Abstract
Background
Osteosynthesis for sacroiliac joint (SIJ) diastasis using an iliosacral screw (ISS) and a trans-iliac-trans-sacral screw (TITSS) can be performed using a closed or an open method. However, no clear indication for open reduction has been established.
Methods
Data on patients with unilateral traumatic SIJ diastasis who underwent ISS and TITSS fixation were retrospectively collected and separated into groups according to the reduction method: closed reduction group (C group) and open reduction group (O group). Demographic data and perioperative image assessments were compared between the groups. The critical distance of the SIJ was identified to elucidate the indication for open reduction of the diastatic SIJ.
Results
Fifty-six patients met the inclusion criteria over a 3-year period. There was no significant difference in the reduction quality of pelvic ring injuries between the groups, according to Matta’s and Lefaivre’s criteria. The improvement in the SIJ distance was significantly greater in the O group than in the C group in the axial plane on multiplanar computed tomography (p = 0.021). This model predicted that a difference of > 3.71 mm between the injured and healthy SIJ was a recommended indication for open reduction, with an area under the curve of 0.791 (95% confidence interval 0.627–0.955, p = 0.004).
Conclusions
Open reduction for SIJ diastasis might achieve better reduction quality than does closed reduction in the axial plane in selected cases. When the difference between the injured and healthy SIJ was wider than 3.71 mm, open reduction was recommended for satisfactory radiological outcomes.
Similar content being viewed by others
Background
The integrity of the posterior weight-bearing sacroiliac joint (SIJ) contributes to pelvic ring stability [1]. SIJ diastasis, a crucial pattern in posterior pelvic ring injuries, often results from high-energy trauma, and the soft tissue surrounding the pelvis is often severely contused and disrupted [2, 3]. Pelvic malunion can cause severe sequelae if untreated, which include leg length discrepancy, posterior pelvic pain, sitting imbalance, and back pain [4, 5].
The optimal treatment for the complex SIJ diastasis remains a challenge for orthopedic surgeons [6]. Minimizing the gap between the ilium and sacrum to the anatomical positions is one of the key goals for achieving satisfactory radiological and functional outcomes [7,8,9]. Therefore, the aim of operative treatment is to restore normal anatomy by rigid fixation to enable early mobilization in order to obtain functional recovery.
Different fixation methods have been developed for SIJ diastasis [10,11,12]. Osteosynthesis is achieved by an open or a closed method followed by internal fixation, including iliosacral screw (ISS) fixation, trans-iliac–trans-sacral screw (TITSS) fixation, sacral bar fixation, spinopelvic osteosynthesis, posterior tension band plating, and anterior SIJ plating [10, 13,14,15,16]. Minimally invasive procedures using percutaneous screws, such as ISS or TITSS fixation, are preferred for osteosynthesis in cases of SIJ diastasis, contributing to a decrease in operating time, surgical bleeding, and soft tissue disruption and preventing nonunion [17, 18].
Reduction of the dislocated SIJ using an open or a closed method should be performed prior to percutaneous screw fixation. Compared with the open method, closed reduction is superior because it reduces intraoperative blood loss and lowers the infection rate without compromising the reduction quality [19,20,21]. However, in some injury patterns such as crescent fracture and completely dislocated SIJ, closed reduction is anticipated to fail and an open approach is recommended to achieve anatomical reduction [22]. Despite this, an absolute indication for open reduction of the SIJ is lacking.
Since there is no quantitative evidence that open reduction should be advocated for widening of the SIJ, the actual indication for open reduction for the diastatic SIJ should be explored. The primary aim of our study was to compare radiological outcomes after osteosynthesis for SIJ diastasis using closed or open reduction, followed by ISS and TITSS fixation. Additionally, the critical distance of the widened SIJ that supports open reduction was elucidated.
