Abstract
Purpose
This study compares the efficacies of minimally invasive decompression by posterior microscopic mini-open technique combined with percutaneous pedicle fixation (hereafter MOT) to traditional open surgery in patients with severe traumatic spinal canal stenosis resulting from Arbeitsgemeinschaft für Osteosynthesefragen (AO) type A3 or A4 thoracolumbar burst fractures and provides references for clinical treatment.
Methods
In total, 133 patients with severe traumatic spinal canal stenosis caused by AO type A3 or A4 thoracolumbar burst fractures who underwent MOT (group A) or traditional open surgery (group B) were retrospectively enrolled. The demographic and radiological data of the two groups were analyzed and compared.
Results
A total of 64 patients were finally recruited in this study. There were no significant differences in gender, age, follow-up time, injury mechanism, injury level, AO classification, American Spinal Injury Association (ASIA) score, visual analogue scale (VAS) score, and duration of hospital stay between the two groups (P > 0.05). After the procedures, the prevertebral height ratio (PHR), the Cobb angle, and the mid-sagittal canal diameter compression ratio (MSDCR) were significantly improved (P < 0.05) in both groups. However, group A demonstrated less intraoperative bleeding and a greater VAS score improvement postoperatively and at the last follow-up but involved a longer operation time (P < 0.05). The PHR and the Cobb angle in the two groups showed no significant difference postoperatively and at the last follow-up (P > 0.05). In contrast, a significant improvement in MSDCR was observed at the last follow-up when compared with the postoperative value (P < 0.05). However, the Cobb angle in group A was better maintained than in group B at the last follow-up (P < 0.05), while the MSDCR in group B demonstrated a greater improvement at the last follow-up than in group A (P < 0.05).
Conclusions
Both the MOT and traditional open surgery are effective treatment options for AO type A3 and A4 thoracolumbar burst fractures with severe traumatic spinal stenosis. The advantages of MOT include the minimally invasive procedure, extremely fine spinal canal decompression, less intraoperative bleeding, and significant pain relief. We suggest that MOT should be preferentially performed for AO type A3 or A4 thoracolumbar burst fractures with severe traumatic spinal stenosis.
Similar content being viewed by others
Introduction
90% of all spinal fractures occur in the thoracolumbar region, and burst fractures account for approximately 60% of cases [1]. Thoracolumbar fractures can cause serious spinal cord injury [2]. Decompression surgery alleviates secondary spinal cord injury and improves neurological recovery after acute spinal cord injury. Short-segment posterior fixation, especially percutaneous minimally invasive fixation, is well accepted for thoracolumbar fractures [3,4,5,6]. However, decompression and bone grafting are challenging in patients with a mid-sagittal canal diameter compression ratio (MSDCR) exceeding 50% [3, 7].
To date, the efficacies of minimally invasive decompression by posterior microscopic mini-open technique combined with percutaneous pedicle fixation (hereafter MOT) and traditional open surgery for thoracolumbar burst fractures with severe traumatic spinal canal stenosis have rarely been reported. The current study compares the efficacies of the two surgical modalities.
Methods
Demographics
From January 2012 to January 2018, 133 consecutive patients with severe traumatic spinal canal stenosis caused by Arbeitsgemeinschaft für Osteosynthesefragen (AO) type A3 or A4 thoracolumbar burst fractures underwent MOT (group A) or traditional open surgeries (group B). Sixty-four patients completed the 1-year follow-ups and were retrospectively enrolled in this study. The inclusion criteria were: (I) patients with single segmental AO type A3 or A4 thoracolumbar fractures; (II) intra-canal fracture fragments causing canal compromise, MSDCR > 50%; (III) no severe damage to the adjacent disks; (IV) the posterior ligamentous complex (PLC) was not severely damaged; and (V) the patients were admitted within 2 weeks of injury. The exclusion criteria were: (I) patients with significant osteoporosis, endocrine diseases, tuberculosis, or other diseases which may affect the vertebral structure; (II) patients with congenital spinal stenosis; (III) patients with incomplete clinical records; and (IV) a follow-up period shorter than 12 months.
