Abstract
Background
The shoulder joint is the most commonly dislocated joint in the human body, and the recurrence rate exceeds 50% after nonsurgical treatment. Although surgical treatment reduces the recurrence rate, there is controversy regarding the optimal surgical approach. Previous studies suggest that the Latarjet procedure yields favourable outcomes for specific populations at risk of recurrence, such as competitive athletes with significant glenoid defects. However, most of the existing related research consists of nonrandomized controlled trials with small sample sizes, and there is a lack of strong evidence regarding the efficacy and safety of the Latarjet procedure.
Methods
The PubMed, Embase, Cochrane Library, and Web of Science databases were systematically searched. Athletes with ≥ 20% glenoid defects were selected for inclusion. The following data were extracted: general patient information, instability rates, return to sports (RTS) rates, imaging features (graft positioning rate and graft healing rate), functional assessments [Rowe score, Athletic Shoulder Outcome Scoring System(ASOSS), visual analogue scale (VAS), forward flexion function, and external rotation function], and complications.
Results
After excluding suspected duplicate cases, a total of 5 studies were included in this meta-analysis. The studies involved a total of 255 patients, including 237 males (93%) and 18 females (7%). The average age at the time of surgery was 25.4 ± 8.5 years. All the studies had a minimum follow-up period of 2 years, with an average follow-up time of 48.7 ± 18.9 months. The pooled rate of return to sport (RTS) was 94.3% (95% CI: 87.3%, 98.8%), and 86.1% (95% CI: 78.2%, 92.5%) of patients returned to their preoperative level of activity. The pooled redislocation rate was 1.1% (95% CI: 0%, 3.8%). Regarding the imaging results, the combined graft retention rate was 92.1% (95% CI: 88.1%, 95.5%), and the graft healing rate was 92.1% (95% CI: 88%, 95.4%). Postoperative functional evaluation revealed that the combined Rowe score, ASOSS score, and VAS score were 93.7 ± 6.5 points, 88.5 ± 4.4 points, and 1.1 ± 10 points, respectively. The forward flexion and external rotation angles were 170.9 ± 6.9 degrees and 65.6 ± 4.5 degrees, respectively. After excluding one study with unclear complications, the combined complication rate was 9.4% (95% CI: 1.0%, 23.6%).
Conclusion
For athletes with shoulder instability and a total of ≥ 20% glenoid bone defects, the Latarjet procedure can achieve excellent functional outcomes, with the majority of patients returning to preoperative levels of sports activity. This procedure also leads to a low recurrence rate. Therefore, the Latarjet procedure has been proven to be a safe and effective treatment.
Similar content being viewed by others
Introduction
The shoulder joint, which has unique anatomical and biomechanical characteristics, is highly susceptible to instability and is the most commonly dislocated joint in the human body, with a dislocation rate exceeding 50% [1]. More than half of patients with shoulder instability experience recurrence after nonsurgical treatment [2]. This recurrent dislocation not only imposes limitations on daily activities but also significantly correlates with the progression of osteoarthritis [3]. Common surgical procedures include the Bankart and Latarjet procedures. Of these, the Bankart repair is the procedure of choice for most anterior shoulder instabilities, and it has yielded favourable outcomes in numerous studies [4,5,6]. However, for athletes at high risk of recurrent shoulder instability, such as those with ≥ 20% glenoid bone defects, the Bankart repair is still associated with a notable risk of recurrence [5, 7,8,9]. Therefore, the selection of surgical procedures necessitates careful consideration of relevant risk factors [10].