Methods
Patient allocation
Medical records of patients who were diagnosed with pelvic ring injury (PRI) and underwent osteosynthesis between January 2017 and December 2021 were retrospectively collected from the fracture registration database of our institute. The inclusion criteria were as follows: (1) unilateral SIJ diastasis and percutaneous screw(s) fixation (ISS, TITSS, or both) through a closed or an open reduction technique; (2) management for SIJ diastasis as the primary or first reduction for PRI (before reduction and fixation of anterior pelvic ring injury); and (3) completeness of medical and radiological records for at least 12 months. Patients under 18 years of age and those who underwent screw fixation as an emergent resuscitative procedure (an antishock screw) or screw fixation with bone cement augmentation (for fragility fracture or pathological fracture of the pelvic ring) were excluded. Medical records and preoperative and postoperative radiological images were meticulously reviewed and analyzed. All operative procedures were performed by a single senior surgeon.
Perioperative protocol and surgical technique
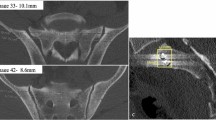
The patients were admitted to the ordinary ward or intensive care unit as required after primary resuscitation. Osteosynthesis for PRI was performed as soon as possible after the patient was hemodynamically stabilized. Prior to definite osteosynthesis, standard radiological images including pelvic radiography (anteroposterior [AP], inlet, and outlet views) and multiplanar computed tomography (mpCT) were obtained for surgical planning. If a pelvic binder was applied during initial image evaluations, the X-rays and mpCT were systematically repeated before surgery to avoid potential underclassification. We collected information on maximal SIJ diastasis along with the difference between healthy and injured SIJ from mpCT in both axial and coronal views (Fig. 1). Patients who were not indicated for ISS or TITSS because of conditions such as sacral dysmorphisms and a shallow bony corridor were excluded for the planning screw placement.
The operation was performed under general anesthesia with the patients in the supine or prone position, depending on the planned procedures and concomitant injuries observed, on a radiolucent table (Modular Table System©; Mizuho OSI, California, USA). The supine position was preferred for those showing contraindications for the prone position. Before beginning sterile draping, the patients’ injuries were evaluated under anesthesia to determine the necessity to upgrade the fracture pattern and change the surgical plan. Real-time fluoroscopic images including AP, inlet, outlet, Judet oblique views, and sacrum lateral views were examined prior to surgical draping to ensure that all images could be obtained clearly without limitations. The intraoperative images were obtained by using a single-arm fluoroscopic intensifier (Ziehm Solo; Ziehm Imaging GmbH, Nuremberg, Germany).
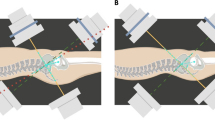
The osteosynthesis strategy for anterior and posterior PRI can be performed simultaneously (supine position) or sequentially (first prone and then supine positions). However, posterior pelvic ring reduction and fixation were performed before the anterior pelvic ring procedure. For the closed reduction technique, the SIJ was reduced by the direct compression force provided by an appropriately placed ISS perpendicular to the orientation of the SIJ (Fig. 2). The TITSS was implanted after ISS fixation for the purpose of augmented fixation.
On the other hand, the surgical approach could be either from the anterior (through the lateral window of the ilioinguinal approach in the supine position) or dorsal (a 5 cm longitudinal incision direct or 1 cm lateral to the posterior superior iliac spine in the prone position) side for the open reduction technique. Using the dorsal approach, the angled Matta clamp (DePuy Synthes, Paoli, PA, USA) was applied with one jaw on the hooked on the anterior cortex of the sacrum and the other on the dorsal cortex of the ilium (Fig. 3). After reduction of the SIJ was confirmed via fluoroscopic images, a provisional Kirschner wire was inserted percutaneously under real-time fluoroscopic examination. A 7.0-mm cannulated screw (Syntec Technology Co., Hsinchu, Taiwan) was applied as the target implant of the ISS. Whenever an additional screw was necessary to provide stability to the posterior pelvic ring, a cannulated screw (TITSS 7.0 mm; Syntec Technology Co., Hsinchu, Taiwan) with an orientation parallel to the groundline wound was applied. The radiation dose and time were recorded during percutaneous screw osteosynthesis.
