Abstract
Background
To obtain the complication rate, fusion rate, and revision rate of the lumbar cortical bone trajectory technique and pedicle screw fixation technique in lumbar interbody fusion surgery by single-arm meta-analysis and lay a basis for orthopedic surgeons to select the fixation techniques and perioperative management.
Methods
PubMed, Ovid Medline, Web of Science, CNKI, and Wanfang databases were searched comprehensively. Data extraction, content analysis, and quality assessment of the literature were performed by two independent reviewers according to the Cochrane Collaboration guidelines using R and STATA software for single-arm meta-analysis.
Results
The total complication rate of the lumbar cortical bone trajectory technique was 6%, including a hardware complication rate of 2%, ASD (adjacent segment degeneration) rate of 1%, wound infection rate of 1%, dural damage rate of 1%, hematoma rate tending to 0%, fusion rate of 94%, and revision rate of 1%. Lumbar pedicle screw fixation techniques had a total complication rate of 9%, with a hardware complication rate of 2%, ASD rate of 3%, wound infection rate of 2%, dural damage rate of 1%, hematoma rate tending to 0%, fusion rate of 94%, and revision rate of 5%. This study was registered with PROSPERO, CRD42022354550.
Conclusion
Lumbar cortical bone trajectory was associated with a lower total complication rate, ASD rate, wound infection rate, and revision rate than pedicle screw fixation. The cortical bone trajectory technique reduces the incidence of intraoperative and postoperative complications and can be an alternative in lumbar interbody fusion surgery.
Similar content being viewed by others
Introduction
In 1959, the pedicle screw (PS) fixation technique that can simultaneously penetrate the three-column structure of the spine was proposed [1, 2]. However, pedicle screws used in patients with osteoporosis are prone to loosening and breakage due to the destruction of the trabecular structure and loss of bone mass resulting in reduced holding strength of the screw [3,4,5]. Santoni et al. proposed the cortical bone trajectory (CBT) technique in 2009 and compared with the pedicle screw (PS) fixation technique, the special screw trajectory of CBT allows most of the screw surrounded by the cortical bone, giving it better mechanical stability and fixation strength [6,7,8,9,10]. In recent years, the CBT technique has gradually gained clinical favor by its advantages of smaller wounds, shorter operative time, and less intraoperative blood loss [11]. However, there was no study that discussed the specific complication, fusion, and revision rate of the two techniques in detail. A single-arm meta-analysis was then performed to provide a reference for the selection of fixation techniques in lumbar interbody fusion surgery and perioperative management.
Methods
Literature search
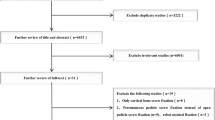
PubMed, Ovid Medline, Web of Science, CNKI, and Wanfang databases were searched for papers published until July 2022 using the following strategies: “Lumbar,” “Pedicle screw,” “PS,” “Traditional trajectory,” “TT,” “Cortical bone trajectory,” “cortical bone trajectory screw,” “Cortical bone screw,” “Cortical screw,” “CS,” “CBS,” “CBT,” “CBTS” with various combinations of the “AND” and “OR.” The references of all retrieved literature were manually searched one by one to improve the recall rate of the literature, and the language was limited to English and Chinese. The systematic review and single-arm meta-analysis were performed with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR2) [12]. A flow diagram of the literature searching strategy is shown in Fig. 1.
Flow diagram of study selection [12]
Study selection and data extraction
After completion of the literature search, all retrieved studies were checked and duplicates were removed. Two reviewers (Wang and Kahaer) independently assessed the quality of each retrieved literature to determine whether they were included and then cross-checked, with a third evaluator (Rexiti) handling any disagreements. After selection, two independent reviewers (Wang and Kahaer) extracted baseline data from the included literature, including authors, publication date, study type, number of events, mean age, gender, follow-up time, and fusion technique. Then, the type and number of complications, number of patients with bone fusion, and number of patients with revision in each literature were extracted to the predesigned data extraction sheet. This study was registered with PROSPERO and updated regularly, ID CRD42022354550.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (1) Literature included patients with lumbar interbody fusion surgery using CBT screw and PS; (2) Preoperative diagnosis of lumbar degenerative diseases, lumbar tuberculosis; (3) Surgical levels were single or double; and (4) Literature reported one of the rates of complication, fusion, and revision.
Exclusion criteria were as follows: (1) Only include the CBT or PS in lumbar interbody fusion surgery; (2) Previous history of lumbar surgery; (3) Patients with lumbar tumors and fractures; (4) Severe medical system diseases, such as chronic obstructive pulmonary disease, coagulation abnormalities, long-term use of glucocorticoids, hypertension in grade III and above; (5) Three or more surgical segments; (6) Follow-up less than 6 months (7) Letter to editor, review, and conference paper.
Quality assessment
Randomized controlled trials (RCTs) were assessed using the Cochrane Risk Bias Assessment Tool, and non-randomized controlled studies (cohort studies, case–control studies) were assessed using the Newcastle–Ottawa Scale (NOS).
