Abstract
Background
Prevalence information is the first step in developing preventive procedures or health services. This study was conducted to systematically evaluate the epidemiology of osteoporotic fractures in Chinese elderly aged ≥ 60 years and to provide evidence-based evidence for the prevention and treatment of osteoporotic fractures.
Methods
We identified relevant studies by searching the literature published in PubMed, Web of Science, Cochrane Library, Embase, CNKI, Wanfang Data, and VIP databases from the establishment of the database until August 2022. We used a random-effects model to obtain prevalence estimates and identified sources of heterogeneity and comparisons of prevalence among different groups through subgroup analysis and sensitivity analysis.
Results
A total of 29 articles were included in this study, and the prevalence of osteoporosis fractures in elderly Chinese was high (18.9%). The prevalence has increased significantly over the past decade (from 13.2% in 2000–2010 to 22.7% in 2012–2022). The prevalence of osteoporosis is higher in women than in men (18.5% vs 14.3%) and increases with age. The northern region was higher than the southern region (20.3% vs 18.9%), and the spine, hip, and distal forearm were the most common sites of fracture.
Conclusion
The prevalence of osteoporotic fractures in the Chinese elderly is 18.9%, and timely prevention and treatment are necessary.
Similar content being viewed by others
Introduction
Osteoporotic fracture is a fracture caused by a low-energy external force, which is a serious consequence of osteoporosis [1]. Osteoporosis can lead to decreased bone strength and increased bone fragility, also known as fragility fractures. The high-risk groups for osteoporotic fractures are mainly the elderly and postmenopausal women. Fractures are mainly in important parts such as the lumbar spine, thoracic spine, and hip joints, and there is a risk of further fractures [2].
Osteoporotic fracture is a significant problem in the field of public health the world [3, 4]. It not only seriously affects the physical and mental health of elderly patients but also causes a substantial economic burden to the family and society [5,6,7]. The mortality and disability rate of osteoporotic fractures is very high. Studies have shown that the mortality rate of some elderly patients in the first year after hip fracture is as high as 17.1–33.0% [8, 9]; the 4-year mortality rate of conservative treatment of osteoporotic vertebral compression fractures (OVCF) can also be as high as 49.4% [10]. The number of patients with osteoporotic fractures is also huge. According to the International Osteoporosis Foundation [11], among middle-aged and older people over 50 years old, about 1/2 of women and 1/5 of men will experience at least one osteoporotic fracture, and 50% of patients may also have secondary fractures. Chinese scholars predict that [12]: it is expected that by 2035, China, will add about 4.83 million cases of osteoporotic fractures; approximately 5.99 million new topics will be added in 2050. The expenses for osteoporotic fractures in significant parts of the Chinese medical system will increase to 132 billion RMB and 163 billion RMB in 2035 and 2050, respectively.
Information on the prevalence of osteoporotic fractures in older adults is the first step in developing preventive procedures or health services for older adults. The problem of our study is the prevalence of osteoporotic fractures in Chinese ≥ 60 year olds. By systematically evaluating the epidemiology of osteoporotic fractures in Chinese ≥ 60 year olds, we can provide evidence-based evidence for the prevention and treatment of osteoporotic fractures.
Methods
Search strategy
This systematic review and meta-analysis were designed, conducted, and reported by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [13]. The ID number registered on Prospero is CRD42023383566. The following algorithm guided the preliminary search:
-
Search strategy
-
P (population): ≥ 60-year-old Chinese seniors
-
I (intervention): no interventions
-
C (comparisons): no comparisons
-
(outcomes): prevalence of osteoporotic fractures in older Chinese people
-
S (study): cross-sectional study
Literature search
The literature search process was conducted by two authors (SL.M; MH.T) independently conducted and the search process started in August 2022. We searched PubMed, Web of Science, Cochrane Library, Embase, CNKI, Wan Fang Data, and VIP database from establishing the database to August 1, 2022. The “subject word + free word” method was used for retrieval. Chinese search terms: “osteoporotic fracture”, “brittle fracture”, “low energy fracture”, “morbidity”, “prevalence”, “epidemiology”; English search terms: “Osteoporotic Fractures”, “OPF”, “fragility fracture”, “prevalence”, “incidence”, “epidemiology”, “China”, “Chinese”. According to the authors’ language capabilities, language of publication was restricted to English and Chinese. The PubMed search formula is as follows ((((Osteoporotic Fractures[All Fields]) OR (fragility fracture[All Fields]))) OR (OPF[All Fields])) AND (((prevalence[All Fields]) OR (epidemiologic[All Fields])) OR (incidence[All Fields]))) AND ((Chinese[All Fields]) OR (China[All Fields])). The literature retrieval process takes PubMed as an example, See Fig. 1.