Following completion of reduction and fixation of the SIJ, anterior pelvic ring reduction and fixation were performed. Intramedullary screw (Syntec Technology Co., Hsinchu, Taiwan) fixation was planned for the pubic rami fractures, for which closed reduction was performed in the prone (antegrade fashion) or supine (antegrade or retrograde fashion) position. When the anterior pelvic injury was indicated for open reduction (pubic symphysis diastasis or failed/inadequate reduction of the pubic rami fractures), a Pfannenstiel incision was placed and plate osteosynthesis (3.5-mm reconstruction plate, DePuy Synthes, Paoli, PA, USA) was performed.
Image assessment protocol
Identical postoperative imaging examinations were performed to examine the reduction quality of the pelvic ring and position of the implants using radiographs, including AP, inlet, and outlet views, and mpCT. Radiological interpretation was performed by an independent medical doctor, who was not involved in the surgeries, using the Picture Archiving and Communication System (Centricity Enterprise Web V3.0; GE Healthcare, Chicago, USA), and the interpretations were re-examined repeatedly by two other senior orthopedic surgeons.
Several classifications and grading systems for fracture patterns, reduction quality, and screw positions were used in this study. The PRI was classified using the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification system [23]. The reduction qualities after osteosynthesis were evaluated from radiographs, including axial and coronal views from mpCT. We adapted the criteria of Matta/Tornetta and Lefaivre to interpret the reduction quality [24,25,26]. Accordingly, the reduction quality of the pelvic ring injury was classified as excellent, good, fair, or poor. For the ISS, we examined the angles between the screw and the SIJ obtained in the axial and coronal views of the mpCT. The angular differences between the implanted screw and the ideal orientation of the ISS, which should be perpendicular to the SIJ in each view, were measured and identified as the angles deviated from the ideal orientation (ADIO) (Fig. 4) [27]. For TITSS, the angular difference between the implanted screw and the ideal orientation, which should be parallel to the groundline in both axial and coronal views of the mpCT scan, were recorded.
Ideal angles between ISS (line S) and the sacroiliac joint (line J). The ideal angles are 90° in both A axial and B coronal views. The actual angles that deviated from these ideal orientations are defined as the ADIO of ISS. The ideal angle between TITSS (line S) and groundline (line G) is 0° in both C axial and D coronal views. The actual angles that deviated from these ideal orientations are defined as the ADIO of TITS. The ISS, TITSS, and ADIO deviated from the ideal orientation. ISS Iliosacral screw, TITSS Trans-iliac-trans-sacral screw, ADIO Angles deviated from the ideal orientation
Statistical analysis
Because of the retrospective nature of the study, Pearson’s correlation analysis was first employed to identify potential variables that were correlated to outcome measurements in terms of a reduction in the SIJ distance. The chi-squared test was used to analyze categorical data. The t-test was used for between-group comparisons of numerical data. Statistical significance was set as p < 0.05. The cutoff point value was defined as the maximum Youden’s index. Statistical analyses were performed using SPSS 26.0 program for Windows (IBM SPSS Statistics for Windows, Version 26.0; IBM Corp, NY, USA).
Results
Fifty-six patients with unilateral SIJ injuries underwent percutaneous screw fixation between January 2017 and December 2021. Table 1 shows that the presence of sacral fracture and the SIJ reduction method were significantly correlated with a reduced SIJ distance on axial and coronal views of mpCT (p = 0.031 and 0.001 for sacral fracture and p = 0.008 and 0.025 for SIJ reduction method, respectively). This result was consistent with our hypothesis that the indication for closed/open reduction may be correlated with the reduction in the SIJ distance.