Statistical analysis
Statistical methods were described in PRISMA statement. Forest plots were drawn by R software version 4.2.1. After importing the raw data into R software, PRAW, PLOGIT, PLN, PAS, and PFT were used to transform the original rates of complication, fusion, and revision of each literature, respectively. The transformed rate was tested for normal distribution. The method closest to normal distribution was selected according to the test results. Then, the combined rate and 95% confidence interval (CI) were obtained by metaprop function and a forest plot was drawn. When I2 < 50% and/or P > 0.1 (low heterogeneity), a fixed-effect model was selected; otherwise, the random-effect model was selected. STATA 16 (Stata Corp., College Station, TX, USA) was used to analyze the sensitivity when I2 > 50%. The specific method was to exclude the literature one by one to obtain the combined conversion rate and 95% CI for determining the effect of each literature on the combined effect size.
Results
Literature characteristic and quality assessment
The literature search yielded 1118 studies, including 835 in English and 283 in Chinese. After removing duplicates, 797 studies were retrieved. Screening by title and abstract left 341 studies for full-text analysis. After full-text screening, it left 38 studies. According to the inclusion and exclusion criteria, 29 studies [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41] met the inclusion criteria, 22 in English and 6 in Chinese. Two RCTs [32, 34], six prospective studies [13, 14, 20, 27, 35, 36], and 21 retrospective studies [15,16,17,18,19, 21,22,23,24,25,26, 28,29,30,31, 33, 37, 38, 40, 41] were included. A total of 982 patients with CBT and 1105 patients with PS were compared. One retrospective cohort study [38] did not report the specific follow-up time, but the hardware complication (intraoperative screw malposition) did not require long-term follow-up;thus, it was included. Among the included studies, Lai et al. [26] included patients with lumbar tuberculosis and the rest research only included patients with lumbar degenerative diseases. Summary of study characteristics is presented in Table 1. Although the follow-up population of Lai’s study was osteoporotic patients with lumbar spinal tuberculosis, we only cited the occurrence of Hardware events in that study, so the impact on this study was not significant.
Two RCTs showed that the articles were of good quality, and the specific assessment result is shown in Fig. 2. The NOS assessment results showed the scores of all included studies covered high-quality 6–9 points, defined as high-quality points. The specific assessment results are shown in Table 2.
Total complication rate
Total complication rate of CBT
Twenty-four studies [13, 14, 16, 17, 19,20,21,22,23, 25,26,27,28,29,30,31,32,33,34, 37,38,39,40,41] consisting of 862 patients reported the complications of CBT (n = 77). There was a significant heterogeneity (I2 = 84%, P < 0.01). Meta-analysis was performed using a random-effects model. Combined statistics showed a total complication rate of 6% (95% CI [3, 12%]) (Fig. 3).
Total complication rate of PS
Twenty-four studies [13, 14, 16, 17, 19,20,21,22,23, 25,26,27,28,29,30,31,32,33,34, 37,38,39,40,41] (consistent with the total complications of CBT) consisting of 998 patients reported the complications of PS (n = 108). There was a significant heterogeneity (I2 = 87%, P < 0.01). Meta-analysis was performed using a random-effects model. Combined statistics showed a total complication rate of 9% (95% CI [4, 15%]) (Fig. 4).
Hardware complication rate
Hardware complications of CBT
Nineteen studies [13, 16, 17, 19,20,21,22,23, 27, 28, 30,31,32,33,34, 37, 38, 40, 41] consisting of 592 patients reported the hardware complications of CBT (n = 23). There was no significant heterogeneity (I2 = 43%, P = 0.03). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a hardware complication rate of 2% (95% CI [1, 4%]) (Fig. 5). Specific types of hardware complications are shown in Table 3.
Hardware complications of PS
Nineteen studies [13, 16, 17, 19,20,21,22,23, 27, 28, 30,31,32,33,34, 37, 38, 40, 41] (consistent with the hardware complications of CBT) consisting of 773 patients reported the hardware complications of PS (n = 29). There was a significant heterogeneity (I2 = 60%, P < 0.01). Meta-analysis was performed using a random-effects model. Combined statistics showed a hardware complication rate of 2% (95% CI [0, 5%]) (Fig. 6). Specific types of hardware complications are shown in Table 3.
Incidence of adjacent segment degeneration (ASD)
ASD in CBT
Eleven studies [13, 14, 19, 20, 22, 23, 28, 30, 32,33,34] consisting of 418 patients reported the incidence of ASD in CBT (n = 10). There was no heterogeneity (I2 = 17%, P = 0.28). Meta-analysis was performed using a fixed-effects model. Combined statistics showed the incidence of ASD was 1% (95% CI [0, 3%]) (Fig. 7).
ASD in PS
Eleven studies [13, 14, 19, 20, 22, 23, 28, 30, 32,33,34] (consistent with the ASD in CBT) consisting of 406 patients reported the incidence of ASD in PS (n = 23). There was a significant heterogeneity (I2 = 70%, P < 0.01). Meta-analysis was performed using a random-effects model. Combined statistics showed the incidence of ASD was 3% (95% CI [0, 7%]) (Fig. 8).