Study inclusion and exclusion criteria
Inclusion criteria: (1) According to the authors’ language capabilities, articles in English, Chinese were eligible. (2) Epidemiological study of osteoporotic fractures in China or Chinese population. (3) The study group included people aged 60 years and older. (4) The prevalence of osteoporotic fractures can be calculated. (5) Cross-sectional study.
Exclusion criteria: (1) The full text or result data cannot be obtained and needs to be completed or missing. (2) The same study was published in different journals. (3) The sample size of the elderly was too small. (≤ 100) (4) Research results published in the form of review, conference summary, expert consensus, etc.
Data extraction and outcomes of interests
The retrieved literature was imported into EndNote software. Firstly, the duplicate literature was screened out, the title and abstract were read, and the research unrelated to the research problem was eliminated. Finally, the remaining literature was read in full text, included, and destroyed according to the inclusion and exclusion criteria. In this process, two evaluators (S-L.M. and M-H.T.) repeatedly cross-checked the included literature. A dispute will be resolved by discussing it between the two parties or introducing the third evaluator (Y.Y) for review.
The primary data extracted are as follows: (1) Basic information included in the literature: author, year of publication, survey area, etc. (2) Calculate the relevant data of the prevalence of osteoporotic fractures (Case Size, Sample Size, etc.); (3) critical information of bias risk assessment.
Methodological quality assessment
The literature quality evaluation criteria proposed by KHAMBALIA, SEEN [14] were used to evaluate and record the quality of the included literature, as shown in Table 1.
Statistical analysis
We used Stata17.0 software to analyze the prevalence data. The classification of heterogeneity depends on I2 statistics [15]: < 25% indicates low level, 25–50% indicates moderate level, and > 50% indicates high heterogeneity. We used a random effects model to estimate the prevalence of osteoporotic fractures, five subgroups were set up: gender (male and female), age group (60–69, 70–79, ≥ 80), region (South, North), publication time (2000–2010, 2012–2022), and fracture site (vertebra, hip, distal forearm, and others). Sensitivity analysis was performed by eliminating references one by one, and statistical significance P-values were set at 0.05 in all statistical analyses. In this study, we did not examine publication bias. Publication bias refers to the fact that studies with significant results are more likely to be published than studies with non-significant results, which can lead to systematic differences between published and unpublished studies [16]. However, observational studies of prevalence do not have significant or negligible results, and it is not recommended to use mature methods to test for this bias in systematic reviews of prevalence studies. Therefore, we did not examine publication bias.
Results
Search result
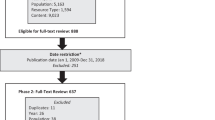
After searching, a total of 7373 articles were obtained. After the layer-by-layer screening, 29 studies [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] were finally included, with a total of 85,944 subjects. The literature screening process and results are shown in Fig. 2.
Basic characteristics and quality assessment results of included studies
The essential characteristics of the included studies are shown in Table 2. The quality evaluation results of the included studies were as follows: there is 1 article [17] of one point, 7 [18, 21, 22, 24, 36, 41, 42] articles of two points, 13 articles [19, 20, 23, 27, 29,30,31,32, 35, 40, 43,44,45] of three points, 5 articles [28, 33, 37,38,39] of four points, and 3 articles [25, 26, 34] of five points. (See Additional file 1 for details).
Meta-analysis results
A total of 29 studies involving 85,944 older adults were included in this study. After meta-analysis, the prevalence of osteoporotic fractures in older people in China was 18.9% [95% CI (16.5%, 21.4%)] (See Fig. 3).
Subgroup analysis
In this study, we set five subgroups: region (South, North)—Qinling-Huaihe as the boundary, north of Qinling-Huaihe as the north, south as the south, gender (men and women), age group (60–69, 70–79, ≥ 80), publication time (2000–2010, 2012–2022), and fracture site (vertebra, hip, distal forearm, and others). The specific results of subgroup analysis are shown in Table 3.