Table 2 shows the characteristics of the patients in the closed reduction group (C group) and open reduction group (O group). There were no differences in the chosen parameters between the two groups. Moreover, there was no difference in the occurrence of sacral fracture between the two groups.
Perioperative comparisons between the two groups are shown in Table 3. More patients were classified as AO B2.3 in the C group (p = 0.002). A significantly higher rate of prone position for surgery was observed in the O group (p < 0.001). More blood loss and a longer operation duration were observed in the O group than in the C group. Although real-time fluoroscopic guidance is essential for percutaneous ISS or TITSS, especially for the C group, we did not find a significant difference between the two reduction techniques. Regarding the measured ADIO of the screws, there were no differences between the two groups despite a larger angle measured in the O group.
The results of the postoperative imaging assessments are shown in Table 4. Both Matta and Lefaivre criteria revealed equal results for the two applied approaches. Upon mpCT assessment, wider SIJ distances before and after osteosynthesis were observed in the O group. However, SIJ distances were also significantly reduced in the O group in both the axial and coronal planes (p = 0.008 and 0.025, respectively).
Both closed and open reduction could achieve good reduction quality, with more SIJ distance reduction observed in the O group (Tables 3, 4). We obtained a receiver operating characteristic (ROC) curve (Fig. 5) to determine if any listed factors, including preoperative SIJ diastasis in the axial/coronal view and preoperative axial/coronal SIJ joint difference between the healthy and injured sides, could predict whether the patients should undergo open or closed reduction. The four factors mentioned above showed an excellent or acceptable discrimination to predict open reduction with an area under the curve (AUC) of 0.822, 0.778, 0.789, and 0.791, respectively.
By calculating the maximum Youden’s index of the four factors mentioned above, we could identify the cut-point of SIJ diastasis that could predict patients who received open reduction and internal fixation (ORIF) (axial SIJ = 6.52 mm, coronal SIJ = 7.26 mm, axial SIJ difference = 3.39 mm, coronal SIJ difference = 3.71 mm). We assumed that if the patients, whose injured SIJ was wider than the cut-point distance, received closed reduction and internal fixation (CRIF), the distance reduced after osteosynthesis would be lesser than that in patients who received ORIF. According to our data, a preoperative SIJ difference of > 3.71 mm between the healthy and injured sides in the coronal plane showed increased SIJ reduction under open reduction with statistical significance (2.18 mm and 6.58 mm in closed and open reduction, respectively, with p = 0.021) (Table 5). The Matta and Lefaivre criteria were used to evaluate differences between CRIF and ORIF, with no statistical significance.
Discussion
Satisfactory treatment of SIJ diastasis poses a great challenge for orthopedic surgeons. If SIJ diastasis is left untreated or undertreated, global pelvic instability may occur and cause short-term and possibly further long-term sequelae. CRIF with ISS, with or without TITSS, is an attractive treatment for diastatic joints because it is less invasive. However, ORIF may be needed when there is an imperfect reduction in the SIJ during screw purchasing. There is no evidence to explore the absolute indication for ORIF in cases of SIJ diastasis. We analyzed 56 patients who underwent percutaneous screw fixation with closed or open reduction. With our results showing a satisfactory screw position and acceptable reduction quality of the PRI, we found a critical difference in SIJ distance between the injured and healthy side (3.71 mm, coronal plane of the mpCT), which is recommended for open reduction of the injury.
Among patients with SIJ injury indicated for surgery, those who were surgically treated showed a better outcome and health-related quality of life [28,29,30,31,32]. To achieve anatomical reduction, different reduction methods and implant choices have been advocated [33]. The anterior approach with plating has the advantage of providing direct visualization to the anterior SIJ and simultaneous access to symphyseal disruption [10, 34, 35]. However, large tissue dissection, especially the elevation of the iliacus from the ilium, may cause postoperative morbidities [25]. Meanwhile, iatrogenic lumbar nerve root injuries may be encountered during the plating procedure [36]. Similarly, a prominent implant and increasing surgical site infection may be followed by posterior plating in terms of tension band plate for the posterior pelvic ring [37].