In 1954, Michel Latarjet introduced an open surgical technique involving the transfer of the coracoid to the anterior edge of the glenoid known as the Latarjet procedure [11]. This bone-blocking procedure boasts clear advantages in patients with severe glenoid bone defects [12]. In addition to restoring shoulder stability, early return to sports (RTS) is pivotal, especially for athletes. Nevertheless, the Latarjet procedure is not without complications, with reported complication rates ranging from 7–30% [13,14,15]. Furthermore, a considerable number of patients face challenges in RTS postoperatively [16]. While several clinical trials suggest that the Latarjet procedure results in lower recurrence rates and excellent clinical outcomes for athletes with glenoid defects greater than 20%, almost all similar studies are nonrandomized controlled trials with small sample sizes; therefore, there is a lack of strong evidence regarding the efficacy and safety of the Latarjet procedure for specific populations [17,18,19,20,21]. Thus, this meta-analysis aimed to assess the effectiveness and safety of the Latarjet procedure for treating athletes with glenoid bone defects ≥ 20% and anterior shoulder instability. These findings will provide robust statistical evidence for clinical application.
Method
This meta-analysis was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21].
Search strategy
On November 6, 2023, we systematically searched the PubMed, Embase, Cochrane Library, and Web of Science databases. Our search utilized MeSH terms and free-text keywords, specifically “Athlete” and “latarjet”. The language was restricted to English, with no limitations regarding publication date. Additionally, we scrutinized the reference lists of the included literature and early reviews to ensure that any studies overlooked during the electronic database searches were included.
Inclusion and exclusion criteria
The inclusion criteria for inclusion in this meta-analysis were as follows: (1) had a glenoid bone defect ≥ 20%, (2) had undergone any Latarjet surgical intervention (including classical the Latarjet procedure and other modified procedures), and (3) had an average follow-up time of 2 years or more. The exclusion criteria were as follows: (1) involved other conditions, such as fractures requiring intervention; (2) the sample size was fewer than 10 participants; and (3) included animal experiments, cell studies, reviews, meta-analyses, duplicates, case reports, or letters.
Literature selection
Two authors independently screened the titles and abstracts of all identified studies from the initial search, and they excluded irrelevant literature. Subsequently, both authors meticulously reviewed the full texts of the remaining studies to determine their eligibility. Any discrepancies were resolved through open discussion with other authors.
Data extraction and quality assessment
The following data were extracted: the study design, publication year, patient count, basic demographic information, follow-up time, surgical technique, measurement method for glenoid bone defects, and comprehensive details on functional outcomes and complications. The major outcomes extracted included instability and recurrence rates, with secondary outcomes encompassing the radiologically confirmed graft integration rate, graft healing rate, Rowe score, Athletic Shoulder Outcome Scoring System(ASOSS), visual analogue scale (VAS), forward flexion, external rotation angle measurements, and occurrence of complicationss. The collected data were duplicated and meticulously organized in a Microsoft Excel spreadsheet. The risk of bias assessment was performed using the Joanna Briggs Institute (JBI) evaluator manual, consistent with orthopaedic standards.
Statistical analysis
All variable data in this meta-analysis were analysed using Stata 18 (StataCorp). Chi-square tests and I² tests were employed for heterogeneity assessment, where p < 0.1 indicated statistical significance. In the presence of significant heterogeneity (p < 0.1 and I²> 50%), random effects models were used for analysis; otherwise, fixed effects models were applied [22].
Results
Literature search and study characteristics
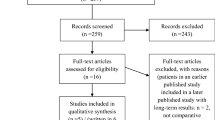
An initial search across four databases (PubMed = 45, Embase = 38, Web of Science = 135, and Cochrane Library = 9) yielded 227 relevant published studies. After excluding 45 duplicate studies using Endnote20, two independent researchers screened the titles and abstracts of the remaining 182 articles, excluding 151 irrelevant studies. Subsequently, a thorough assessment of the remaining 21 articles led to the exclusion of 16 publications due to the unavailability of full texts, noncompliance with the inclusion criteria, or suspected duplicate cases. Finally, five articles [17,18,19,20,21] were included in the meta-analysis, and the PRISMA selection flowchart is shown in Fig. 1.