Sensitivity analysis
We used the method of sequentially eliminating individual studies and recombining the total effect size to analyze the sensitivity of the total prevalence. The results showed that the majority of osteoporotic fractures in the elderly in China was between 16.0 and 21.0%, and there was no directional degeneration in each development, suggesting that the research results were relatively stable (See Fig. 4).
Discussion
Our results show that osteoporotic fractures in the elderly in China have the following characteristics: First, the prevalence rate of osteoporotic fractures in women is higher than that in men in the same age group. Secondly, according to age, the prevalence rate of people over 80 years old is the highest, followed by 70–79 years old, and finally 60–69 years old. Third, the prevalence rate in the north is higher than that in the south. Fourth, the prevalence of osteoporotic fractures has increased significantly in the past decade (from 13.2% in 2000–2010 to 22.7% in 2012–2022). Fifth, the common sites of osteoporotic fractures are the spine, hip, and distal forearm. Finally, the prevalence of osteoporotic fractures among the Chinese elderly is high (18.9%), and the related prevention and treatment should not be relaxed.
The root cause of osteoporotic fracture lies in osteoporosis. Osteoporosis can lead to the destruction of bone fine structure, the decrease in bone mass, and the decrease in bone strength. it is very easy to cause a fracture when exposed to slight external force in daily life. One of the main risk factors for osteoporosis is gender, which is an unalterable factor. According to a comprehensive study in Iraq, the prevalence of osteoporosis is 12% in men, 3% in premenopausal women, and 19% in postmenopausal women, indicating significant gender differences [46]. There are similar results in the USA (4.5% vs 15.4%) [47]. The reason for this difference may be related to the rapid bone loss caused by the rapid decline of ovarian function and the decrease in estrogen levels in postmenopausal women. The longer the time of menopause, the more obvious the decrease in bone mineral density, resulting in osteopenia and further development of osteoporosis, increasing the risk of osteoporotic fracture [39]. Previous studies have shown that women lose about 55% of their body bone mass in their lifetime, while men lose about 35% of their body bone mass [48]. Gender is an important factor leading to osteoporosis and osteoporotic fracture. Women can take menopause as an important time point for the prevention and treatment of osteoporotic fractures and intervene in time. Aging is another unchangeable factor, and the South Korean National Health and Nutrition Survey (KNHANES) shows a significant age difference [49]. A large-scale survey in Austria shows that the prevalence of osteoporosis increases with age [50]. A cohort study showed that young participants diagnosed with osteoporosis had a higher prevalence of osteoporosis than older participants (35% vs 10.0%). It has been recognized that bone mineral density (BMD) decreases with age after reaching the optimal value. A clinical study involving 17,083 subjects showed that bone mass reduction rates in women aged 50–64 and ≥ 65 years old were 31% and 62%, respectively [51]. Our research is consistent with these studies. The region is also an unchangeable factor. The prevalence rate in the north is higher than that in the south, which is consistent with some previous studies. The prevalence of osteoporosis in northern Iraq is higher than that in southern Iraq, and the regional differences are due to differences in vitamin D levels. It is reported that vitamin D3 synthesis may not be sufficient to explain the decrease in BMD due to the lack of ultraviolet light at high latitudes [52]. In addition, the climatic environment may also affect the prevalence of osteoporotic fractures to some extent. The climate in the north is cold, and the roads are icy. In a cold environment, people's clothing will be thicker, physical flexibility will decrease, coupled with road icing, slippery roads, and other factors, will increase the chance of fall injury, leading to an increase in the prevalence of fractures. However, the specific mechanism behind this difference is not clear. The common sites of osteoporotic fractures were the spine (11.6%), hip (4.5%), and distal forearm (3.0%). The location of fracture is mainly related to physiological factors, specific anatomical location, and stress mode. Previous studies have also shown that [3]: the common sites of osteoporotic fractures are vertebrae (thoracic and lumbar vertebrae), hip (proximal femur), distal forearm, and other key parts, such as ribs, fibula, and other parts. In addition, in the past 10 years, the prevalence rate of osteoporotic fractures in the elderly in China has been on the rise. From 13.2% in 2000–2010 to 22.7% in 2012–2022, this difference may be caused by differences in health and medical resources between the past and the present.