Wound infection rate
Wound infection of CBT
Seventeen studies [13, 16, 19,20,21,22,23, 25, 27,28,29,30,31, 33, 34, 39, 41] consisting of 637 patients reported the wound infection of CBT (n = 10). There was no significant heterogeneity (I2 = 0%, P = 0.93). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a wound infection rate of 1% (95% CI [0, 2%]) (Fig. 9).
Wound infection of PS
Seventeen studies [13, 16, 19,20,21,22,23, 25, 27,28,29,30,31, 33, 34, 39, 41] (consistent with wound infection of CBT) consisting of 733 patients reported the wound infection of PS (n = 20). There was no significant heterogeneity (I2 = 0%, P = 0.99). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a wound infection rate of 2% (95% CI [1, 4%]) (Fig. 10).
Incidence of dural damage
Incidence of dural damage in CBT
Nineteen studies [13, 16, 17, 19,20,21,22,23, 25, 28,29,30,31, 33, 34, 37, 39,40,41] consisting of 492 patients reported incidence of dural damage in CBT (n = 15). There was no significant heterogeneity (I2 = 29%, P = 0.12). Meta-analysis was performed using a fixed-effects model. Combined statistics showed the incidence of dural damage was 1% (95% CI [0, 3%]) (Fig. 11).
Incidence of dural damage in PS
Nineteen studies [13, 16, 17, 19,20,21,22,23, 25, 28,29,30,31, 33, 34, 37, 39,40,41] (consistent with incidence of dural damage in CBT) consisting of 750 patients reported incidence of dural damage in PS (n = 16). There was no significant heterogeneity (I2 = 0%, P = 0.58). Meta-analysis was performed using a fixed-effects model. Combined statistics showed the incidence of dural damage was1% (95% CI [0, 2%]) (Fig. 12).
Incidence of hematoma
Incidence of hematoma in CBT
Thirteen studies [13, 16, 19,20,21,22,23, 25, 28,29,30, 33, 34] consisting of 461 patients reported the hardware complications of CBT (n = 4). There was no significant heterogeneity (I2 = 0%, P = 1.00). Meta-analysis was performed using a fixed-effects model. Combined statistics showed the incidence of hematoma was 0% (95% CI [0, 1%]) (Fig. 13).
Incidence of hematoma in PS
Thirteen studies [13, 16, 19,20,21,22,23, 25, 28,29,30, 33, 34] (consistent with the incidence of hematoma in CBT) consisting of 549 patients reported the hardware complications of PS (n = 2). There was no significant heterogeneity (I2 = 0%, P = 0.97). Meta-analysis was performed using a fixed-effects model. Combined statistics showed the incidence of hematoma was 0% (95% CI [0, 0%]) (Fig. 14).
Fusion rate
Fusion rate of CBT
Seventeen studies [13, 15, 17, 18, 21,22,23,24,25, 28, 32,33,34,35,36, 39, 41] consisting of 569 patients reported the fusion rate of CBT (n = 526). There was no significant heterogeneity (I2 = 39%, P = 0.05). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a fusion rate of 94% (95% CI [92, 96%]) (Fig. 15).
Fusion rate of PS
Seventeen studies [13, 15, 17, 18, 21,22,23,24,25, 28, 32,33,34,35,36, 39, 41] (consistent with the fusion rate of CBT) consisting of 619 patients reported the fusion rate of PS (n = 578). There was no significant heterogeneity (I2 = 41%, P = 0.04). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a fusion rate of 94% (95% CI [92, 96%]) (Fig. 16).
Revision rate
Revision rate of CBT
Eight studies [14, 16, 19, 22, 23, 27, 37, 39] consisting of 390 patients reported the revision rate of CBT (n = 5). There was no significant heterogeneity (I2 = 0%, P = 0.48). Meta-analysis was performed using a fixed-effects model. Combined statistics showed a revision rate of 1% (95% CI [0, 2%]) (Fig. 17).
Revision rate of PS
Eight studies [14, 16, 19, 22, 23, 27, 37, 39] (consistent with the revision rate of CBT) consisting of 410 patients reported the revision rate of PS (n = 23). There was a significant heterogeneity (I2 = 56%, P = 0.03). Meta-analysis was performed using a random-effects model. Combined statistics showed a revision rate of 5% (95% CI [2, 8%]) (Fig. 18).
Sensitivity analysis
In this study, seven of the results showed I2 > 50%, including the total complication rate of CBT, total complication rate of PS, hardware complication rate of PS, ASD rate of PS, and revision rate of PS. The sensitivity analysis results were as follows (Additional file 1: Figure S1, Additional file 2: Figure S2, Additional file 3: Figure S3, Additional file 4: Figure S4, Additional file 5: Figure S5). Lai et al. [26] had a slight effect on the meta-analysis results of the total complication rate of CBT and PS, the other literature had no significant effect on the combined effect size, and the meta-analysis results were stable.