A total of 5 studies were included in this meta-analysis; these included 3 retrospective case series and 2 retrospective comparative studies. The combined sample size of the 5 studies was 392 patients. Since all the studies were conducted at the same medical institution in Argentina, we carefully examined the characteristics of each case and identified 137 suspected duplicate cases. Despite our efforts to contact the authors for additional data, we were unable to obtain the necessary information. To ensure the accuracy of our analysis, we excluded the suspected duplicate cases and ultimately included 255 patients in this meta-analysis. Among these patients, 237 (93%) were males and 18 (7%) were females. The average age at the time of surgery was 25.4 ± 8.5 years. All the studies had a minimum follow-up period of 2 years, with an average follow-up time of 48.7 ± 18.9 months. Table 1 provides an overview of the key characteristics of the included studies.
For clinical outcome assessment, all five studies reported rates of redislocation, RTS occurrence, radiologically confirmed graft healing, Rowe score, ASOSS score, forward flexion, and external rotation function scores [17,18,19,20,21]. Four studies reported graft integration rates [17, 19,20,21], four reported VAS scores [18,19,20,21], and four provided information on complications [17,18,19, 21], with three studies noting complications [17, 19, 21]. One study lacked detailed complication descriptions for the analysed subgroups and was thus excluded from the complication analysis [20].
Quality assessment results
The risk of bias assessment was performed using the Joanna Briggs Institute (JBI) evaluator manual, which comprises ten items evaluating the quality of case reporting, including case selection, disease or health problem assessment, and case data presentation. The quality assessment details are available in Table 2.
Analysis results
Rate of instability
All five studies included in this meta-analysis, encompassing a total of 255 patients, reported postoperative redislocation information [17,18,19,20,21]. There was a low level of heterogeneity between the studies (I2 = 38.00%, p = 0.168); thus, a fixed effects model was used. The redislocation rate was 1.1% (95% CI = 0%, 3.8%), as shown in Fig. 2.
Return to sports
All five studies included in this meta-analysis, comprising 255 patients, reported information related to RTS after the Latarjet procedure [17,18,19,20,21]. A random effects model was used (I²=71.1%, p = 0.008), and the combined RTS rate was 94.3% (95% CI 87.3%, 98.8%), as shown in Fig. 3A. A random effects model was applied to the proportion of patients who recovered preoperatively (I²=61.5%, p = 0.034), revealing a combined proportion of 86.1% (95% CI = 78.2%, 92.5%), as shown in Fig. 3B.
Radiological outcomes
The radiological outcomes primarily included graft integration rates and graft healing rates, as shown by CT scans at least three months after surgery. Four studies involving 226 patients reported graft integration rates after the Latarjet procedure [17, 19,20,21], with no heterogeneity observed between studies (I²=0%, p = 0.000). The combined postoperative graft integration rate was 92.1% (95% CI 88.1%, 95.5%), as illustrated in Fig. 4A. All four studies, encompassing 226 patients, reported graft healing rates [17,18,19,20,21], with no heterogeneity observed between studies (I²= 0%, p = 0.000). The combined graft healing rate for 255 patients postoperatively was 92.1% (95% CI 88%, 95.4%), as displayed in Fig. 4B.
Functional outcomes
All five studies included in this meta-analysis involving 255 patients reported Rowe scores, ASOSS scores, forward flexion function, and external rotation function scores [17,18,19,20,21]. Four studies involving 195 patients reported VAS scores [18,19,20,21]. The data were extracted at two time points: before surgery and at the latest follow-up. During the meta-analysis, patients were divided into two groups according to postoperative functional outcome scores: the experimental group and the control group. The results showed significant improvements in postoperative Rowe scores, ASOSS scores, VAS scores, and forward flexion function scores compared to preoperative scores. Rowe scores were influenced by heterogeneity (I²= 97.56%, P = 0.00) according to the random effects model (SMD = 8.10;95% CI 5.05, 11.14; P = 0.00); ASOSS scores showed low heterogeneity between studies (I²= 43.93%, P = 0.13) according to the fixed effects model(SMD = 9.09; 95% CI(8.50, 9.67; P = 0.00); VAS scores were influenced by heterogeneity (I²= 78.09%, P = 0.00) according to the random effects model (SMD=-2.13; 95% CI -2.67, -1.59, P = 0.00); forward flexion function scores exhibited low heterogeneity between studies (I²= 48.60%, P = 0.10) according to the fixed effects model (SMD = 0.42; 95% CI 0.25, 0.60; P = 0.00). The external rotation function score was influenced by heterogeneity (I²=57.04%, P = 0.05) according to the random effects model, with no significant difference between the two groups (SMD = 0.21; 95% CI -0.06, 0.47; P = 0.13), as shown in Fig. 5. The average Rowe score, ASOSS score, and VAS score at the latest follow-up were 93.7 ± 6.5, 88.5 ± 4.4, and 1.1 ± 10, respectively. The forward flexion and external rotation angles were 170.9°±6.9° and 65.6°±4.5°, respectively.