Clinical and radiographic records
All patient clinical and radiographic data were recorded at admission, postoperatively, and at the last follow-up (12–24 months after surgery). The clinical records included the general date, follow-up time, injury mechanism, hospital stay, operation time, intraoperative bleeding volume, visual analogue scale (VAS) score [8], American Spinal Injury Association (ASIA) scores [9], and AO spine injury classification [10].
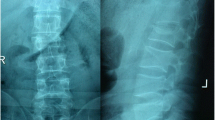
Radiographic data included the prevertebral height ratio (PHR) [3], the injured vertebral Cobb angle, and the mid-sagittal canal diameter compression ratio (MSDCR) [11]. See Fig. 1.
MOT methods
After general anesthesia, the patient was placed in a prone position, and the abdomen was suspended. Percutaneous pedicle screw fixation was performed under fluoroscopic guidance; percutaneous pedicle screws were placed in the superior and inferior vertebra adjacent to the injured vertebra. An approximately 3 cm posterior midline incision, centered on the injured vertebra, was performed to expose the lamina space of the injured vertebra. Fenestration of the vertebral lamina was then completed under microscopy, and the fracture fragments were visualized and repositioned into the vertebral body using the L-shaped operative tool, followed by longitudinal distraction of the vertebral body anterior margin. Subsequently, a curette was used to identify the fracture lines at the posterior wall of the injured vertebral body. Anterior and middle column reduction was performed and a 5-mm-diameter bone grafting channel was prepared. Proper reduction was confirmed using fluoroscopy, and autologous bones or allograft bones were implanted in the injured vertebral body via the bone grafting channel 3–4 mm deep from the posterior wall of the injured vertebral body. After adequate hemostasis, the wound was flushed, and a drainage tube was placed as necessary. The incisions were sutured layer by layer. See Fig. 2.
MOT methods a, b four guide needles were inserted into the adjacent vertebral pedicles under fluoroscopic guidance; c the positions of the percutaneous pedicle screws were confirmed radiographically after implantation; d fenestration of the vertebral lamina was performed via the 3 cm incision under microscopy; e visualizing and repositioning the fracture fragments into the vertebral body under microscopy; f using a curette to pry the injured endplates to achieve anterior and middle column reduction; g the satisfactory reduction was confirmed by lateral radiograph; h autologous bones and allograft bones were implanted in the injured vertebral body under microscopy; i a drainage tube was placed, and the incision was intradermally sutured
Statistical analysis
The SPSS20.0 statistical software (IBM Corp., Armonk, NY, USA) was used for data analysis. Quantitative data were presented as mean ± standard deviation. Within-group comparisons of PHR, Cobb angle, MSDCR, and VAS score at multiple time points were analyzed with repeated measures analysis of variance combined with Bonferroni correction. Mann–Whitney U test was used for ASIA scores within-group comparisons. Age, follow-up time, hospital stay, operation time, intraoperative bleeding volume, PHR, Cobb angle, MSDCR, and VAS score between the two groups were compared by independent-sample t tests. Gender, injury mechanism, injury level, and AO classification between the two groups were compared by chi-square test. A probability less than 0.05 was considered statistically significant.
Results
Comparison of general conditions
A total of 64 patients were finally recruited; 69 patients were excluded due to incomplete clinical records or lost to follow-up. These 64 patients included 28 patients who underwent MOT and were classified as group A (21 males and 7 females), and 36 patients who underwent traditional open surgeries and were classified as group B (25 males and 11 females). Statistical analysis revealed no significant intergroup differences in gender, age, follow-up time, injury mechanism, injured level, AO classification, ASIA score, and MSDCR between the two groups (all P > 0.05, Table 1).
Perioperative data
All procedures were completed successfully. No significant difference was found concerning the duration of hospital stay between both groups (P > 0.05, Table 2). A longer mean operative time and lower mean intraoperative bleeding volume were found in group A compared to group B. The differences were statistically significant (all P < 0.05).