Discussion
To solve the problem of decreased pedicle screw holding force caused by trabecular structure destruction and bone loss in patients with osteoporosis, which is leading to screw loosening and breakage, Santoni et al. [6] proposed the CBT technique in 2009. In recent years, the CBT technique has gradually become popular in clinical practice [11, 42]. However, there is still a lack of large-sample clinical studies, which affects the clinical application of the CBT technique.
At present, the studies on the clinical efficacy of CBT and PS techniques mainly focus on the comparison of complication rate, fusion rate, revision rate, operation time, blood loss, and other indicators. Keorochana et al. [43] and Qiu et al. [44] demonstrated that the CBT technique had a lower total complication rate than the PS technique. Wang et al. [8] demonstrated that the CBT technique had a lower ASD rate than the PS technique, but there were no significant differences in the hardware complication rate, wound infection rate, fusion rate, and revision rate. Kim et al. [45] confirmed that the CBT technique had lower ASD rate, total complication rate, and revision rate than the PS technique, but no significant differences in hardware complication rate, wound infection rate and fusion rate. Chang et al. [46] proved that the CBT technique had lower ASD rate and total complication rate than the PS technique, but no significant difference in hardware complication rate and wound infection rate. Zhang et al. [47] showed that the CBT technique had lower ASD rate and total complication rate than the PS technique, but there was no difference in fusion rate. Overall, the available studies concluded that the CBT technique was superior in reducing the incidence of ASD and total complications to the PS technique, but there were some controversies existed in fusion rate, revision rate, and hardware complication rate.
However, the aforementioned studies did not give specific statistics on complication rate, fusion rate, and revision rate for the two techniques with large sample sizes. This study synthesized 29 published studies to discuss the complication rate, fusion rate, and revision rate for the CBT and PS techniques in lumbar interbody fusion surgery. This study demonstrated that the total complication rate of the CBT technique was 6%, with a hardware complication rate of 2%, ASD rate of 1%, wound infection rate of 1%, dural damage rate of 1%, low hematoma rate tending to 0%, fusion rate of 94%, and revision rate of 1%. The total complication rate of the PS technique was 9%, with a hardware complication rate of 2%, ASD incidence of 3%, the wound infection rate of 2%, dural damage incidence of 1%, hematoma incidence tending to 0%, fusion rate of 94%, and revision rate of 5%. On balance, the results of this study are similar to those of published literature on the clinical efficacy of the CBT and PS techniques, further demonstrating the reliability of the findings of this study.
ASD was a common complication due to degeneration of the adjacent segmentafter lumbar interbody fusion surgery [48]. ASD occurs mainly in the upper segment above the fused segment and was considered to be an important factor affecting patient prognosis [48, 49]. The results of this study showed a slightly lower incidence rate of ASD with the CBT technique than with the PS technique, and we believe that this result is related to the following factors. First, soft tissue damage at the surgical site is a potential cause of ASD [49,50,51,52], and PS placement requires extensive expose of fascia, muscles, and ligaments, whereas the CBT technique requires only a small amount of muscle stripping at the paravertebral level to complete the surgery due to the inward insertion point, which causes less damage to soft tissues at the surgical site. Peng et al. [29] and Ohkawa et al. [53] measured blood creatine kinase concentrations in patients treated with the CBT technique and the PS technique respectively, and found that the blood creatine kinase concentrations in patients treated with the CBT technique were significantly lower than those in patients treated with the PS technique, which also indicated that the CBT technique caused less damage to the muscle tissue around the surgical site. Second, several biomechanical studies have shown that the increased disk stress in adjacent segments can lead to the development of ASD [49, 54, 55]. Liu et al. [56] demonstrated that the intervertebral disk stress in the adjacent segmentsfor pedicle screw fixation technique was significantly greater than that of the cortical bone trajectory technique in flexion, extension, lateral bending, and rotation, so the incidence of ASD was lower for the cortical bone trajectory technique than for the pedicle screw fixation technique. Third, degeneration of facet joints was an independent risk factor for the development of ASD [57, 58]. The PS placement inevitably damages the facet joint, which in turn leads to uneven forces on the upper lumbar disk during axial rotation and further decreases the stability of the vertebral body, thus further accelerating the development of ASD [59, 60].
Wound infections in lumbar interbody fusion surgery often lead to unfavorable prognoses [61]. The greater operative time, blood loss, postoperative drainage, and the size of the incision were the important risk factors for postoperative wound infection. Several studies [45,46,47,48, 62,63,64,65] demonstrated that the operative time, intraoperative blood loss, and the size of the incision of the CBT technique were significantly lower than those of the PS technique. In terms of postoperative drainage, Liu et al. [27] demonstrated that the postoperative drainage of the CBT technique (102 ± 10 ml) was significantly lower than that of the PS technique (246 ± 15 ml) and that the operative time, intraoperative blood loss, postoperative drainage, and the size of the incision were all superior to those of the PS technique, resulting in a lower rate of postoperative wound infection.