A, Forest plot of Rowe scores before and after surgery; B, Forest plot of ASOSS scores before and after surgery; C, Forest plot of VAS scores before and after surgery; D, Forest plot of preoperative and postoperative forward flexion function scores; E, Forest plot of preoperative and postoperative external rotation function scores
Complications
This study examined the postoperative complications of the Latarjet procedure in athletes with unstable shoulder joints and glenoid bone defects ≥ 20%. One study with unclear complications was excluded from the analysis. The overall incidence of complications was 9.4% (95% CI: 1.0%, 23.6%) based on a total of 27 reported cases from 4 studies. Among the 5 patients who experienced recurrence of instability, 2 underwent revision surgery with autologous iliac crest grafts, while 3 received physical therapy; all of these patients were able to return to their presurgical exercise levels. Additionally, two patients reported postoperative shoulder pain, which resolved after arthroscopic screw removal. Four patients developed postoperative infections, all of whom responded well to treatment. Specifically, one patient with intra-articular infection was treated with open lavage, while the other three patients with superficial infection were treated with oral antibiotics. Furthermore, 13 new cases of arthritis were observed after surgery, including 10 cases of mild arthritis and 3 cases of moderate arthritis. No instances of severe arthritis were documented across any of the studies. Graft fragmentation, haematoma, and musculocutaneous neuropraxia each occurred in one patient, and all patients showed improvement following conservative treatment. Detailed information about the complications can be found in Table 3.
Discussion
The most significant finding of this study is that the Latarjet procedure results in excellent functional outcomes and a low recurrence rate for athletes with ≥ 20% glenoid bone defects and anterior shoulder instability. This finding was substantiated by statistical evidence.
The primary objective of restoring patient stability is to prevent the recurrence of instability and facilitate patient return to normal life and work. Athletes, in particular, face heightened demands on shoulder stability and function due to increased physical and competitive stress. Previous research has demonstrated that soft tissue repair surgeries in high-risk athletes are associated with increased recurrence risk [5, 8, 23,24,25]. However, the postoperative instability rate after the Latarjet procedure varies, ranging from 1–16% [26,27,28,29], with a 1.1% recurrence rate in this study. The heterogeneity among studies may be attributed to significant differences in baseline characteristics between studies; for example, Lima et al. [29] focused on females with relatively low shoulder instability rates, while females composed only 7% of the participants in this study. In contrast, clinical study results on RTS rates generally agree. A systematic review revealed that 83% of athletes who underwent bone reconstruction surgery were able to undergo RTS [30]. Hurley et al. [31] evaluated the efficacy of the Latarjet procedure for shoulder instability over a 10-year follow-up and reported an RTS rate of 84.9%, with 76.3% of patients returning to their preoperative activity level. Rassoul et al.‘s [5] systematic review comparing arthroscopic the Bankart repair, arthroscopic Bankart repair with Remplissage (REMP), arthroscopic Latarjet procedure, and open Latarjet procedure showed that open the Latarjet procedure had a similar RTS rate (83.6%), but this rate was significantly lower than that of the arthroscopic Bankart repair (97.5%), REMP (95.5%), and arthroscopic Latarjet procedure (94.0%). Davis et al.‘s [32] study suggested that REMP is superior to simple Bankart repair or the Latarjet procedure, with an RTS rate of 86%. In our study, the postoperative RTS rate was 94.3%, with an average of 86.1% of patients returning to their preoperative activity level. This result is slightly greater than that of previous studies and is similar to the findings of Horinek et al. [33], who considered REMP and the Latarjet procedure to have similar outcomes in patients with shoulder instability and > 15 glenoid defects.