Most of the diagnostic criteria for osteoporotic fractures included in the study were “osteoporosis + fracture-related diagnosis”. BMD based on DXA is the current “gold standard” for diagnosing osteoporosis, but DXA can be measured at the lumbar spine, proximal femur, or left forearm (non-dominant distal radius 1/3) [53]. Due to the different conditions of bone loss in different parts, the BMD measurement results were significantly different [54]. This condition may affect the prevalence of osteoporosis and osteoporotic fractures. In this study, we also noted that some of the included studies supplemented the detection of bone metabolic markers in the diagnosis of osteoporotic fractures. Relevant studies have shown that some bone metabolic markers (BTM) have great potential in monitoring the degree of osteoporosis progression [55, 56].
At present, according to China's Seventh National population Census [57]: China has 264 million people over 60 (about 18.7% of the total population), and more than 190 million people over 65 (about 13.5% of the total population), making it the country with the largest elderly population in the world. In addition, the relevant osteoporosis epidemiological survey showed that [58]: the prevalence rate of osteoporosis was 19.2% in people over 50 years old, including 32.1% in women and 6.9% in men. The prevalence rate of osteoporosis in people over 65 years old is 32.0%, including 51.6% in women and 10.7% in men. The prevalence rate of osteoporosis in women (32.1% over 50 years old) was significantly higher than that in Europe, America, Japan, and South Korea (16.5% in the USA, 15.8% in Canada, and 38.0% in South Korea). At present, osteoporosis has become the third largest chronic disease harmful to human health after cardiovascular disease and diabetes. Osteoporotic fractures are a disease of fundamental importance prevalent in global health systems, and their incidence is minimized by proper management [59]. Given the current situation in China, proactive prevention and control measures are needed to raise citizens' awareness of the situation through a three-step prevention plan. In addition, it is also necessary to actively evaluate the efficacy and safety of anti-osteoporosis drugs, which can refer to relevant foreign studies [60, 61]. Timely intervention and treatment of osteoporosis are the key to prevent osteoporotic fractures.
This is the first systematic review and meta-analysis of the prevalence of osteoporotic fractures in the elderly in China, and relevant prevalence information is the first step in developing preventive procedures or health care services for the elderly population. In addition, the relevant data obtained in our study have many potential benefits in clinical application, which need to be further explored such as screening for the disease, recommended screening tools, and so on. We searched in detail through multiple databases to avoid missing important evidence. Included studies were analyzed using a standardized process, and included studies were evaluated for quality, heterogeneity, sensitivity, etc. Subgroups were set up based on sex, age, region, publication time, fracture site, and subgroup analysis to gain more insight into the possible causes of heterogeneity between studies. The study also has some limitations. First, we collected representative data for each region but differed in terms of sample source, sample size, diagnostic criteria, etc., which may affect comparisons between included studies. Secondly, the heterogeneity of the included studies was high, and the source of heterogeneity could not be found through sensitivity analysis and subgroup analysis. Third, the number of groups is relatively small, and the representativeness may be affected to some extent.
Future studies should mitigate the degree of heterogeneity by conducting additional subgroups to investigate other relevant risk factors. Secondly, subgroup analysis does not imply any causal variables. Therefore, more studies need to be recruited from longitudinal follow-up studies and use meta regression techniques to identify predictors of osteoporotic fractures. Finally, further research should also investigate osteoporotic fractures in middle-aged adults to accelerate the design and implementation of targeted therapies to prevent or mitigate the progression of osteoporotic fractures in community and clinical settings.
Conclusion
In the past 10 years, the prevalence of osteoporotic fractures in the older age group ≥ 60 has increased in China. The prevalence of osteoporotic fractures increases with age, higher in women than in men and higher in the north than in the south. With the increasing prevalence of osteoporotic fractures, the relevant prevention and control measures in the health sector become more important.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Chinese Society of Osteology. Guidelines for the diagnosis and treatment of osteoporotic fractures (2022). Chin J Orthopaed. 2022;42(22):1473–91.
Osteoporosis Prevention and Rehabilitation Committee of Chinese Rehabilitation Society.Chinese expert consensus on secondary prevention of osteoporotic fractures. Chin Med 2022;102(45): 3581–3591.
Lems WF, Dreinhöfer KE, Bischoff-Ferrari H, et al. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis. 2017;76(5):802–10. https://doi.org/10.1136/annrheumdis-2016-210289.
Willson T, Nelson SD, Newbold J, et al. The clinical epidemiology of male osteoporosis: a review of the recent literature. Clin Epidemiol 2015;7:65–76. https://doi.org/10.2147/clep.S40966.