Iliosacral screw was first introduced by Matta et al. for posterior pelvic ring fixation [25]. Despite some reports raising concerns that ISS may be associated with more intraoperative exposure to X-rays and neurologic damage [38], it became a popular fixation method because it is less invasive and results in less blood loss and a lower infection rate along with good stabilization [39,40,41]. Khaled et al. reported that over 90% of patients with posterior pelvic ring instability could achieve excellent or good radiology outcome after ISS treatment [42]. A closed reduction maneuver is suggested for ISS insertion to preserve blood supply to the bone, limit scarring in the surrounding soft tissues, cause less blood loss, and reduce morbidity from open reduction [21, 41, 43].
However, drawbacks and limitations exist with application of the closed reduction method for SIJ injury [44]. Katharina et al. reported failed anatomical reduction by closed reduction in 5 of 31 patients, resulting in poorer functional outcome [45]. In a study by Starr et al. [21], closed reduction failed in 2 of 27 patients with SIJ injury because of an extended duration between the time of injury and surgery as well as marked displacement. Consequently, open reduction through an anterior or a posterior approach plays a role in managing SIJ diastasis. Through the anterior approach, fragments and/or debris within the SIJ could be visualized, and the surrounding fibrous tissue could be easily removed [34]. Using the posterior approach, sacral fracture visualization and nerve root decompression could be performed simultaneously with SIJ anatomical reduction and fixation with a percutaneous IS screw [46, 47].
However, there is no clear indication for the use of open reduction over closed reduction to achieve widening of the SIJ diastasis. Lindsay et al. [5] presented a similar satisfactory reduction quality via both closed and open reduction for ISS insertion. Both methods can achieve excellent or good reduction quality; however, no definite indications were documented in the present study. Some studies suggested open reduction in case of failure of closed reduction [44, 45]. According to the results of this study, we proposed that with a distance difference wider than 3.71 mm between the injured and healthy SIJ in the coronal plane, the open method is recommended for SIJ reduction, either from the anterior or mostly from the posterior approach. To our knowledge, this is the first study to focus on the indication of open reduction for diastatic SIJ by screw fixation.
Despite efforts to avoid bias, this study has several limitations. First, it had a retrospective design. Second, the selection of closed or open reduction was primarily based on the surgeon’s experience. However, our results advise that inadequate reduction may be achieved by closed reduction if the SIJ diastasis exceeds the critical value. Third, comprehensive evaluation of the bone quality was not performed for each patient. One factor that led to a successful closed reduction was the linear compressive force exerted by the ISS. Closure of the SIJ may be imperfect if the sacrum density is weak. Finally, the functional outcomes of the enrolled patients have not been reported. The actual relationship between the reduction quality and post-surgery functional performance could not be explored. Further studies should be conducted using a prospective method, focusing on the selection of patients who have undergone open reduction based on an established algorithm. Furthermore, the functional outcomes should be reported, and the correlation with the algorithm should be examined.
Conclusions
In conclusion, fixation of the SIJ with the ISS and TITSS, either through closed or open reduction, could attain satisfactory and comparable radiological outcomes. Furthermore, for patients in whom the distance between the injured and healthy SIJ is > 3.71 mm in the coronal plane, surgeons should be prepared to perform open reduction (including ensuring the availability of sterile draping and appropriate reduction instruments) in case of unsatisfactory reduction by the closed method.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SIJ:
-
Sacroiliac joint
- ISS:
-
Iliosacral screw
- TITSS:
-
Trans-iliac-trans-sacral screw
- PRI:
-
Pelvic ring injury
- AP:
-
Anteroposterior
- mpCT:
-
Multiplanar computed tomography
- AO:
-
Arbeitsgemeinschaft für Osteosynthesefragen
- ADIO:
-
Angles deviated from the ideal orientation
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- ORIF:
-
Open reduction and internal fixation
- CRIF:
-
Closed reduction and internal fixation
References
Tile M. Pelvic ring fractures: should they be fixed. J Bone Jt Surg Br. 1988;70:1–12. https://doi.org/10.1302/0301-620X.70B1.3276697.