Hurley et al. [31] evaluated the clinical efficacy of the Latarjet procedure for shoulder instability over a 10-year follow-up and reported an average Rowe score of 88.5. Horinek et al. [34] assessed VAS scores and forward flexion and external rotation angles and reported average VAS scores of 2.2 preoperatively and 1.3 at the last follow-up; forward flexion angles of 171° preoperatively and 178° at the last follow-up; and external rotation angles of 64° preoperatively and 82° at the last follow-up. Rossi et al. [35] evaluated ASOSS scores in a cohort study of athletes and reported an average preoperative ASOSS score of 53.1 and an average score of 93.7 at the last follow-up. The specific reasons for the difference in external rotation function are unknown, but there is a noticeable difference in measuring 0° abduction passive external rotation and 90° abduction passive external rotation. However, existing studies do not provide detailed descriptions. Current research suggests that the Latarjet procedure may result in a decrease of approximately 5° in the external rotation angle, necessitating proactive rehabilitation exercises postoperatively [28].
The other results in our study align closely with previous ones. The majority of patients achieved good to excellent scores, indicating satisfactory functional outcomes for this patient group. Additionally, biomechanical studies suggest a negative correlation between the incidence of glenoid defects and shoulder joint stability, with a glenoid defect of 20% considered a critical threshold for recurrence in Bankart repair treatment for shoulder instability [36, 37]. Like glenoid defects, shoulder instability in young athletes is a risk factor for postoperative recurrence after surgery [23]. Therefore, the population included in this meta-analysis had relatively greater risk factors for recurrence than did the population included in the aforementioned studies.
The occurrence rate of adverse events after the Latarjet procedure is significant, with Mizuno et al. [38] reporting a 20% incidence of bony arthritis changes in an average 20-year follow-up after the Latarjet procedure. Recently, Hurley et al. [31] conducted a systematic review evaluating the long-term risk of bony arthritis after the Latarjet procedure and reported a 38.2% incidence of arthritis changes in patients followed for at least 10 years. In this study, with a minimum follow-up time of 2 years, the combined incidence of new arthritis was 3.9%,with no evidence of severe bony arthritis changes. Other adverse events included graft nonhealing, haematoma, and infection, consistent with previous research [28, 39,40,41]. While earlier studies provided high-quality research evidence through long-term follow-up, a series of changes, including surgical instruments and continued education stemming from long-term follow-up, also impact postoperative functional outcomes. In this study, the Latarjet procedure for athletes with glenoid bone defects ≥ 20% and anterior shoulder instability demonstrated favourable functional outcomes.
Despite these notable findings, this study has certain limitations. First, there was considerable heterogeneity between the included studies, particularly in terms of baseline patient characteristics. Second, the studies included in this analysis had small sample sizes and lacked control groups. As a result, our assessment focused primarily on efficacy and risk, with no definitive evidence establishing the superiority of the Latarjet procedure over alternative interventions. Additionally, despite the consistent use of assessment methods in the included literature to mitigate bias, the homogeneity in the geographic origin and medical institution of all studies, coupled with a relatively limited sample size and predominantly male patients, necessitates caution in extrapolating these results to broader populations. Consequently, larger-scale randomized controlled trials should be meticulously designed to confirm the clinical efficacy of the Latarjet procedure compared with other interventions across diverse patient cohorts.
Conclusion
In summary, this meta-analysis provides robust evidence supporting the Latarjet procedure’s exceptional functional outcomes for athletes with glenoid bone defects ≥ 20%. The majority of patients exhibited a successful return to sports preoperatively, and there was a low recurrence rate, suggesting that the Latarjet procedure is a safe and effective therapeutic option in clinical practice. However, due to the inherent limitations of limited clinical data, future research should include multicentre randomized controlled trials featuring extended follow-up periods to substantiate and refine these findings.
