissue abnormalities of the forearm were, which might have limited the postoperative mobility of the rotation. After the age of 2, the children could play and interact with others and perform different activities, which was favorable for postoperative rehabilitation training. Therefore, we suggest that surgery should be performed after the age of 2 years.
Currently, mobility techniques and various rotational osteotomies are the primary therapeutic options for CRUS. Rotational osteotomies are the most commonly used treatment modality for CRUS, with the advantage of relative simplicity of operation and the disadvantage of placing the forearm in a functional position without allowing for active rotation of the forearm. Although mobilization procedures are thought to be the ideal surgical procedure because they rebuild the brachioradial and upper radioulnar joints and partially restore forearm rotation function, they have not gained widespread acceptance due to their complexity, the need for microsurgical techniques, and the high incidence of recurrent synostosis [10].
Early findings in the literature documented the use of soft tissue such as fat or muscle to fill the separated zone, with postoperative recurrence of bony bridging and the forearm not gaining rotational motion [18]. Until Kanaya adjusted the approach using free vascularized fascia-fat graf to fill in the space between the divided radius and ulna and then reset the radial head by osteotomy at the proximal radius, the outcomes were satisfactory [19]. However, it has been reported in the literature that in addition to the proximal radioulnar synostosis, patients with CRUS also suffer from ulnar and radial deformities, soft tissue abnormalities and a high rate of redislocation of the radial head, so the results of fusion zone separation and reconstruction are still not perfect and the restoration of forearm rotational function is still a challenge for orthopedic surgeons [9, 20, 21].
Based on comprehensive domestic and international experience, the present study improved fusion zone separation and reconstruction in many aspects and described the reconstruction of the forearm rotation function with an external fixator, which significantly improved the forearm rotational function. First, this technique uses subcutaneous free-fat flaps with tips to fill the fusion area without microsurgical techniques. With a good blood supply itself and adequate volume to cover the separated synostosis, the fat flap has a good survival result and prevents recurrence successfully. Second, osteotomy at both the ulna and radius is significant. Importantly, osteotomy of the upper 1/3 of the ulna not only corrects the ulnar deformity but also leads to a more complete improvement in forearm rotation. The radial osteotomy is located above the pronator teres and pronator teres, providing an anatomical basis for postoperative forearm rotation. The radial shortening osteotomy lengthens the blood vessels, nerves, and muscles to some degree to avoid excessive tension. Third, the advantages of using an external fixator to fix the end of the osteotomy are outstanding. During the procedure, more than one adjustment to the radial head can be made if needed, as the external fixator serves as a temporary fixator. Throughout the procedure, the radial line of force in different positions of the forearm can be evaluated. If the radial head dislocates, the external fixator can be released, and the radial head can be realigned again. A good reduction in the radial head may contribute to a more desirable forearm rotation function [12]. In addition, the color of the skin and the swelling of the forearm can be visually observed. Compartment syndrome is one of the most common complications in the treatment of CRUS [10, 22], because the forearm has no cover with an external fixator, it can be quickly identified and treated if compartment syndrome occurs. This technique is less invasive. Compared with internal fixation, the external fixator can avoid extensive exposure, reduce the chance of vascular nerve injury, and does not require the original incision to remove the implants in the secondary surgery. This technique also has less impact on elbow flexion and extension function. In a report by Murase et al. [23], all four of their children developed impaired elbow extension after fixation with a plaster cast, whereas the use of an external fixator with unrestricted elbow motion prevented the occurrence of joint stiffness. However, the external fixator has the possibility of causing nail tract infections [7], which occurred in one patient in this study Pin site infections are a major side effect of external fixation; literature reports occurrences ranging from 3 to 80%. The development of infection is related to the purpose of application, surgical method, rate of pin site loosening, pin material, and pin-site care [24]. Two weeks following surgery, one patient in our study experienced pain, little discharge, and skin redness. We gave the patient instructions to take oral antibiotics and cleaned the pin site twice a day using hydrogen peroxide and saline. Following the 5-day matching treatment, the patient made a full recovery. It is advised to maintain the pin site dry and clean using antiseptic materials such saline, iodide solution, ointment, cream, and sterile gauzes to prevent [25].
Our article's primary weaknesses are its short follow-up period and the comparatively modest patient enrollment. Even though it is challenging to do because of the disease's rarity and the research' usually single-center design, long-term follow-up is essential. With an average follow-up of ten years, Kanaya et al. observed a decrease in supination angle; nevertheless, the cause is uncertain [22]. Therefore, longer-term follow-up research and a larger sample of clinical studies are required to evaluate the effectiveness of our technique. In our cases, a shortening osteotomy was performed at the proximal part of the radius. While some scholars reported the shortening osteotomy of the middle shaft with posterior radial head dislocation has improved the rotation arc significantly [12]. Therefore, it will be very meaningful to design and simulate the surgical osteotomy process with 3D software to determine the optimal osteotomy position in the future.
Conclusion
Reconstruction of the forearm rotation function with an external fixator has the advantages of easy operation, effective results, and fewer complications, and it can restore partial rotational function of the forearm. This technique might be a valuable addition to resolving deformities on CRUS as orthopedic technology continues to develop. Its effect needs to be confirmed in a larger patient population and a longer time follow-up.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Cleary JE, Omer GE Jr. Congenital proximal radio-ulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am. 1985;67(4):539–45.
Kasten P, Rettig O, Loew M, Wolf S, Raiss P. Three-dimensional motion analysis of compensatory movements in patients with radioulnar synostosis performing activities of daily living. J Orthop Sci. 2009;14(3):307–12.