Trafton PG. Pelvic ring injuries. Surg Clin N Am. 1990;70:655–69. https://doi.org/10.1016/S0039-6109(16)45135-2.
Routt ML, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995;9:207–14. https://doi.org/10.1097/00005131-199506000-00005.
Tripathy SK, Goyal T, Sen RK. Nonunions and malunions of the pelvis. Eur J Trauma Emerg Surg. 2015;41:335–42. https://doi.org/10.1007/s00068-014-0461-0.
Lindsay A, Tornetta P, Diwan A, Templeman D. Is closed reduction and percutaneous fixation of unstable posterior ring injuries as accurate as open reduction and internal fixation. J Orthop Trauma. 2016;30:29–33. https://doi.org/10.1097/BOT.0000000000000418.
Ashby K, Yilmaz E, Mathkour M, Olewnik Ł, Hage D, Iwanaga J, et al. Ligaments stabilizing the sacrum and sacroiliac joint: a comprehensive review. Neurosurg Rev. 2022;45:357–64. https://doi.org/10.1007/s10143-021-01625-y.
Pastor T, Tiziani S, Kasper CD, Pape HC, Osterhoff G. Quality of reduction correlates with clinical outcome in pelvic ring fractures. Injury. 2019;50:1223–6. https://doi.org/10.1016/j.injury.2019.04.015.
Suzuki T, Shindo M, Soma K, Minehara H, Nakamura K, Uchino M, et al. Long-term functional outcome after unstable pelvic ring fracture. J Trauma. 2007;63:884–8. https://doi.org/10.1097/01.ta.0000235888.90489.fc.
Lai CY, Lai PJ, Tseng IC, Su CY, Hsu YH, Chou YC, et al. Postoperative reduction quality may be the most important factor that causes worse functional outcomes in open and closed pelvic fractures. World J Surg. 2022;46:568–76. https://doi.org/10.1007/s00268-021-06386-9.
Simpson LA, Waddell JP, Leighton RK, Kellam JF, Tile M. Anterior approach and stabilization of the disrupted sacroiliac joint. J Trauma. 1987;27:1332–9. https://doi.org/10.1097/00005373-198712000-00003.
Fowler TT, Bishop JA, Bellino MJ. The posterior approach to pelvic ring injuries: a technique for minimizing soft tissue complications. Injury. 2013;44:1780–6. https://doi.org/10.1016/j.injury.2013.08.005.
Pascal-Moussellard H, Hirsch C, Bonaccorsi R. Osteosynthesis in sacral fracture and lumbosacral dislocation. Orthop Traumatol Surg Res. 2016;102:S45-57. https://doi.org/10.1016/j.otsr.2015.12.002.
Khaleel VM, Pushpasekaran N, Prabhu N, Pandiyan A, Koshy GM. Posterior tension band plate osteosynthesis for unstable sacral fractures: a preliminary study. J Clin Orthop Trauma. 2019;10(Suppl 1):S106–11. https://doi.org/10.1016/j.jcot.2019.05.017.
Patel S, Ghosh A, Jindal K, Kumar V, Aggarwal S, Kumar P. Spinopelvic fixation for vertically unstable AO type C pelvic fractures and sacral fractures with spinopelvic dissociation—a systematic review and pooled analysis involving 479 patients. J Orthop. 2022;29:75–85. https://doi.org/10.1016/j.jor.2022.01.010.
Yinger K, Scalise J, Olson SA, Bay BK, Finkemeier CG. Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma. 2003;17:481–7.