The conventional concept was that the revision rate of the CBT technique is higher than that of the PS technique because of the high difficulty of inserting the CBT screw. The CBT technique mainly passes through the cortical bone located at the lamina and the medial wall of the pedicle and has a higher cephalad angle and lateral angle, making it possible to cause the pedicle fracture or screw entering the spinal canal, which leads to a higher revision rate and a lower fusion rate [66, 67]. However, this study demonstrated that the revision rate of the CBT technique was slightly lower than that of the PS technique. The result is related to the following factors. First, screw malpositioning and loosening was the main cause of revision [66, 68], and some advanced techniques are often used as an aid when inserting the CBT screw, such as the use of a 3D printing guiding plate, intraoperative CT navigation, and robotics to confirm the entry point and trajectory, which can undoubtedly improve the accuracy of screw placement [69,70,71]. Also, due to the difficulty of the CBT technique, most of the surgeons have been systematically trained for increasing the accuracy of the procedure before operation. Second, cancellous bone is more prone to osteoporosis than cortical bone. For every 10 g/cm3 decrease in bone density, the maximum pullout resistance of the screw decreases by 60 N [72]. Compared with the PS technique, the CBT technique has a higher cephalad angle and lateral angle, and the vast majority of the screw trajectory was surrounded with the cortical bone, allowing for the better biomechanical stability [42, 73]. In this study, we concluded that the CBT technique has a higher fusion rate,lower revision and complication rate.
This study has several limitations. This study differs from the traditional meta-analysis, which can only yield superiority and inferiority between different techniques. This study is a single-arm meta-analysis to derive specific complication, fusion, and revision rate, based on which the two techniques were compared. Although this single-arm meta-analysis minimized the heterogeneity, some limitations remain. For example, to make the CBT technique comparable with the PS technique, only the literature that included both techniques was included, and those that used only one technique were not included. In addition, the studies included in this study were mainly retrospective studies, and there were only two RCTs, which may increase the bias. This study demonstrated that the total complication rate of the CBT technique was lower than that of the PS technique, in which there was only a slight difference in recent complications except for the rate of wound infection, but a large difference in remote complications. Further changes in complication,fusion and revision rate in the lumbar PS and CBT techniques need to be further evaluated by large-sample multi-center RCTs.
Conclusion
The total rates of complications, ASD, wound infection, and revision of the CBT technique were lower than those of the PS technique in lumbar interbody fusion surgery, and there was a slight difference between the other results. CBT technique might be an alternative choice in clinical application.
Availability of data and materials
All datasets generated for this study are included in the article/Additional file 6.
References
Boucher HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41-B(2):248–59.
Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VKH, Papadopoulos SM, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976). 2005;30(8):915–22.
Rosinski A, Odeh K, Ungurean VJ, Leasure J, Kondrashov D. Non-pedicular fixation techniques for the treatment of spinal deformity: a systematic review. JBJS Rev. 2020;8(5):e0150–e0150.
Tarawneh AM, Salem KMI. A systematic review and meta-analysis of randomized controlled trials comparing the accuracy and clinical outcome of pedicle screw placement using robot-assisted technology and conventional freehand technique. Glob Spine J. 2021;11(4):575–86.
Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am Vol. 1999;81A(11):1519–28.
Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MAW, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366–73.
Mai HT, Mitchell SM, Hashmi SZ, Jenkins TJ, Patel AA, Hsu WK. Differences in bone mineral density of fixation points between lumbar cortical and traditional pedicle screws. Spine J. 2016;16(7):835–41.
Wang J, He X, Sun T. Comparative clinical efficacy and safety of cortical bone trajectory screw fixation and traditional pedicle screw fixation in posterior lumbar fusion: a systematic review and meta-analysis. Eur Spine J. 2019;28(7):1678–89.
Matsukawa K, Kaito T, Abe Y. Accuracy of cortical bone trajectory screw placement using patient-specific template guide system. Neurosurg Rev. 2020;43(4):1135–42.
Baluch DA, Patel AA, Lullo B, Havey RM, Voronov LI, Nguyen NL, et al. Effect of physiological loads on cortical and traditional pedicle screw fixation. Spine (Phila Pa 1976). 2014;39(22):E1297–302.
Momin AA, Steinmetz MP. Evolution of minimally invasive lumbar spine surgery. World Neurosurg. 2020;140:622–6.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2020;2021:88.
Marengo N, Ajello M, Pecoraro MF, Pilloni G, Vercelli G, Cofano F, et al. Cortical bone trajectory screws in posterior lumbar interbody fusion: minimally invasive surgery for maximal muscle sparing-a prospective comparative study with the traditional open technique. Biomed Res Int. 2018;2018:1–7.
Sakaura H, Ikegami D, Fujimori T, Sugiura T, Mukai Y, Hosono N, et al. Early cephalad adjacent segment degeneration after posterior lumbar interbody fusion: a comparative study between cortical bone trajectory screw fixation and traditional trajectory screw fixation. J Neurosurg Spine. 2020;32(2):155–9.
Sakaura H, Ikegami D, Fujimori T, Sugiura T, Yamada S, Mukai Y. Surgical outcomes after posterior lumbar interbody fusion using traditional trajectory screw fixation or cortical bone trajectory screw fixation: a comparative study between the polyetheretherketone cage and the same shape titanium-coated polyetheretherke. Clin Neurol Neurosurg. 2021;209:106945.