Jang S-Y, Cha Y, Lee JC, et al. Population-based analysis for risk of suicide death in elderly patients after osteoporotic fracture: a nested case-control study. J Korean Med Sci. 2021;36(36):e225. https://doi.org/10.3346/jkms.2021.36.e225.
Johansson L, Svensson HK, Karlsson J, et al. Decreased physical health-related quality of life-a persisting state for older women with clinical vertebral fracture. Osteoporos Int. 2019;30(10):1961–71. https://doi.org/10.1007/s00198-019-05044-0.
Diem SJ, Lui L-Y, Langsetmo L, et al. Effects of mobility and cognition on maintenance of independence and survival among women in late life. J Gerontol A Biol Sci Med Sci. 2018;73(9):1251–7. https://doi.org/10.1093/gerona/glx209.
Hori K, Siu AM, Nguyen AN, et al. Osteoporotic hip fracture mortality and associated factors in Hawai’i. Arch Osteoporos. 2020;15(1):183. https://doi.org/10.1007/s11657-020-00847-9.
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14(1):203. https://doi.org/10.1186/s13018-019-1226-6.
Edidin AA, Ong KL, Lau E, et al. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the medicare population. Spine. 2015;40(15):1228–41. https://doi.org/10.1097/brs.0000000000000992.
Geusens P, Bours SPG, Wyers CE, et al. Fracture liaison programs. Best Pract Res Clin Rheumatol. 2019;33(2):278–89. https://doi.org/10.1016/j.berh.2019.03.016.
Si L, Winzenberg TM, Jiang Q, et al. Projection of osteoporosis-related fractures and costs in China: 2010–2050. Osteoporos Int. 2015;26(7):1929–37. https://doi.org/10.1007/s00198-015-3093-2.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1.
Khambalia AZ, Seen LS. Trends in overweight and obese adults in Malaysia (1996–2009): a systematic review. Obes Rev. 2010;11(6):403–12. https://doi.org/10.1111/j.1467-789X.2010.00728.x.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Easterbrook PJ, Berlin JA, Gopalan R, et al. Publication bias in clinical research. Lancet (London, England). 1991;337(8746):867–72. https://doi.org/10.1016/0140-6736(91)90201-y.
Xia W, Liu Q, Lv J, et al. Prevalent vertebral fractures among urban-dwelling Chinese postmenopausal women: a population-based, randomized-sampling, cross-sectional study. Arch Osteoporos. 2022;17(1):120. https://doi.org/10.1007/s11657-022-01158-x.
Lo SST. Prevalence of osteoporosis in elderly women in Hong Kong. Osteoporosis Sarcopenia. 2021;7(3):92–7. https://doi.org/10.1016/j.afos.2021.09.001.
Zhang CX, Nie JS, Xue XH, et al. Prevalence and risk factors of osteoporotic fracture in menopausal women. Prev Med Inf J. 2020;36(09):1212–6.
Chai B. Epidemiological study on the prevalence of osteoporosis and vertebral fracture in postmenopausal women in Xiaodian district of Taiyuan City. Shanxi: Shanxi Medical University; 2019.
Ju ZY. Epidemiological study of osteoporotic vertebral fractures in Shanghai residents over 60 years old. Shanghai: Shanghai Jiao Tong University; 2018.
Gao C. An epidemiological survey of osteoporosis and vertebral fractures in postmenopausal women and elderly men in Shanghai. Shanghai: Shanghai Jiao Tong University; 2017.
Chen X, Chen BL, Wang J, et al. Incidence of thoracolumbar compression fractures in elderly aged 65 years and above in a community in Shanghai. Shanghai Med. 2017;38(10):41–3.
Cui L, Chen L, Xia W, et al. Vertebral fracture in postmenopausal Chinese women: a population-based study. Osteoporos Int. 2017;28(9):2583–90. https://doi.org/10.1007/s00198-017-4085-1.
Ma ZJ, Suo ZG, Ma R, et al. Epidemiological investigation and analysis of osteoporotic fractures in middle-aged and elderly people. Med Inf. 2016;29(18):403–4. https://doi.org/10.3969/j.issn.1006-1959.2016.18.370
Chen XH, Shen H, Xia JQ. Epidemiological characteristics and related factors of osteoporotic fractures in middle-aged and elderly people. Chin J Gerontol. 2016;36(13):3299–301.
