Abstract
Background
Large malignant bone tumors and revision limb salvage procedures often result in massive bone loss, leaving a short residual bone segment that cannot accommodate a standard stem for endoprosthesis fixation. Three-dimensional-printed (3DP) short stem with porous structure seems to be an alternative for short-segment fixation. This retrospective study aims to evaluate surgical outcomes, radiographical results, limb functions, and complications of using 3DP porous short stems in massive endoprosthesis replacement.
Methods
Between July 2018 to February 2021, 12 patients with massive bone loss undergoing reconstruction with custom-made, short-stemmed massive endoprostheses were identified. Endoprosthesis replacement involved the proximal femur (n = 4), distal femur (n = 1), proximal humerus (n = 4), distal humerus (n = 1), and proximal radius (n = 2).
Results
The mean percentage of resected bone was 72.4% of the whole length of the bone, ranging from 58.4 to 88.5%. The mean length of 3DP porous short stems was 6.3 cm. The median follow-up was 38 months (range, 22–58 months). The mean MSTS score was 89%, ranging from 77% to 93%. Radiographical assessment results showed bone in-growth to the porous structure in 11 patients, and the implants were well osseointegrated. Breakage of the 3DP porous short stem occurred in one patient intraoperatively. The patient developed aseptic loosening (Type 2) four-month after surgery and underwent revision with a plate applied to assist fixation. The implant survivorship was 91.7% at 2 years. No other complications were detected, such as soft-tissue failures, structural failures, infection, or tumor progression.
Conclusions
3DP custom-made short stem with porous structure is a viable method for fixation of the massive endoprosthesis in the short segment after tumor resection, with satisfactory limb function, great endoprosthetic stability, and low complication rates.
Similar content being viewed by others
Background
Limb salvage surgery has been the standard treatment for bone and soft-tissue tumors in extremities due to advances in imaging modalities, neoadjuvant chemotherapy, and surgical techniques [1,2,3]. Compared with biological reconstruction, endoprosthesis replacement following tumor resection brings many advantages, including immediate stability, rapid rehabilitation, and early weight bearing [4, 5]. In the last decades, modular stemmed endoprosthesis has become a widely used, preferred modality for the reconstruction of osteoarticular defects of the upper and lower extremities [6, 7]. However, large malignant bone tumors and revision limb salvage procedures often result in massive bone loss, leaving a short residual bone segment that cannot accommodate a standard intramedullary stem [8].
In this situation, a short-stemmed endoprosthesis is a common choice to avoid total endoprosthesis replacement which impairs function significantly because of sacrificing two native joints [9]. Nevertheless, short-stemmed endoprostheses conceivably have an increased risk of aseptic loosening [8]. Nowadays, several techniques have been developed especially to improve the fixation efficacy in the short segment, such as compress osseointegration stems [10, 11], short stems with cross-pin [12, 13], or extra-cortical plate [8], and telescope allograft augment technique [14]. Using these techniques, a 9–22% failure rate due to aseptic loosening or structural failure at short- to long-term follow-up has been demonstrated.
Recently, three-dimensional-printed (3DP) endoprosthesis has become a powerful tool for complex reconstruction in extremities, improving limb and joint salvage rates [15]. Moreover, a 3DP short stem with porous structure seems to be an alternative for short-segment fixation and has been reported that creates a stable endoprosthesis fixation in intercalary reconstruction [16,17,18]. However, the clinical efficacy and outcomes of using this technique in osteoarticular reconstruction for fixation of the massive endoprosthesis remain unclear. Previously, resection of an extensive length of bone has been shown associated with implant failure, and the greater the percentage of bone resected, the greater the probability of failure [19]. Therefore, it is necessary and interesting to examine whether 3DP porous short stem is an alternative for short-segment fixation of the massive endoprosthesis.
This retrospective study aims to evaluate surgical outcomes, radiographical assessments, limb functions, and complications of using 3D-printed porous short stems in massive endoprosthesis replacement.