Data availability
No datasets were generated or analysed during the current study.
References
Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542–9. https://doi.org/10.2106/JBJS.I.00450.
Hovelius L, Olofsson A, Sandstrom B, Augustini BG, Krantz L, Fredin H, Tillander B, Skoglund U, Salomonsson B, Nowak J, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90:945–52. https://doi.org/10.2106/JBJS.G.00070.
Verweij L, Pruijssen EC, Kerkhoffs G, Blankevoort L, Sierevelt IN, van Deurzen D, van den Bekerom M. Treatment type may influence degree of post-dislocation shoulder osteoarthritis: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29:2312–24. https://doi.org/10.1007/s00167-020-06263-3.
Garcia GH, Taylor SA, Fabricant PD, Dines JS. Shoulder instability management: a Survey of the American shoulder and elbow surgeons. Am J Orthop (Belle Mead NJ). 2016;45:E91–7.
Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to Sport after Surgical Treatment for Anterior Shoulder instability: a systematic review. Am J Sports Med. 2019;47:1507–15. https://doi.org/10.1177/0363546518780934.
Pathak S, Haidermota MJ, Sancheti HV. Arthroscopic bankart and remplissage for Anteroinferior Instability with Subcritical Bone loss has a low recurrence rate. Arthrosc Sports Med Rehabil. 2022;4:e695–e703. https://doi.org/10.1016/j.asmr.2021.12.014.
Nakagawa S, Mae T, Sato S, Okimura S, Kuroda M. Risk factors for the postoperative recurrence of instability after arthroscopic bankart repair in athletes. Orthop J Sports Med. 2017;5:1808773918. https://doi.org/10.1177/2325967117726494.
Kukkonen J, Elamo S, Flinkkila T, Paloneva J, Mantysaari M, Joukainen A, Lehtinen J, Lepola V, Holstila M, Kauko T, et al. Arthroscopic bankart versus open latarjet as a primary operative treatment for traumatic anteroinferior instability in young males: a randomised controlled trial with 2-year follow-up. Br J Sports Med. 2022;56:327–32. https://doi.org/10.1136/bjsports-2021-104028.
Verweij L, van Spanning SH, Grillo A, Kerkhoffs G, Priester-Vink S, van Deurzen D, van den Bekerom M. Age, participation in competitive sports, bony lesions, ALPSA lesions, > 1 preoperative dislocations, surgical delay and ISIS score > 3 are risk factors for recurrence following arthroscopic Bankart repair: a systematic review and meta-analysis of 4584 shoulders. Knee Surg Sports Traumatol Arthrosc. 2021;29:4004–14. https://doi.org/10.1007/s00167-021-06704-7.
Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470–7. https://doi.org/10.1302/0301-620X.89B11.18962.
LATARJET M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–7.
Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BJ, Dewing CB, LeClere L, Romeo AA. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92(Suppl 2):133–51. https://doi.org/10.2106/JBJS.J.00906.
Hendy BA, Padegimas EM, Kane L, Harper T, Abboud JA, Lazarus MD, Romeo AA, Namdari S. Early postoperative complications after Latarjet procedure: a single-institution experience over 10 years. J Shoulder Elb Surg. 2021;30:e300–8. https://doi.org/10.1016/j.jse.2020.09.002.
Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V, Latarjet. Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:1184–211. https://doi.org/10.1016/j.arthro.2014.04.005.
Williams H, Evans JP, Furness ND, Smith CD. It’s not all about redislocation: a systematic review of complications after anterior shoulder stabilization surgery. Am J Sports Med. 2019;47:3277–83. https://doi.org/10.1177/0363546518810711.
Rossi LA, Tanoira I, Brandariz R, Pasqualini I, Ranalletta M. Reasons why athletes do not return to sports after arthroscopic Bankart repair: a comparative study of 208 athletes with Minimum 2-Year follow-up. Orthop J Sports Med. 2021;9:941618450. https://doi.org/10.1177/23259671211013394.