Satake H, Kanauchi Y, Kashiwa H, Ishigaki D, Takahara M, Takagi M. Long-term results after simple rotational osteotomy of the radius shaft for congenital radioulnar synostosis. J Shoulder Elbow Surg. 2018;27(8):1373–9.
Simmons BP, Southmayd WW, Riseborough EJ. Congenital radioulnar synostosis. J Hand Surg Am. 1983;8(6):829–38.
Ogino T, Hikino K. Congenital radio-ulnar synostosis: compensatory rotation around the wrist and rotation osteotomy. J Hand Surg Br. 1987;12(2):173–8.
Rutkowski PT, Samora JB. Congenital radioulnar synostosis. J Am Acad Orthop Surg. 2021;29(13):563–70.
Shingade VU, Shingade RV, Ughade SN. Results of single-staged rotational osteotomy in a child with congenital proximal radioulnar synostosis: subjective and objective evaluation. J Pediatr Orthop. 2014;34(1):63–9.
Hung NN. Derotational osteotomy of the proximal radius and the distal ulna for congenital radioulnar synostosis. J Child Orthop. 2008;2(6):481–9.
Kanaya F, Kinjo M, Nakasone M, Okubo H, Miyagi W, Nishida K. Preoperative radius head dislocation affects forearm rotation after mobilization of congenital radioulnar synostosis. J Orthop Sci. 2023;28(6):1285–90.
Kanaya F, Ibaraki K. Mobilization of a congenital proximal radioulnar synostosis with use of a free vascularized fascio-fat graft. J Bone Joint Surg Am. 1998;80(8):1186–92.
Chen CL, Kao HK, Chen CC, Chen HC. Long-term follow-up of microvascular free tissue transfer for mobilization of congenital radioulnar synostosis. J Plast Reconstr Aesthet Surg. 2012;65(12):e363–5.
Sakamoto S, Doi K, Hattori Y, Dodakundi C, Montales T. Modified osteotomy (Kanaya’s procedure) for congenital proximal radioulnar synostosis with posterior dislocation of radial head. J Hand Surg Eur. 2014;39(5):541–8.
Gong MQ, Huang XW, Wang C, Zha YJ, Li Y, Zhang LD, et al. Management of chronic neglected lateral condyle elbow non-union in adults: functional results of a cohort study and a proposed treatment algorithm. Int Orthop. 2017;41(1):157–64.
Pei X, Han J. Efficacy and feasibility of proximal radioulnar derotational osteotomy and internal fixation for the treatment of congenital radioulnar synostosis. J Orthop Surg Res. 2019;14(1):81.
Failla JM, Amadio PC, Morrey BF. Post-traumatic proximal radio-ulnar synostosis. Results of surgical treatment. J Bone Joint Surg Am. 1989;71(8):1208–13.
Nema SK, Ramasubramani P, Pasupathy P, Austine J. Corrective derotation osteotomies to treat congenital radioulnar synostosis in children: results of a systematic review and meta-analysis. Indian J Orthop. 2022;56(5):717–40.
Jia Y, Geng C, Song Z, Lv S, Dai B. Congenital unilateral proximal radioulnar synostosis: a surgical case report. Medicine (Baltimore). 2020;99(16): e19782.
Miura T, Nakamura R, Suzuki M, Kanie J. Congenital radio-ulnar synostosis. J Hand Surg Br. 1984;9(2):153–5.
Kanaya F. Mobilization of congenital proximal radio-ulnar synostosis: a technical detail. Tech Hand Up Extrem Surg. 1997;1(3):183–8.
Nakasone M, Nakasone S, Kinjo M, Murase T, Kanaya F. Three-dimensional analysis of deformities of the radius and ulna in congenital proximal radioulnar synostosis. J Hand Surg Eur. 2018;43(7):739–43.
Liu L, Liu C, Rong YB, Bai F, Chen SL. Radial pronation angle: a novel radiological evaluation index of congenital proximal radioulnar synostosis. Ann Plast Surg. 2020;84(5 S Suppl 3):S196-s201.
Kanaya K, Iba K, Yamashita T. Long-term results after a free vascularized adipofascial graft for congenital proximal radioulnar synostosis with an average follow-up of 10 years: a series of four cases. J Shoulder Elbow Surg. 2016;25(8):1258–67.
Murase T, Tada K, Yoshida T, Moritomo H. Derotational osteotomy at the shafts of the radius and ulna for congenital radioulnar synostosis. J Hand Surg Am. 2003;28(1):133–7.
Jennison T, McNally M, Pandit H. Prevention of infection in external fixator pin sites. Acta Biomater. 2014;10(2):595–603.
Ktistakis I, Guerado E, Giannoudis PV. Pin-site care: can we reduce the incidence of infections? Injury. 2015;46(Suppl 3):S35–9.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the Medical Science and Technology Project of Henan Province(LHGJ20190385).
Author information
Authors and Affiliations
Contributions
YD is the guarantor of the integrity of the entire study. YD and JX designed the study and contributed to the drafting and critical revision of the manuscript, the approval of the final manuscript, and the manuscript editing. FW, YJ, GF, YL, and HX collected and interpreted the clinical data. All authors reviewed the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all individual participants included in this study. This study was approved by the institutional review board of the Third Affiliated Hospital of Zhengzhou University.
Consent for publication
All patients and their families gave their written informed consent for the publication of their individual data and identifying photographs.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dong, Y., Xu, J., Wang, F. et al. Observation on the effect of reconstruction of the forearm rotation function with an external fixator in the treatment of congenital radioulnar synostosis. J Orthop Surg Res 19, 625 (2024). https://doi.org/10.1186/s13018-024-05112-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-05112-0