Methods
Patients
Institutional review board approval was obtained for this retrospective study. Twelve patients with massive bone loss underwent reconstruction with 3DP custom-made, short-stemmed massive endoprostheses between July 2018 to February 2021 were identified. A short stem was defined as being < 100 mm in length. A total of nine primary reconstructions following primary tumor resection and three revision procedures were performed. According to the anatomical site, endoprosthesis replacement involved the proximal femur (n = 4), distal femur (n = 1), proximal humerus (n = 4), distal humerus (n = 1), and proximal radius (n = 2). There were five females and seven males, with a mean age at the time of diagnosis of 35 years. Preoperatively, all patients underwent detailed radiography examinations, including X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) of the affected limb. Details of each patient’s diagnosis and clinical characteristics were collected and are shown in Table 1.
Endoprosthesis properties
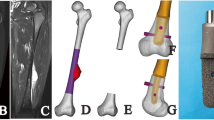
All endoprostheses were custom-made for each patient, and all short porous stems were designed by our clinical team. Firstly, CT scan data (DICOM format) were collected and imported into Mimics software for reconstructing 3D models (Fig. 1). After that, osteotomy was simulated based on the safe excision margin determined by pre-operative X-ray, CT, and MRI. The short stem was designed by imitating the shape of the remaining medullary cavity, which was described in detail in our previous articles [16, 20]. A total of three types of short stems were designed for fixation of the endoprosthesis in the short residual bone segments: diaphysis curved stem in the distal femur segment, intra-neck curved stem in the proximal femur segment, and straight stem in the proximal humerus, distal humerus, and distal radius segment. After that, the stem (STL format) was separated into two parts: an internal solid body and an external porous structure layer (2.5 mm in the femur, 1.5 mm in the humerus, and 1 mm in the radius). Lastly, modular endoprostheses were prepared for the proximal femur replacement, the distal femur replacement, and the proximal humerus replacement. And bionic hemi-elbow implants were prepared for the distal humerus and proximal radius replacement (Additional files 1).
All the implants were fabricated by Chunli Co., Ltd. (Tongzhou, Beijing, China). The short stems with the porous structure and bionic hemi-elbow implants were fabricated using the electron beam melting technique (ARCAM Q10plus). And the modular endoprostheses were manufactured through the forging method, which can be assembled with the 3DP porous short stem.
Surgical procedure and postoperative management
All the surgeries were performed by the same senior surgeon (Fig. 2). After general anesthesia, the patient's position and surgical approach were selected based on the location of the tumor to obtain adequate tumor exposure. Careful dissection of the soft tissue, as well as identification and protection of related major neurovascular structures, were performed. And then, osteotomies were undertaken precisely according to the preoperative design. Next, the medullary cavity was reamed, and the porous short stem was inserted into the prepared medullary cavity. The insertion of transverse screws was determined by the stability evaluation intraoperatively. At last, soft-tissue coverage of the endoprosthesis was performed.
Postoperatively, the operative lower limb was kept non-weight bearing with a splint or brace for 4–6 weeks after surgery. Thereafter, patients were encouraged to gradually increase weight bearing on the affected limb, while for the upper limbs, the operative limb was protected with a brace for 3–4 weeks after surgery. After that, the patients were allowed to have motion as tolerated.
Follow-up and evaluation
All patients were followed up once a month for the first 3 months and every 3 months thereafter. At each follow-up, the patients underwent detailed physical examinations. X-ray was performed to evaluate the implant status, regularly (Fig. 3). In addition, the T-SMART was used to evaluate the bone in-growth to the porous structure. The surgical outcomes, including intraoperative complications, operative time, and blood loss, were collected from the operation records. The limb functions were evaluated according to the Musculoskeletal Tumor Society (MSTS) scoring system. Complications were categorized according to the Henderson classification: soft-tissue failure (Type 1), aseptic loosening (Type 2), structural failure (Type 3), infection (Type 4), and tumor progression (Type 5) [21].
Statistical analysis
Descriptive statistics including medians, means, and percentages were conducted. Kaplan–Meier survival analysis was used to analyze implant survivorship, which was defined as the time from primary endoprosthesis replacement to revision surgery due to any reason.
