Abstract
Background
In this retrospective case investigation, we analysed the data of patients with osteonecrosis of the femoral head (ONFH) to reveal demographic and clinical diagnostic features of ONFH in three northeastern provinces of China and provide a reference for its prevention, diagnosis, and treatment.
Methods
We collected data from patients in Beijing Orthopaedic Hospital of Liaoning, focusing on the aetiology and diagnosis of ONFH. Medical records and self-designed questionnaires were used to collect information for statistical analysis, including age, aetiology, reason for glucocorticoid use, hospital level at first visit, and diagnosis.
Results
In total, 906 patients with complete medical records were included in the analysis. The mean patient age was 47.65 ± 12.12 years. The peak age distribution was in the 40s for men and the 50s for women. Among the total cohort, 72 patients (7.95%; 40 men and 32 women) had traumatic ONFH, 198 (21.85%; 131 men and 67 women) had steroid-induced ONFH, 230 (25.39%; 121 men and 109 women) had idiopathic ONFH, and 406 (44.81%; 397 men and 9 women) had alcohol-induced ONFH. Six hundred and twenty patients were diagnosed with ONFH at the first visit, while 286 patients were misdiagnosed, with a diagnosis rate of 68.43%. The diagnosis rate at the first visit in tertiary hospitals was 76.14%. The diagnosis rate at the first visit in second-class hospitals was 52.07%.ONFH was most likely to be misdiagnosed as lumbar disc herniation.
Conclusions
Most patients with ONFH in three northeastern provinces of China were middle-aged, male, and had alcohol-induced ONFH. The misdiagnosis rate of ONFH at the first visit was very high, especially for misdiagnosis of lumbar disc herniation, indicating that the diagnosis of ONFH requires further improvement.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Osteonecrosis of the femoral head (ONFH) involves a series of pathological changes, such as the death of bone marrow components and bone cells, subchondral fracture, and articular surface collapse, resulting in hip pain and dysfunction owing to various causes [1,2,3]. At present, most studies on ONFH have focused on aetiology and treatment, and there have been few epidemiological investigations. The number of new cases of ONFH in the United States increases by 10,000 to 20,000 each year [4], and approximately 75% of patients are between 30 and 60 years old [5]. In China, the number of new ONFH cases increases by 100,000 to 200,000 each year [6]. With improvement in people’s quality of life and innovations in diagnosis and treatment technologies, these proportions continue to increase each year. However, ONFH is easily misdiagnosed or missed owing to its complex aetiology, the difficulty of detecting it in its early stages, and its high disability rate.
In this study, we conducted a retrospective case investigation among 906 patients with ONFH in three northeastern provinces of China with the aim of revealing the demographic and clinical diagnosis characteristics of ONFH in these provinces and providing a reference for the prevention, diagnosis, and treatment of ONFH.
Materials and methods
All procedures performed in this study were in accordance with the ethical standards of the World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. The study protocol was approved by the Ethics Committee of Aviation General Hospital (No: HK2019-01-04). The ethics committee of our hospital approved this retrospective analysis.
The inclusion criteria of this study were as follows: (1) ONFH diagnosed according to the “Clinical Guidelines for the diagnosis and treatment of femoral head necrosis in Adults“ [7]; (2) patients were diagnosed according to clinical diagnosis, X-ray (orthographic position, frog position), computed tomography or magnetic resonance imaging, and had complete clinical data. The exclusion criteria were: (1) < 18 years old; (2) diagnosed with tuberculosis of the hip joint, bone tumour, acetabular dysplasia, ankylosing spondylitis, necrosis of the hip joint after infection, or femoral head lesions caused by haemophilic arthritis.
Data collection
We collected data of hospitalised patients diagnosed with ONFH between May 2023 and November 2023 in Beijing Orthopaedic Hospital of Liaoning. The medical records were initially screened through the information access system. Key words such as “femoral head necrosis”, “femoral head aseptic necrosis”, “femoral head ischemic necrosis”, and “osteonecrosis of the femoral head” were used to screen the discharge diagnosis, and we collected patient data within the retrieval time range.
Survey form design
We designed a survey table including: (1) general information of patients: age, sex; (2) aetiology of ONFH: (i) history of alcohol abuse (defined as those reporting an average consumption of ≥ 40 g pure alcohol per day for men and ≥ 20 g pure alcohol per day for women during the previous 12 months [8]) and (ii) steroid use (systematic steroid users defined as those with an intake of ≥ 2 g of prednisone or its equivalent within a period of 3 months [9]); (3) diagnosis: first visit hospital level, preliminary diagnosis; and (4) Association Research Circulation Osseous (ARCO) stage.
Statistical analysis
IBM SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Data are expressed as mean ± standard deviation. The Wilcoxon test and Kruskal–Wallis test were used to compare age groups. Rate comparisons were performed using the Pearson chi-square test and continuity correction test. P < 0.05 was considered to indicate statistical significance.