Radiographic findings
The PHR, the Cobb angle, and the MSDCR in the two groups after surgery and at the last follow-up were significantly improved when compared with the preoperative values (all P < 0.05, Table 3). No significant difference in PHR and Cobb angle was found between the two groups after the operation and at the last follow-up (P > 0.05), but improvements in MSDCR were observed at the last follow-up compared with the postoperative values (P < 0.05).
The preoperative PHR was heavier in group B than in group A (P < 0.05), but there was no significant difference between the postoperative and last follow-up values (P > 0.05). The Cobb angle in group B was larger than in group A before the operation (P < 0.05), showing no significant difference from the postoperative values (P > 0.05). However, the Cobb angle in group A was better maintained than in group B at the last follow-up (P < 0.05). No significant difference in MSDCR was observed in the two groups between the preoperative and post-operation values (P > 0.05). In contrast, the MSDCR in group B showed a greater improvement than in group A at the last follow-up (P < 0.05).
Visual analogue scale (VAS) score
There was no significant difference in VAS score between the groups before operation (P > 0.05, Table 4). The VAS score on postoperative day 1 and at the last follow-up was significantly lower than the respective preoperative values in both groups (P < 0.05). However, the improvement in VAS score was significantly more favorable in Group A than in Group B (P < 0.05).
American Spinal Injury Association (ASIA) scores
The ASIA scores demonstrated significant differences between the preoperative values and the last follow-up values in the two groups (P < 0.05, Table 5).
A typical case of MOT
A 47-year-old male patient was diagnosed with AO type A4 fractures at the L2 level with a large posterior wall retropulsed fragment into the spinal canal, causing significant spinal canal encroachment, exhibiting ASIA E neurological status. MOT treatment resulted in improvements in the prevertebral height and Cobb angle, and the fragment in the spinal canal showed a good reduction. At the last follow-up, the patient had ASIA E neurological status, and the radiographic results showed good fracture union. Although partial bone graft resorption was observed, the prevertebral height, Cobb angle, and spinal canal patency were well maintained, see Fig. 3.
A 47-year-old man with L2 burst fracture (AO type A4) with severe traumatic spinal stenosis. a Preoperative anteroposterior radiograph; b preoperative lateral radiograph; c preoperative CT axial view; d preoperative CT sagittal view; e postoperative anteroposterior radiograph; f postoperative lateral radiograph; g postoperative CT axial view; h postoperative CT sagittal view; i 2-year postoperative anteroposterior radiograph; j 2-year postoperative lateral radiograph; k 2-year postoperative CT axial view; and l 2-year postoperative CT sagittal view
Discussion
The definition of severe traumatic spinal stenosis caused by thoracolumbar burst fractures
The definition of severe traumatic spinal stenosis of thoracolumbar fractures remains controversial. Wolter [12] defined a retropulsed fragment into the spinal canal causing MSDCR > 2/3 as severe spinal stenosis. Meves et al. [13] reported a positive correlation between spinal canal narrowing and the severity of the incomplete neurological deficit. Patients with 25, 50, and 75% narrowing of the thoracolumbar spinal canal exhibited a 12, 41, and 78% probability of neurological deficit, respectively. In the lumbar spinal canal, the probability was 8, 30, and 68%, respectively. Based on our previous experience, patients with MSDCR > 50% have a high probability of neurological deficit, which coincided with the findings of previous studies by Mohanty et al. [14] Therefore, MSDCR > 50% is recommended as a standard to define severe traumatic spinal stenosis due to difficult fracture reduction and the high probability of neurological deficit.