Results
The mean resection length was 22.5 cm (12.5–31 cm). The mean percentage of resected bone was 72.4% of the whole length of the bone, ranging from 58.4 to 88.5%. The mean length of the 3DP porous short stem was 6.3 cm. The median follow-up was 38.5 months (range, 22–58 months). At the latest follow-up, all 12 patients were disease-free, without local tumor recurrence or distant metastasis.
Surgical outcomes
Breakage of the 3DP porous short stem occurred in one patient intraoperatively, leaving only the proximal part of the stem preserved for fixation. For another 11 patients, the endoprosthesis was successfully implanted according to the postoperative planning, without any intraoperative nerve or vessel injury occurring. While there was one periprosthetic fracture intraoperatively, and a wire was applied to assist fixation. The mean operative time was 168 min, and the mean intraoperative blood loss was 430 ml.
Radiological and functional outcomes
Bone in-growth to the porous structure was seen in all 11 patients with successful implantation (Fig. 4). And the radiographic results revealed good interfaces in the 11 3DP porous stems. After surgery, all patients experienced satisfactory limb function, and the mean MSTS score was 89%, ranging from 77% to 93%.
Complications
The patient with intraoperative breakage of the stem developed aseptic loosening (Type 2) four-month after the surgery (Additional file 2). Revision surgery was performed with a plate applied to assist fixation. The endoprosthesis condition was good at the last follow-up. In the remaining 11 patients, no other complications were detected, such as soft-tissue failures, structural failures, infection, or tumor progression. The implant survivorship was 91.7% at 2 years (Fig. 5).
Discussion
Limb-sparing surgery for patients with extensive bone loss, which often results in a short residual bone segment, remains a great challenge for surgeons. An alternative is using 3DP porous short stem for fixation of the massive endoprosthesis in the short segment. This approach aims to promote osseointegration and permanent biologic fixation by providing a porous interface. This paper retrospectively analyzed the clinical results of 3DP porous short stem in massive endoprosthesis replacement. Exciting results were observed in our series, with satisfactory limb function, great endoprosthetic stability, and low complication rates.
In all 12 patients, following sacrificing one joint inevitably, successful preservation of another native joint was achieved, and the bone defects were successfully reconstructed with short-stemmed endoprostheses. As function outcomes, MSTS scores at the last follow-up averaged 89%, comparable with the results of modular standard length stemmed endoprosthesis in other publications [22, 23]. Other than short-stemmed endoprosthesis, total femur/humerus replacement is another common option for the treatment of large malignant bone tumors of the femur/humerus. In a study by Sevelda et al. [24], 34 patients undergoing conventional and 10 patients undergoing expandable total femur replacements were followed up for a mean of 57 months and 172 months, respectively. The mean MSTS score was 70% (27–97%) of total femur replacement and 88% (60–97%) of expandable total femur replacement, respectively. Schneider et al. [25] reported the functional outcome of total humeral replacement after tumor resection; the median MSTS score in 9 of 13 surviving patients after a median follow-up of 75 months was 87% (67–92%). Compared with total femur/humerus replacement, 3DP short-stemmed endoprosthesis avoided the sacrifice of two native joints, resulting in better limb function.