Results
The relevant data of 906 inpatients who met the inclusion criteria were retrieved from the electronic medical record inquiry system, and the data were input into the information table. Patients with ONFH comprised 689 males and 217 females. The sex ratio was 3.175:1. Among them, 299 patients had unilateral ONFH and 607 had bilateral ONFH. There were 1027 hips classified as ARCO stage II, 184 classified as ARCO stage IIIA, 189 classified as ARCO stage IIIB, and 113 classified as ARCO stage IV.
Age distribution
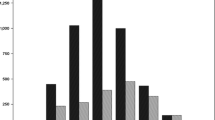
The mean patient age in the total cohort was 47.65 ± 12.12 years, and the mean age was significantly older for women (51.05 ± 14.26 years) than for men (46.58 ± 11.16 years) (Z = − 5.177, P = 0.000). The peak age distribution was in the 40s for men and the 50s for women (Fig. 1). The average age was 48.40 ± 10.06 years among patients with alcohol-induced ONFH, 42.59 ± 13.46 years among patients with steroid-induced ONFH, 47.25 ± 14.66 years among those with trauma-induced ONFH, and 50.82 ± 12.09 among those with idiopathic ONFH. The mean age significantly differed between the four aetiological groups (χ2 = 44.06, P = 0.000). The group with the oldest age of onset was the idiopathic ONFH group, followed by the alcohol-induced, trauma-induced, and steroid-induced ONFH groups from oldest to youngest, respectively (Table 1).
Aetiological characteristics of patients with ONFH
Among the total cohort (Figs. 2), 72 patients (7.95%; 40 men and 32 women) had traumatic ONFH, 198 (21.85%; 131 men and 67 women) had steroid-induced ONFH, 230 (25.39%; 121 men and 109 women) had idiopathic ONFH, and 406 (44.81%; 397 men and 9 women) had alcohol-induced ONFH. Sex was associated with different aetiologies (Fig. 3). The prevalences of steroid-induced and alcohol-induced ONFH were significantly higher in men than women (χ2 = 23.23, P = 0.000 for steroid-induced OFNH; χ2 = 477.87, P = 0.000 for alcohol-induced ONFH). Alcohol-induced ONFH was the most common type of ONFH, and mainly affected men. There were no significant differences between men and women in the prevalences of traumatic and idiopathic ONFH (P > 0.05).The leading three diseases that required glucocorticoid administration leading to OFNH were autoimmune disease (17%), skin disease (16.16%), and nervous system diseases (10.10%). A total of 198 patients with steroid-induced ONFH had underlying diseases (Table 2).
Diagnostic analysis
Of the 906 included patients, 620 patients were diagnosed with ONFH at the first visit; 286 patients were misdiagnosed, giving a diagnosis rate of 68.43% at the first visit. The diagnostic method was radiography for 226 patients, Computed tomography (CT)for 67 patients, Magnetic resonance imaging (MRI) for 261 patients, radiography plus CT for 65 patients, and radiography plus MRI for 287 patients. When misdiagnosed patients were finally diagnosed with ONFH, the proportions of patients with ARCO stages IIIA, IIIB, and IV were significantly higher than those of patients who were correctly diagnosed with ONFH at the first visit (Table 3). In the misdiagnosed group, 95 hips underwent head preservation surgery and 252 hips underwent total hip replacement; in the correctly diagnosed group, 758 hips underwent head preservation surgery and 408 hips underwent total hip arthroplasty (THA). The incidence of THA was significantly lower in the diagnosed group than in the misdiagnosed group (χ2 = 6.99, P = 0.008). Most patients with ONFH (n = 616) were first treated at a tertiary hospital; 469 patients were diagnosed with ONFH and 147 patients were misdiagnosed. The diagnosis rate at the first visit in tertiary hospitals was 76.14%. The first visit among 290 patients with ONFH was to a second-class hospital; 151 patients were diagnosed with ONFH and 139 patients were misdiagnosed. The diagnosis rate at the first visit in second-class hospitals was 52.07%. Misdiagnosis according to different levels of hospital is shown in Table 4, and the probability of misdiagnosis with different diseases is shown in Fig. 4. ONFH was most likely to be misdiagnosed as lumbar disc herniation.
Discussion
ONFH is a devastating disease affecting the hip joint that can cause severe clinical symptoms and greatly reduce quality of life among patients [10,11,12,13,14]. At present, epidemiological studies on ONFH have mainly been routine descriptive studies and aetiological studies [6, 8, 15]. In the present study, we describe in detail not only the age distribution and aetiology of ONFH but also diagnosis and misdiagnosis of OFNH according to different hospital levels.