Chen L, Cheng J, Li B, et al. Epidemiological survey of osteoporosis in the elderly in northeast Chongqing. Chin J Osteoporosis. 2016;22(08):1050–2.
Xu F, Tian Y. Analysis of pathogenic factors and characteristics of 8563 cases of osteoporotic fracture. Mod Diagn Ther. 2015;26(17):3928–9.
Li ZJ, Zhang Y, Gu QS, et al. Epidemiological investigation of osteoporotic fractures in elderly people in Wenjiang district, Chengdu. Sichuan Med. 2015;36(02):156–9. https://doi.org/10.16252/j.cnki.issn1004-0501-2015.02.008
Wu AG, Wang BX, Dai GD, et al. Epidemiological survey on the prevalence of osteoporotic fractures in elderly people in Pingshan, Shenzhen. Clin Res. 2014;4:637–9. https://doi.org/10.3969/j.issn.1671-7171.2014.04.005
Yang YS, Sun LY. Study on prevalence of osteoporotic vertebral compression fracture in middle-aged and elderly people in Guiyang area. Chin Foreign Med. 2013;32(24):65–6. https://doi.org/10.16662/j.cnki.1674-0742.2013.24.061
Chen F, Bai WD, Sun YW, et al. Epidemiological investigation and analysis of senile osteoporotic fractures in Luogang District, Guangzhou. Chin Mod Doctor. 2013;51(02):13–4.
Wang ZQ. Epidemiological investigation and analysis of osteoporotic fracture in Changchun City. Changchun: Jilin University; 2012.
Wang H, Li C, Xiang Q, et al. Epidemiology of spinal fractures among the elderly in Chongqing, China. Injury 2012;43(12): 2109–2116. https://doi.org/10.1016/j.injury.2012.04.008.
Chen WY, Zhang S, Ding XL. Investigation on the prevalence of osteoporosis and fracture in the elderly in Haikou. Chin J Gerontol. 2010;30(06):824–6.
Zhang W, Di J, Wang Y, et al. Incidence of osteoporotic fracture in elderly population in Hebei Province and analysis of related factors. Hebei Med. 2009;31(14):1826–7.
Xie JQ, Lao HC, Zhao G. Preliminary statistics and analysis of primary osteoporotic fractures in some elderly people in Zhaotong, Yunnan Province. Chin J Bone Tumors Osteopathies. 2009;8(05):260–2.
Ma H, Li WJ, Feng WL, et al. Preliminary investigation on the epidemiology of osteoporotic fractures in the elderly in Xishuangbanna. Chin J Bone Tumors Bone Dis. 2009;8(05):263–5.
Zhao G, Hu ZM, Lao HC, et al. Preliminary investigation and analysis of incidence of osteoporotic fracture in some elderly population in Kunming. Chin J Osteoporosis. 2007;04:257–9.
Zhang JX, Wang HM, Zhang S, et al. Epidemiological investigation of senile osteoporotic fractures in rural Quanzhou City. Chin J Osteoporosis. 2007;12:860–3.
Zhu HM, Zhang Y, Zhu XY, et al. Changes in the prevalence of osteoporotic fractures in elderly patients in the past 8 years. Geriatrics Health Care. 2003;02:89–92.
Liu FY, Guo ZH, Feng Q, et al. Analysis of osteoporotic fractures and hunchback in multi-ethnic elderly people in Yunnan Province. Chin J Osteoporosis. 2002;03:50–4.
An Z, Yang DZ, Zhang ZJ, et al. Epidemiological investigation and analysis of osteoporotic vertebral compression fractures. Chin J Osteoporosis. 2002;1:86–7.
Shen L, Xie J, Yang YP, et al. A preliminary investigation on the incidence of osteoporotic fractures in elderly people in Wuhan. Chin J Orthopaedics Traumatol Tradit Chin Med. 2001;05:3–6.
Xu DL, Li FB, Chen WQ, et al. Epidemiological investigation and analysis of osteoporotic fractures and osteoarthropathy in elderly population in Guangzhou. Chin J Osteoporosis 2000;3:75–77+63.
Irani AD, Poorolajal J, Khalilian A, et al. Prevalence of osteoporosis in Iran: a meta-analysis. J Res Med Sci. 2013;18(9):759–66.
Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–6. https://doi.org/10.1002/jbmr.2269.