Takenaka S, Mukai Y, Tateishi K, Hosono N, Fuji T, Kaito T. Clinical outcomes after posterior lumbar interbody fusion: comparison of cortical bone trajectory and conventional pedicle screw insertion. Clin Spine Surg. 2017;30(10):E1411–8.
Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Kudo D, Shimada Y. Short-term results of transforaminal lumbar interbody fusion using pedicle screw with cortical bone trajectory compared with conventional trajectory. Asian Spine J. 2015;9(3):440–8.
Konomi T, Yasuda A, Fujiyoshi K, Yato Y, Asazuma T. Incidences and risk factors for postoperative non-union after posterior lumbar interbody fusion with closed-box titanium spacers. Asian Spine J. 2020;14(1):106–12.
Ninomiya K, Iwatsuki K, Ohnishi YI, Yoshimine T. Radiological evaluation of the initial fixation between cortical bone trajectory and conventional pedicle screw technique for lumbar degenerative spondylolisthesis. Asian Spine J. 2016;10(2):251–7.
Orita S, Inage K, Kubota G, Sainoh T, Sato J, Fujimoto K, et al. One-year prospective evaluation of the technique of percutaneous cortical bone trajectory spondylodesis in comparison with percutaneous pedicle screw fixation: a preliminary report with technical note. J Neurol Surg Part A Cent Eur Neurosurg. 2016;77(6):531–7.
Nakajima N, Maenaka T, Kano H. Postoperative low back pain after posterior lumbar interbody fusion surgery using cortical bone trajectory screws. Asian Spine J. 2020;14(5):655–62.
Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Posterior lumbar interbody fusion with cortical bone trajectory screw fixation versus posterior lumbar interbody fusion using traditional pedicle screw fixation for degenerative lumbar spondylolisthesis: a comparative study. J Neurosurg Spine. 2016;25(5):591–5.
Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Cortical bone trajectory screw fixation versus traditional pedicle screw fixation for 2-level posterior lumbar interbody fusion: comparison of surgical outcomes for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2018;28(1):57–62.
Hung CW, Wu MF, Hong RT, Weng MJ, Yu GF, Kao CH. Comparison of multifidus muscle atrophy after posterior lumbar interbody fusion with conventional and cortical bone trajectory. Clin Neurol Neurosurg. 2016;145:41–5.
Wang CY, Yuan HW, Tian ZH. Comparison results between cortical bone trajectory screw and conventional pedicle screw in posterior lumbar interbody fusion for single-segment degenerative lumbar disease. J Clin Orthop. 2018;21(4):444–7.
Lai Z, Shi SY, Fei J, Han GH, Hu SP. Case-control study on cortical bone trajectory screw and pedicle screw internal fixation for the treatment of senile patients with lumbar tuberculosis. China J Orthop Traumatol. 2020;33(7):636–42.
Liu YZ, Hai Y, Zhang XN, Yin P, Liu T, Ding HT, et al. Comparison of cortical bone trajectory screw fixation and pedicle screw fixation in posterior lumbar fusion. Natl Med J China. 2019;99(19):1473–8.
Sundar K. Comparison of clinical outcomes of transforaminal lumbar interbody fusion with cortical bone trajectory screws and traditional pedicle screws fixation. 2019. Doi:10.27014/d.cnki.gdnau.2019.001399
Peng J, Zhan Y, Liu Y, Zong Y, Mao Y. Comparison of effectiveness of cortical bone trajectory screw fixation and pedicle screw fixation in posterior lumbar interbody fusion. Chin J Reparative Reconstr Surg. 2017;31(11):1341–5.
Zhang P, Ye J, Huang L, Ying X, Zhu B, Jin Y, et al. Comparison of affected-vertebra fixation of cortical bone trajectory screw and pedicle screw for lumbar tuberculosis: a minimum 3-year follow-up. Biomed Res Int. 2022;2022:1–7.
Zhang HQ, Wang CC, Zhang RJ, Zhou LP, Jia CY, Ge P, et al. Predictors of accurate intrapedicular screw placement in single-level lumbar (L4–5) fusion: robot-assisted pedicle screw, traditional pedicle screw, and cortical bone trajectory screw insertion. BMC Surg. 2022;22(1):1–10.
Lee GW, Ahn MW. Comparative study of cortical bone trajectory-pedicle screw (cortical screw) versus conventional pedicle screw in single-level posterior lumbar interbody fusion: a 2-year post hoc analysis from prospectively randomized data. World Neurosurg. 2018;109:E194–202.
Lee GW, Shin JH. comparative study of two surgical techniques for proximal adjacent segment pathology after posterior lumbar interbody fusion with pedicle screws: fusion extension using conventional pedicle screw vs cortical bone trajectory-pedicle screw (cortical screw). World Neurosurg. 2018;117:E154–61.