Vanderschot P, Meuleman C, Lefèvre A, Broos P. Trans iliac-sacral-iliac bar stabilisation to treat bilateral lesions of the sacro-iliac joint or sacrum: anatomical considerations and clinical experience. Injury. 2001;32:587–92. https://doi.org/10.1016/S0020-1383(01)00039-0.
Routt ML, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997;11:584–9. https://doi.org/10.1097/00005131-199711000-00007.
Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br. 2007;89:145–54. https://doi.org/10.1302/0301-620X.89B2.18551.
Schweitzer D, Zylberberg A, Córdova M, Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008;39:869–74. https://doi.org/10.1016/j.injury.2008.03.024.
Abou-Khalil S, Steinmetz S, Mustaki L, Leger B, Thein E, Borens O. Results of open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable pelvic ring injuries: retrospective study of 36 patients. Eur J Orthop Surg Traumatol. 2020;30:877–84. https://doi.org/10.1007/s00590-020-02646-x.
Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61-B2.2 and 61-B2.3, or Young-Burgess “lateral compression type II” pelvic fractures). J Orthop Trauma. 2002;16:116–23.
Elzohairy MM, Salama AM. Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. Orthop Traumatol Surg Res. 2017;103:223–7. https://doi.org/10.1016/j.otsr.2016.12.002.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1-33.
Tornetta P, Matta JM. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res. 1996;329:186–93. https://doi.org/10.1097/00003086-199608000-00022.
Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;242:83–97.
Lefaivre KA, Starr AJ, Barker BP, Overturf S, Reinert CM. Early experience with reduction of displaced disruption of the pelvic ring using a pelvic reduction frame. J Bone Jt Surg Br. 2009;91:1201–7. https://doi.org/10.1302/0301-620X.91B9.22093.
Chen JP, Tsai PJ, Su CY, Tseng IC, Chou YC, Chen IJ, et al. Percutaneous iliosacral screw and trans-iliac trans-sacral screw with single C-arm fluoroscope intensifier is a safe treatment for pelvic ring injuries. Sci Rep. 2022;12:368. https://doi.org/10.1038/s41598-021-04351-z.
Henderson RC. The long-term results of nonoperatively treated major pelvic disruptions. J Orthop Trauma. 1989;3:41–7. https://doi.org/10.1097/00005131-198903010-00008.
Chen PH, Hsu WH, Li YY, Huang TW, Huang TJ, Peng KT. Outcome analysis of unstable posterior ring injury of the pelvis: comparison between percutaneous iliosacral screw fixation and conservative treatment. Biomed J. 2013;36:289–94. https://doi.org/10.4103/2319-4170.112757.
Dujardin FH, Hossenbaccus M, Duparc F, Biga N, Thomine JM. Long-term functional prognosis of posterior injuries in high-energy pelvic disruption. J Orthop Trauma. 1998;12:145–50. https://doi.org/10.1097/00005131-199803000-00001. (discussion 150–1).
Verma V, Sen RK, Tripathy SK, Aggarwal S, Sharma S. Factors affecting quality of life after pelvic fracture. J Clin Orthop Trauma. 2020;11:1016–24. https://doi.org/10.1016/j.jcot.2020.08.011.
McLaren AC, Rorabeck CH, Halpenny J. Long-term pain and disability in relation to residual deformity after displaced pelvic ring fractures. Can J Surg. 1990;33:492–4.
Liuzza F, Silluzio N, Florio M, El Ezzo O, Cazzato G, Ciolli G, et al. Comparison between posterior sacral plate stabilization versus minimally invasive transiliac-transsacral lag-screw fixation in fractures of sacrum: a single-centre experience. Int Orthop. 2019;43:177–85. https://doi.org/10.1007/s00264-018-4144-z.
Leighton RK, Waddell JP. Techniques for reduction and posterior fixation through the anterior approach. Clin Orthop Relat Res. 1996;329:115–20. https://doi.org/10.1097/00003086-199608000-00014.