Rossi LA, Tanoira I, Bruchmann MG, Pasqualini I, Ranalletta M. The Latarjet procedure in competitive athletes younger than 20 years old with a significant glenoid bone loss. Shoulder Elb. 2022;14:21–8. https://doi.org/10.1177/1758573220944166.
Brandariz RN, Gorodischer TD, Pasqualini I, Rossi LA, Tanoira I, Ranalletta M. The Latarjet Procedure without Remplissage is effective to Restore Stability in athletes with glenoid bone defects Greater Than 25% and off-Track Hill-Sachs lesions. Arthroscopy. 2021;37:2455–61. https://doi.org/10.1016/j.arthro.2021.03.048.
Ranalletta M, Rossi LA, Bertona A, Tanoira I, Maignon GD, Bongiovanni SL. Modified Latarjet Procedure without Capsulolabral Repair for the treatment of failed previous operative stabilizations in athletes. Arthroscopy. 2018;34:1421–7. https://doi.org/10.1016/j.arthro.2017.12.006.
Rossi LA, Bertona A, Tanoira I, Maignon GD, Bongiovanni SL, Ranalletta M. Comparison between modified Latarjet Performed as a primary or Revision Procedure in competitive athletes: a comparative study of 100 patients with a Minimum 2-Year follow-up. Orthop J Sports Med. 2018;6:1809864657. https://doi.org/10.1177/2325967118817233.
Rossi LA, Tanoira I, Gorodischer T, Pasqualini I, Ranalletta M. Similar results in return to sports, recurrences, and Healing Rates between the Classic and Congruent-Arc Latarjet for athletes with recurrent glenohumeral instability and a failed stabilization. Arthroscopy. 2020;36:2367–76. https://doi.org/10.1016/j.arthro.2020.05.013.
Yao H, Chen X, Tan X. Efficacy and safety of apatinib in the treatment of osteosarcoma: a single-arm meta-analysis among Chinese patients. BMC Cancer. 2021;21:449. https://doi.org/10.1186/s12885-021-08154-3.
Asker M, Brooke HL, Walden M, Tranaeus U, Johansson F, Skillgate E, Holm LW. Risk factors for, and prevention of, shoulder injuries in overhead sports: a systematic review with best-evidence synthesis. Br J Sports Med. 2018;52:1312–9. https://doi.org/10.1136/bjsports-2017-098254.
Alkaduhimi H, van der Linde JA, Willigenburg NW, Paulino PN, van Deurzen DF, van den Bekerom MP. Redislocation risk after an arthroscopic Bankart procedure in collision athletes: a systematic review. J Shoulder Elb Surg. 2016;25:1549–58. https://doi.org/10.1016/j.jse.2016.05.002.
Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006;22:947–53. https://doi.org/10.1016/j.arthro.2006.05.015.
An VV, Sivakumar BS, Phan K, Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elb Surg. 2016;25:853–63. https://doi.org/10.1016/j.jse.2015.11.001.
Jeon YS, Jeong HY, Lee DK, Rhee YG. Borderline Glenoid Bone defect in anterior shoulder instability: Latarjet Procedure Versus Bankart Repair. Am J Sports Med. 2018;46:2170–6. https://doi.org/10.1177/0363546518776978.
Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elb. 2018;10:15–24. https://doi.org/10.1177/1758573217728716.
Lima E, Oses GL, de Godoy GP, Lara P, Ribeiro LM, de Figueiredo EA, Pochini AC, Andreoli CV, Belangero PS, Ejnisman B. Evaluation of Latarjet procedure in female athletes: a 3-year follow-up prospective cohort study. JSES Int. 2022;6:343–8. https://doi.org/10.1016/j.jseint.2022.01.007.
van Iersel TP, van Spanning SH, Verweij L, Priester-Vink S, van Deurzen D, van den Bekerom M. Why do patients with anterior shoulder instability not return to sport after surgery? A systematic review of 63 studies comprising 3545 patients. JSES Int. 2023;7:376–84. https://doi.org/10.1016/j.jseint.2023.01.001.