Lee GW, Son JH, Ahn MW, Kim HJ, Yeom JS. The comparison of pedicle screw and cortical screw in posterior lumbar interbody fusion: a prospective randomized noninferiority trial. Spine J. 2015;15(7):1519–26.
Chen YR, Deb S, Pham L, Singh H. Minimally invasive lumbar pedicle screw fixation using cortical bone trajectory—a prospective cohort study on postoperative pain outcomes. Cureus. 2016;8(7):e714–e714.
Chin KR, Lubinski JR, Zimmers KB, Sands BE, Pencle F. Clinical experience and two-year follow-up with a one-piece viscoelastic cervical total disc replacement. J Spine Surg. 2017;3(4):630–40.
Hoffman H, Verhave B, Jalal MS, Beutler T, Galgano MA, Chin LS. Comparison of cortical bone trajectory screw placement using the midline lumbar fusion technique to traditional pedicle screws: a case-control study. Int J Spine Surg. 2019;13(1):33–8.
Wochna JC, Marciano R, Catanescu I, Katz J, Spalding MC, Narayan K. Cortical trajectory pedicle screws for the fixation of traumatic thoracolumbar fractures. Cureus. 2018;10(6):e2891–e2891.
Malcolm JG, Moore MK, Choksh FH, Ahmad FU, Refai D. Comparing cortical trajectory transforaminal lumbar interbody fusions against pedicle trajectory transforaminal lumbar interbody fusions and posterolateral fusions: a retrospective cohort study of 90-day outcomes. Neurosurgery. 2018;83(6):1234–9.
Liu Z, Kou H, Shang G, Ji Y, Chen X, Sun Z, et al. Comparison of cortical bone trajectory screws and traditional trajectory screws in treatment of lumber degenerative patients with osteoporosis: a retrospective analysis. Chin J Anat Clin. 2020;25(3):278–84.
Fu R, Geng X, Fu G, Bing A. Cortical bone trajectory versus traditional pedicle screw techniques for osteoporotic lumbar degenerative disease. Orthop J China. 2020;28(5):405–10.
Delgado-Fernandez J, Garcia-Pallero MA, Blasco G, Pulido-Rivas P, Sola RG. Review of cortical bone trajectory: evidence of a new technique. Asian Spine J. 2017;11(5):817–31.
Keorochana G, Pairuchvej S, Trathitephun W, Arirachakaran A, Predeeprompan P, Kongtharvonskul J. Comparative outcomes of cortical screw trajectory fixation and pedicle screw fixation in lumbar spinal fusion: systematic review and meta-analysis. World Neurosurg. 2017;102:340.
Qiu L, Niu F, Wu Z, Zhang W, Chen F, Tan J, et al. Comparative outcomes of cortical bone trajectory screw fixation and traditional pedicle screws in lumbar fusion: a meta-analysis. World Neurosurg. 2022;164:e436–45.
Kim KT, Song MG, Lee EC, Seo MS, Lee DY, Kim DH. Can the cortical bone trajectory screw technique be an alternative method to the pedicle screw in posterior lumbar fusion? A systematic review and metaanalysis. Acta Orthop Traumatol Turc. 2021;55(6):552–62.
Chang MC, Choo YJ, Lee GW. Pedicle screws versus cortical screws in posterior lumbar interbody fusion surgery for degenerative spondylolisthesis: a systematic review and meta-analysis. Spine J. 2021;21(7):1126–34.
Zhang T, Guo N, Chen T, Yan J, Zhao W, Xu G. Comparison of outcomes between cortical screws and traditional pedicle screws for lumbar interbody fusion: a systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):1–11.
Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Takahashi Y, Iwasaki M. Adjacent segment disease after single segment posterior lumbar interbody fusion for degenerative spondylolisthesis minimum 10 years follow-up. Spine (Phila Pa 1976). 2018;43(23):E1384–8.
Saavedra-Pozo FM, Deusdara RAM, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014;14(1):78–83.
Nassr A, Lee JY, Bashir RS, Rihn JA, Eck JC, Kang JD, et al. Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine (Phila Pa 1976). 2009;34(2):189–92.
Kim HJ, Kelly MP, Ely CG, Dettori JR, Riew KD. The risk of adjacent-level ossification development after surgery in the cervical spine: are there factors that affect the risk? A systematic review. Spine (Phila Pa 1976). 2012;37(221):S65–74.
Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am Vol. 2005;87A(3):558–63.
Ohkawa T, Iwatsuki K, Ohnishi Y, Ninomiya K, Yoshimine T. Isthmus-guided cortical bone trajectory reduces postoperative increases in serum creatinine phosphokinase concentrations. Orthop Surg. 2015;7(3):232–8.
Dmitriev AE, Cunningham BW, Hu NB, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty—an in vitro human cadaveric model. Spine (Phila Pa 1976). 2005;30(10):1165–72.
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002;27(22):2431–4.
Liu CW, Wang LL, Xu YK, Chen CM, Wang JC, Tsai WT, et al. Traditional and cortical trajectory screws of static and dynamic lumbar fixation- a finite element study. BMC Musculoskelet Disord. 2020;21(1):463.