In the present study, the implants were well osseointegrated in all 11 patients with successful implantation of 3DP porous short stems. And the radiographic assessment results revealed good interfaces in the 11 3DP porous stems. When fixation of the endoprosthesis in a short segment, a short stem reduces the bone/cement interface or bone in-growth interface, and therefore the endoprosthetic stability is reduced. Previously, cross-pin [10, 11] and extra-cortical plate [8] were frequently selected to assist the stability of the short stem. Despite the initial stability being relatively easy to secure with the assistance of these two techniques, concerns regarding the long-term survival of endoprostheses remain due to their high failure rates. Additionally, fixation with an extra-cortical plate requires adequate cortex exposure, which might imperil the attachment of non-osseous tissue around the joint and therefore impair joint stability. In addition, the telescope allograft technique is developed to augment the length of the native bone when residual bone stock is insufficient for a standard stem, with the advantage of lengthening the bone stock [14]. But the use of allograft inevitably involves the complications related to poor integration with host bone, such as a nonunion and delayed union. In our study, porous short stems were custom-made to match the shape of the remaining medullary cavity. The stem with an ellipse cross section, curved shape, and transverse screws enabled primary fixation. And the plate was only selected to assist initial stability in patients undergoing revision, in which the medullary cavity was incomplete after primary replacement failure. The stem was equipped with a porous structure rather than a coating surface, to facilitate osseointegration. Therefore, custom-made porous short stems created great endoprosthetic stability in our series.
Aseptic loosening remains a common cause of megaprosthetic reconstruction failure in the current generation of implants [26]. Further study has shown that the presence of a radiolucent area of more than 20% without cortical expansion remodeling is an important risk main of loosening due to the contact area of the bone-endoprosthesis decreases [27]. Similarly, short residual bone stock after extensive tumor resection restricts the stem length, and therefore also reduces the contact area of the bone-endoprosthesis. It has been suggested that a greater than 50% of the resection length to the whole length of bone might lead to a higher rate of loosening [9]. A study by Guo et al. also found that a resection length of greater than 14 cm independently predicted the failure of cemented endoprostheses [28]. In the present study, 3DP porous short-stemmed endoprosthesis seems to be not insensitive to resection length. The percentage of resection of bone was > 50% of the length of the bone in all patients, but ranged from 58.4 to 88.5% of the whole length of the bone. Except for one case with 3DP short stem breakage intraoperatively, no aseptic loosening was observed with a median follow-up of 38 months in 11 patients with successful implantation of the stem. Anatomically, a short residual metaphyseal segment is reverse-funnel-shaped, with a larger diameter in shorter the bone segment. This means that the stem is limited in length in the shorter bone segment, while the diameter of the stem can increase. Therefore, the porous interface of the 3DP short stem for osteointegration can be secure in a shorter stem with a larger diameter.
In this present study, only one complication needs further revision. Indeed, that was a design mistake, the transverse screws reducing the internal solid body of the stem and impairing the strength. With regard to the design of the porous stem for endoprosthesis fixation in a thin medullary cavity, consideration should be given to using the transversal screws carefully. In addition, no other complications were detected. The implant survivorship was 91.7% at 2 years (Additional file 1).
Certain limitations of this study should be noted. First, this is a retrospective study with no comparison group or control group. Secondly, the number of patients included in this study is relatively small. Third, the time of follow-up was relatively short, and the clinical outcome needs to be further investigated with long-term follow-up (Additional file 2).
Conclusion
3DP custom-made short stem with porous structure is a viable method for fixation of the massive endoprosthesis in the short segment after tumor resection, with satisfactory limb function, great endoprosthetic stability, and low complication rates.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Evans DR, Lazarides AL, Visgauss JD, Somarelli JA, Blazer DG, Brigman BE, Eward WC. Limb salvage versus amputation in patients with osteosarcoma of the extremities: an update in the modern era using the National Cancer Database. BMC Cancer. 2020;20(1):995.
Imura Y, Takenaka S, Kakunaga S, Nakai T, Wakamatsu T, Outani H, Tanaka T, Tamiya H, Oshima K, Hamada K. Survival analysis of elderly patients with osteosarcoma. Int Orthop. 2019;43:1741–7.
Zhang Z, Shi Y, Fu J, Liu D, Zhu D, Liu X, Dang J, Fan H. Customized three dimensional printed prosthesis as a novel intercalary reconstruction for resection of extremity bone tumours: a retrospective cohort study. Int Orthop. 2022;46(12):2971–81.
Zekry KM, Yamamoto N, Hayashi K, Takeuchi A, Alkhooly AZA, Abd-Elfattah AS, Elsaid ANS, Ahmed AR, Tsuchiya H. Reconstruction of intercalary bone defect after resection of malignant bone tumor. J Orthop Surg. 2019;27(1):2309499019832970.