Riouallon G, Chanteux L, Upex P, Zaraa M, Jouffroy P. Anterior approach to the sacroiliac joint for pelvic ring fractures: technical note. Orthop Traumatol Surg Res. 2020;106:845–7. https://doi.org/10.1016/j.otsr.2020.02.016.
Bai Z, Gao S, Liu J, Liang A, Yu W. Anatomical evidence for the anterior plate fixation of sacroiliac joint. J Orthop Sci. 2018;23:132–6. https://doi.org/10.1016/j.jos.2017.09.003.
Goldstein A, Phillips T, Sclafani SJ, Scalea T, Duncan A, Goldstein J, et al. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–33. https://doi.org/10.1097/00005373-198604000-00004.
Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: technique and perioperative complications. Arch Orthop Trauma Surg. 2011;131:809–13. https://doi.org/10.1007/s00402-010-1230-0.
Gire JD, Jiang SY, Gardner MJ, Bishop JA. Percutaneous versus open treatment of posterior pelvic ring injuries: changes in practice patterns over time. J Orthop Trauma. 2018;32:457–60. https://doi.org/10.1097/BOT.0000000000001236.
Barei DP, Bellabarba C, Mills WJ, Routt ML. Percutaneous management of unstable pelvic ring disruptions. Injury. 2001;32 Suppl 1:SA33–44. https://doi.org/10.1016/s0020-1383(01)00059-6.
Zhang R, Yin Y, Li S, Hou Z, Jin L, Zhang Y. Percutaneous sacroiliac screw versus anterior plating for sacroiliac joint disruption: a retrospective cohort study. Int J Surg. 2018;50:11–6. https://doi.org/10.1016/j.ijsu.2017.12.017.
Khaled SA, Soliman O, Wahed MA. Functional outcome of unstable pelvic ring injuries after iliosacral screw fixation: single versus two screw fixation. Eur J Trauma Emerg Surg. 2015;41:387–92. https://doi.org/10.1007/s00068-014-0456-x.
Kim CH, Kim JW. Plate versus sacroiliac screw fixation for treating posterior pelvic ring fracture: a systematic review and meta-analysis. Injury. 2020;51:2259–66. https://doi.org/10.1016/j.injury.2020.07.003.
Yarboro SR, Hadeed MM, Vess EM, Weiss DB. A locked sacroiliac joint dislocation requiring open reduction: a case report. JBJS Case Connect. 2019;9:e0384. https://doi.org/10.2106/JBJS.CC.18.00384.
Jäckle K, Spering C, Seitz MT, Höller S, Meier MP, Hahn FM, et al. Anatomic reduction of the sacroiliac joint in unstable pelvic ring injuries and its correlation with functional outcome. Eur J Trauma Emerg Surg. 2022;48:1491–8. https://doi.org/10.1007/s00068-020-01504-z.
Ward EF, Tomasin J, Vander Griend RA. Open reduction and internal fixation of vertical shear pelvic fractures. J Trauma. 1987;27:291–5.
Pohlemann T, Angst M, Schneider E, Ganz R, Tscherne H. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993;7:107–17.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, Grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: R-SC and Y-HY; Investigation: R-SC, I-JC, C-YL, and J‑PC; Writing: R-SC and Y-HY; Writing—review and supervision: Y-HY. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective chart review study involving human participants was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Board (IRB NO: 202100620B0) of Chang Gung Memorial Hospital, Taoyuan City, Taiwan. Informed consent was waived by the Institutional Review Board (IRB NO: 202100620B0) of Chang Gung Memorial Hospital, Taoyuan City, Taiwan due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chien, RS., Chen, IJ., Lai, CY. et al. Critical distance of the sacroiliac joint for open reduction using screw fixation for traumatic sacroiliac joint diastasis: a retrospective study. J Orthop Surg Res 19, 268 (2024). https://doi.org/10.1186/s13018-024-04759-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04759-z