Hurley ET, Jamal MS, Ali ZS, Montgomery C, Pauzenberger L, Mullett H. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: a systematic review of studies at 10-year follow-up. J Shoulder Elb Surg. 2019;28:e33–9. https://doi.org/10.1016/j.jse.2018.08.028.
Davis WH, DiPasquale JA, Patel RK, Sandler AB, Scanaliato JP, Dunn JC, Parnes N. Arthroscopic remplissage combined with Bankart Repair results in a higher rate of return to Sport in athletes compared with Bankart Repair alone or the Latarjet Procedure: a systematic review and Meta-analysis. Am J Sports Med. 2023;51:3304–12. https://doi.org/10.1177/03635465221138559.
Horinek JL, Menendez ME, Narbona P, Ladermann A, Barth J, Denard PJ. Arthroscopic Bankart Repair with Remplissage as an alternative to Latarjet for Anterior Glenohumeral Instability with more than 15% glenoid bone loss. Orthop J Sports Med. 2022;10:951747313. https://doi.org/10.1177/23259671221142257.
Horinek JL, Menendez ME, Narbona P, Ladermann A, Barth J, Denard PJ. Remplissage yields similar 2-Year outcomes, fewer complications, and low recurrence compared to Latarjet across a wide range of Preoperative Glenoid Bone loss. Arthroscopy. 2022;38:2798–805. https://doi.org/10.1016/j.arthro.2022.03.031.
Rossi LA, Tanoira I, Gorodischer T, Pasqualini I, Ranalletta M. Recurrence and revision rates with arthroscopic Bankart Repair compared with the Latarjet Procedure in Competitive Rugby players with Glenohumeral instability and a glenoid bone loss < 20. Am J Sports Med. 2021;49:866–72. https://doi.org/10.1177/0363546520988154.
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. https://doi.org/10.2106/00004623-200001000-00005.
Nacca C, Gil JA, Badida R, Crisco JJ, Owens BD. Crit Glenoid Bone Loss Posterior Shoulder Instability. 2018;46:1058–63. https://doi.org/10.1177/0363546518758015.
Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elb Surg. 2014;23:1691–9. https://doi.org/10.1016/j.jse.2014.02.015.
Marjanovic B, Poberaj B, Kolar M, Nabergoj M, Kopac C, Gosnik B, Merkac J, Mirnik N. 11% complications rate after Latarjet procedure at up to 14 years follow-up. Musculoskelet Surg. 2022;106:227–37. https://doi.org/10.1007/s12306-021-00697-9.
Garcia JJ, Do AF, Belchior RJ, de Carvalho LQ, Markarian GG, Montero E. Comparative systematic review of fixation methods of the Coracoid and Conjoined Tendon in the Anterior Glenoid to treat anterior shoulder instability. Orthop J Sports Med. 2019;7:1809867963. https://doi.org/10.1177/2325967118820539.
Malahias MA, Fandridis E, Chytas D, Chronopulos E, Brilakis E, Antonogiannakis E. Arthroscopic versus open latarjet: a step-by-step comprehensive and systematic review. Eur J Orthop Surg Traumatol. 2019;29:957–66. https://doi.org/10.1007/s00590-019-02398-3.
Acknowledgements
Not applicable.
Funding
Foundation item: The key project of construction of clinical center of Yunnan Provincial Health Commission (Project Number: ZX20191001). Grants from Yunnan Orthopedics and Sports Rehabilitation Clinical Medicine Research Center (Project Number: 202102AA310068).
Author information
Authors and Affiliations
Contributions
LW, SRH conceived and coordinated the study, designed, performed, and wrote the paper. XW, XYL carried out the data collection,TW, HBT carried out revised the paper. All authors reviewed the results and approved the final version of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
The data, including any individual details and images of individuals involved in this study, have been approved by the patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, L., He, S., Wu, X. et al. Efficacy and safety of the Latarjet procedure for the treatment of athletes with glenoid bone defects ≥ 20%: a single-arm meta-analysis. J Orthop Surg Res 19, 159 (2024). https://doi.org/10.1186/s13018-024-04641-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04641-y