Advantages of MOT
MOT combines the advantages of minimally invasive procedures and open surgeries: (a) Percutaneous pedicle screw fixation and fenestration of the vertebral lamina were performed via the minimally invasive incisions while protecting the paraspinal muscle and PLC. Thoracolumbar segmental stability was maintained, and postoperative pain and bleeding were reduced [4]; (b) the fracture fragments can be directly and indirectly pressed into the fractured vertebral body using the L-shaped operative tool and the elastic tension of the posterior longitudinal ligament; and c) satisfactory anterior and middle column reduction and adequate bone graft can be achieved via the spinal canal (Fig. 3). In these studies, the postoperative PHR, Cobb angles, and MSDCR were improved compared with preoperative values (P < 0.05). The findings suggested that both the MOT and traditional open surgery effectively achieve decompression of the spinal canal, correct spinal deformity, and rebuild spinal stability. No significant difference was found in the PHR and the Cobb angle in the two groups between the postoperative values and the last follow-up values (P > 0.05), but the Cobb angle in group A was better maintained than in group B at the last follow-up (P < 0.05). Although both procedures can restore and maintain spinal stability, the MOT yields better results than traditional open surgery. The VAS score of the two groups was significantly lower after surgery (P < 0.05), while the VAS score of group A was lower than group B on postoperative day 1 and at the last follow-up (P < 0.05). MOT resulted in excellent pain relief. Four pedicle screw techniques are still controversial from the biomechanical point of view. However, no internal fixation failure was found during follow-up in this study. Considering the absence of serious PLC injury and dislocation in type A3 and A4 fractures, through adequate bone grafting in the vertebral body, correction of kyphosis, rigid fixation with four pedicle screws, protection of paraspinal muscles, and external fixation of the thoracolumbar brace, we believe that four pedicle screw techniques are effective for type A3 and A4 fractures.
The significance of using a surgical microscope in MOT
Due to the small and deep incision for decompression, a restricted view of the surgical area and inadequate lighting, such as in traditional open surgery, hinders the decompression procedure and compromises safety. The surgical microscope can compensate for the above limitations. The major advantages of the microscope include better illumination, magnification, and coaxial vision, which contribute to avoiding spinal cord and nerve root injuries as well as dural lesions [15]. The intraoperative bleeding volume of MOT was less than traditional open surgeries (P < 0.05). One major reason is the application of the surgical microscope, as the perivertebral venous plexus anatomy can be identified intraoperatively and controlled with compression hemostasis and electrocautery accurately [16].
Experience in MOT
Details of decompression and reduction
Type A3 fractures are incomplete burst fractures affecting a single endplate and the posterior wall. Type A4 fractures are complete burst fractures involving both endplates, with the involvement of the posterior cortex, a greater degree of height loss, and possible spinal canal encroachment. The latter is responsible for the highest incidence of neurological injury of all A subtypes. Depending on the severity of compression of the nerve root and spinal cord, different orders of decompression and reduction should be considered [17]. When neural tissue is severely compressed or immobilized by bony fragments in the spinal canal or fractured lamina, especially at the T11-12 vertebral level, the decompression and reduction should be performed in the following order: fenestration → longitudinal distraction → reduction by curette. Type A4 fractures are usually treated in this order. In the absence of serious compression or incarceration of neural tissue, the decompression and reduction should be performed as follows: longitudinal distraction → fenestration → reduction by curette. Type A3 fractures are usually treated in this order. Fenestration should be performed on the side of the neural tissue compression or severe injury. Unilateral fenestration is recommended unless the bilateral lamina or lateral wall of the spinal canal was fractured seriously.
Bone graft skills
In our previous study, sagittal fracture lines were observed over the pedicle horizontal in thoracolumbar fractures with loss of vertebral body height. This region overlaps with the interlaminar space, so a 3-cm incision at this region is sufficient for decompression, reduction, and bone graft. As the adjacent disks and PLC were not severely damaged, the MOT did not require posterolateral fusion or interbody fusion. Fixation was performed by the posterior approach and bone graft did not induce significant changes in the intervertebral spaces, and the anterior column achieved spontaneous fusion [6, 18,19,20]. In this study, the postoperative PHR and Cobb angle improved significantly (P < 0.05) and remained stable at the last follow-up (P < 0.05). These results are in accordance with the above points.