Haddad BI, Alisi MS, Yasin MS, Hamdan MQ, Hassan FOA. Lower limb reconstruction using tibial strut autograft after resection of primary malignant bone tumors in skeletally immature patients. Arch Bone Joint Surg. 2021;9(5):567.
Theil C, Schwarze J, Gosheger G, Moellenbeck B, Schneider KN, Deventer N, Klingebiel S, Grammatopoulos G, Boettner F, Schmidt-Braekling T. Implant survival, clinical outcome and complications of megaprosthetic reconstructions following sarcoma resection. Cancers. 2022;14(2):351.
Grinberg SZ, Posta A, Weber KL, Wilson RJ: Limb salvage and reconstruction options in osteosarcoma. Curr Adv Osteosarcoma Clin Persp Past Present Future 2020:13–29.
Stevenson J, Wigley C, Burton H, Ghezelayagh S, Morris G, Evans S, Parry M, Jeys L. Minimising aseptic loosening in extreme bone resections: custom-made tumour endoprostheses with short medullary stems and extra-cortical plates. Bone Joint J. 2017;99(12):1689–95.
Qu H, Guo W, Yang R, Tang X, Yan T, Li D, Yang Y, Zang J. Cortical strut bone grafting and long-stem endoprosthetic reconstruction following massive bone tumour resection in the lower limb. Bone Joint J. 2015;97(4):544–9.
Calvert GT, Cummings JE, Bowles AJ, Jones KB, Wurtz LD, Randall RL. A dual-center review of compressive osseointegration for fixation of massive endoprosthetics: 2- to 9-year followup. Clin Orthop Relat Res. 2014;472(3):822–9.
Goulding KA, Schwartz A, Hattrup SJ, Randall RL, Lee D, Rispoli DM, Lerman DM, Beauchamp C. Use of compressive osseointegration endoprostheses for massive bone loss from tumor and failed arthroplasty: a viable option in the upper extremity. Clin Orthopaedics Relat Res®. 2017;475:1702–11.
Bernthal N, Upfill-Brown A, Burke Z, Ishmael C, Hsiue P, Hori K, Hornicek F, Eckardt J. Long-term follow-up of custom cross-pin fixation of 56 tumour endoprosthesis stems: a single-institution experience. Bone Joint J. 2019;101(6):724–31.
Cannon CP, Eckardt JJ, Kabo JM, Ward WG Sr, Kelly CM, Wirganowicz PZ, Asavamongkolkul A, Nieves R, Eilber FR. Custom cross-pin fixation of 32 tumor endoprostheses stems. Clin Orthopaedics Relat Res. 2003;417:285–92.
Hindiskere S, Staals E, Donati DM, Manfrini M. What is the survival of the telescope allograft technique to augment a short proximal femur segment in children after resection and distal femur endoprosthesis reconstruction for a bone sarcoma? Clin Orthop Relat Res. 2021;479(8):1780–90.
Benady A, Meyer JS, Ran Y, Mor Y, Gurel R, Rumack N, Golden E, Gortzak Y, Segal O, Merose O. Intercalary and geographic lower limb tumor resections with the use of 3D printed Patient Specific Instruments-when less is more. J Orthop. 2022;32:36–42.
Wang J, An J, Lu M, Zhang Y, Lin J, Luo Y, Zhou Y, Min L, Tu C. Is three-dimensional–printed custom-made ultra-short stem with a porous structure an acceptable reconstructive alternative in peri-knee metaphysis for the tumorous bone defect? World J Surg Oncol. 2021;19(1):1–11.
Zhao D, Tang F, Min L, Lu M, Wang J, Zhang Y, Zhao K, Zhou Y, Luo Y, Tu C. Intercalary reconstruction of the “ultra-critical sized bone defect” by 3D-printed porous prosthesis after resection of tibial malignant tumor. Cancer Manag Res. 2020;12:2503.