Fang Y, Zhu T. Advances in the treatment of postmenopausal osteoporosis. Chin J Osteoporosis. 2019;25(08):1192–200.
Park EJ, Joo IW, Jang M-J, et al. Prevalence of osteoporosis in the Korean population based on Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2011. Yonsei Med J. 2014;55(4):1049–57. https://doi.org/10.3349/ymj.2014.55.4.1049.
Eisman J, Clapham S, Kehoe L. Osteoporosis prevalence and levels of treatment in primary care: the Australian BoneCare Study. J Bone Min Res. 2004;19(12):1969–75. https://doi.org/10.1359/jbmr.040905.
Siris ES, Brenneman SK, Barrett-Connor E, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50–99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006;17(4):565–74. https://doi.org/10.1007/s00198-005-0027-4.
McGuire. Institute of Medicine. 2009. School meals: building blocks for healthy children. Washington, DC: the National Academies Press. Advances in nutrition (Bethesda, Md), 2011, 2(1): 64–65. https://doi.org/10.3945/an.110.000018.
Osteoporosis and bone mineral salt Disease Branch, Chinese Medical Association.Guidelines for Diagnosis and treatment of primary osteoporosis (2017). Chinese Journal of Osteoporosis and Bone Mineral Salt Diseases 2017;10(5):413–444.
LiuFu GJ. Investigation of bone mineral density of postmenopausal women in Maoming area and study on the detection rate of different parts. Chin Med Innov. 2017;14(13):72–5.
Migliorini F, Maffulli N, Spiezia F, et al. Biomarkers as therapy monitoring for postmenopausal osteoporosis: a systematic review. J Orthopaedic Surg Res 2021;16(1): 318. https://doi.org/10.1186/s13018-021-02474-7.
Migliorini F, Maffulli N, Spiezia F, et al. Potential of biomarkers during pharmacological therapy setting for postmenopausal osteoporosis: a systematic review. J Orthop Surg Res. 2021;16(1):351. https://doi.org/10.1186/s13018-021-02497-0.
Bulletin of the 7th National Population Census (No. 5)—Age Composition of the population. Chinese Statistics, 2021, (05): 10–11.
Epidemiological survey of osteoporosis in China and release of the results of the special action of "Healthy Bones". Chinese Journal of Osteoporosis and bone mineral Salt Diseases, 2019;12(04):317–318.
Migliorini, F., Giorgino, R., Hildebrand, F., et al. Fragility fractures: Risk factors and management in the elderly. Medicina (Kaunas, Lithuania), 2021. https://doi.org/10.3390/medicina57101119.
Migliorini F, Colarossi G, Eschweiler J, et al. Antiresorptive treatments for corticosteroid-induced osteoporosis: a Bayesian network meta-analysis. Br Med Bull. 2022;143(1):46–56. https://doi.org/10.1093/bmb/ldac017.
Migliorini F, Maffulli N, Colarossi G, et al. Effect of drugs on bone mineral density in postmenopausal osteoporosis: a Bayesian network meta-analysis. J Orthop Surg Res. 2021;16(1):533. https://doi.org/10.1186/s13018-021-02678-x.
Acknowledgements
We thank all colleagues working in the Department of Epidemiology and Health Statistics at the Second School of Clinical Medicine, Zhejiang University of Traditional Chinese Medicine.
Funding
The study was funded by the National Natural Science Foundation of China (82274272); National Natural Science Foundation of China (81973884); Natural Science Foundation of Zhejiang Province (LY19H290004); Zhejiang Traditional Chinese Medicine Administration (2022ZZ020); Zhejiang Traditional Chinese Medicine Administration (2022ZA085); Department of Education of Zhejiang Province, (Y202248737). These funders had no role in the study design, data collection, and analysis, interpretation of data, and writing the manuscript.
Author information
Authors and Affiliations
Contributions
SLM is responsible for thesis writing and article; MHT and YY are accountable for the conception and design, feasibility analysis, and revision of the thesis. BBT and YGC are responsible for collecting data, extracting and analyzing data, and quality evaluation; KL and XLS conducted revision and overall quality control. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval is not necessary for the meta-analysis of the published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Basic characteristics of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Meng, S., Tong, M., Yu, Y. et al. The prevalence of osteoporotic fractures in the elderly in China: a systematic review and meta-analysis. J Orthop Surg Res 18, 536 (2023). https://doi.org/10.1186/s13018-023-04030-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04030-x