Treatment strategy for the spinal canal
Anatomic reduction is not necessary if the process may cause damage to the spinal cord or nerves. Miyashita et al. [21] found that there is no significant effect on the recovery of neurological function when MSDCR < 30%. After removing the fragments or soft tissues compressing the neural structures, bone resorption can complete spinal canal remodeling. This is related to intraspinal venous pulsation [22]. The results of this study showed no significant difference in MSDCR between preoperative and postoperative values in the two groups (P > 0.05), revealing that both the MOT and traditional open surgery effectively achieve decompression of the spinal canal. However, the MSDCR in traditional open surgery at the last follow-up (6.22 ± 2.54%) was superior to MOT (8.15 ± 4.83%) (P < 0.05). The mechanisms involved remain unclear and require further investigation.
Limitations in this study
This was a retrospective study with small sample size and a short follow-up time. To confirm the long-term effectiveness and advantages of MOT, the sample size should be expanded in further research. Meanwhile, the effectiveness after removing the internal fixation requires further investigation.
Conclusions
Both the MOT and traditional open surgery effectively treat AO type A3 and A4 thoracolumbar burst fractures with severe traumatic spinal stenosis. The advantages of MOT include minimal invasion, extremely fine spinal canal decompression, lower intraoperative bleeding, and obvious pain relief. We suggest that MOT should be preferentially performed for AO type A3 or A4 thoracolumbar burst fractures with severe traumatic spinal stenosis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MOT:
-
Minimal invasive decompression by posterior microscopic mini-open technique combined with percutaneous pedicle fixation
- AO:
-
Arbeitsgemeinschaft für Osteosynthesefragen classification
- ASIA:
-
American Spinal Injury Association score
- VAS:
-
Visual analogue scale score
- PHR:
-
Prevertebral height ratio
- MSDCR:
-
Mid-sagittal canal diameter compression ratio
- PLC:
-
Posterior ligamentous complex
References
Huang J, Zhou L, Yan Z, Zhou Z, Gou X. Effect of manual reduction and indirect decompression on thoracolumbar burst fracture: a comparison study. J Orthop Surg Res. 2020;15:532–9. https://doi.org/10.1186/s13018-020-02075-w.
Sharwood LN, Mueller H, Ivers RQ, Vaikuntam B, Driscoll T, Middleton JW. The epidemiology, cost, and occupational context of spinal injuries sustained while‘ working for income’ in NSW: a record-linkage study. Int J Environ Res Public Health. 2018;15:2121–9. https://doi.org/10.3390/ijerph15102121.
Yao W, Zhou T, Huang K, Dai M, Mo F, Xu J, et al. A comparison of monoaxial pedicle screw versus polyaxial pedicle screw in short-segment posterior fixation for the treatment of thoracolumbar fractured vertebra. Ann Transl Med. 2021;9:669–76. https://doi.org/10.21037/atm-21-881.
Wang X, Liu Y, Wang X, Chen H, Cao P, Tian Y, et al. Beneficial effects of percutaneous minimally invasive surgery for patients with fractures in the thoracic spine. Exp Ther Med. 2018;16:5394–9. https://doi.org/10.3892/etm.2018.6887.
Smits AJ, Polack M, Deunk J, Bloemers FW. Combined anteroposterior fixation using a titanium cage versus solely posterior fixation for traumatic thoracolumbar fractures: a systematic review and meta-analysis. J Craniovertebr Junction Spine. 2017;8:168–78. https://doi.org/10.4103/jcvjs.JCVJS_8_17.
Liang C, Liu G, Liang G, Zheng X, Yin D, Xiao D, et al. Healing pattern classification for thoracolumbar burst fractures after posterior short-segment fixation. BMC Musculoskelet Disord. 2020;21:373–82. https://doi.org/10.1186/s12891-020-03386-z.
Li X, Guan Z, Chen X, Chen B, Kong L, Han J, et al. Modified minimally invasive technique for decompression and reduction of thoracolumbar burst fracture with neurological symptoms: technical note. J Orthop Surg Res. 2021;16:626–32. https://doi.org/10.1186/s13018-021-02783-x.