Shao X, Dou M, Yang Q, Li J, Zhang A, Yao Y, Chu Q, Li K, Li Z. Reconstruction of massive bone defects after femoral tumor resection using two new-designed 3D-printed intercalary prostheses: a clinical analytic study with the cooperative utilization of multiple technologies. BMC Musculoskelet Disord. 2023;24(1):1–17.
Unwin P, Cannon S, Grimer R, Kemp H, Sneath R, Walker P. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br. 1996;78(1):5–13.
You Q, Lu M, Min L, Zhang Y, Wang J, Wang Y, Zheng C, Zhou Y, Tu C. Hip-Preserved reconstruction using a customized cementless intercalary endoprosthesis with an intra-neck curved stem in patients with an ultrashort proximal femur: midterm follow-up outcomes. Front Bioeng Biotechnol. 2022;10: 795485.
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. JBJS. 2011;93(5):418–29.
Tsukushi S, Nishida Y, Hirose T, Nakata E, Nakagawa R, Nakamura T, Imanishi J, Nagano A, Tamiya H, Ueda T. Short-term clinical outcomes of Kyocera Modular Limb Salvage System designed cementless stems for the endoprosthetic reconstruction of lower extremities: a Japanese Musculoskeletal Oncology Group multi-institutional study. BMC Cancer. 2022;22(1):781.
Yan T-Q, Zhou W-H, Guo W, Yang R-L, Dong S, Liang W-M, Sun Y-F. Endoprosthetic reconstruction for large extremity soft-tissue sarcoma with juxta-articular bone involvement: functional and survival outcome. J Surg Res. 2014;187(1):142–9.
Sevelda F, Schuh R, Hofstaetter JG, Schinhan M, Windhager R, Funovics PT. Total femur replacement after tumor resection: limb salvage usually achieved but complications and failures are common. Clin Orthopaedics Relat Res®. 2015;473(6):2079–87.
Schneider KN, Bröking JN, Gosheger G, Lübben T, Hardes J, Schorn D, Smolle MA, Theil C, Andreou D. What is the implant survivorship and functional outcome after total humeral replacement in patients with primary bone tumors? Clin Orthop Relat Res. 2021;479(8):1754.
Pala E, Trovarelli G, Calabrò T, Angelini A, Abati CN, Ruggieri P. Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthopaedics Rela Res®. 2015;473:891–9.
Piakong P, Kiatisevi P, Yau R, Trovarelli G, Lam Y-L, Joyce D, Ruggieri P, Temple HT, Letson D, Binitie O. What is the 10-year survivorship of cemented distal femoral endoprostheses for tumor reconstructions and what radiographic features are associated with survival? Clin Orthop Relat Res. 2020;478(11):2573.
Guo W, Ji T, Yang R, Tang X, Yang Y. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg Br. 2008;90(8):1084–9.
Funding
This work was supported by 1·3·5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18036).
Author information
Authors and Affiliations
Contributions
ZZL, MXL, YL, and CQT were involved with the concept and design of this manuscript. TJG and YQZ were involved with the acquisition of the subject and data. ZZL, YQZ, MXL, and CQT were involved in the design of the prosthesis. LM, YZ, LM, and CQT were involved in the postsurgical evaluation of the patient. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki as revised in 2008 and was authorized by the Ethics Committee of West China Hospital. The patient signed the informed consent form before surgery.
Consent for publication
The patients provided informed consent to publish and report individual clinical data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Video showing bionic implant design of proximal radius.
Additional file 2.
A child aged 11 years with breakage of the porous short stem intraoperatively. (a) X-ray after the surgery showing only the proximal part of the stem preserved and inserted the residual segment; (b) X-ray four months after the surgery showing aseptic loosening; (c) revision was performed with a plate applied to assist fixation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Lu, M., Zhang, Y. et al. 3D-printed custom-made short stem with porous structure for fixation of massive endoprosthesis in joint‐preserving reconstruction after tumor resection. J Orthop Surg Res 18, 468 (2023). https://doi.org/10.1186/s13018-023-03954-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03954-8