In this study, male patients accounted for 76.05% and female patients accounted for 23.95% of the total, with a sex ratio of approximately 3.175:1, indicating that men had the highest incidence of ONFH; this finding is consistent with trends described in other studies [5, 16]. The onset time was earlier among male patients, with most developing ONFH between 40 and 49 years of age. In contrast, the peak onset age for women was 50–59 years. These patients are in the middle and younger age groups and represent the main labour force and backbone of the family and society. ONFH in these age groups seriously affects social and family life. Therefore, the prevention and treatment of ONFH should be focused on young and middle-aged populations.
The pathogenesis of ONFH is complex and remains unclear, but commonly accepted causes involve glucocorticoid use, alcohol abuse, and trauma [17,18,19]. In the present study, there was a very high prevalence of alcohol-induced ONFH among male patients. Connective tissue diseases remain the main reason for glucocorticoid administration [15, 20]. However, in our study, glucocorticoids were used for many conditions such as upper respiratory tract infection, allergic rhinitis, skin allergies, and muscle strain, among others. Glucocorticoids should be used with caution in patients with skin diseases, upper respiratory infection, allergic rhinitis, gout, and lumbago. Although many patients did not use glucocorticoids for long periods or in large doses [9], many had a history of using small doses at the time. The relationship between the use of low-dose hormones and the occurrence of ONFH requires further study.
A large number of patients have ONFH in China [6, 8]. The diagnosis rate of early ONFH at the first visit was only 68.43%. More than half of the patients in the study cohort presented at tertiary hospitals for their first visit, and the rate of first diagnosis of ONFH in tertiary hospitals was only 76.14%. We found that the most commonly misdiagnosed disease was lumbar disc herniation, followed by soft tissue injury. On physical examination, patients with ONFH have limited hip flexion, internal rotation, and external rotation. Additionally, MRI is up to 100% sensitive for the diagnosis of ONFH [21]. Therefore, physical examination and MRI are very valuable to avoid misdiagnosis and missed diagnosis of early ONFH. It is very important to obtain a timely diagnosis to enable the performance of ‘joint- preserving’ treatments and delay THA for as long as possible. Combining core decompression with bone grafting, bone marrow-derived cell transplantation, or other techniques seems to provide better outcomes than core decompression alone [22, 23]. However, approximately one-third of the osteotomies performed in patients with ONFH are reportedly converted to THA during a period of approximately 7 years [24]. Therefore, osteotomy should be performed cautiously in carefully selected older adult patients with ONFH [24]. The reported factors that negatively affect the postoperative efficacy of joint-preserving treatments are male sex, a longer symptom duration before treatment, a higher visual analogue scale score for pain, and a lower Harris Hip Score [25]. Joint-preserving treatments are also reportedly effective for the management of ONFH in skeletally immature patients [26].
There are some limitations in this study. First, this was a small sample size; further multi-centre research with a larger sample is required. Second, only patients diagnosed with ONFH were included in this study. Patients with hip dysplasia and primary or secondary hip osteoarthritis who were misdiagnosed with ONFH were not included. Third, further study is needed to investigate whether the severity of ONFH varies in accordance with the aetiology and patient age.
Conclusion
Most patients with ONFH in the three northeastern provinces of China in this study were middle-aged men with alcohol-induced ONFH. The misdiagnosis rate of ONFH at the first visit was very high, especially for misdiagnosis of lumbar disc herniation, indicating that the diagnosis of ONFH requires further improvement.
Data availability
No datasets were generated or analysed during the current study.
References
Petek D, Hannouche D, Suva D. Osteonecrosis of the femoral head: pathophysiology and current concepts of treatment[J]. Effort Open Rev. 2019;4(3):85–97.
Homma Y, Masubuchi Y, Shirogane Y, et al. Grafting of autologous concentrated bone marrow processed using a point-of-care device for patients with osteonecrosis of the femoral head: a phase 1 feasibility and safety study[J]. Regen Ther. 2022;20:18–25.
Liu L, Gao F, Sun W, et al. Investigating clinical failure of core decompression with autologous bone marrow mononuclear cells grafting for the treatment of non-traumatic osteonecrosis of the femoral head[J]. Int Orthop. 2018;42(7):1575–83.
Narayanan A, Khanchandani P, Borkar RM, et al. Avascular necrosis of femoral head: a metabolomic, Biophysical, biochemical, Electron Microscopic and Histopathological Characterization[J]. Sci Rep. 2017;7(1):10721.
Lamb JN, Holton C, O’Connor P, et al. Avascular necrosis of the hip[J]. BMJ. 2019;365:l2178.
Cui L, Zhuang Q, Lin J, et al. Multicentric epidemiologic study on six thousand three hundred and ninety five cases of femoral head osteonecrosis in China[J]. Int Orthop. 2016;40(2):267–76.
Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head[J]. J Bone Joint Surg Am. 1995;77(3):459–74.