Choi KC, Kim JS, Shim HK, Ahn Y, Lee SH. Changes in the adjacent segment 10 years after anterior lumbar interbody fusion for low-grade isthmic spondylolisthesis. Clin Orthop Relat Res. 2014;472(6):1845–54.
Oh HS, Seo HY. The relationship between adjacent segment pathology and facet joint violation by pedicle screw after posterior lumbar instrumentation surgery. J Clin Med. 2021;10(13):2911.
Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976). 1998;23(14):1550–8.
Kim HJ, Chun HJ, Lee HM, Kang KT, Lee CK, Chang BS, et al. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J. 2013;13(10):1301–8.
Chen SH, Lee CH, Huang KC, Hsieh PH, Tsai SY. Postoperative wound infection after posterior spinal instrumentation: analysis of long-term treatment outcomes. Eur Spine J. 2015;24(3):561–70.
Deng H, Chan AK, Ammanuel SG, Chan AY, Oh T, Skrehot HC, et al. Risk factors for deep surgical site infection following thoracolumbar spinal surgery. J Neurosurg Spine. 2020;32(2):292–301.
Fei Q, Li J, Lin J, Li D, Wang B, Meng H, et al. Risk factors for surgical site infection after spinal surgery: a meta-analysis. World Neurosurg. 2016;95:507–15.
Fang C, Zhu T, Zhang P, Xia L, Sun C. Risk factors of neurosurgical site infection after craniotomy: a systematic review and meta-analysis. Am J Infect Control. 2017;45(11):E123–34.
Ee WWG, Lau WLJ, Yeo W, von Bing Y, Yue WM. Does minimally invasive surgery have a lower risk of surgical site infections compared with open spinal surgery? Clin Orthop Relat Res. 2014;472(6):1718–24.
Cheng WK, Akpolat YT, Inceoglu S, Patel S, Danisa OA. Pars and pedicle fracture and screw loosening associated with cortical bone trajectory: a case series and proposed mechanism through a cadaveric study. Spine J. 2016;16(2):E59–65.
Patel SS, Cheng WK, Danisa OA. Early complications after instrumentation of the lumbar spine using cortical bone trajectory technique. J Clin Neurosci. 2016;24:63–7.
Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976). 1993;18(15):2231–9.
Marengo N, Matsukawa K, Monticelli M, Ajello M, Pacca P, Cofano F, et al. Cortical bone trajectory screw placement accuracy with a patient-matched 3-dimensional printed guide in lumbar spinal surgery: a clinical study. World Neurosurg. 2019;130:E98–104.
Khan A, Rho K, Mao JZ, O’Connor TE, Agyei JO, Meyers JE, et al. Comparing cortical bone trajectories for pedicle screw insertion using robotic guidance and three-dimensional computed tomography navigation. World Neurosurg. 2020;141:E625–32.
Shi W, Aierken G, Wang S, Abuduwali N, Xia Y, Rezhake R, et al. Application study of three-dimensional printed navigation template between traditional and novel cortical bone trajectory on osteoporosis lumbar spine. J Clin Neurosci. 2021;85:41–8.
Petrone S, Marengo N, Ajello M, Lavorato A, Penner F, Cofano F, et al. Cortical bone trajectory technique’s outcomes and procedures for posterior lumbar fusion: a retrospective study. J Clin Neurosci. 2020;76:25–30.
Matsukawa K, Yato Y, Imabayashi H, Hosogane N, Asazuma T, Chiba K. Biomechanical evaluation of lumbar pedicle screws in spondylolytic vertebrae: comparison of fixation strength between the traditional trajectory and a cortical bone trajectory. J Neurosurg Spine. 2016;24(6):910–5.
Funding
This study was supported by the National Center for Orthopedics and Sports Rehabilitation Clinical Medicine, Clinical Application-oriented Medical Innovation Fund (approval no. 2021-NCRC-CXJJ-ZH-14).
Author information
Authors and Affiliations
Contributions
YXW and KA were involved in concept, literature search, and data collection. KA and MA were involved in statistics, data analysis, and interpretation. YXW, KA, and PR drafted the article. YXW, KA, HLG, and PR were involved in critical revision of article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study design was approved by the Ethics Committee of Xinjiang Medical University before data collection and analysis (approval no. 20210401-01). All methods were carried out in accordance with relevant guidelines and regulations.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Sensitivity analysis of total complication rate of CBT.
Additional file 2: Figure S2.
Sensitivity analysis of total complication rate of PS.
Additional file 3: Figure S3.
Sensitivity analysis of hardware complication rate of PS.
Additional file 4: Figure S4.
Sensitivity analysis of the incidence of ASD in PS.
Additional file 5: Figure S5.
Sensitivity analysis of revision rate of PS.
Additional file 6
: Table S1. CBT and PS data summary.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Kahaer, A., Maimaiti, A. et al. Complication, fusion, and revision rate in the lumbar cortical bone trajectory and pedicle screw fixation techniques: a systematic review and meta-analysis. J Orthop Surg Res 18, 382 (2023). https://doi.org/10.1186/s13018-023-03820-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03820-7