Krasowska K, Skrobot W, Liedtke E, Sawicki P, Flis DJ, Dzik KP, et al. The preoperative supplementation with vitamin D attenuated pain intensity and reduced the level of pro-inflammatory markers in patients after posterior lumbar interbody fusion. Front Pharmacol. 2019;10:527–34. https://doi.org/10.3389/fphar.2019.00527.
Asia, Committee ISIS. The 2019 revision of the international standards for neurological classification of spinal cord injury (ISNCSCI)-what’s new? Spinal Cord. 2019;57:815–7. https://doi.org/10.1038/s41393-019-0350-9.
Reinhold M, Audige L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013;22:2184–201. https://doi.org/10.1007/s00586-013-2738-0.
Hashimoto T, Kaneda K, Abumi K. Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine. 1988;13:1268–72. https://doi.org/10.1097/00007632-198811000-00011.
Wolter D. Recommendation for the classification of spinal injuries. Unfallchirurg. 1985;88:481–4.
Meves R, Avanzi O. Correlation between neurological deficit and spinal canal compromise in 198 patients with thoracolumbar and lumbar fractures. Spine. 2005;30:787–91. https://doi.org/10.1097/01.brs.0000157482.80271.12.
Mohanty SP, Bhat NS, Abraham R, Ishwara KC. Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008;16:20–3. https://doi.org/10.1177/230949900801600105.
Damodaran O, Lee J, Lee G. Microscope in modern spinal surgery: advantages, ergonomics and limitations. ANZ J Surg. 2013;83:211–4. https://doi.org/10.1111/ans.12044.
Wang K, Shang F, Jian FZ, Wu H. Effect of simultaneous surgical treatment in scoliosis associated with intraspinal abnormalities: a retrospective study. Exp Ther Med. 2020;20:108–14. https://doi.org/10.3892/etm.2020.9236.
Bains RS, Althausen PL, Gitlin GN, Gupta MC, Benson DR. The role of acute decompression and restoration of spinal alignment in the prevention of post-traumatic syringomyelia: case report and review of recent literature. Spine (Phila Pa). 2001;26:399–402. https://doi.org/10.1097/00007632-200109010-00028.
Zhong W, Liang X, Luo X, Huang T, Quan Z. Complications rate of and risk factors for the unplanned reoperation of degenerative lumbar spondylolisthesis in elderly patients: a retrospective single-Centre cohort study of 33 patients. BMC Geriatr. 2020;20:301–6. https://doi.org/10.1186/s12877-020-01717-2.
Farcy JP, Weidenbaum M, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1990;15:958–65. https://doi.org/10.1097/00007632-199009000-00022.
Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture. Asian Spine J. 2015;9:133–46. https://doi.org/10.4184/asj.2015.9.1.133.
Miyashita T, Ataka H, Tanno T. Clinical results of posterior stabilization without decompression for thoracolumbar burst fractures: is decompression necessary? Neurosurg Rev. 2012;35:447–55. https://doi.org/10.1007/s10143-011-0363-0.
Sjostrom L, Jacobsson O, Karlstrom G, Pech P, Rauschning W. Spinal canal remodelling after stabilization of thoracolumbar burst fractures. Eur Spine J. 1994;3:312–7. https://doi.org/10.1007/BF02200143.
Acknowledgements
We thank the reviewers and editors for their helpful comments on this article.
Funding
This work was financially supported by the National Natural Science Foundation of China (Grant No. 31960209), Guizhou Science and Technology Fund Project (Grant No. [2020]1Y093).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with the approval from the Ethic committee of Affiliated Hospital of Zunyi Medical University.
Consent for publication
Written informed consent to publish the clinical details and images of the patient was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, B., Zhou, Y., Zou, H. et al. A comparative study on efficacies of posterior microscopic mini-open and open technique for thoracolumbar burst fractures with severe traumatic spinal stenosis. J Orthop Surg Res 17, 518 (2022). https://doi.org/10.1186/s13018-022-03412-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03412-x