Zhao DW, Yu M, Hu K, et al. Prevalence of nontraumatic osteonecrosis of the femoral head and its Associated Risk factors in the Chinese Population: results from a nationally Representative Survey[J]. Chin Med J (Engl). 2015;128(21):2843–50.
Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later[J]. J Bone Joint Surg Am. 2006;88(5):1117–32.
Chughtai M, Piuzzi NS, Khlopas A, et al. An evidence-based guide to the treatment of osteonecrosis of the femoral head[J]. Bone Joint J. 2017;99–B(10):1267–79.
Cheng EY, Cui Q, Goodman SB, et al. Diagnosis and treatment of femoral head osteonecrosis: a protocol for development of evidence-based clinical practice Guidelines[J]. Surg Technol Int. 2021;38:371–8.
Ha YC, Jung WH, Kim JR, et al. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images[J]. J Bone Joint Surg Am. 2006;88(Suppl 3):35–40.
Wei QS, Li ZQ, Hong ZN, et al. Predicting Collapse in Osteonecrosis of the femoral Head using a New Method: preserved angles of anterior and lateral femoral Head[J]. J Bone Joint Surg Am. 2022;104(Suppl 2):47–53.
Mont MA, Cherian JJ, Sierra RJ, et al. Nontraumatic osteonecrosis of the femoral head: where do we stand today? A ten-year Update[J]. J Bone Joint Surg Am. 2015;97(19):1604–27.
Fukushima W, Fujioka M, Kubo T, et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head[J]. Clin Orthop Relat Res. 2010;468(10):2715–24.
Cohen-Rosenblum A, Cui Q. Osteonecrosis of the femoral Head[J]. Orthop Clin North Am. 2019;50(2):139–49.
Koo KH, Mont MA, Cui Q, et al. The 2021 Association Research Circulation Osseous classification for early-stage osteonecrosis of the femoral head to computed tomography-based Study[J]. J Arthroplasty. 2022;37(6):1074–82.
Mont MA, Zywiel MG, Marker DR, et al. The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review[J]. J Bone Joint Surg Am. 2010;92(12):2165–70.
Steinberg ME, Brighton CT, Steinberg DR et al. Treatment of avascular necrosis of the femoral head by a combination of bone grafting, decompression, and electrical stimulation[J]. Clin Orthop Relat Res, 1984(186):137–53.
Yue J, Wan F, Zhang Q, et al. Effect of glucocorticoids on miRNA expression spectrum of rat femoral head microcirculation endothelial cells[J]. Gene. 2018;651:126–33.
Zhao D, Zhang F, Wang B, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version). J Orthop Translat. 2020;21:100–10.
Sadile F, Bernasconi A, Russo S, et al. Core decompression versus other joint preserving treatments for osteonecrosis of the femoral head: a meta-analysis[J]. Br Med Bull. 2016;118(1):33–49.
Migliorini F, Maffulli N, Eschweiler J, et al. Core decompression isolated or combined with bone marrow-derived cell therapies for femoral head osteonecrosis[J]. Expert Opin Biol Ther. 2021;21(3):423–30.
Quaranta M, Miranda L, Oliva F, et al. Osteotomies for avascular necrosis of the femoral head[J]. Br Med Bull. 2021;137(1):98–111.
Migliorini F, Maffulli N, Baroncini A, et al. Prognostic factors in the management of osteonecrosis of the femoral head: a systematic review[J]. Surgeon. 2023;21(2):85–98.
Migliorini F, La Padula G, Oliva F, et al. Operative management of avascular necrosis of the femoral head in skeletally immature patients: a systematic Review[J]. Life (Basel). 2022;12(2):179.
Acknowledgements
We thank Nancy Schatken BS, MT (ASCP), from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Wangyan Liu and Ju’an Yue collect data and write articles; Xiaozhong Guo, Randong Wang and Hao Fu were responsible for literature review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. All methods were approved by the Ethics Committee of Aviation General Hospital (No: HK2019-01-04). Written informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
All authors agree to publish “Epidemiological investigation and diagnostic analysis of osteonecrosis of the femoral head in three northeastern provinces of China” in the Journal of Orthopaedic Surgery and Research.
Competing interests
The authors declare no competing interests.
Abbreviations
ARCO Association Research Circulation Osseous.
Computed tomography (CT).
MRI Magnetic resonance imaging.
ONFH Osteonecrosis of the femoral head.
THA Total hip arthroplasty.
Data and materials availability statement
All data and materials used to support the findings of this study are included within the article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, W., Yue, J., Guo, X. et al. Epidemiological investigation and diagnostic analysis of osteonecrosis of the femoral head in three northeastern provinces of China. J Orthop Surg Res 19, 292 (2024). https://doi.org/10.1186/s13018-024-04768-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04768-y